Abstract
Background
The large number of diagnostic procedures undertaken in emergency departments (ED) is vital to the early diagnosis and treatment of patients. The use of ionising radiation in diagnosis adds a lifetime attributable risk (LAR) of cancer depending on the region imaged, the frequency of imaging, and dose per exposure.
Aims
This pilot study aims to assess the degree of radiation awareness amongst ED doctors at major metropolitan and regional health services in Australia, in terms of the dose and risks associated with common imaging. Secondary aims were to provide a template to practically evaluate ED doctor radiation awareness, identify factors impacting upon radiation awareness (e.g., location, seniority of doctor), and to suggest practical means to improve radiation awareness.
Methods
Physicians in the EDs of two major health services (one regional and one metropolitan) in Australia were surveyed and asked to compare the radiation dose from each procedure to what the general population is exposed to naturally from background radiation. Additionally, the physicians were asked to estimate the LAR of cancer from each diagnostic procedure. These estimates were compared to literature-sourced values to assess the accuracy of physician responses.
Results
Results showed that there was significant variance with regard to knowledge of dose and risk, and that respondents tended to greatly overexaggerate the radiation levels and risk associated with diagnostic imaging. Despite failing to attribute correct values, in many cases, respondents ranked scans correctly. Responses comparing differences amongst the two health services and amongst different levels of medical hierarchy largely overlapped with no clear difference between these factors.
Conclusion
Physicians reported low confidence in their knowledge of radiation awareness and indicated the need for additional education, which would assist them in communicating the risks to patients. Furthermore, such education would assist physicians in tailoring their diagnostic imaging requests so as to minimise radiation levels in patients.
Keywords: Radiation awareness, education, diagnostic imaging
What this study adds:
-
What is known about this subject?
The literature shows that radiation awareness of ED doctors is low and advice to patients about radiation risk is inaccurate.
-
What new information is offered in this study?
At both the metropolitan and regional levels, ED doctors of all hierarchies overestimated the radiation dose received and the risk associated with procedures.
-
What are the implications for research, policy, or practice?
Lack of awareness of radiation dose and long-term risks amongst ED doctors can be addressed via visual reminders (e.g., on routine imaging forms) and supplementary material such as pamphlets.
Background
CT scans, nuclear medicine studies, and general x-rays are all commonly prescribed by physicians to assist in patient diagnosis. Imaging plays a key role not only in rapid diagnosis in the ED, but also in ruling out important and potentially life-threatening differential diagnoses; e.g., differentiating between respiratory and cardiac causes of shortness of breath. Moreover, negative imaging results can be at times necessary in order to proceed with treatment—e.g., the requirement to rule out haemorrhagic stroke before administration of thrombolysis in suspected cerebrovascular infarction (stroke).
Diagnostic imaging modalities that employ ionising radiation to gather information about the patient’s anatomy and physiology pose an associated radiation injury risk, whether deterministic or stochastic.1 The Sievert (Sv) is the radiation dose quantity used to express the radiation damage caused to the body as a weighted average of total absorbed organ dose.2 In everyday life we are all exposed to naturally occurring background radiation, which arises from cosmic and terrestrial radiation, and radionuclides within the body. In Australia, the average background radiation is approximately 2mSv,3 and this low dose of continuous ionising radiation is not seen as a health risk. Unless exposure to radiation is necessary to provide effective diagnosis and treatment, it is important that any additional radiation is kept as low as reasonably achievable (ALARA). Table 1 presents the average radiation dose for each procedure as compared to naturally occurring background radiation and the associated LAR of cancer according to the Board on Radiation Research Effects report.4
Table 1: Typical dose associated with common scans ordered by ED doctors.
