Abstract
Objective: This study examined the feasibility and acceptability of a body motion–activated videogame, targeting the prevention of opioid relapse among youth in the context of outpatient treatment.
Materials and Methods: Participants attended four weekly gameplay sessions. Surveys were conducted at baseline and following each week's gameplay and assessed satisfaction with gameplay, craving intensity, and self-efficacy to refuse opioids.
Results: Participants expressed a high level of satisfaction with the videogame throughout the 4 weeks and agreed with the statement that they would be more likely to attend treatment sessions if the game was present (mean=4.6; standard deviation [SD]=0.7) and would recommend the videogame to other people in treatment (mean=4.2; SD=0.8). All participants recommended playing the videogame as part of treatment at least weekly, with a third recommending playing daily. Self-reported cravings declined over the 4-week period from baseline (mean=12.7; SD=8.4) to Week 4 (mean=9.8; SD=8.3), although the decline was not significant. Although participants stated that they liked the game, one-third of participants had dropped out of the study by the fourth session of gameplay.
Conclusions: Preliminary evidence indicates that a motion videogame for addiction recovery may be feasible and acceptable within the context of outpatient treatment, although additional efforts are needed to keep youth in treatment. Future studies are needed to assess the impact of the game on long-term abstinence, treatment adherence, and engagement.
Introduction
Opioid dependence is increasingly recognized as a serious public health problem among adolescents. Nonmedical use of prescription drugs, which includes opiates, was the second most frequently used illicit drug among 12–17 year olds, following marijuana.1 Treatment admissions for opioid use disorders increased 196 percent between 1995 and 2000.2 Adolescent and young adult opioid dependence is associated with numerous negative outcomes, including overdose, human immunodeficiency virus transmission, school failure, criminal behavior, and other social problems.
The community standard of care for opioid-dependent youth entails detoxification, followed by traditional psychosocial treatments.3–5 Treatment programs suffer from poor retention in post–residential outpatient care, and youth experience high rates of relapse.6 Although the integration of pharmacotherapy with psychosocial treatment holds considerable promise for improving outcomes7—both with buprenorphine5,6,8 and with extended-release naltrexone9—dropout and problems with enduring treatment engagement remain major barriers to success.
There is a need to develop innovative strategies to promote abstinence and prevent dropout among youth. One strategy is to create a model of treatment that emphasizes experiential, activity-based approaches to recovery. One promising method for doing this is with videogames, which have high levels of general use among adolescents and young adults.10
Videogames have been explored as a therapeutic tool for alleviating psychological conditions such as stress, anxiety, and mood disorders,11 increasing physical activity, and promoting disease and pain management.12,13 Videogames have also been used to treat addiction. One example of such a game was a virtual reality simulation game, aimed at smoking cessation that involved finding and crushing virtual cigarettes. A study of the game showed that smokers in the group whose gameplay consisted of crushing virtual cigarettes had a statistically significant reduction in nicotine addiction over the group that grasped virtual balls.14 Although the results are promising, the dissemination of such a game is limited by the high cost of the virtual reality system that was used for the game.
The current study examines how a game that runs on an off-the-shelf gaming motion sensor, the Microsoft® (Redmond, WA) Kinect®, can be used in opioid addiction treatment by helping patients build drug refusal and avoidance skills, important skills to develop during treatment.15 Specifically, this study examines the initial use of a newly developed prototype of a body motion–activated game targeting opioid relapse prevention in the context of a community outpatient care program for youth addiction. Of interest was game acceptability,16 including participant satisfaction with the technical aspects of the game and interest in having the game integrated into treatment, as well as recommendations for improvement. Also of interest was whether the gameplay itself might lead to unintended cravings by exposing players to drug cues. Furthermore, to inform a larger trial, issues related to feasibility—including feasibility of recruitment, delivery of the intervention, and adherence to the intervention17—were examined.
Materials and Methods
Study procedures
The study was approved (protocol number 081319) by the George Washington University Institutional Review Board on September 27, 2013. Participants were recruited from the youth opioid outpatient group program at the Mountain Manor Treatment Center (MMTC) in Baltimore, MD. MMTC is a Joint Commission–accredited community treatment program for substance use disorders and co-occurring “dual diagnosis” substance use and mental health conditions. Typically, patients enter the outpatient program immediately after having undergone an episode of inpatient treatment for opioid addiction at MMTC.
