Abstract
Episodic (less than weekly) drug use and binge drinking increase HIV-related sexual risk behaviors among men who have sex with men (MSM), yet no evidence-based interventions exist for these men. We describe an adaptation process of the Personalized Cognitive Counseling (PCC) intervention for utilization with high-risk, HIV-negative episodic, substance-using MSM. Participants (N=59) were racially diverse, and reported unprotected anal intercourse and concurrent binge drinking (85 %), use of poppers (36 %), methamphetamine (20 %) and cocaine (12 %). Semi-structured interviews with 20 episodic, substance-using MSM elicited sexual narratives for engaging in unprotected anal intercourse while using alcohol or drugs. Emergent qualitative themes were translated into self-justifications and included in a revised PCC self-justification elicitation instrument (SJEI). The adapted SJEI was pretested with 19 episodic, substance-using MSM, and the final adapted PCC was pilot-tested for acceptability and feasibility with 20 episodic, substance-using MSM. This process can be used as a roadmap for adapting PCC for other high-risk populations of MSM.
Keywords: HIV prevention, Evidence-based intervention, Adaptation, Episodic substance use, MSM
A well-recognized tension exists between the need to replicate the success of evidence-based behavioral interventions by maintaining fidelity to core elements, and the need to adapt aspects of interventions to make them socioculturally appropriate and relevant to new populations and settings (Galbraith et al. 2011). A careful and deliberate adaptation process can balance these demands to ensure that an adapted evidence-based behavioral intervention will remain efficacious under new conditions (McKleroy et al. 2006; Solomon et al. 2006; Wingood and DiClemente 2008). The purpose of this paper is to describe a process that HIV program developers, providers, and researchers can use to adapt and expand the reach of evidence-based behavioral interventions to different populations and settings.
This study was supported by the Centers for Disease Control and Prevention (CDC) Adopting and Demonstrating the Adaptation of Prevention Techniques (ADAPT-2) to conduct formative research to adapt and evaluate the efficacy of an existing evidence-based behavioral intervention in a randomized controlled trial (CDC 2007). In this paper, we present the findings of formative research to adapt the Personalized Cognitive Counseling (PCC) intervention, an evidence-based behavioral intervention originally developed for and rigorously evaluated with repeat-testing, HIV-negative men who have sex with men (Dilley et al. 2002; 2007), for episodic substance-using men who have sex with men (MSM) at high-risk of HIV acquisition.
Episodic Substance use Associated with HIV Risk Among MSM
MSM remain the population most disproportionately affected by the HIV epidemic in the United States. In 2010, MSM accounted for an estimated 77 % of all diagnosed HIV infections among adult and adolescent males (CDC 2012), despite representing only 4 % of the US male population (Purcell et al. 2012). The estimated number of HIV diagnoses among MSM increased 10 % from 2007 to 2010. Among MSM diagnosed with a new HIV infection in 2010, 37 % were black/African American, 35.6 % white, and 23 % Latino (CDC 2012). The National HIV/AIDS Strategy released by the White House’s Office of National AIDS Policy (2010) prioritized MSM for targeting HIV prevention activities and reducing health disparities.
Non-injection substance use and alcohol consumption are well-documented drivers of the HIV epidemic among MSM (Santos et al. 2011). Between 2003 and 2005, a national sample of over 10,000 MSM reported a 42 % previous-year prevalence for any non-injection substance use, and the most commonly used drugs included marijuana (77 %), cocaine (37 %), ecstasy (29 %), poppers (28 %), and stimulants (27 %) (Sanchez et al. 2006). While polysubstance use is common among many MSM (Carey et al. 2009; Santos et al. 2011), studies found that the majority of MSM who use drugs use them episodically (less than weekly) and most do not inject (Sanchez et al. 2006). Substances used have various effects ranging from increasing libido, sexual confidence, feelings of social connection and invulnerability, expectancies of cognitive escape and sexual satisfaction, to impairing judgment. These effects are implicated as psychological factors leading MSM to take increased sexual risk while under the influence of substances (Diaz et al. 2005; Drumright et al. 2006; McKirnan et al. 2001; Semple et al. 2002). Across populations of MSM, use of methamphetamine, poppers, crack or powder cocaine, and heavy alcohol use are most consistently and often independently associated with a variety of high-risk behaviors, including unprotected anal intercourse (Halkitis et al. 2009; Heath et al. 2012; Hirshfield et al. 2004; Mansergh et al. 2006; Remien et al. 1995), HIV seroconversion (Carey et al. 2009; Plankey et al. 2007) and other sexually transmitted infections (Colfax et al. 2004; Drumright et al. 2006; Hirshfield et al. 2004).
Reducing or modifying behaviors in the setting of substance use may lead to clinically significant reductions in sexual risk (Colfax et al. 2004). Studies found that MSM who enter substance use treatment decrease both their substance use and sexual risk (Paul et al. 1993; 1994; Remien et al. 1995; Stall et al. 1999). However, many MSM are not accessing treatment for their substance use (Sanchez et al. 2006). The few behavioral interventions that demonstrated sexual risk reduction among substance users targeted treatment-seeking individuals (Shoptaw et al. 2005), and are often resource and time intensive (Mansergh et al. 2010). These interventions may not be appropriate for the majority of MSM, whose substance use is often infrequent and non-injection (Carey et al. 2009; Morgenstern et al. 2009). Given the high rate of episodic substance use among MSM, its link with sexual risk in this population, and the paucity of proven interventions for episodic, substance-using MSM, we sought to adapt an evidence-based behavioral intervention appropriate for this population.
Personalized Cognitive Counseling Intervention
As a brief single-session intervention conducted in the context of an HIV testing and counseling session, PCC was deemed appropriate for counseling episodic, substance-using MSM. PCC can be integrated into existing HIV testing services, and demonstrated sustained effects in reducing sexual risk behaviors among MSM in two randomized trials (Dilley et al. 2002; 2007). Moreover, PCC can be delivered by either trained counselors or para-professionals, and acceptability among high-risk HIV-negative MSM is high (Dilley et al. 2011).