| Study | Effective dose (mSv)8 | Equivalent yearly background dose* | Approximate LAR (1 in) >20 year old |
|---|---|---|---|
| General x-ray | |||
| Chest | 0.02 | 0.01 | 700,000 |
| Abdomen | 0.07 | 0.4 | 20,000 |
| Pelvis | 0.07 | 0.4 | 20,000 |
| Limbs | 0.0005 | 0.0003 | 28,000,000 |
| C-Spine | 0.07 | 0.04 | 200,000 |
| CT | |||
| Chest | 8 | 4 | 1,740 |
| Abdomen | 10 | 5 | 1,400 |
| CTPA | 6 | 3 | 2,300 |
| Brain | 2 | 1 | 7,000 |
| C-Spine | 4 | 2 | 3,500 |
| Nuclear medicine | |||
| V/Q scan9 | 1.7 | 0.9 | 8,200 |
* The dose is given as a fraction of yearly background radiation and LAR is calculated.4
The emerging emphasis on evidence-based medicine often necessitates imaging as part of well-accepted guidelines such as the NEXUS criteria5 and the Canadian C-spine rule.6 It is clear that imaging plays a central role in the early management of ED patients and such studies—and correspondingly, radiation dose—can accumulate quite rapidly with time for valid clinical reasons. Clinically, the effects of radiation appear in the long-term as an increase in the LAR of cancer. While it is impractical to withhold imaging from patients particularly in early management of acute conditions, physicians should be aware of the impact of radiation dose involved with imaging, particularly in the case of younger patients and when other alternatives for imaging are available. One example is the detection of pulmonary embolism in young women: while a contrast tomography pulmonary angiogram (CTPA) has higher specificity and sensitivity for acute pulmonary embolism than the alternative ventilation/perfusion (V/Q) scan, the CTPA delivers a much higher dose of radiation to the breasts of young women, which can mean unnecessary longer-term risks associated with radiation exposure.7
Recent studies found that there is a limited knowledge of the radiation dose associated with prescribed imaging modalities.10,11 Similarly, an American study concluded that most patients are not given information about the risks associated with radiation dose from CT scans,12 which could be attributed to the physicians and radiologists’ inadequate understanding of radiation risks associated with common CT scans.13 This pilot study aims to determine the awareness of radiation dose and risks associated with procedures that are ordered by physicians in the ED at a major metropolitan hospital and a regional hospital in Australia, and to assess differences in knowledge between physicians in these two settings, respectively.
Method
Study outcomes
The primary outcome was to determine the baseline level of radiation awareness amongst ED doctors. The secondary outcomes were to assess differences between metropolitan and regional doctors in terms of radiation awareness, whether doctors felt they had enough teaching in radiation dose risks, and whether they would appreciate more education in this area. The primary outcome was continuous while the secondary outcomes were binary.
Study design and cohort selection
A cross-sectional survey was piloted at two major hospitals to obtain a baseline awareness of knowledge amongst ED doctors, which can later be investigated in larger studies. A well-known, tertiary metropolitan health service was selected to represent practitioner radiation awareness in metropolitan areas, and a well-known regional health service was chosen to represent the same in a large regional area. The aim was to determine if there was a difference in awareness between metropolitan and regional doctors. The largest ED at each of the two services was identified.
Exposure variables
The variables controlled in this study were site location (metropolitan or regional) and clinical hierarchy.
Data collection
At the metropolitan site, the authors requested a senior ED clinician to ask ED doctors to complete and return a paper questionnaire. At the regional site, doctors were identified based on records of currently employed ED staff, and were individually approached by the authors and asked to complete the questionnaire. Survey respondents were asked to identify whether they worked at a metropolitan or regional health service, their positional hierarchy within the hospital system (i.e., intern/resident, registrar, and consultant), and their length of employment as a physician (duration of time they have practiced medicine).
Participants were then asked to compare the radiation dose delivered by various types of imaging to the average yearly background radiation dose. Furthermore, they were asked how much that radiation dose would increase an individual’s attributable risk of cancer. The procedures surveyed are listed in Table 1. Clinicians’ responses were compared to the average values found in the literature for each procedure. Participants were also asked to comment on whether they believed current workplace radiation awareness was sufficient and whether they felt confident answering patient queries regarding radiation dose.
Results
There were 42 respondents in total: 16 responses from the metropolitan service and 26 responses from the regional service. Table 2 lists the features of the participant groups (metropolitan and regional). The total respondent hierarchy was 17 interns, eight residents, four admitting officers, six registrars, and seven consultants (Table 3). Some site-specific hierarchies were either not present or could not be recruited.