Patients learned of the study through recruitment announcements made by counselors during weeknight opioid outpatient group sessions. Participants were recruited between November 18, 2013 and December 2, 2013. Interested individuals were assessed for eligibility and, if eligible, consented by research staff using a written consent form. To be eligible to participate, participants had to be at least 16 years of age, attending MMTC as an outpatient for opioid addiction treatment, and willing to attend a gameplay session.
Participants were given a $20 gift card for participating in each session for a maximum total of $80. Enrollment was limited to nine subjects in accordance with the U.S. Office of Management & Budget rules related to the contract funding this project. The study was based on research designs conducive to understanding implementation feasibility.16
Participants were asked to attend four weekly videogame group sessions, each 45 minutes in length. Sessions were held immediately before or after MMTC opioid outpatient group sessions on Monday, Tuesday, and Thursday evenings from 6:30 to 7:30 p.m. Sessions were offered in a room on campus provided by MMTC. Upon enrollment in the study, participants filled out a baseline survey. Each gameplay session consisted of a pregame survey (or baseline survey for the first session), gameplay, and a brief postgame survey. Gameplay was conducted in a group setting (typically three or four participants), and each participant was encouraged to play the game for 10 minutes and watch the other players when they were not playing. Phone calls, text messages, and subject interception at MMTC were used to remind participants of their upcoming research sessions.
Intervention
The relapse prevention motion videogame (“Recovery Warrior”) was developed for use with Microsoft's Kinect for Windows® (Microsoft) running on a Windows personal computer. The game was developed as an early-stage prototype of a game that would ultimately look, feel, and play like professional videogame software. The prototype has two distinct modes: “Recovery Ninja” (Fig. 1) and “Recovery Runner” (Fig. 2).
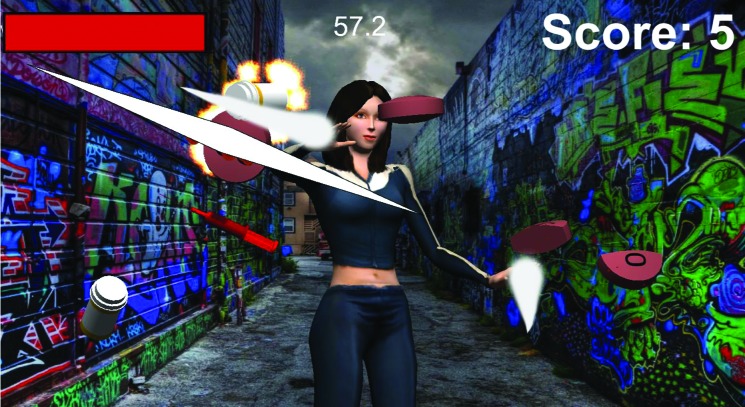
FIG. 1.
Screenshot from “Recovery Ninja.” (Color graphics available at www.liebertonline.com/g4h)
FIG. 2.
Screenshot from “Recovery Runner.” (Color graphics available at www.liebertonline.com/g4h)
The goal of “Recovery Ninja” is to destroy drugs that fly at the player's three-dimensional avatar. The player must make chopping, punching, and hitting gestures in order to destroy the drugs and win the game. “Recovery Runner” depicts the player's avatar running through a dark three-dimensional city, which progressively brightens as the player succeeds in staying away from drugs. Instead of destroying drugs (as in “Recovery Ninja”), the player must avoid them by physically ducking, dodging, and jumping to control the avatar's movements and avoid touching the drugs.
Both modes use whole-body motion and voice recognition features. Game strategy requires a variety of arm, leg, and whole-body movements to physically enact the motions of destroying or evading opioids. Voice features in both modes involve the player shouting refusal phrases, like “I'm Clean!,” in order to gain additional strength for their avatar. All game art was created in a hyper-realistic, idealized, and heroic style, the preferred style choice as determined in focus groups conducted prior to Phase I, and players are given a choice of several distinct hyper-realistic avatars with which to play. The prototype has only a single level of gameplay, with each game session lasting on average 3 minutes, although multiple levels and variants are anticipated in future versions to keep players engaged for longer periods of time.