PCC is predicated on the hypothesis that many MSM who take risks do so despite knowing the potential for HIV infection. The intervention is guided by two social cognitive theories: Bandura’s theory of self-regulation (Bandura 1977a, b) and stages of behavior change (DiClemente and Prochaska 1985; DiClemente et al. 1985). A central construct in both theories is the crucial role of self-observation as a first and necessary step in the self-regulatory process (Bandura 1977a; 1977b). A core characteristic involves the individual considering possible actions with respect to changing behavior perceived as detrimental to personal goals and health (DiClemente and Prochaska 1985; DiClemente et al. 1985). Gold expanded on the self-observation concept to focus specifically on self-justifications regarding high-risk sexual behaviors among MSM (Gold and Skinner 1992). Gold and colleagues proposed that “on-line” cognitions (e.g., those that are present leading up to and during sexual encounters when the individual is in the “heat of the moment”) are different from “off-line” cognitions (e.g., those that exist at any other time in the “cold light of day”) (Gold and Aucote 2003; Gold and Rosenthal 1995, 1998; Gold and Skinner 1992; Gold et al. 1994). These self-justifications are beliefs, thoughts, attitudes, and values that relate to the behavior and the risk involved. The individual employs one or more self-justification to allow the desired, but known to be risky, behavior to occur. To the extent that this hypothesis is correct, it follows that if one could appropriately modify or attenuate self-justifications, risky behavior could be modified or prevented. In a series of studies, Gold and colleagues investigated these ideas and identified self-justifications associated with unprotected anal sex among MSM (Gold and Rosenthal 1995; Gold and Skinner 1992; Gold et al. 1994). Dilley and colleagues took this approach one step further and adapted the self-justification idea for use in a single-session, face-to-face, cognitive counseling intervention for HIV-negative, repeat-testing MSM (Dilley et al. 2002). Dilley’s PCC intervention elicits participant’s “heat of the moment” self-justifications in the company of an empathic, trained counselor. The counselor helps the participant relive the experience, identify self-justifications used at the time of the risky sexual encounter, and re-examine them in “the cold light of day.”
Adaptation of PCC for Episodic, Substance-using MSM: Project ECHO
We conducted formative research to adapt PCC for ethnically diverse, HIV-negative episodic, substance-using MSM. We followed the CDC’s guidance for adapting evidence-based behavioral interventions to address the target population’s needs while maintaining fidelity to the intervention core elements and internal logic hypothesized to be responsible for behavior change (McKleroy et al. 2006). The critical component of adapting PCC involved modifying the self-justification elicitation instrument (SJEI) used in the original research. The SJEI elicits thoughts, attitudes and beliefs held by clients before, during and after high-risk unprotected anal intercourse. The SJEI is meant to serve as a memory jog for PCC participants, create a mental and emotional recall of an encounter of unprotected sex, and promote reflection about self-justifications, thoughts, and feelings that resonate during unprotected sex. Additionally, the SJEI provides PCC counselors with a starting point for the session by directing them toward topics relevant to participants’ sexual risk taking behavior requiring in-depth investigation. As the Dilley et al. studies (Dilley et al. 2002; 2007) included less than 20 % of MSM reporting any substance use, the original SJEI included only three self-justification statements addressing substance use during high-risk sexual situations.
Methods
Formative research activities were conducted in San Francisco, CA between March 2009 and January 2010. The research protocol was reviewed and approved by the Committee on Human Research, the institutional review board for the University of California, San Francisco, and the CDC Institutional Review Board. The study is described on clinicaltrials.gov (NCT01279044).
Recruitment and Enrollment
The study targeted episodic, substance-using MSM who engage in sexual activity that increases their risk of HIV acquisition, specifically high-risk unprotected anal intercourse. Recruitment involved street outreach at community venues including outside of bars, clubs, grocery stores, gyms, and other venues frequented by MSM. To recruit a racially and ethnically diverse sample of episodic, substance-using MSM, recruitment also occurred at community-based organizations serving African American, Latino, and Asian and Pacific Islander MSM. For venue-based recruitment, study recruiters informed potential participants of the study, emphasized that participation is voluntary, and provided flyers describing the study. The same recruitment strategies were used for all formative research activities.
Interested persons were screened in the field for eligibility based on a brief set of inclusion criteria (i.e., identified as male, aged 18 years or older, self-reported HIV-negative, current San Francisco Bay resident, and reported unprotected anal intercourse with another man while under the influence of alcohol and/or drugs during past 3 months). If deemed initially or likely to be eligible, potential participants were screened by telephone using more detailed eligibility criteria: (1) identified as male; (2) aged 18 years or older; (3) self-reported serostatus as HIV-negative or unknown; (4) reported unprotected anal intercourse with another man while under the influence of at least one or any combination of the following substances: methamphetamine, poppers, crack or powder cocaine, or binge alcohol consumption (i.e., five or more drinks) within 2 h before or during sex (during the past 3 months); (5) reported unprotected anal intercourse with at least one HIV-positive or unknown serostatus partner or more than one HIV-negative partner (during the past 3 months); (6) were willing to participate in an intervention addressing episodic substance use and sexual risk behavior; (7) were not enrolled in substance use treatment, a self-help program or an HIV prevention study; (8) were planning to remain in San Francisco Bay area for duration of study activities; (9) were willing to provide full informed consent; and (10) were able to speak, read and understand English.
Participants were considered ineligible if they reported weekly or greater than weekly drug use (of targeted substances including methamphetamine, poppers, crack or powder cocaine) or greater than 3 alcoholic drinks consumed daily or more than weekly binge drinking during the past 3 months. The definition for “episodic” substance use was derived from prior research studies of MSM conducted in San Francisco (Colfax et al. 2004). Participants who reported use of “club drugs” such as ecstasy, ketamine, and GHB were not excluded from the study. All ineligible participants were provided information about community referrals for more intensive substance use treatment. Of the 123 MSM screened, 59 (48 %) were determined eligible and consented to participate. Main reasons for ineligibility included no reported substance use with unprotected anal intercourse (31.9 %), no reported unprotected anal intercourse (18.5 %), and reporting only one unprotected anal intercourse episode with an HIV-negative partner (10.9 %) during the past 3 months. Ineligible men did not differ significantly from eligible men in terms of age, race/ethnicity, proportion identifying as gay or bisexual, HIV testing history, or participation in substance use treatment or self-help programs (all p values>0.05).
Procedures
The adaptation of PCC involved a three-phase process: (1) conducting in-depth interviews with 20 episodic, substance-using MSM to identify and abstract relevant self-justifications for unprotected anal intercourse and concurrent substance use, (2) pretesting the adapted SJEI with 19 episodic, substance-using MSM to determine relevance and representativeness of self-justification items, and (3) pilot-testing the complete PCC intervention session with 20 episodic, substance-using MSM to determine feasibility and acceptability. In each study phase, participants were convenience samples of eligible men, and not randomly assigned to study phases, consistent with the formative research study design. However, participation was limited to one formative study phase per participant to ensure greater diversity in the sample and to reduce exposure bias.
Phase 1: In-Depth Interviews
The aim of the in-depth, semi-structured interviews (Carey and Gelaude 2008) was to elicit a nuanced understanding of the personal and social contexts in which substance use and high-risk sexual behavior occur (e.g., physical setting, partner type and emotional state); and the thoughts, attitudes and beliefs used to self-justify substance use and high-risk sexual behavior. The structure of the interviews permitted probing for explanations of actions and feelings (Rubin 1995), and allowed participants to describe a personal narrative of their lived experiences (Seidman 1991). Interviews began with broader questions regarding their health before proceeding to more intimate inquiries (Glaser and Strauss 1967). The interviews were audiotaped and transcribed for qualitative coding (Skinta et al. 2012).