Table 2: Comparative features of participant groups.
| Metropolitan Centre |
| • Generally more senior doctors (80% of respondents were registrars or consultants) |
| • Consultants hold a Fellowship of the Australian College of Emergency Medicine (FACEM) |
| • Doctors whose primary medical degree is from Australia |
| • Specialist advice from medical physics department for radiation dose optimisation |
| Regional Centre |
| • Generally more junior doctors (74% of respondents were interns) |
| • Consultant doctors are senior doctors with more experience but without a formal FACEM |
| • Doctors whose primary medical degree is from a country other than Australia |
| • No specific monitoring or regulation regarding radiation dose optimisation |
Table 3: Respondents by site and hierarchy.
| n | Parent Organisation | ||
|---|---|---|---|
| Metropolitan | Regional | Total | |
| Consultant | 7 | – | 7 |
| Registrar | 6 | – | 6 |
| Admitting Officer | – | 4 | 4 |
| Resident | 1 | 7 | 8 |
| Intern | 2 | 15 | 17 |
| Total | 16 | 26 | 42 |
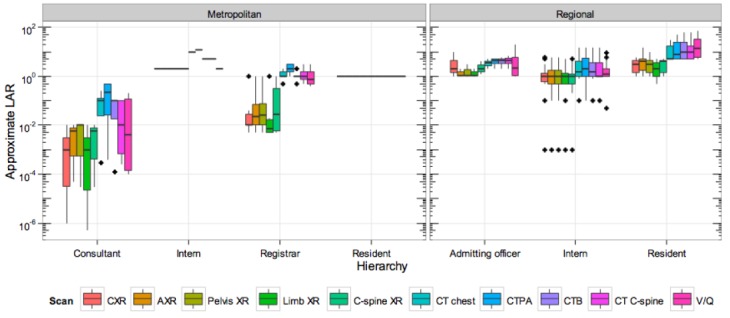
The distributional properties of the pilot survey are graphically analysed via box-plots. Box-plots of risk and dose by hierarchy and geographic location are presented in Figure 1 and 2. These show the large variation within any given cohort and the difference from the values suggested by the literature. The highly skewed nature of the data and heterogeneous variances preclude parametric tests for significant differences across cohorts in both dose and risk. Further, low per-cohort sample size across both geographic and hierarchy factors precludes meaningful non-parametric testing.
Figure 1: Average dose response for doctors by hierarchy and location.
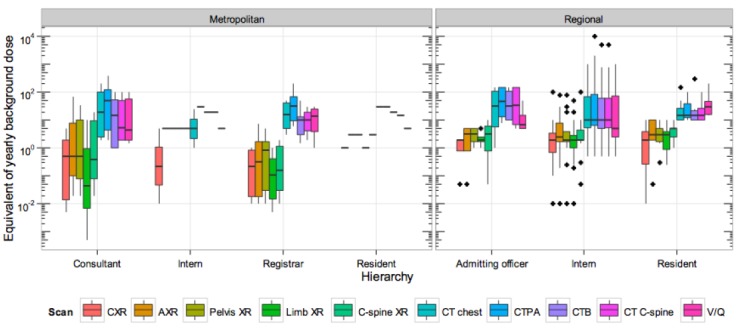
Figure 2: Average risk response for doctors by hierarchy and location.
Discussion
At every hierarchical level, at both the metropolitan and regional hospitals, the radiation dose received from and risk associated with procedures were overestimated (Table 4). Amongst both metropolitan and regional groups, the most overestimated imaging type was the limb x-ray (median response 1,000 times the amount reported in the literature), followed by the chest x-ray (median 150 times that in literature). In fact, these two diagnostic tests expose the patients to the lowest radiation dose. This indicates that while respondents could often correctly rank procedures in terms of risk or dose, they were unable to properly differentiate between the magnitudes of radiation dose received by different diagnostic procedures. In reality, the radiation dose received by CT could be 1,000 times more (or greater) than that of any general x-ray procedure. This was not reflected in the results (Table 4).
Table 4: Median responses by imaging type with comparison to the literature.
| Dose x background | Cancer Risk | |||
|---|---|---|---|---|
| Imaging Type | Median Response | Multiple of literature rate (from Table 1) | Median Response (%) | Multiple of literature rate (from Table 1) |
| General x-ray | ||||
| Chest | 1.50 | 150 | 1.00 | 1,000,000 |
| Abdomen | 2.00 | 5.71 | 1.00 | 20,000 |
| Pelvis | 2.00 | 5.71 | 1.00 | 20,000 |
| Limbs | 1.25 | 1000 | 1.00 | 5,000,000 |
| C-Spine | 2.00 | 57.14 | 1.00 | 200,000 |
| CT | ||||
| Chest | 15.00 | 3.75 | 2.00 | 4,000 |
| CTPA | 20.00 | 4.00 | 2.50 | 3,571 |
| Brain | 12.00 | 12.00 | 2.00 | 20,000 |
| C-Spine | 11.00 | 5.50 | 1.50 | 5,000 |
| Nuclear medicine | ||||
| V/Q scan9 | 9.00 | 6.43 | 1.10 | 5,500 |
Given this level of overestimation of radiation dose for a basic, highly in-demand form of imaging such as the chest x-ray (CXR) amongst emergency doctors, it is possible that medical and surgical teams think similarly. A pertinent question is: is there any means of following up or educating patients regarding their increased risk, particularly those in at-risk groups?
