Abstract
Objective
Vaccine effectiveness analysis serves as a critical evaluation for immunization programmes and vaccination coverage. It also contributes to maintaining public confidence with the vaccine providers. This study estimated measles vaccine effectiveness at the population level using Australian national notifications data between 2006 and 2012.
Methods
Notification data were obtained from the National Notifiable Diseases Surveillance System. Vaccination status was classified according to whether a case had received zero, one or two doses of measles-containing vaccine. Cases aged less than 1 year and those with unknown vaccination status were excluded. All children with disease onset between 1 January 2006 and 31 December 2012 who were born after 1996 were included. Cases were matched to controls extracted from the Australian Childhood Immunization Register according to date of birth and jurisdiction of residence. Vaccine effectiveness was estimated by conditional logistic regression. Sensitivity analyses were conducted to test data robustness.
Results
Vaccine effectiveness was estimated at 96.7% (95% confidence interval [CI]: 94.5–98.0%) for one dose and 99.7% (95% CI: 99.2–99.9%) for two doses of measles vaccine. For at least one dose, effectiveness was estimated at 98.7% (95% CI: 97.9–99.2%). Sensitivity analyses did not significantly alter the base estimates.
Discussion
Vaccine effectiveness estimates suggested that the measles vaccine was protective at the population level between 2006 and 2012. However, vaccination coverage gaps may have contributed to recent measles outbreaks and may represent a serious barrier for Australia to maintain measles elimination status.
Introduction
The Australian National Immunization Program (NIP) has funded the measles vaccine since 1972, with the first national vaccine schedule including measles vaccine for all infants aged 12 months in 1975.1 In 1989, measles-mumps-rubella (MMR) vaccine was included on the schedule for all infants 12 months of age, with a second dose being included soon after, originally for children aged 10–14 years. Since the late 1990s, two doses have been recommended and scheduled at 12 months and 4–5 years, with the second dose changed to 4 years from 2000.1 From July 2013, the second dose has been rescheduled to 18 months due to the introduction of the measles-mumps-rubella-varicella vaccine.1,2 As part of a dedicated effort for measles elimination, various funded catch-up campaigns have been conducted to ensure that those born since the 1970s have received two doses of measles-containing vaccine. Anyone born since 1966 has also been recommended to receive two doses.1
Though efforts to eliminate measles have resulted in a notable decrease in measles notifications since the mid-1990s in Australia, vaccination coverage rates have been below 95%, the optimal rate for herd immunity to protect against outbreaks.3 Consequently, imported cases have continued to trigger outbreaks, for example one that occurred in New South Wales in 2012 that infected 168 cases.4
Few measles vaccine effectiveness analyses have been published in Australia after the Measles Control Campaign in the late 1990s, except after an outbreak in New South Wales in 2006.5
This report assessed the vaccine effectiveness at the population level in Australia between 2006 and 2012 and explored results within the epidemiological context of measles in an era of elimination.
Methods
Case definition
As required by legislation, all Australian states and territories must notify public health authorities of all probable and confirmed cases of measles using the national notifiable diseases case definition.6 A confirmed case requires laboratory definitive evidence or a combination of clinical and epidemiological evidence. A probable case requires laboratory suggestive evidence and clinical evidence.
Case selection
All measles cases notified to the National Notifiable Diseases Surveillance System (NNDSS) with an onset between 1 January 2006 and 31 December 2012 who were born after 1996 were included. Data were restricted to 2006 through 2012 because the NNDSS data for all states and territories were more complete from 2006 onwards. Those aged less than 1 year were excluded as they were not eligible for measles vaccination.
Controls were selected from the Australian Childhood Immunization Register (ACIR) database. The ACIR is a population-based register which includes all children of citizens and permanent residents enrolled in the national publicly funded health-care system regardless of vaccination status.7 For each case, controls were randomly sampled from the ACIR and matched to cases by date of birth (plus or minus one day) and state or territory of residence. Twenty age-matched controls were sampled for each case to maximize precision based on previously used methods.8 Only cases aged less than 17 years were included in the analysis because the ACIR began in 1996.