A qualitative interview guide was developed with input from members of the target population, persons familiar with episodic, substance-using MSM, and researchers with experience working with substance-using MSM. The guide was composed of standard questions and follow-up probes pertaining to drug and alcohol use, sexual encounters, and sexual relationships in general. The guide also asked participants to describe the details of their last (or most memorable) unprotected sex act with another man while using drugs and/or alcohol (i.e., the sexual narrative). Participants were then queried about their attraction and relationship to the man mentioned in the narrative; the time, place and context of the encounter; a detailed description of the encounter; the role of drugs and alcohol; whether HIV serostatus was discussed; and self-justifications used for participating in high-risk behaviors.
Self-Justification Data Abstraction
The qualitative research team conducted a focused, task-driven qualitative analysis of the interview data consistent with content analysis techniques (Miles and Huberman 1994; Strauss and Corbin 1990). Structural coding was applied to broad topic areas for more in-depth team-based review (MacQueen et al. 1998; Nichter et al. 2002). Two analysts were assigned to analyze each participant’s transcript and abstract statements of self-justifications for engaging in risky sexual behavior. Self-justifications included any statement in which the participant referred to what he was thinking or feeling before, during or after an unprotected sexual encounter while under the influence of drugs and/or alcohol. Self-justifications included spontaneous statements that reflected thoughts and feelings about the decision to have unprotected anal intercourse, and described whether or not he was under the influence of the targeted substances when making those decisions. Once abstraction was complete, analysts met to reach consensus on the abstracted statements. If two analysts disagreed about the interpretation of data for an abstracted statement, further discussion would ensue. If consensus could not be reached between the two analysts, then the data would not be retained. A document reflecting the retained statements was generated for each participant. The lead analyst (K. Knight) reviewed all self-justifications and created an aggregate document of self-justification statements while conducting quality assurance to ensure that selected statements did not over-represent a small number of participants’ interview data, but were evenly abstracted from the entire sample.
Self-Justification Coding
Each analyst individually read and coded self-justification quotes by a topic theme that seemed to best reflect the stated content. This form of structural coding is an interpretative process that summarizes the meaning of participants’ statements (MacQueen et al. 1998; 2008). Analysts offered summary statements and/or used the participant’s own language with the goal of identifying themes about which SJEI items can be modified or developed. For example:
Self-justification quote: I’ve just decided [not to use cocaine again] because that’ s when my memories, that’ s when my inhibitions, you know, they go away and that’ s when I practice in maybe unsafe sexual behavior.
Content code: Cocaine erases memories and inhibitions, and leads to unsafe sex
Self-justification quote: I fear that … I do have an addictive personality anyway, so I fear that I may drink sometimes to calm down; lower the anxiety levels of dating someone who’s HIV-positive, and when I’m gonna have sex with him. It kinda makes it easier for me.
Content code: Alcohol lowers anxiety of having sex with HIV + partner
Selection of Self-Justification Themes and Item Development
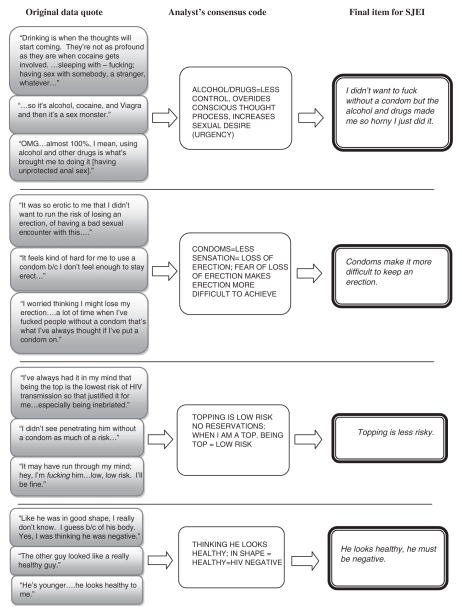
The lead analyst compiled a document which included all the team members’ codes. The analysts then met to select the content codes that most accurately reflected the range of statements under each topic area. Next, self-justifications generated by episodic, substance-using MSM were compared to SJEI items from the original PCC. The analysts decided which of the original PCC SJEI items should be retained for testing with participants, and identified content of new items for the adapted SJEI. Criteria for the creation of new items included linkage of alcohol and/or drug use to unprotected anal intercourse, frequency of theme occurrence across participants, and topics that would resonate with a wide range of MSM (e.g., condom use and calculating risk). Figure 1 illustrates the process for identifying themes from the original interview data, and the creation of SJEI items.
Fig. 1.
Process for translating participant responses into Self-Justification Elicitation Instrument (SJEI) items
Phase 2: Pretesting the Adapted SJEI
The adapted SJEI included 48 questions (17 items retained from the original PCC SJEI and 31 newly developed items) and mirrored the original PCC SJEI in format. Participants were asked to endorse each statement using a Likert scale ranging from 1 (“Very true” or “I had this thought strongly (in the forefront of my mind)”) to 4 (“Not true at all” or “I didn’t have this thought at all”). The response “I can’t remember” or “I can’t remember at all whether I had this thought or not” was available and scored as 0. Frequencies of responses were calculated and ranked.
During 1-h interviews, each participant reviewed the instrument to identify items that were confusing or unclear, and items that elicit self-justifications for concurrent unprotected anal intercourse and substance use. The interviewer took detailed notes during and after each pretest interview, and the sessions were tape-recorded. During this phase, feedback from respondents was used to revise or omit items found to be confusing, irrelevant, or inappropriate for the final SJEI. The team examined the sequence of items and flow of the instrument to ensure items were distributed in such a way as to maximize elicitation of self-justifications.
Phase 3: Pilot-Testing the Adapted PCC Intervention
The final phase involved pilot-testing the PCC intervention session in its entirety. During the 30- to 50-min sessions, the following activities occurred: (1) the counselor asked the participant to recall a recent memorable encounter of unprotected anal intercourse with another man of unknown or serodiscordant HIV status; (2) the participant completed the revised SJEI in relation to the risky sexual encounter; (3) the participant was encouraged by the counselor to identify and express his thoughts, feelings or attitudes that may have led to the high-risk sexual encounter; (4) the participant and counselor examined the encounter to identify self-justifications that led to risky behavior; and (5) the participant agreed to strategies to avoid similar high-risk situations in the future. At the conclusion of the PCC session, participants were also asked if the refined SJEI accurately captured typical self-justifications commonly used by episodic, substance-using MSM to justify concurrent unprotected anal intercourse and substance use.
Results
A total of 59 episodic, substance-using MSM were enrolled into the three formative research phases (see Table 1). Overall, 37 % of participants were over the age of 35 years, and 53 % were non-white (including blacks, Hispanics/Latinos, Asian Pacific Islanders, Native Americans, and mixed race/other groups). A majority (85 %) reported binge drinking concurrent with unprotected anal intercourse during the past 3 months. The percentages of men reporting unprotected anal intercourse with concurrent substance use included 20 % using methamphetamine, 36 % poppers, and 12 % powder or crack cocaine.
Table 1.