Theoretical mechanism of “Recovery Warrior”
The development of the game was based on the Social Cognitive Theory, self-schemas, repetitive priming, and the Reinforcement Theory of Motivation.18,19 Based on Social Cognitive Theory, it is hypothesized that by repeatedly role-playing destroying drugs/avoiding drugs in the context of the game, players will experience increases in their self-efficacy and behavioral capability for drug refusal and avoidance in the real world.18 This may occur because players will develop self-schemas of themselves as drug destroyers or avoiders rather than users.20 These skills assist with behavioral response retraining so that destroying or avoiding drugs becomes a more automatic response, similar to work that has been done with retraining alcohol behaviors.21 Furthermore, drug refusal skills and self-schemas as nonusers will be further enhanced by the constant repetition of phrases like “I'm Clean!” throughout the game, so that participants will be primed to use it if offered drugs in a future situation.22
Additionally, based on Reinforcement Theory of Motivation, we hypothesize that youth will be better able to learn these skills, if the learning process is paired with rewards. In this case, rewards associated with playing videogames may include such positive feelings as a sense of mastery and eustress and, specific to the physical activity component of the game, from the release of endorphins from the game-based exercise and physical exertion.23,24 Finally, because this game is being designed as a social game to be played in the company of others in treatment, and eventually as a multiplayer game, it is also hypothesized that social learning will contribute to the mastery of refusal skills and drug avoidance.18 Participants will learn the skills of avoiding drugs/refusing drugs by not only repeatedly playing themselves, but by watching others practicing these skills in the context of the game.
Measures
Measures for this study were derived from the baseline survey and postgameplay surveys at each of the four sessions. The baseline survey included the collection of demographic and drug use history of participants, baseline craving levels, and self-efficacy for refusing drugs.
As a measure of acceptability, participants were asked to rate their satisfaction with the technical aspects of the game on the postgameplay survey. Participants rated their satisfaction on six aspects of the game on a 5-point Likert scale from “not at all satisfied” (= 1) to “very satisfied” (= 5). Satisfaction ratings included satisfaction with overall gameplay, the goal of the game, the game setting, the motion detection, the voice command, and the length of gameplay.
Also as a measure of acceptability,16 participants were asked to report each week on their level of interest in playing the game as part of treatment. Several items were assessed including whether participants would be more likely to attend outpatient sessions if the game was available (rated from “definitely not agree” [= 1] to “definitely agree” [= 5]), their interest in playing the game as part of treatment (rated from “not interested” [= 1] to “extremely interested” [= 5]), and whether they would recommend the game to others in treatment (rated from “not recommend at all” [= 1] to “strongly recommend” [= 5]). In addition, on the final week (Week 4) postgame survey, participants were also asked about their recommendations for integration of gameplay into treatment, including their recommendations for the ideal number of sessions, social context of play, length of play, and stage in recovery when the game would be used.
Although the primary aim of the study was focused on acceptability, secondary outcomes included the preliminary testing of the game on changes in self-efficacy refusal skills, craving levels, and abstinence. For self-efficacy for refusal, the Marijuana Resistance Self-Efficacy scale25,26 was included on the baseline and follow-up surveys and adapted for opiate use to assess participant self-efficacy in ability to refuse offers of opioids and to resist opiate use in a variety of scenarios. It used a four-item, 4-point scale (from 1=very easy to 4=very hard) that asked how easy or hard it would be to refuse opioids if offered, explain why you didn't want it, to avoid the situation in the first place, and to leave the situation. For cravings, the five-item Penn Alcohol Craving Scale (PACS)27 was included on the baseline and follow-up postgame surveys, but altered to apply to opioid use and used to assess the intensity of a participant's cravings (from 0=none at all to 6=very strong and summed for a total of 30 points). Abstinence was measured using urine analysis at 4 weeks postbaseline. For participants who did not have a urine test at 4 weeks, the next test result was used within an 8-week time frame. Participants who did not take a urine test were counted as having a positive test result.
Because gameplay involved the viewing of hyper-realistic depictions of drugs, there was concern that the game could unintentionally increase cravings for drug use during or following gameplay. Therefore in addition to the PACS, which measured general cravings, an item of the postgame survey measured recall of cravings during gameplay. Participants rated their levels of craving during gameplay on a scale from “none at all” (= 1) to “strong urge” (= 7).
Results
Participation in group play
Nine participants were recruited from a total of 24 patients in MMTC's outpatient opioid clinic and enrolled in the study. Participation in group play declined each week, and by Week 4, only six of the nine participants (66.9 percent) were present for the treatment session. Participants present at Week 4 attended all four videogame sessions; one (11.1 percent) attended two sessions, and two (22.2 percent) attended only one session. There were no significant demographic differences between the participants who attended all sessions and those who dropped out when conducting Fisher's exact test on all variables listed in Table 1. Furthermore, the craving score for the sample that completed all sessions was similar to the craving score for those who dropped out (12.67 [standard deviation (SD)=8.37] versus 11.67 [SD=7.10]), respectively.