Vaccination status for cases was obtained from the NNDSS and was summarized as zero, one, two doses or unknown. Where the NNDSS had only classified a case as partially or fully vaccinated, vaccination status was interpreted according to the case’s age and the vaccination schedule in place at the time of illness for analysis. “Fully vaccinated” was interpreted as one dose for anyone aged less than 4 years at the time of disease onset and two doses for anyone aged 4 years or older. “Partially vaccinated” therefore was interpreted as one dose for anyone aged 4 years or older. Any doses recorded within two weeks before disease onset were excluded from analysis. Vaccination status for controls, as well as gender and Indigenous status was obtained from the ACIR. Controls who had received a dose within two weeks of onset of disease in their matched case were considered to have had an invalid dose but were still included in the analysis.
Statistical methods
Using NNDSS data, trends in measles notifications from 1995 through 2012 were briefly described.
Comparisons of characteristics between cases and controls were analysed using the Pearson χ2 test at a significance level of P < 0.05. Conditional logistic regressions controlling for age and jurisdiction were conducted to estimate odds ratios (ORs) for receiving one, two or at least one dose of measles vaccine for cases and their matched controls. Odds ratios were also generated for broad age groups (0–5 years; 6–10 years; 11–15 years) in stratified analysis. Vaccine effectiveness (VE) estimates were calculated based on the formula9 VE = (1 – OR)*100. All analysis was done using Stata version 12.0 (Stata Corporation, College Station, TX, USA).
Ethics approval was not required as de-identified NNDSS and ACIR data are routinely provided to the National Centre for Immunization Research and Surveillance (NCIRS) for disease surveillance on behalf of the Australian Commonwealth Department of Health.
Sensitivity analyses
Sensitivity analyses were conducted as there were many participants with unknown vaccination status. Analyses were conducted first by categorizing all those with unknown vaccination status as having been vaccinated with age-dependent dosages and then categorizing all as unvaccinated. Vaccine effectiveness calculations were then executed using the same method described above.
Results
Secular trends among measles notifications
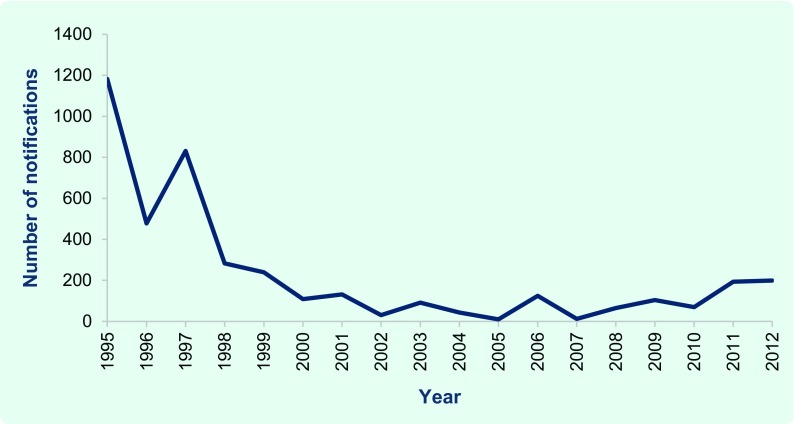
Between 1995 and 2012, 4111 measles notifications were reported to the NNDSS. Efforts to achieve and maintain measles elimination have resulted in a decrease in notifications in Australia since the mid- to late 1990s following the impact of the addition of the second dose to the NIP in 1992. There were 1182 notifications of measles in Australia in 1995 and the notifications decreased throughout the 1990s except in 1997. Notifications between 2000 and 2012 ranged from 10 to 199 annually (Fig. 1).
Fig. 1.
Since 2000, a disproportionate number of notifications were reported for those aged 20 to 59 years (52.4% on average). Notifications in 2011 and 2012 also showed an increase in cases aged 10 to 19 years (31.5% in 2011 and 25.6% in 2012). Most notifications in 2012 were from the New South Wales outbreak; among those cases, there was an increase in the number of notifications among infants less than 1 year of age (21.4% in the outbreak) who were too young to be vaccinated.