Characteristics of HIV-negative episodic SUMSM participating in formative research, Project ECHO, San Francisco, CA, 2009–2010
| Characteristic | Phase 1: in-depth interviews n (%) | Phase 2: pretest n (%) | Phase 3: pilot test n (%) | All groups n (%) |
|---|---|---|---|---|
| Sample size | 20 | 19 | 20 | 59 |
| Age group | ||||
| 18–24 | 3 (15) | 5 (26) | 4 (20) | 12 (20) |
| 25–34 | 7 (35) | 8 (42) | 10 (50) | 25 (42) |
| 35–44 | 7 (35) | 1 (5) | 5 (25) | 13 (22) |
| ≥45 | 3 (15) | 5 (26) | 1 (5) | 9 (15) |
| Race/ethnicity | ||||
| Non-whitea | 13 (65) | 8 (42) | 10 (50) | 31 (53) |
| White | 7 (35) | 11 (58) | 10 (50) | 28 (47) |
| Reported UAI with concurrent substance useb | ||||
| Methamphetamine | 6 (30) | 4 (21) | 2 (10) | 12 (20) |
| Poppers | 5 (25) | 7 (37) | 9 (45) | 21 (36) |
| Cocaine | 2 (10) | 2 (11) | 3 (15) | 7 (12) |
| Binge drinking | 17 (85) | 15 (79) | 18 (90) | 50 (85) |
Including black (n=3; 5 %), Hispanic/Latino (n=18; 31 %), Asian Pacific Islander (n=6; 10 %), Native American (n=1; 2 %) and mixed race/other (n=3; 5 %) for all groups
Categories are not mutually exclusive
Phase 1: Results of In-Depth Interviews
Nine themes emerged as a result of the qualitative analysis of participants’ self-justifications of their last (or most memorable) concurrent unprotected anal intercourse with another man while using drugs and/or alcohol (see Table 2). Emergent themes included: (1) substance use as facilitator of risk, (2) transmission risk calculus, (3) assumptions regarding partner’s HIV status, (4) cognitive escape, (5) sensation seeking/spontaneity, (6) condom-related issues, (7) opportunities for sex, (8) expectations or obligations for unprotected sex, and (9) feelings of invincibility. Over half of the items included in the pretested SJEI addressed these themes. We present examples of participants’ responses according to the top four emergent self-justification themes.
Table 2.
Emergent themes and self-justifications derived from in-depth interviews with HIV-negative, episodic SUMSM, Project ECHO, San Francisco, CA, 2009–2010 (N=20)
| Theme (number of items included in SJEI pretest) |
|---|
| Theme 1: Substance use as facilitator of risk (8) |
| Substances lower inhibitions (and allows for experimentation) |
| Substances make it physically easier to have anal sex |
| Not thinking—too high or drunk |
| Drugs make sex last longer, better control ejaculation, and heightens sensation |
| Substance use got out of control |
| Theme 2: Transmission risk calculus (7) |
| Topping is low risk, undetectable viral load, no ejaculation involved, dipping only, partner is on medication |
| Conflicting thoughts (know it is a risk but it feels so good) |
| Rare occurrence (just this once) |
| HIV is a manageable disease |
| Theme 3: Assumptions regarding partner’s HIV status (6) |
| Assumed partner is HIV-negative (based on looks or partner would have told them) |
| Trust partner due to social conversations or social network |
| Theme 4: Cognitive Escape (4) |
| To escape, let go of control |
| Didn’t want to think about HIV or risk |
| Abdicate control and not wanting to take responsibility |
| Theme 5: Sensation seeking/spontaneity (4) |
| Just happened—didn’t plan on it |
| Human nature/instinct (to not use condoms) |
| Physical release/animalistic instinct—just wanting to “get off” |
| Theme 6: Condom-related issues (4) |
| Condom failure—broke, came off |
| Decreased performance or sensation due to condoms |
| Decreases spontaneity |
| Intimacy—a desire to feel closer |
| Theme 7: Opportunities for sex (4) |
| Ego boost—young, hot, attractive partner |
| The opportunity presented itself |
| Theme 8: Expectation or obligation (3) |
| Reciprocity |
| I closed the deal online so I must follow through |
| We had unprotected anal sex before so why stop now? |
| Theme 9: Invincibility (2) |
| Still negative after risky behavior |
| Sense of invincibility |
The most common theme involved self-justifications regarding substance use as a facilitator of risky sexual behaviors. One participant commented that being under the influence of alcohol lowered his inhibitions which “… totally affects your judgment … and you end up doing unprotected sex.” Other self-justifications involved substances making it physically easier to have sex, not requiring too much thinking while high or drunk, and allowing them to lose control. As stated by a participant:
Poppers I guess it does loosen me up and makes me feel real good, and that head rush kind of feels nice I guess. In terms of Ecstasy, I just remember just feeling when I did the MDMA … it just kind of felt euphoric where it’s just like you’re going with the flow; like there’s nothing you have to worry about and like you would massage me and that would just feel really good.
The second theme involved self-justifications of a “transmission risk calculus” involving knowledge of HIV risk associated with specific behaviors, and willingness to make sexual decisions based on levels of risk. Specific self-justifications included engaging in unprotected insertive anal sex as a lower risk behavior, asking about viral load levels of HIV-infected partners, and not ejaculating in the anus. As stated by one participant:
Well I can just tell you that you know I have practiced that behavior [unprotected anal sex] when I’m a top. I’ve always had it in my mind that as the lowest risk of transmission for HIV being the top you know. And so that justified it for me, especially being inebriated. I mean I didn’t have any reservations about doing it, honestly at that time I didn’t.
Participants also reported having conflicting thoughts between knowledge of insertive unprotected anal intercourse as a risk factor for HIV and their desire to engage in the behavior anyway. For example, a participant commented “I didn’t see myself when I penetrated him without a condom … as much of a risk, because it really technically is not. It’s still a risk, but it’s not as high as being on the receptive end.” Other self-justifications included viewing the episode of unprotected anal intercourse and substance use as a rare occurrence, and conceptualizing HIV as a manageable chronic disease.
The third theme involved self-justifications related to assumptions about sex partner’s HIV status. Participants reported assuming their partner was HIV-negative based on looking healthy, being young, or perceiving non-disclosure of HIV as an indicator of the partner not being infected. For example, a participant stated:
I kept thinking: ‘He’s 21 years old. Yeah, there are young people contracting HIV left and right these days, younger and younger. But maybe he is telling me the truth.’ So I’m sitting here convincing myself that it’s okay, telling myself it’s okay and he’s younger, he looks healthy to me. Just all these stupid things.
A similar sentiment was echoed by another participant:
I’m not sure, because I was drunk, but maybe I think I may have asked him [about his HIV status]. And the thing is he is … one of the smartest people I’ve met his age…. He would have said something about [HIV] to me if he had you know doubts about me.