Table 1.
Demographics Characteristics and Drug Use History
| Full sample (n=9) | Completers of 4 weeks (n=6) | Dropouts (n=3) | |
|---|---|---|---|
| Age (years) | |||
| <18 | 0 (0.00) | 0 (0.00) | 0 (0.00) |
| 18–20 | 5 (55.56) | 4 (66.67) | 1 (33.33) |
| 21–23 | 3 (33.33) | 1 (16.67) | 2 (66.67) |
| 24 | 1 (11.11) | 1 (16.67) | 0 (0.00) |
| Grade | |||
| 12th grade | 2 (22.22) | 1 (16.67) | 1 (33.33) |
| College | 2 (22.22) | 1 (16.67) | 1 (33.33) |
| Not in school | 5 (55.56) | 4 (66.67) | 1 (33.33) |
| Gender | |||
| Male | 8 (88.89) | 5 (83.33) | 3 (100.00) |
| Female | 1 (11.11) | 1 (16.67) | 0 (0.00) |
| Race/ethnicity | |||
| White | 6 (66.67) | 4 (66.67) | 2 (66.67) |
| Black or African American | 3 (33.33) | 2 (33.33) | 1 (33.33) |
| Other | 0 (0.00) | 0 (0.00) | 0 (0.00) |
| Mother's education | |||
| Didn't graduate | 1 (11.11) | 1 (16.67) | 0 (0.00) |
| HS graduate/GED | 2 (22.22) | 2 (33.33) | 0 (0.00) |
| College or higher | 5 (55.56) | 2 (33.33) | 3 (100.0) |
| No response | 1 (11.11) | 1 (16.67) | 0 (0.00) |
| Father's education | |||
| Didn't graduate | 0 (8.3) | 0 (0.00) | 0 (0.00) |
| HS graduate/GED | 4 (44.44) | 2 (33.33) | 0 (0.00) |
| College or higher | 1 (55.56) | 1 (16.67) | 3 (100.0) |
| No response | 4 (44.44) | 3 (50.00) | 0 (0.00) |
| Drugs treated fora | |||
| All opioids | 9 (100.0) | 5 (55.56) | 0 (0.00) |
| Heroin | 6 (66.67) | 4 (44.44) | 2 (33.33) |
| Percocet (oxycodone/acetaminophen) | 2 (13.33) | 1 (11.11) | 1 (16.67) |
| Other/more than one | 1 (25) | 0 (0.00) | 1 (16.67) |
| Cocaine | 1 (11.11) | 0 (0.00) | 1(16.67) |
| Ecstasy | 2 (22.22) | 2 (22.22) | 0 (0.00) |
| Benzodiazepine | 1 (11.11) | 1 (11.11) | 0 (0.00) |
| Cannabis | 2 (22.22) | 1 (11.11) | 1 (16.67) |
| Used in the past 7 days | |||
| No | 9 (100.0) | 6 (46.15) | 3 (23.08) |
| Yes | 0 (0.00) | 0 (0.00) | 0 (0.00) |
| Date last used | |||
| <1 month | 4 (44.44) | 4 (44.44) | 1 (33.33) |
| 1–2 months | 4 (44.44) | 4 (44.44) | 2 (66.67) |
| >2 months | 1 (11.11) | 1 (11.11) | 0 (0.00) |
Data are number (percentage) values.
Open-response question so categories are not mutually exclusive.
HS, high school.
Characteristics of participants
On average, participants were 20.6 years old (range, 18–24 years). Half of the participants were not attending school at the time of the study (55.6 percent), whereas 22.2 percent were in 12th grade, and the other 22.2 percent were taking college classes. The majority of participants were males (88.9 percent). All participants identified themselves as white (66.7 percent) or black (33.3 percent). Most had a mother and father who had finished college (55.6 percent for both) or high school/GED (22.2 percent, 44.4 percent respectively) (Table 1).
All participants were in treatment for opioid addiction. Participants reported being in treatment for use of heroin (66.7 percent), acetaminophen and oxycodone (Percocet®; Endo Pharmaceuticals, Malvern, PA) (13.3 percent), and other or more than one opioid (25.0 percent). At baseline, all participants reported not having used opioids in the last 7 days. Four (44.4 percent) reported last using within the last month, 4 (44.4 percent) reported last using 1–2 months ago, and one reported last using more than 2 months ago (11.1 percent). In addition to opioid use, participants reported using cocaine (11.1 percent), ecstasy (22.2 percent), benzodiazepine (11.1 percent), and cannabis (22.2 percent).