Study participants
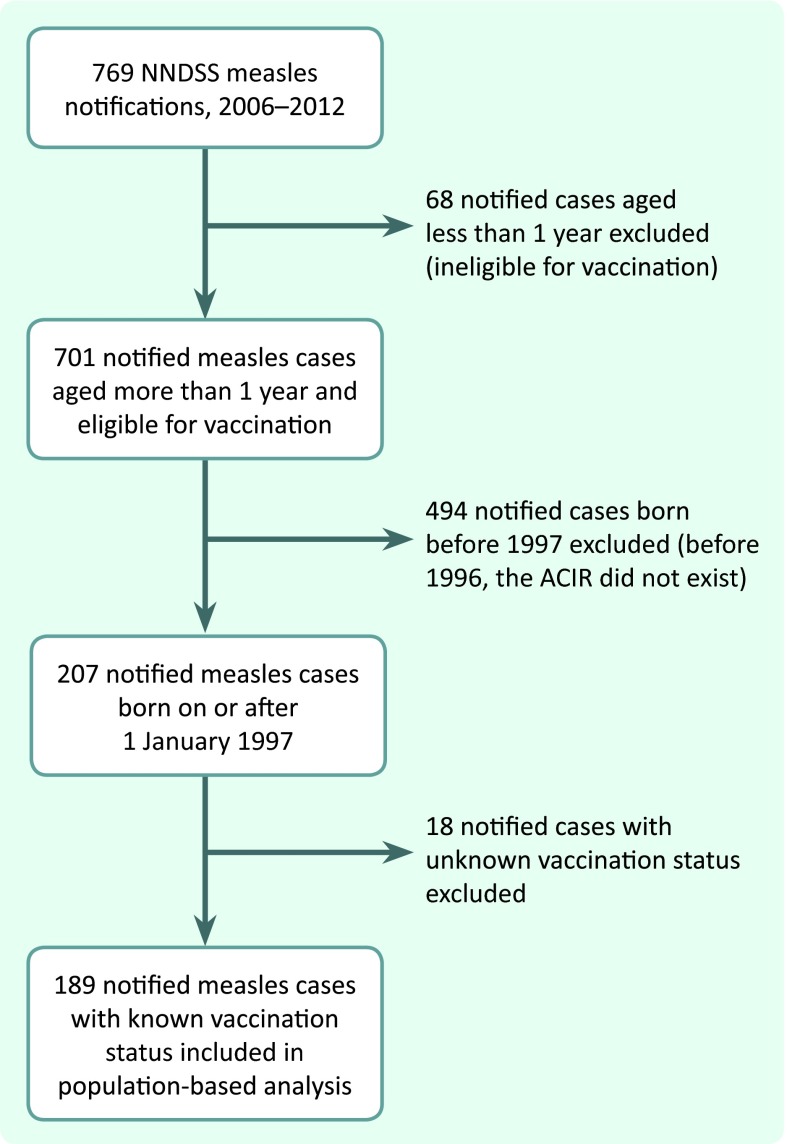
According to the inclusion criteria, 769 notifications were initially included. After excluding all notifications with disease onset before 2006, and those with a date of birth before 1997 or aged less than 1 year at the time of illness, 207 notifications remained. The majority of cases (40.1%) were aged 1 to 4 years, 30.4% were aged 5 to 9 years and 29.5% were aged 10 to 15 years.
Eighteen cases were excluded from the analysis due to their unknown vaccination status. More than half of the excluded cases (55.5%, n = 10) were aged 10–15 years. Seven cases included in the analysis were classified as having received zero doses of vaccine because they had received a dose immediately after exposure. Ultimately, 189 cases were included in the vaccine effectiveness analysis (Fig. 2).
Fig. 2.
Flow diagram showing case selection for vaccine effectiveness analysis, Australia, 2006–2012
ACIR, Australian Childhoon Immunization Register; NNDSS, National Notifiable Diseases Surveillance System.
Twenty controls were matched for each case, resulting in a total of 3780 controls. There were no significant differences between cases and controls in terms of gender (P = 0.34) and Indigenous status (P = 0.52).