Participants also reported they trusted their partners due to social conventions within their sexual networks. For example, a participant stated:
… there are certain communities that I run with that are really good at holding each other accountable, and are really honest with each other and really care about each other’s well-being…. [We] wouldn’t introduce something into the group who was not already kind of … screened by the group.
The fourth theme involved self-justifications related to cognitive escape. Participants justified their risky sexual behavior due to a desire to escape or let go of their self-control. As stated by one participant: “… there’s an element of escape like of wanting to just kind of say ‘fuck it’ to everything and just like kind of get away.” Participants also justified their risky sex behavior by abdicating responsibility to the sex partner:
There’s a notion of … letting go of the responsibility or letting go by throwing caution to the wind. I guess it’s the adrenalin rush from it you know that ‘oh I shouldn’t be doing this’ or ‘someone’s making me do this’ … kind of twist in your mind that somehow give the responsibility to the other person rather than taking it for myself.
Participants sometimes acknowledged they should take better control of these situations: “I think it’s a responsibility thing … I’ll let other people get me fucked up rather than actually choosing to do it myself, even though in a roundabout way it’s exactly what I was doing put [me] in that situation.”
Phase 2: Results of SJEI Pretest
Next, 19 episodic, substance-using MSM participated in the pretesting of the adapted SJEI. Table 3 presents the wording of the four most frequently endorsed SJEI items in each of the four most frequently endorsed self-justification themes. These items addressed self-justifications involving concomitant substance use as facilitator of risky sex (percent endorsed ranged from 73.7 to 89.5 %), transmission risk calculus (range 57.9 to 84.2 %), assumptions regarding partner (range 57.9 to 63.2 %), and cognitive escape (range 42.1 to 79.0 %). A large percentage of participants endorsed several SJEI items as “very true.”
Table 3.
Sample SJEI items from the four most frequently endorsed self-justification themes among HIV-negative, episodic SUMSM, Project ECHO, San Francisco, CA, 2009–2010 (N=19)
| SJ theme and SJEI items | Percentage endorsing Slightly, moderately, or very true |
Percentage endorsing Very true |
|---|---|---|
| Theme 1: Substance use as facilitator of risk | ||
| Alcohol and drugs make it easier to have sex (or different kinds of sex) | 89.5 | 47.4 |
| I didn’t want to fuck without a condom but the alcohol/drugs made me so horny I just did it | 79.0 | 21.1 |
| Sex is always better when I am drunk or high | 73.7 | 5.3 |
| I was bored and the opportunity to drink/use drugs and have sex came up | 73.7 | 21.1 |
| Theme 2: Transmission risk calculus | ||
| Part of me is saying this is risky, but another part is telling me to go for it | 84.2 | 36.8 |
| I know this is risky, but that’s part of what makes it so hot | 84.2 | 21.1 |
| Topping isn’t that risky | 63.2 | 21.1 |
| It’ll be alright to fuck without a condom as long as we don’t cum in the ass | 57.9 | 36.8 |
| Theme 3: Assumptions regarding partner’s HIV status | ||
| He would have told me if he were positive | 63.2 | 15.8 |
| I know enough about this guy, I figure I can trust him | 57.9 | 26.3 |
| He said he was negative, and I have been tested. So it must be safe | 57.9 | 10.5 |
| This guy looks healthy, he is probably negative | 57.9 | 5.3 |
| Theme 4: Cognitive escape | ||
| I don’t want to think about risk. I just want to be drunk/high and have hot sex | 79.0 | 26.3 |
| I didn’t intend to have sex without a condom, but I was too fucked up and I couldn’t think properly | 73.7 | 26.3 |
| Usually I am more careful. But I am too fucked up to think about using a condom | 52.6 | 5.3 |
| Escape, escape, escape! I just want to forget about everything and have sex | 42.1 | 15.8 |
To gain further qualitative understanding of participants’ experiences with the adapted SJEI, we elicited participant comments. Participants reacted positively to the adapted SJEI, and many appreciated the informal language used. Participants commented: “Current street language is refreshing, good” and “[The upfront language] makes me want to be more honest.” Participants also commented on the comprehensiveness and utility of the instrument: “A lot of the wording seems very close to the actual thoughts I had or have had; so it felt authentic,” and “Felt it was all there—the reasons I had unprotected sex and how I would think about it.” A few participants provided comments regarding minor wording changes to specific items and the written instructions. Six additional items were added to the SJEI based on the pretest.
Phase 3: Results of Pilot-Testing the Final SJEI and PCC Session
Twenty episodic, substance-using MSM participating in the pilot-test reported similar feedback regarding the SJEI as those participating in the pretest phase of the study. One participant, however, did not agree with the use of the informal language, stating “I think the use of the word ‘fuck’ makes the sex sound cheap. Why not be a little gentler? Not all gay sex is depraved.” Other participant reactions included one participant for whom English is a second language stating that the SJEI was clear and the language appropriate. According to one participant: “It was good. The questions were straight to the point. A little scary, but also makes you wake up and realize things as well.” No additional self-justifications were identified for inclusion in the final adapted SJEI based on the pilot-testing. The majority of participants expressed positive feedback regarding the adapted PCC session. In particular, participants stated that the intervention was a reality check for them, made them think about the role of substance use in their decisions to engage in risky sex, and appreciation for the opportunity to explore their risky behaviors with the counselor.
Discussion
We demonstrated the process required to adapt the PCC evidence-based behavioral intervention for a new population of episodic, substance-using MSM. The adaptation process involved modifying a key component of the PCC intervention, the SJEI, for use as a socio-culturally appropriate tool to elicit particular thoughts and feelings that led to decisions to engage in unprotected anal intercourse with concurrent substance use. Consistent with CDC guidelines for adapting evidence-based behavioral interventions (McKleroy, et al. 2006), we completed a three-step formative research process including in-depth interviews with the target population to identify self-justifications for engaging in concurrent unprotected anal intercourse and substance use, pretesting the adapted SJEI, and pilot-testing the adapted PCC intervention. This process included the collection of formative data to assess socio-culturally relevant behaviors and contexts; the application of new information to modify a key characteristic of an existing evidence-based behavioral intervention; and the pilot-testing of the adapted evidence-based behavioral intervention prior to full intervention implementation.
Nine themes emerged from the in-depth interviews. The four most common themes reported by episodic, substance-using MSM included substance use as facilitator of risk, transmission risk calculus (i.e., assessment of risk level per sex act), assumptions regarding partners, and cognitive escape. Over half of the items included in the pretested SJEI addressed these themes. Other themes that emerged from the qualitative analysis included sensation seeking/spontaneity, condom-related issues, opportunities for sex, expectations/obligations to partners, and invincibility. While many new self-justifications were identified, episodic, substance-using MSM also echoed self-justifications included in the original PCC instrument. This suggests certain reasons for engaging in high risk behavior resonate with MSM in general.