The results of this study indicate that confidence amongst emergency physicians is low with regard to answering patient questions about radiation dosage in imaging. Most doctors surveyed—73 per cent metropolitan, 69 per cent regional—indicated that they would not be confident discussing risks with their patients. Some noted that although they may not be able to quantify the risk to the patient they would feel comfortable discussing the diagnostic benefits versus any associated radiation dose. However, given the magnitude of overestimation of the responses relating to risk from the participants in this study, it is possible that the risk of diagnostic imaging procedures may be exaggerated to the patient.
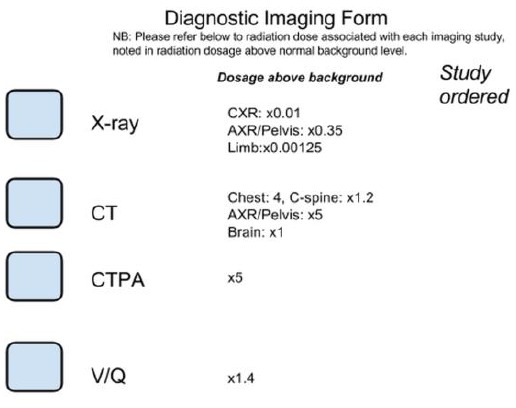
When asked if the radiation awareness in the workplace is sufficient, most participants responded “No” (86 per cent metropolitan, 92 per cent regional). However, the authors suggest that this issue would likely not be best treated with extra training, but by providing ED physicians with resources to refer to when discussing radiation risk with patients. Given the time pressures in the ED, the authors suggest that, for physicians, information on risk—in the form of radiation dosage above background dosage—be included on standard imaging ordering forms (Figure 3). Likewise, this information could be printed on a patient information pamphlet and kept in the ED to be distributed to patients, or explained to the patient by the physician if time and circumstances permit.
Figure 3: Example method of incorporating radiation dosage onto diagnostic imaging forms.
Lastly, good record keeping that clearly states the amount of radiation the patient was subjected to is recommended.14 This is particularly useful when the patient must undergo repeat studies in a short time period. A radiation management plan for patients is recommended by the authors to ensure that the patient's radiation safety risk is as low as reasonably achievable. This should be championed by the hospital radiation safety officer.
Limitations
The ability to compare groups using statistical tests was hampered by low per-cohort sample size along with large variances in responses. Given the distributional properties of the data (approximately log-normal) the authors log-transformed the responses for chest x-ray dose and conducted a sample size estimation for an ANOVA test across hierarchy groups using the G*Power programme. Assuming homogenous variances, for a small-medium effect size (f=0.20) as determined by the data, and power of 0.8, the authors calculate a total sample size of 280 (56 per cohort) may be needed in future studies to detect a significant effect.
While the largest hospital of both health services was surveyed, the generalisability of the results could be affected by having only two recruitment sites along with limitations on the equivalence and availability of different levels of clinical hierarchy.
Interpersonal contact and the researchers being present at the regional centre proved to be a more successful recruitment method than the one employed at the metropolitan centre. Further improvements of this study could include conducting the study over multiple sites across multiple organisations, increased participant numbers sufficient for statistical comparisons, and a sampling design prioritising baseline respondent characteristics with lower occurrence rates.
Conclusion
The results from this study indicate that emergency doctors’ awareness of radiation dose and the risk associated with diagnostic imaging is low. Furthermore, doctors tended to overestimate the risk. However, statistical confirmation of these observations is contingent on testing with a larger sample size. The study also suggests that ED doctors had a low level of confidence regarding their radiation knowledge and that further education would be received favourably. The authors suggest that including a clinically relevant and easily relatable example of dose estimate on imaging request forms is a non-invasive and successful way to increase physician knowledge.
ACKNOWLEDGEMENTS
None
Footnotes
PEER REVIEW
Not commissioned. Externally peer reviewed.
CONFLICTS OF INTEREST
The authors declare that they have no competing interests.