Vaccine effectiveness estimates
The overall estimated vaccine effectiveness for one dose of MMR was 96.7% (95% CI: 94.5–98.0%). For at least one dose, vaccine effectiveness was estimated to be 98.7% (95% CI: 97.9–99.2%) and for two doses, it was 99.7% (95% CI: 99.2–99.9%) (Table 1).
Table 1. Vaccination status and vaccine effectiveness for notified measles cases and matched controls, Australia, 2006–2012.
| Doses | Number of cases (%) n = 189 |
Number of controls (%) n = 3 780 |
VE% (95% CI) |
|---|---|---|---|
| 0 | 160 (84.7) | 437 (11.6) | – |
| 1 | 22 (11.6) | 1403 (37.1) | 96.7 (94.5–98.0) |
| At least 1 | 29 (15.3) | 3343 (88.4) | 98.7 (97.9–99.2) |
| 2 | 7 (3.7) | 1940 (51.3) | 99.7 (99.2–99.9) |
CI, confidence interval; VE, vaccine effectiveness.
Stratified analysis for age revealed that the estimated vaccine effectiveness for one dose of MMR was 97.9% (95% CI: 95.8–98.9%) for those aged 0 to 5 years, 98.6% (95% CI: 91.8–99.8%) for those aged 6 to 10 years and 82.7% (95% CI: 58.9–92.7%) for those aged 11 to 15 years. The estimate of the 11 to 15 year age group was significantly lower than that of the 0 to 5 year age group. Among these age groups, vaccine effectiveness estimates for two doses ranged from 99.3% to 99.8%. The differences among each group were not significant (Table 2).
Table 2. Vaccination status and vaccine effectiveness estimates for notified measles cases and matched controls stratified by age group, Australia, 2006–2012.
| Age (years) | Doses | Number of cases (%) n = 189 |
Number of controls (%) n = 3 780 |
VE% (95% CI) |
|---|---|---|---|---|
| 0–5 | 0 | 75 (39.7) | 334 (8.8) | – |
| 1 | 11 (5.8) | 1206 (31.9) | 97.9 (95.8–98.9) | |
| 2 | 1 (0.5) | 200 (5.3) | 99.7 (95.5–100.0) | |
| 6–10 | 0 | 53 (28.0) | 55 (1.5) | – |
| 1 | 2 (1.1) | 104 (2.8) | 98.6 (91.8–99.8) | |
| 2 | 3 (1.6) | 1001 (26.5) | 99.8 (99.0–100.0) | |
| 11–15 | 0 | 32 (16.9) | 48 (1.3) | – |
| 1 | 9 (4.8) | 93 (2.5) | 82.7 (58.9–92.7) | |
| 2 | 3 (1.6) | 739 (19.6) | 99.3 (97.5–99.8) |
CI, confidence interval; VE, vaccine effectiveness.
Sensitivity analysis
When all cases with unknown vaccination status were categorized as having been vaccinated, 16 individuals were categorized as receiving two doses and two individuals were categorized as receiving one dose. The vaccine effectiveness was then estimated at 96.9% for one dose (95% CI: 94.9–98.1%) and 99.1% (95% CI: 98.3–99.5%) for two doses.
When all 18 individuals with unknown vaccination status were categorized as unvaccinated, the vaccine effectiveness estimate was 97.5% for one dose (95% CI: 95.7–98.6%) and 99.8% for two doses (95% CI: 99.5–99.9%) (Table 3).