There are several aspects to the adaptation process described here which bear mention. While the formative data collection was led by a senior qualitative researcher, project staff with little or no prior experience analyzing qualitative data were trained to carry out this work. Our approach for formative data collection, structural coding and group consensus analysis can be replicated by public health departments and community-based organizations with a minimal degree of technical assistance. In addition, data collection, analysis, and pilot-testing were conducted with an eye on time management. We considered the minimal number of interviews needed to generate formative data sufficient to adapt the SJEI, move swiftly through the data reduction and abstraction process, and develop new SJEI items. Health departments and other organizations interested in implementing the adaptation process outlined here would not necessarily need technical assistance beyond the existing skills and resources typically deployed during in-house routine project evaluations. If technical assistance were requested, it could take the form of brief training in the administration of a semi-structured interview guide for formative data collection with the target population, and brief training in the data reduction, abstraction, and SJEI development as outlined here.
There are several limitations that merit discussion. First, formative data collection took place with a limited number of episodic, substance-using MSM (Dilley et al. 2007). A larger sample may have captured greater diversity of self-justifications for sexual risk taking behavior among episodic, substance-using MSM. However, based on the relative diversity of participants in terms of age, race/ethnicity and substances used, the reported self-justifications are likely to be applicable to various subgroups of episodic, substance-using MSM. We intend to assess the diversity of self-justifications reported by participants during the randomized trial phase of the study. Second, the formative data collection instrument was focused on self-justifications for unsafe sexual encounters while using drugs or alcohol. While this is consistent with the aims of the study, the findings may be limited in terms of broader social, familial, historical and structural factors contributing to unsafe sex in this population. It is possible that these factors would have emerged through other formative approaches including the life story interview (Atkinson 1998) or an ethnographic approach (Spradley 1979). Third, as with all formative qualitative studies, it is possible that the viewpoints of participants who were very emotive and forthcoming could eclipse the data of those participants who were less verbose or articulate during the group data analysis phases. To safeguard against this risk for uneven data quality and quantity, we trained study interviewers in conducting qualitative interviews about sensitive topics with MSM, and conducted quality control on interview length and topic guide fidelity during the formative phase. Finally, group consensus decision-making about relevant self-justifications can run the risk of “group think” where certain ideas gain traction, and others remain unvoiced in the group setting. Although it is difficult to assess the level of knowledge and specificity that may have been available if we used a more sophisticated coding system, our methodology was effective in terms of knowledge production and the pragmatic way in which we implemented our adaptation process. Similar methods were used in another adaptation of the PCC intervention (Skinta et al. 2012), and, more importantly, the adapted SJEI was viewed favorably by MSM in the pretest and pilot-test in this study.
Service providers are increasingly under pressure to make limited fiscal resources stretch farther to achieve high-impact HIV prevention (CDC 2011), including the adaptation of existing evidence-based behavioral interventions for high-risk populations. As researchers and public health professionals often lack basic roadmaps to help them adapt evidence-based behavioral interventions, this paper offers a pragmatic approach to adapt an evidence-based behavioral intervention for MSM at high-risk of HIV infection. Moreover, now that PCC is being nationally disseminated by the CDC’s Diffusion of Effective Behavioral Intervention Project (Collins et al. 2006), it will be necessary to adapt the intervention for different populations of MSM (Veniegas et al. 2009). The next step is to test the efficacy of the adapted PCC intervention with episodic, substance-using MSM; a randomized controlled trial is currently being implemented. Our three-phase adaptation process can serve as a useful roadmap for researchers and HIV prevention providers to follow as they expand the use of the PCC and other evidence-based behavioral interventions for high-risk populations.
Acknowledgments
This research was supported by the Centers for Disease Control and Prevention under cooperative agreement UR6PS000684 to Public Health Foundation Enterprises, City of Industry, California. The authors would like to acknowledge the participants in our study for their willingness to share their innermost thoughts and feelings. Thanks are also to Deborah J. Gelaude, Duane Moody and Vel McKleroy for their contributions to the development of the qualitative interview guide.
Footnotes
Disclaimer The findings and conclusions in this paper are those of the authors and do not necessarily represent the views of the US Centers for Disease Control and Prevention.
Contributor Information
Kelly R. Knight, Email: kelly.knight@ucsf.edu, Department of Anthropology, History and Social Medicine, University of California, San Francisco, 3333 California Street, Suite 485, San Francisco, CA 94143-0850, USA
Moupali Das, San Francisco Department of Public Health, HIV Prevention Section, Substance Use Research Unit, San Francisco, CA, USA.
Erin DeMicco, San Francisco Department of Public Health, HIV Prevention Section, Substance Use Research Unit, San Francisco, CA, USA.
Jerris L. Raiford, Prevention Research Branch, Division of HIV/AIDS Prevention, NCHHSTP, CDC, Atlanta, GA, USA
Tim Matheson, San Francisco Department of Public Health, HIV Prevention Section, Substance Use Research Unit, San Francisco, CA, USA.
Alic Shook, San Francisco Department of Public Health, HIV Prevention Section, Substance Use Research Unit, San Francisco, CA, USA.
Erin Antunez, San Francisco Department of Public Health, HIV Prevention Section, Substance Use Research Unit, San Francisco, CA, USA.
Glenn-Milo Santos, San Francisco Department of Public Health, HIV Prevention Section, Substance Use Research Unit, San Francisco, CA, USA.
Rand Dadasovich, San Francisco Department of Public Health, HIV Prevention Section, Substance Use Research Unit, San Francisco, CA, USA.