All individuals who dropped out were males, between 18 and 23 years of age, spread across educational categories and racial/ethnic groups, had college-educated parents, and were users of heroin, cocaine, Percocet, and other opioids. None of the individuals who dropped out had used in the past week, but all had last used in the past 2 months.
Satisfaction with gameplay
Participants expressed a high level of satisfaction with the technical aspects of the videogame following gameplay at Week 1 (mean=4.7; SD=0.50) and satisfaction was maintained over the remaining weeks of gameplay. At Week 1, participants were satisfied with the goal of the game (mean=4.8; SD=0.44), the setting of the game (mean=4.6; SD=0.53), and the length of gameplay (mean=4.6; SD=0.53). They were also satisfied with the motion detection feature (mean=4.2; SD=0.83) and the voice command feature using refusal language (mean=4.22; SD=0.97) (Table 2).
Table 2.
Satisfaction with Gameplay
| Week 1 (n=9) | Week 2 (n=7) | Week 3 (n=6) | Week 4 (n=6) | |
|---|---|---|---|---|
| Average satisfaction with gameplay | ||||
| Overall gameplaya | 4.67 (0.50) | 4.71 (0.49) | 4.83 (0.41) | 4.50 (0.84) |
| The goal of the gamea | 4.78 (0.44) | 4.71 (0.49) | 4.83 (0.41) | 4.67 (0.82) |
| The game settinga | 4.56 (0.53) | N/A | ||
| The motion detectiona | 4.22 (0.83) | N/A | ||
| The voice command “I'm Clean”a | 4.22 (0.97) | 1.14 (1.07) | 4.33 (1.03) | 4.17 (0.98) |
| The length of gameplaya | 4.56 (0.53) | 4.00 (0.82) | 4.67 (0.52) | 4.50 (0.84) |
| Interest in treatment with games | ||||
| More likely to make it to treatment if game was availableb | 4.56 (0.73) | 4.86 (0.38) | 4.83 (0.41) | 4.67 (0.52) |
| Less resistant going to treatment knowing that the game was there to playb | 4.00 (0.50) | 4.43 (0.53) | 4.17 (1.17) | 4.50 (0.84) |
| Interest in playing this videogame as part of treatment planc | 4.56 (0.73) | 3.71 (1.21) | 4.83 (0.41) | 4.50 (0.84) |
| Likelihood of recommending this game to other people in treatmentd | 4.22 (0.83) | 4.00 (1.41) | 3.83 (1.60) | 3.67 (1.51) |
| Craving level | ||||
| Strength of craving during gameplaye | 1.78 (1.30) | 1.86 (0.90) | 3.00 (1.79) | 1.50 (0.55) |
Data are mean (standard deviation) values.
Rated on a scale from not at all satisfied (1) to very satisfied (5).
Rated on a scale from definitely not agree (1) to definitely agree (5).
Rated on a scale from not interested (1) to extremely interested (5).
Rated on a scale from not recommend at all (1) to strongly recommend (5).
Rated on a scale from none at all (1) to strong urge and would have used if available (7).
NA, not applicable.
At Week 1, participants reported on their satisfaction with the game in the context of their treatment. They had a high level of agreement that if video gameplay were offered as part of their treatment, they would be more likely to make it to more treatment sessions (mean=4.6; SD=0.73). They also agreed that they would be less resistant to going to treatment knowing that the videogame was there for them to play (mean=4.0; SD=0.50), they would be interested in playing the videogame as part of treatment (mean=4.6; SD=0.73), and they would recommend the videogame to other people in treatment (mean=4.2; SD=0.83). Satisfaction was sustained for most variables throughout the 4 weeks with the exception of the likelihood of recommending the game to a friend, which declined from 4.2 to 3.7 by Week 4. Participants did not feel that playing the videogame led to strong cravings to use drugs. Participants reported at Weeks 1 and 4 low levels of urge to use during gameplay (1.8 at Week 1; 1.5 at Week 4).
Participants were also asked at Week 1 to share what they liked and disliked about the game in an open-ended format. Participants reported liking the videogame because they learned specific game techniques, felt it helped them stay clean, enjoyed gameplay, used physical movement to gain points, and liked everything about the game. The most commonly reported reason for not liking the videogame had to do with technical problems, followed by it being too easy.