Table 3. Sensitivity analyses of vaccination status and vaccine effectiveness for notified measles cases and matched controls, Australia, 2006–2012.
| Original VE% (95% CI) | Sensitivity analyses | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| VE% (95% CI) categorizing all unknown vaccination status* as unvaccinated | VE% (95% CI) categorizing all unknown vaccination status* as vaccinated | ||||||||
| Doses | No. cases (%) n = 189 |
No. controls (%) n = 3 780 |
VE estimate (95% CI) | No. cases (%) n = 207 |
No. controls (%) n = 4 140 |
VE estimate (95% CI) | No. cases (%) n = 207 |
No. controls (%) n = 4 140 |
VE estimate (95% CI) |
| 0 dose | 160 (84.7) |
437 (11.6) |
– | 160 (77.3) |
476 (11.5) |
– | 178 (86.0) |
476 (11.5) |
– |
| 1 dose | 22 (11.6) |
1403 (37.1) |
96.7 (94.5–98.0) |
24 (11.6) |
1478 (35.7) |
96.9 (94.9–98.1) |
22 (10.6) |
1478 (35.7%) | 97.5 (95.7–98.6) |
| 2 doses | 7 (3.7) |
1940 (51.3) |
99.7 (99.2–99.9) |
23 (11.1) |
2186 (52.8) |
99.1 (98.3–99.5) |
7 (3.4) |
2186 (52.8) |
99.8 (99.5–99.9) |
* Eighteen cases with unknown vaccination status were excluded from the original analysis. Dosage was categorized according to the age of the individual.
CI, confidence interval; VE, vaccine effectiveness.
No significant differences were found in the estimates of these two scenarios when compared to the original estimates.
Discussion
Vaccine effectiveness estimation is a critical component for evaluating an immunization schedule and its changes. Though it was unlikely that poor vaccine effectiveness played a part in contributing to measles transmission in Australia between 2006 and 2012, it is nevertheless important to conduct regular vaccine effectiveness analyses to rule out possible vaccine failure as a contributing factor. As Australia strives to maintain measles elimination status (broadly defined as the absence of transmission of endemic measles11), it is critical not only to understand why and how transmission continues to occur but also to be able to document all evidence that explains current measles epidemiology. This study is an important contribution to this evidence.
Results demonstrated that Australian measles vaccine has been effective (overall at least one dose was found to be 98.7%). The vaccine effectiveness estimates were similar to those following the 2006 New South Walesoutbreak that yielded 96% vaccine effectiveness.5 Recent analyses from other developed countries have also concluded similar effectiveness12–14 with the exception of a study in 2008 for a population-wide outbreak in Ukraine that concluded 93.1% effectiveness for two doses.15
Selection and misclassification biases are known to affect vaccine effectiveness analyses. Specifically, problems with case definitions, case ascertainment and ascertainment of vaccination status may bias the analysis.16 In this study, biases were reduced by using standard notification procedures with a sensitive case definition which minimized the number of missing cases. The distinct clinical features, high infectivity of the illness and the required laboratory evidence (both for probable and confirmed cases) minimized case misclassification.17 Suspected cases were also not reported to the NNDSS.18 It was possible that using de-identified ACIR data to obtain controls may have resulted in a case being matched to his/her self. However, due to the availability of numerous eligible matches, of which 20 were randomly selected, the possibility of this occurring was considered rare.
Vaccination status data were obtained from the NNDSS and were reliant upon the information provided by each state and territory. While vaccination status is only sometimes validated by medical records and ACIR data, self-reported data may be subject to recall bias. Studies have demonstrated that parental recall of vaccination status may overestimate vaccination coverage and a requirement for written verification may lead to underestimates.19,20 Notes from the 2012 New South Wales outbreak cases revealed that sometimes self-reports were accepted as proof of vaccination. For this analysis, vaccination status was accepted as whatever was reported in the NNDSS data.
In this report, the high number of cases with unknown vaccination status (8.7%, n = 18/207) may have been influenced by more than just incomplete NNDSS data. It has been suggested that the ACIR may underestimate coverage by 5% for both first and second doses of measles-containing vaccines.21 Although the results from the sensitivity analyses showed no significant differences compared to the original estimates where 18 cases were excluded due to unknown vaccination status, it is evident that the recording of vaccination status could be improved.
Finally, confounding may be problematic for the analysis. Socioeconomic data were not available in the data set for adjustment in this study. Cases and controls were, however, matched by date of birth and jurisdiction of residence. Also, cases and controls were found not significantly different in regards to gender or Indigenous status.