James W. Dilley, Department of Psychiatry, University of California San Francisco and San Francisco General Hospital, San Francisco, CA, USA
Grant N. Colfax, San Francisco Department of Public Health, HIV Prevention Section, Substance Use Research Unit, San Francisco, CA, USA
Jeffrey H. Herbst, Prevention Research Branch, Division of HIV/AIDS Prevention, NCHHSTP, CDC, Atlanta, GA, USA
References
- Atkinson R. The life story interview (Sage University Papers Series on Qualitative Research Methods) Vol. 44. Thousand Oaks, CA: Sage; 1998. [Google Scholar]
- Bandura A. Self-efficacy: Toward a unifying theory of behavioral change. Psychological Reviews. 1977a;84:191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- Bandura A. Social learning theory. Englewood Cliffs, NJ: Prentice Hall; 1977b. [Google Scholar]
- Carey JW, Gelaude D. Systematic methods for collecting and analyzing multidisciplinary team-based qualitative data. In: Guest G, MacQueen KM, editors. Handbook for team-based qualitative research. Lanham, MD: AltaMira; 2008. [Google Scholar]
- Carey JW, Mejia R, Bingham T, Ciesielski C, Gelaude D, Herbst JH, Stall R. Drug use, high-risk sex behaviors, and increased risk for recent HIV infection among men who have sex with men in Chicago and Los Angeles. AIDS and Behavior. 2009;13:1084–1096. doi: 10.1007/s10461-008-9403-3. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. PS07-004: Adopting and Demonstrating the Adaptation of Prevention Techniques for Persons at Highest Risk of Acquiring or Transmitting Human Immunodeficiency Virus (ADAPT 2)—(UR6) Atlanta, GA: Centers for Disease Control and Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD and TB Prevention, Division of HIV/AIDS Prevention; 2007. [Google Scholar]
- Centers for Disease Control and Prevention. High-impact HIV prevention. Atlanta, GA: Centers for Disease Control and Prevention, National Center for HIV/AIDS, Viral Hepatitis, STD and TB Prevention, Division of HIV/AIDS Prevention; 2011. Retrieved December 9, 2012from http://www.cdc.gov/hiv/strategy/dhap/pdf/nhas_booklet.pdf. [Google Scholar]
- Centers for Disease Control and Prevention. HIV Surveillance Report, 2010. Vol. 22. Atlanta, GA: Centers for Disease Control and Prevention; 2012. Retrieved December 9, 2012, from http://www.cdc.gov/hiv/topics/surveillance/resources/reports/ [Google Scholar]
- Colfax G, Vittinghoff E, Husnik MJ, McKirnan D, Buchbinder S, Koblin B EXPLORE Study Team. Substance use and sexual risk: a participant- and episode-level analysis among a cohort of men who have sex with men. American Journal of Epidemiology. 2004;159:1002–1012. doi: 10.1093/aje/kwh135. [DOI] [PubMed] [Google Scholar]
- Collins C, Harshbarger C, Sawyer R, Hamdallah M. The diffusion of effective behavioral interventions project: Development, implementation and lessons learned. AIDS Education and Prevention. 2006;18(Suppl A):5–20. doi: 10.1521/aeap.2006.18.supp.5. [DOI] [PubMed] [Google Scholar]
- Diaz RM, Heckert AL, Sanchez J. Reasons for stimulant use among Latino gay men in San Francisco: A comparison between methamphetamine and cocaine users. Journal of Urban Health. 2005;82(1 Suppl 1):i71–i78. doi: 10.1093/jurban/jti026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiClemente C, Prochaska J. Processes and stages of self-change: coping and competence in smoking behavior change. In: Shiffman S, Wills T, editors. Coping and substance abuse. San Diego, CA: Academic; 1985. [Google Scholar]
- DiClemente C, Prochaska J, Gilbertini M. Self-efficacy and the stages of self-change of smoking. Cognitive Therapy and Research. 1985;9:181–200. [Google Scholar]
- Dilley JW, Schwarcz S, Murphy J, Joseph C, Vittinghoff E, Scheer S. Efficacy of personalized cognitive counseling in men of color who have sex with men: Secondary data analysis from a controlled intervention trial. AIDS and Behavior. 2011;15:970–975. doi: 10.1007/s10461-010-9771-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dilley JW, Woods WJ, Loeb L, Nelson K, Sheon N, Mullan J, McFarland W. Brief cognitive counseling with HIV testing to reduce sexual risk among men who have sex with men: Results from a randomized controlled trial using paraprofessional counselors. Journal of Acquired Immune Deficiency Syndromes. 2007;44:569–577. doi: 10.1097/QAI.0b013e318033ffbd. [DOI] [PubMed] [Google Scholar]
- Dilley JW, Woods WJ, Sabatino J, Lihatsh T, Adler B, Casey S, McFarland W. Changing sexual behavior among gay male repeat testers for HIV: A randomized, controlled trial of a single-session intervention. Journal of Acquired Immune Deficiency Syndromes. 2002;30:177–186. doi: 10.1097/00042560-200206010-00006. [DOI] [PubMed] [Google Scholar]
- Drumright LN, Patterson TL, Strathdee SA. Club drugs as causal risk factors for HIV acquisition among men who have sex with men: A review. Substance Use & Misuse. 2006;41:1551–1601. doi: 10.1080/10826080600847894. [DOI] [PubMed] [Google Scholar]
- Galbraith JS, Herbst JH, Whittier DK, Jones PL, Smith BD, Fisher HH. Taxonomy for strengthening the identification of core elements for evidence-based behavioral interventions for HIV/AIDS prevention. Health Education Research. 2011;26:872–885. doi: 10.1093/her/cyr030. [DOI] [PubMed] [Google Scholar]
- Glaser B, Strauss A. The discovery of grounded theory: Strategies for qualitative research. New York City, NY: Aldine; 1967. [Google Scholar]
- Gold RS, Aucote HM. ‘I’m less at risk than most guys’: Gay men’s unrealistic optimism about becoming infected with HIV. International Journal of STDs and AIDS. 2003;14:18–23. doi: 10.1258/095646203321043200. [DOI] [PubMed] [Google Scholar]
- Gold RS, Rosenthal DA. Preventing unprotected anal intercourse in gay men: A comparison of two intervention techniques. International Journal of STDs and AIDS. 1995;6:89–94. doi: 10.1177/095646249500600205. [DOI] [PubMed] [Google Scholar]
- Gold RS, Rosenthal DA. Examining self-justifications for unsafe sex as a technique of AIDS education: The importance of personal relevance. International Journal of STDs and AIDS. 1998;9:208–213. doi: 10.1258/0956462981922052. [DOI] [PubMed] [Google Scholar]
- Gold RS, Skinner MJ. Situational factors and thought processes associated with unprotected intercourse in young gay men. AIDS. 1992;6:1021–1030. doi: 10.1097/00002030-199209000-00017. [DOI] [PubMed] [Google Scholar]
- Gold RS, Skinner MJ, Roass MW. Unprotected anal intercourse in HIV-infected and non-HIV-infected gay men. Journal of Sex Research. 1994;31:59–77. [Google Scholar]
- Halkitis PN, Mukherjee PP, Palamar JJ. Longitudinal modeling of methamphetamine use and sexual risk behaviors in gay and bisexual men. AIDS and Behavior. 2009;13:783–791. doi: 10.1007/s10461-008-9432-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heath J, Lanoye A, Maisto SA. The role of alcohol and substance use in risky sexual behavior among older men who have sex with men: A review and critique of the current literature. AIDS and Behavior. 2012;16:578–589. doi: 10.1007/s10461-011-9921-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hirshfield S, Remien RH, Humberstone M, Walavalkar I, Chiasson MA. Substance use and high-risk sex among men who have sex with men: A national online study in the USA. AIDS Care. 2004;16:1036–1047. doi: 10.1080/09540120412331292525. [DOI] [PubMed] [Google Scholar]