Structural integration into treatment
At the Week 4 session, participants were surveyed about specific suggestions for the structural integration of gameplay into treatment. All participants recommended playing the videogame as part of treatment at least one time each week, with a third (33.3 percent) recommending playing daily. Participants had different ideas on the social context in which the videogame should be played: two-thirds (66.7 percent) thought it should be played individually with others watching, multiplayer with other watching (33.3 percent), and/or individually in a private room (33.3 percent). The majority of participants (83.3 percent) wanted each gameplay session to last for more than 15 minutes, and all believed that the videogame should be introduced to patients within the first month of entering the treatment program (Table 3).
Table 3.
Recommendations for Integration of Gameplay in Treatment (n=6) Measured at Week 4
| n (percentage) | |
|---|---|
| Recommended number of gameplay sessionsa | |
| 1 time a day | 2 (33.33) |
| 2 times a day | 0 (0.00) |
| 3–4 times a week | 2 (33.33) |
| 1 time a week | 2 (33.33) |
| 1 time a month | 0 (0.00) |
| Recommendations for social context of playa | |
| Individually in a private room | 2 (33.33) |
| Individually with others watching | 4 (66.67) |
| Multiplayer with others watching | 2 (33.33) |
| Recommended length of play | |
| <15 minutes | 1(16.67) |
| 16–30 minutes | 2 (33.33) |
| 31–45 minutes | 1 (16.67) |
| 46–60 minutes | 1 (16.67) |
| >61 minutes | 1 (16.67) |
| Recommended inclusion in stage of recovery | |
| Within the first week of entering treatment | 2 (33.33) |
| Within the first month of entering treatment | 4 (66.67) |
| After the first month of treatment | 0 (0.00) |
Data are number (percentage) values.
Open-response question so categories are not mutually exclusive.
Recovery-related outcomes
Over the 4-week period of gameplay, self-efficacy to refuse opioids remained constant. At baseline and follow-up, participants reported having a mean self-efficacy score of 2.1, where 1 was “very easy” to resist and 4 was “very hard” (Table 4). For cravings, participants reported a decreased craving level at Week 4 (mean=9.8; SD=8.3) compared with baseline (mean=12.7; SD=8.4), a decline of 2.4 points on the PACS scale; however, this decrease was not significant. Based on the urine analysis, four out of nine (44.4 percent) participants remained abstinent by the conclusion of the study.
Table 4.
Changes in Average Craving Levels (from Week 1 to Week 4)
| Week 1 (n=9) | Week 4 (n=6) | Change | |
|---|---|---|---|
| Craving levelsa | 12.7 (8.4) | 9.8 (8.3) | −2.4 |
| If someone you know offered you opioids, how easy would it be for you…b | 2.14 (1.1) | 2.14 (1.3)c | 0.0 |
| • To refuse it? | |||
| • To explain why you didn't want it? | |||
| • To avoid the situation in the first place? | |||
| • To just leave the situation? |
Discussion
This study represents the first known study of a body motion–activated game targeting opioid relapse prevention. Initial results for the game's acceptability are encouraging as participants rated highly the technical aspects of the game and the option for its integration into treatment. The majority of participants envisioned a treatment scenario where gameplay would occur once a week or more in a group setting with others watching within the first month of outpatient treatment.
Despite participant reports of high acceptability of the game, problems were encountered in keeping participants engaged in treatment throughout the 4-week period, as three of the nine participants did not attend the final group play sessions. This may indicate that although the game has some positive features, these may be insufficient to increase attendance in treatment. Although low participation may be due to factors exogenous to the game, such as factors that limited participants' ability to attend regularly scheduled outpatient care that preceded gameplay sessions or ability to stay at MMTC for additional time following outpatient treatment for game sessions, these factors nonetheless indicate that attendance is likely to be an issue that may affect the success of the game.
Concerns about the game triggering drug cravings were not substantiated as participants reported low levels of cravings following gameplay, and craving declined over the study period; however, this decrease was not significant. This might relate to the hyper-realistic animation style or other features used in the game or to the context provided by delivering the game within treatment. These results should be explored further in future studies that include a control group and a larger sample size.
Although not a primary outcome of the study, the gameplay did not appear to increase levels of self-efficacy for drug refusal as self-efficacy remained constant throughout the study period. It may be that the game does not operate as hypothesized through self-efficacy; however, a larger sample and a control group are needed to confirm these preliminary data. Additional measures are also required to understand the effects of the game on priming and self-schemas of drug use. In this pilot, no measures were included to examine changes in self-schemas as a result of gameplay.20
The version of the game presented to the youth was an early prototype version with simplified features and few levels of gameplay. Some participants reported technical problems with the game and that the gameplay was too easy. To address these concerns, the prototype now uses improved motion sensing and a wider range of difficulty modes with greater level progression.