If vaccine effectiveness was excluded as a contributing factor in recent transmission and outbreaks in Australia, it may mean vaccination coverage has remained problematic to maintaining measles elimination. The Australian nationwide coverage estimates from 2010 reported 93.9% MMR coverage for those aged 24-months and 89.1% for those aged 60 months with New South Wales-specific coverage estimates at 93.8% and 89.3% for 24 months and 60 months of age, respectively.3 These percentages, however, conceal small pockets of lower coverage rates. The lowest 24-month coverage rates by Medicare Local catchments were recorded by North Coast New South Wales and Eastern Sydney at 89%. The lowest 60 month coverage rate was recorded in Eastern Sydney at 84%.22 These coverage estimates fall well short of the 95% mark, which is what World Health Organization (WHO) guidelines state is required to maintain elimination.18
The 2012 New South Wales outbreak highlighted areas where coverage gaps exist, demonstrating that those aged 10 to 19 years (29.2%, n = 40/168) and those of Pacific Islander descent (21.4%, n = 36/168) comprised a high proportion of cases.4 Evidence suggests that South Western Sydney high school students of Pacific Islander background may have missed out on routine childhood vaccinations both before and after their arrival in Australia.4 Although vaccination coverage among Pacific Island nations varies,23 WHO and the United Nations Children’s Fund estimates of Samoan vaccination coverage between 2003 and 2011 range from 45% to 67%; it is only in 2012 that estimates appear higher at 85%.23 Those aged 10 to 19 years who were born in Australia were eligible to have received two doses of measles-containing vaccine as part of the 1998 Measles Control Campaign that successfully vaccinated 96% of the targeted primary school age group.24 Further studies are needed to better understand the nature of the coverage gaps among this age group and those of Pacific Islander descent for targeted strategies to improve vaccination uptake.
In addition to coverage gaps, waning immunity was likely a cause of recent measles outbreaks. The vaccine effectiveness estimate calculated for those aged 11 to 15 years who had received one dose of vaccine was lower (82.7%) than that of the younger age groups (99.7% and 98.6% for those aged 0 to 5 years and those aged 6 to 10 years, respectively). This suggested that vaccine-induced immunity may be waning among older children, particularly if they have received only one dose of vaccine.25,26
Maternal antibody-induced immunity may also be waning earlier than anticipated. Though infant data were not incorporated into this study, infants are at high risk for measles infection and transmission; thus this age group is a critical component for understanding measles epidemiology. In the New South Wales 2012 outbreak, infants less than 1 year of age comprised 21.4% (n = 36) of cases.4 If this is indeed indicative of early waning of maternal antibodies, it may be problematic as more mothers are protected by vaccine-conferred immunity rather than immunity induced by measles infection.27–30
Although recent serosurvey results have demonstrated an effective reproductive number (R) of < 1 for measles transmission, meaning that the average number of secondary cases produced by a typical case remains below the epidemic threshold and indigenous transmission has been eliminated,31 a 2013 report noted that seropositivity has decreased since 1999 and that R could be approaching 1.32 This could be a major setback for Australia’s sustained measles elimination.
Conclusion
Our results not only provided evidence that vaccination failure had not contributed to measles infections between 2006 and 2012 but also served to evaluate measles immunization programmes in Australia. The analyses assisted in describing elimination era measles epidemiology and also highlighted the contribution of vaccination coverage gaps which require targeted improvement. In addition, vaccine effectiveness analyses served as essential contributions to maintain public and provider confidence in vaccinations, which are vital for maintaining measles elimination status in Australia and advancing the elimination goal globally.
Acknowledgements
The authors would like to acknowledge the Vaccine Preventable Diseases Surveillance Section, Health Emergency Management Branch, Office of Health Protection, Australian Government Department of Health for data from the National Notifiable Diseases Surveillance System and Medicare Australia, Department of Human Services for ACIR data.
Conflicts of interest
None declared.
Funding
None.