- MacQueen K, McLellan E, Kay K, Milstein B. Codebook development for team-based qualitative analysis. Cultural Anthropology Methods. 1998;10:31–36. [Google Scholar]
- MacQueen KM, McLellan-Lemal E, Bartholow K, Milstein B. Team-based codebook development: Structure, process, and agreement. In: Guest G, MacQueen KM, editors. Handbook for team-based qualitative research. Lanham, MD: AltaMira; 2008. pp. 119–135. [Google Scholar]
- Mansergh G, Koblin BA, McKirnan DJ, Hudson SM, Flores SA, Weigand RE, Project MIX, Team S. An intervention to reduce HIV risk behavior of substance-using men who have sex with men: A two-group randomized trial with a nonrandomized third group. PLoS Medicine. 2010;7(8):e1000329. doi: 10.1371/journal.pmed.1000329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mansergh G, Shouse RL, Marks G, Guzman R, Rader M, Colfax GN. Methamphetamine and sildenafil (Viagra) use are linked to unprotected receptive and insertive anal sex, respectively, in a sample of men who have sex with men. Sexually Transmitted Infections. 2006;82:131–134. doi: 10.1136/sti.2005.017129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKirnan DJ, Vanable PA, Ostrow DG, Hope B. Expectancies of sexual “escape” and sexual risk among drug and alcohol-involved gay and bisexual men. Journal of Substance Abuse. 2001;13:137–154. doi: 10.1016/s0899-3289(01)00063-3. [DOI] [PubMed] [Google Scholar]
- McKleroy VS, Galbraith JS, Cummings B, Jones P, Harshbarger C, Collins C, Carey JW. Adapting evidence-based behavioral interventions for new settings and target populations. AIDS Education and Prevention. 2006;18(4 Suppl A):59–73. doi: 10.1521/aeap.2006.18.supp.59. [DOI] [PubMed] [Google Scholar]
- Miles MB, Huberman AM. Qualitative data analysis. Thousand Oaks, CA: Sage; 1994. [Google Scholar]
- Morgenstern J, Bux DA, Jr, Parsons J, Hagman BT, Wainberg M, Irwin T. Randomized trial to reduce club drug use and HIV risk behaviors among men who have sex with men. Journal of Consulting and Clinical Psychology. 2009;77:645–656. doi: 10.1037/a0015588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nichter M, Nichter M, Thompson PJ, Shiffman S, Moscicki AB. Using qualitative research to inform survey development on nicotine dependence among adolescents. Drug and Alcohol Dependence. 2002;68(Suppl 1):S41–56. doi: 10.1016/s0376-8716(02)00214-4. [DOI] [PubMed] [Google Scholar]
- Office of National AIDS Policy. National HIV/AIDS Strategy for the United States. Washington, DC: Office of National AIDS Policy, The White House; 2010. [Google Scholar]
- Paul JP, Stall R, Davis F. Sexual risk for HIV transmission among gay/bisexual men in substance-abuse treatment. AIDS Education and Prevention. 1993;5:11–24. [PubMed] [Google Scholar]
- Paul JP, Stall RD, Crosby GM, Barrett DC, Midanik LT. Correlates of sexual risk-taking among gay male substance abusers. Addiction. 1994;89:971–983. doi: 10.1111/j.1360-0443.1994.tb03357.x. [DOI] [PubMed] [Google Scholar]
- Plankey MW, Ostrow DG, Stall R, Cox C, Li X, Peck JA, Jacobson LP. The relationship between methamphetamine and popper use and risk of HIV seroconversion in the multicenter AIDS cohort study. Journal of Acquired Immune Deficiency Syndromes. 2007;45:85–92. doi: 10.1097/QAI.0b013e3180417c99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Purcell DW, Johnson C, Lansky A, Prejean J, Stein R, Denning P, Crepaz N. Estimating the population size of men who have sex with men in the United States to obtain HIV and syphilis rates. Open AIDS Journal. 2012;6:98–107. doi: 10.2174/1874613601206010098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Remien RH, Goetz R, Rabkin JG, Williams JB, Bradbury M, Gorman JM. Remission of substance use disorders: Gay men in the first decade of AIDS. Journal of Studies on Alcohol. 1995;56:226–232. doi: 10.15288/jsa.1995.56.226. [DOI] [PubMed] [Google Scholar]
- Rubin HIR. Qualitative interviewing: The art of hearing data. Thousand Oaks, CA: Sage; 1995. [Google Scholar]
- Sanchez T, Finlayson T, Drake A, Behel S, Cribbin M, DiNenno E, Lansky A. Human immunodeficiency virus (HIV) risk, prevention, and testing behaviors—United States, National HIV Behavioral Surveillance System: Men who have sex with men, November 2003–April 2005. MMWR Surveillance Summary. 2006;55:1–16. [PubMed] [Google Scholar]
- Santos GM, Das M, Colfax GN. Interventions for non-injection substance use among US men who have sex with men: What is needed. AIDS and Behavior. 2011;15(Suppl 1):S51–S56. doi: 10.1007/s10461-011-9923-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seidman I. Interviewing as qualitative research: A guide for researchers in education and the social sciences. New York, NY: Teachers College Press; 1991. [Google Scholar]
- Semple SJ, Patterson TL, Grant I. Motivations associated with methamphetamine use among HIV+men who have sex with men. Journal of Substance Abuse Treatment. 2002;22:149–156. doi: 10.1016/s0740-5472(02)00223-4. [DOI] [PubMed] [Google Scholar]
- Shoptaw S, Reback CJ, Peck JA, Yang X, Rotheram-Fuller E, Larkins S, Hucks-Ortiz C. Behavioral treatment approaches for methamphetamine dependence and HIV-related sexual risk behaviors among urban gay and bisexual men. Drug and Alcohol Dependence. 2005;78:125–134. doi: 10.1016/j.drugalcdep.2004.10.004. [DOI] [PubMed] [Google Scholar]
- Skinta MD, Murphy JL, Paul JP, Schwarcz SK, Dilley JW. Thoughts, attitudes and feelings of HIV-positive MSM associated with high transmission-risk sex. Health Education & Behavior. 2012;39:315–323. doi: 10.1177/1090198111427390. [DOI] [PubMed] [Google Scholar]
- Solomon J, Card JJ, Malow RM. Adapting efficacious interventions: Advancing translational research in HIV prevention. Evaluation & the Health Professions. 2006;29:162–194. doi: 10.1177/0163278706287344. [DOI] [PubMed] [Google Scholar]
- Spradley JP. The ethnographic interview. New York, NY: Holt, Rinehart and Winston; 1979. [Google Scholar]
- Stall RD, Paul JP, Barrett DC, Crosby GM, Bein E. An outcome evaluation to measure changes in sexual risk-taking among gay men undergoing substance use disorder treatment. Journal of Studies on Alcohol and Drugs. 1999;60:837–845. doi: 10.15288/jsa.1999.60.837. [DOI] [PubMed] [Google Scholar]
- Strauss A, Corbin J. Basics of qualitative research: Grounded theory procedures and techniques. Newbury Park, CA: Sage; 1990. [Google Scholar]
- Veniegas RC, Kao UH, Rosales R. Adapting HIV prevention evidence-based interventions in practice settings: An interview study. Implementation Science. 2009;4:76. doi: 10.1186/1748-5908-4-76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wingood GM, DiClemente RJ. The ADAPT-ITT model: A novel model of adapting evidence-based HIV interventions. Journal of Acquired Immune Deficiency Syndromes. 2008;47:S40–S46. doi: 10.1097/QAI.0b013e3181605df1. [DOI] [PubMed] [Google Scholar]