Strengths of this study include that it was the first study of a videogame aimed at the treatment of opioid addiction. The game was built around an affordable off-the shelf motion-sensing peripheral that is widely used by youth, the Microsoft Kinect, which is most famous for its use with Microsoft's popular Xbox® videogame platform. The potential for dissemination is high, with possibility for play not only in treatment centers and to incentivize attendance but also potentially for play at home. Limitations include that the study experienced some loss to follow-up as a third of participants dropped out of treatment during the follow-up period and were not available to complete the study's four sessions of gameplay. Although this is a high level of attrition and was likely aggravated by winter weather closings and that the study period spanned the December–January holidays, this level of attrition is not unusual for youth attending outpatient drug treatment facilities. The high attrition rate will need to be better explored in future studies to help ensure that gameplay did not deter attendance. Furthermore, the study design was limited in that it is not possible to separate outcomes attributable to the game versus other treatment factors. Future, larger-scale studies will use a control group to better measure differences that may be more specifically attributable to gameplay. Additionally, the study did not use a fixed game, as the game was being revised and improved during the formative evaluation. As a result, participants did not play the exact same version of the videogame from week to week.
These results suggest that a motion videogame for addiction recovery is acceptable to youth within the context of outpatient treatment for opioid addiction; however, this small-scale pilot study cannot directly measure the impact on recovery. Although difficulties were encountered related to participant attendance, overall the results are encouraging for the next stages of game development and testing. Future studies are needed to assess the impact of the game on abstinence and further understand the mechanisms of action and how they affect overall recovery.
Acknowledgments
The authors would like to thank the counseling staff at MMTC, including Dr. Hoa Vo and Adamma Anumba, for their help with recruitment for and conduct of the study. This study was supported by contract HHSN271201300006C under grant N43DA-13-4419 (SBIR Topic #150) from the National Institute of Drug Abuse to Media Rez LLC (Principal Investigator D.G.).
Author Disclosure Statement
D.G. is the President of Media Rez LLC. Media Rez is planning to sell “Recovery Warrior” as a commercial venture. L.C.A. has the potential to benefit financially from the sale of “Recovery Warrior.” M.J.F. is the Medical Director of MMTC, where patients were enrolled in this study, and a part-time faculty member of the Johns Hopkins University. He is a beneficiary of the trust that owns MMTC. M.J.F. also serves on the governing board of the trust and the Board of Directors of MMTC. This arrangement has been reviewed and approved by the Johns Hopkins University in accordance with its conflict of interest policies. L.E.L., J.M.V.A., and J.M.S.-R. declare no competing financial interests exist.
References
- 1.Substance Abuse and Mental Health Services Administration. Results from the 2012 National Survey on Drug Use and Health: Summary of National Findings. NSDUH Series H-46. HHS Publication (SMA) 13-4795. Rockville, MD: Substance Abuse and Mental Health Services Administration; 2013 [Google Scholar]
- 2.Substance Abuse and Mental Health Services Administration. Table 5.1a. Admissions Aged 12–17 by Primary Substance of Abuse: TEDS 1995–2005. http://wwwdasis.samhsa.gov/teds05/TEDSAd2k5Tbl5.1a.htm (accessed July7, 2015)
- 3.Subramaniam GA, Stitzer MA. Clinical characteristics of treatment-seeking prescription opioid vs. heroin-using adolescents with opioid use disorder. Drug Alcohol Dep 2009; 101:13–19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Subramaniam G, Fishman M, Woody G. Treatment of opioid-dependent adolescents and young adults with buprenorphine. Curr Psychiatry Rep 2009; 11:360–363 [DOI] [PubMed] [Google Scholar]
- 5.Woody GE, Poole SA, Subramaniam G, et al. Extended vs short-term buprenorphine-naloxone for treatment of opioid-addicted youth: A randomized trial. JAMA 2008; 300:2003–2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Marsch LA, Bickel WK, Badger GJ, et al. Comparison of pharmacological treatments for opioid-dependent adolescents: A randomized controlled trial. Arch Gen Psychiatry 2005; 62:1157–1164 [DOI] [PubMed] [Google Scholar]