References
- 1.National Centre for Immunisation Research and Surveillance (NCIRS) Significant events in measles, mumps and rubella vaccination practice in Australia. New South Wales: The University of Sydney; 2013. http://www.ncirs.edu.au/immunisation/history/Measles-mumps-rubella-history-December-2013.pdf accessed 15 June 2015. [Google Scholar]
- 2.Australian Technical Advisory Group on Immunisation (ATAGI) The Australian Immunisation Handbook, 10th edition. Canberra: Australian Government Department of Health and Ageing; 2013. http://www.immunise.health.gov.au/internet/immunise/publishing.nsf/Content/Handbook10-home accessed 15 June 2015. [Google Scholar]
- 3.Hull B, et al. Annual immunisation coverage report, 2010. Communicable Diseases Intelligence Quarterly Report. 2013;37:E21–39. doi: 10.33321/cdi.2013.37.2. [DOI] [PubMed] [Google Scholar]
- 4.Najjar Z, et al. Sustained outbreak of measles in New South Wales, 2012: risks for measles elimination in Australia. Western Pacific Surveillance and Response Journal. 2014;5:14–20. doi: 10.5365/wpsar.2013.4.4.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sheppeard V, et al. Vaccine failures and vaccine effectiveness in children during measles outbreaks in New South Wales, March-May 2006. Communicable Diseases Intelligence Quarterly Report. 2009;33:21–6. doi: 10.33321/cdi.2009.33.3. [DOI] [PubMed] [Google Scholar]
- 6.Australian national notifiable diseases case definitions: measles case definition. Canberra: Australian Government Department of Health and Ageing; 2004. http://www.health.gov.au/internet/main/publishing.nsf/Content/cda-surveil-nndss-casedefs-cd_measl.htm accessed 15 June 2015. [Google Scholar]
- 7.Hull BP, Deeks SL, McIntyre PB. The Australian Childhood Immunisation Register-A model for universal immunisation registers? Vaccine. 2009;27:5054–60. doi: 10.1016/j.vaccine.2009.06.056. [DOI] [PubMed] [Google Scholar]
- 8.Quinn HE, et al. Duration of protection after first dose of acellular pertussis vaccine in infants. Pediatrics. 2014;133:e513–9. doi: 10.1542/peds.2013-3181. [DOI] [PubMed] [Google Scholar]
- 9.Orenstein WA, et al. Field evaluation of vaccine efficacy. Bulletin of the World Health Organization. 1985;63:1055–68. [PMC free article] [PubMed] [Google Scholar]
- 10.Number of notifications of measles, received from state and territory health authorities in the period of 1991 to 2012 and year-to-date notifications for 2013. Canberra: National Notifiable Diseases Surveillance System (NNDSS); 2013. [Google Scholar]
- 11.Field guidelines for measles elimination. Manila: World Health Organization Regional Office for the Western Pacific; 2004. http://www.wpro.who.int/publications/docs/FieldGuidelines_for_MeaslesElimination_0F24.pdf accessed 15 June 2015. [Google Scholar]
- 12.Arenz S, et al. Effectiveness of measles vaccination after household exposure during a measles outbreak: a household contact study in Coburg, Bavaria. The Pediatric Infectious Disease Journal. 2005;24:697–9. doi: 10.1097/01.inf.0000172900.70430.c2. [DOI] [PubMed] [Google Scholar]
- 13.Wichmann O, et al. Large measles outbreak at a German public school, 2006. The Pediatric Infectious Disease Journal. 2007;26:782–6. doi: 10.1097/INF.0b013e318060aca1. [DOI] [PubMed] [Google Scholar]
- 14.Yeung LF, et al. A limited measles outbreak in a highly vaccinated US boarding school. Pediatrics. 2005;116:1287–91. doi: 10.1542/peds.2004-2718. [DOI] [PubMed] [Google Scholar]
- 15.Velicko I, et al. Nationwide measles epidemic in Ukraine: the effect of low vaccine effectiveness. Vaccine. 2008;26:6980–5. doi: 10.1016/j.vaccine.2008.09.012. [DOI] [PubMed] [Google Scholar]