FUNDING
Not applicable
ETHICS COMMITTEE APPROVAL
HREC Approval number is LNR/14/Austin/481
Please cite this paper as: Badawy MK, Sayakkarage D, Ozmen M. Awareness of radiation dose associated with common diagnostic procedures in emergency departments: A pilot study. AMJ 2015;8(11): 338-344. http//dx.doi.org/10.4066/AMJ.2015.2452
References
- 1.Mettler FA, Upton AC. Medical Effects of Ionizing Radiation. Pennsylvania. Saunders Elsevier. 2008:564 p. [Google Scholar]
- 2.International Commission on Radiological Protection. The 2007 Recommendations of the International Commission on Radiological Protection. ICRP Publication 103. Ann ICRP. 2007;37(2-4):2. doi: 10.1016/j.icrp.2007.10.003. [DOI] [PubMed] [Google Scholar]
- 3.Webb DV, Solomon SB, Thomson JEM. Background radiation levels and medical exposure levels in Australia. Radiat Protection Aust. 1999;16:7–14. [Google Scholar]
- 4.National Research Council: Committee to Assess Health Risks from Exposure to Low Levels of Ionizing Radiation. Health Risks from Exposure to Low Levels of Ionizing Radiation: BEIR VII-Phase 2: Washington, DC; 2006. [PubMed] [Google Scholar]
- 5.Hoffman JR, Wolfson AB, Todd K. et al. Selective cervical spine radiography in blunt trauma: methodology of the National Emergency X-Radiography Utilization Study (NEXUS) Ann Emerg Med. 1998 Oct;32(4):461–9. doi: 10.1016/s0196-0644(98)70176-3. [DOI] [PubMed] [Google Scholar]
- 6.Stiell IG, Wells GA, Vandemheen KL. et al. The Canadian C-spine rule for radiography in alert and stable trauma patients. JAMA. 2001;286(15):1841–8. doi: 10.1001/jama.286.15.1841. [DOI] [PubMed] [Google Scholar]
- 7.Freeman LM. Don't bury the V/Q scan: it's as good as multidetector CT angiograms with a lot less radiation exposure. J Nucl Med. 2008 Jan;49(1):5–8. doi: 10.2967/jnumed.107.048066. Epub 2007 Dec 12. [DOI] [PubMed] [Google Scholar]
- 8.Hart D, Wall B, Britain G. Radiation exposure of the UK population from medical and dental X-ray examinations: NRPB Chilton. 2002 [Google Scholar]
- 9.Valentin J. Radiation dose to patients from radiopharmaceuticals: (Addendum 2 to ICRP Publication 53) ICRP Publication 80 Approved by the Commission in September 1997. Annals of the ICRP. 1998;28(3):1. doi: 10.1016/s0146-6453(99)00006-8. [DOI] [PubMed] [Google Scholar]
- 10.Keijzers GB, Britton CJ. Doctors' knowledge of patient radiation exposure from diagnostic imaging requested in the emergency department. Med J Aust. 2010 Oct 18;193(8):450–3. doi: 10.5694/j.1326-5377.2010.tb03998.x. [DOI] [PubMed] [Google Scholar]
- 11.Gervais N, Veronique G, Jacques J. et al. How aware are Belgian permanent and resident emergency physicians of common medical costs and radiation doses? Eur J Emerg Med. 2011 Dec;18(6):344–50. doi: 10.1097/MEJ.0b013e3283466eea. doi: 10.1097/MEJ.0b013e3283466eea. [DOI] [PubMed] [Google Scholar]
- 12.Lee CI, Haims AH, Monico EP. et al. Diagnostic CT Scans: Assessment of Patient, Physician, and Radiologist Awareness of Radiation Dose and Possible Risks 1. Radiology. 2004;231(2):393–8. doi: 10.1148/radiol.2312030767. [DOI] [PubMed] [Google Scholar]
- 13.Thomas KE, Parnell-Parmley JE, Haidar S. et al. Assessment of radiation dose awareness among pediatricians. Pediatr Radiol. 2006 Aug;36(8):823–32. doi: 10.1007/s00247-006-0170-x. Epub 2006 May 13. [DOI] [PubMed] [Google Scholar]
- 14.Street M, Brady Z, Van Every B. et al. Radiation exposure and the justification of computed tomography scanning in an Australian hospital emergency department. Intern Med J. 2009 Nov;39(11):713–9. doi: 10.1111/j.1445-5994.2009.01956.x. doi: 10.1111/j.1445-5994.2009.01956.x. Epub 2009 Mar 23. [DOI] [PubMed] [Google Scholar]