- 7.Fishman M, Curran E, Shah S, et al. Treatment outcomes with relapse prevention medications for opioid dependence in youth. Poster presented at the College on Problems of Drug Dependence Annual Meeting, Boca Raton, FL, June22, 2011 [Google Scholar]
- 8.Minozzi S, Amato L, Bellisario C, Davoli M. Maintenance treatments for opiate dependent adolescents. Cochrane Database Syst Rev 2014; 6:CD007210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fishman M, Winstanley E, Curran E, et al. Treatment of opioid dependence in adolescents and young adults with extended release naltrexone: Preliminary case series and feasibility. Addiction 2010; 105:1669–1676 [DOI] [PubMed] [Google Scholar]
- 10.Lenhart A, Jones S, Macgill A. Pew Research Internet Project: Adults and Video Games. 2008. www.pewinternet.org/2008/12/07/adults-and-video-games/ (accessed July7, 2015)
- 11.Clark L. Wham, sock, kapow! Can Batman defeat his biggest foe yet and combat mental health discrimination? An exploration of the video games industry and its potential for health promotion. J Psychiatr Ment Health Nurs 2013; 20:752–760 [DOI] [PubMed] [Google Scholar]
- 12.LeBlanc AG, Chaput JP, McFarlane A, et al. Active video games and health indicators in children and youth: A systematic review. PLoS One 2013; 8:e65351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Primack BA. Carroll MV, McNamara M, et al. Role of video games in improving health-related outcomes: A systematic review. Am J Prev Med 2012; 42:630–638 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Girard B, Turcotte V, Bouchard S, Girard B. Crushing virtual cigarettes reduces tobacco addiction and treatment discontinuation. Cyberpsychol Behav 2009; 12:477–483 [DOI] [PubMed] [Google Scholar]
- 15.Skinner ML, Haggerty KP, Fleming CB, et al. Opiate-addicted parents in methadone treatment: Long-term recovery, health, and family relationships. J Addict Dis 2010; 30:17–26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bowen DJ, Kreuter M, Spring B, et al. How we design feasibility studies. Am J Prev Med 2009; 36:452–457 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Leon AC, Davis LL, Kraemer HC. The role and interpretation of pilot studies in clinical research. J Psychiatr Res 2011; 45:626–629 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bandura A. Social cognitive theory of mass communications. In: Bryant J, Oliver MB, eds. Media Effects: Advances in Theory and Research, 2nd ed. Mahwah, NJ: Lawrence Erlbaum; 2009: pp. 94–124 [Google Scholar]
- 19.Skinner BF. The operant side of behavior therapy. J Behav Ther Exp Psychiatry 1988; 19:171–179 [DOI] [PubMed] [Google Scholar]
- 20.Sheeran P, Orbell S. Self-schemas and the theory of planned behaviour. Eur J Soc Psychol 2000; 30:533–550 [Google Scholar]
- 21.Wiers RW, Rinck M, Kordts R, et al. Retraining automatic action-tendencies to approach alcohol in hazardous drinkers. Addiction 2010; 105:279–287 [DOI] [PubMed] [Google Scholar]
- 22.Grill-Spector K, Henson R, Martin A. Repetition and the brain: Neural models of stimulus-specific effects. Trends Cogn Sci 2006; 10:14–23 [DOI] [PubMed] [Google Scholar]
- 23.Lieberman DA. Digital games for health behavior change: Research, design, and future directions. In: Noar SM, Harrington NG, eds. Routledge Communication Series: eHealth Applications: Promising Strategies for Behavior Change. New York: Routledge; 2012: pp. 110–127 [Google Scholar]
- 24.Noar SM, Harrington NG, eds. Routledge Communication Series: eHealth Applications: Promising Strategies for Behavior Change. New York: Routledge; 2012 [Google Scholar]
- 25.Hecht ML, Miller-Day M. The Drug Resistance Strategies Project: Using narrative theory to enhance adolescents' communication competence. In: Frey L, Cissna K, eds. Routledge Handbook of Applied Communication. New York: Routledge; 2009: pp. 535–557 [Google Scholar]
- 26.Pettigrew J, Miller-Day M, Hecht ML, Krieger J. Alcohol and other drug resistance strategies employed by rural adolescents. J Appl Commun Res 2011; 39:103–122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Flannery BA, Volpicelli JR, Pettinati HM. Psychometric properties of the Penn Alcohol Craving Scale. Alcohol Clin Exp Res 1999; 23:1289–1295 [PubMed] [Google Scholar]