- 16.Torvaldsen S, McIntyre PB. Observational methods in epidemiologic assessment of vaccine effectiveness. Communicable Diseases Intelligence Quarterly Report. 2002;26:451–7. doi: 10.33321/cdi.2002.26.43. [DOI] [PubMed] [Google Scholar]
- 17.Hinman AR, Orenstein WA, Papania MJ. Evolution of measles elimination strategies in the United States. The Journal of Infectious Diseases. 2004;189(Suppl 1):S17–22. doi: 10.1086/377694. [DOI] [PubMed] [Google Scholar]
- 18.Heywood AE, et al. Elimination of endemic measles transmission in Australia. Bulletin of the World Health Organization. 2009;87:64–71. doi: 10.2471/BLT.07.046375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lister S, et al. Immunisation coverage in Australian children: a systematic review 1990–1998. Communicable Diseases Intelligence. 1999;23:145–70. doi: 10.33321/cdi.1999.23.21. [DOI] [PubMed] [Google Scholar]
- 20.Hawe P. Measles control: a best-practice challenge in public health. Australian Journal of Public Health. 1994;18:241–3. doi: 10.1111/j.1753-6405.1994.tb00237.x. [DOI] [PubMed] [Google Scholar]
- 21.Hull BP, et al. Immunisation coverage in Australia corrected for under-reporting to the Australian Childhood Immunisation Register. Australian and New Zealand Journal of Public Health. 2003;27:533–8. doi: 10.1111/j.1467-842X.2003.tb00829.x. [DOI] [PubMed] [Google Scholar]
- 22.Healthy communities: immunisation rates for children in 2011–2012. Sydney: National Health Performance Authority; 2013. http://www.nhpa.gov.au/internet/nhpa/publishing.nsf/Content/Report-Download-Healthy-Communities-Immunisation-rates-for-children-in-2011–12/$FILE/HC_ImmRate_TechSupp_FINAL_web.pdf accessed 15 June 2015. [Google Scholar]
- 23.WHO vaccine-preventable diseases: monitoring system: 2013 global summary. Geneva: World Health Organization; 2015. http://apps.who.int/immunization_monitoring/globalsummary accessed 15 June 2015. [Google Scholar]
- 24.Turnbull FM, et al. The Australian measles control campaign, 1998. Bulletin of the World Health Organization. 2001;79:882–8. [PMC free article] [PubMed] [Google Scholar]
- 25.Chen CJ, et al. Waning population immunity to measles in Taiwan. Vaccine. 2012;30:6721–7. doi: 10.1016/j.vaccine.2012.05.019. [DOI] [PubMed] [Google Scholar]
- 26.He H, et al. Waning immunity to measles in young adults and booster effects of revaccination in secondary school students. Vaccine. 2013;31:533–7. doi: 10.1016/j.vaccine.2012.11.014. [DOI] [PubMed] [Google Scholar]
- 27.Ramsay ME, et al. The elimination of indigenous measles transmission in England and Wales. The Journal of Infectious Diseases. 2003;187(Suppl 1):S198–207. doi: 10.1086/368024. [DOI] [PubMed] [Google Scholar]
- 28.Wise J. Measles outbreak hits northeast England. BMJ (Clinical research ed.) 2013;346(jan31 1):f662. doi: 10.1136/bmj.f662. [DOI] [PubMed] [Google Scholar]
- 29.Vivancos R, et al. An ongoing large outbreak of measles in Merseyside, England, January to June 2012. Euro Surveillance : European Communicable Disease Bulletin. 2012;•••:17. doi: 10.2807/ese.17.31.20234-en. [DOI] [PubMed] [Google Scholar]
- 30.Measles outbreak cases rise again as school vaccinations enter final week. Cardiff: Public Health Wales; 2013. http://www.wales.nhs.uk/sitesplus/888/news/27327 accessed 15 June 2015. [Google Scholar]
- 31.Gidding HF, et al. Sustained measles elimination in Australia and priorities for long term maintenance. Vaccine. 2007;25:3574–80. doi: 10.1016/j.vaccine.2007.01.090. [DOI] [PubMed] [Google Scholar]
- 32.Wood J, et al. Declining seropositivity in Australia and elimination status. Canberra: Communicable Disease Control Conference; 19–20 March 2013. [Google Scholar]