Abstract
Background and Purpose
This case report describes a physical therapist's use of diagnostic ultrasound imaging in the decision making process used to refer a patient to a physician for a suspected fibular stress fracture. The purpose of this case report is to 1) describe the history, subjective examination, and objective examination findings of a fibular stress fracture, 2) describe the ultrasound findings associated with a fibular stress fracture, and 3) describe the decision making process of a physical therapist in the decision to refer the patient to a medical physician for further work‐up.
Case Description
A 52‐year‐old female recreational runner with a recent increase in running intensity self‐referred to a physical therapist with a 19‐day history of lateral lower leg pain. Examination revealed relatively normal ankle range of motion, mild weakness of ankle invertors and evertors, no increase in pain with resisted muscle tests of the ankle, and tenderness to palpation over the fibularis brevis muscle and distal fibula. Diagnostic ultrasound examination of the fibularis muscles revealed cortical irregularity of the distal third of the fibula in the location of tenderness.
Outcomes
The physical therapist used the abnormal ultrasound findings, running history, symptoms, and physical examination for differential diagnosis, and decided to refer the patient to a physician for further examination. Radiographs revealed a fibular stress fracture. Follow‐up ultrasound imaging demonstrated a mixed hypoechoic‐hyperechoic appearance of the fibular cortex typical of healing fracture and the presence of bony callus.
Discussion
Diagnostic ultrasound imaging is increasingly being used by physical therapists to guide rehabilitation. Ultrasound imaging of musculotendinous structures may display adjacent bone. Physical therapists should be knowledgeable of normal and abnormal bony ultrasound imaging findings. Abnormal ultrasound findings may be one sign indicating the need to refer a patient for consultation by a physician.
Keywords: Differential diagnosis, musculoskeletal ultrasound, running, stress fracture
BACKGROUND AND PURPOSE
Stress fractures are common injuries in runners, athletes, and military recruits due to repeated mechanical loading experienced during activities such as running and marching.1-8 Excessive repetitive submaximal loading of normal bone without sufficient rest time results in greater osteoclastic than osteoblastic activity of the loaded bone.9,10 This excessive stress on normal bone leads to the development of microfractures, which is known as a stress reaction.9 If repeated submaximal loading continues without sufficient rest, the bone stress reaction may progress to a stress fracture, a fracture of the bone cortex.9,10 The reported incidence of stress fractures in athletes varies according to sport; however, track and field athletes have been reported to have the highest incidence rates of lower extremity (LE) stress fractures.11 Incidence of LE stress fractures among competitive track and field athletes may be as high as 20%.11,12 Incidence of LE stress fractures among recreational and competitive runners was reported to be 8.3% in males and 13.2% in females.13 The bones with the greatest incidence of stress fractures include the tibia, metatarsal, fibula, tarsal, femur, and pubic bones.2,3,7,10,11,14,15 The incidence of fibular stress fractures in athletes and military recruits is reported to range from 3.5% ‐ 29.6%, depending on the population.2-4,7,10,11,14,16 In a recent literature review, Kahanov and colleagues16 reported the proportion of fibular stress fractures among runners to be 7% ‐ 12% of all stress fractures; however, the proportion may be as high as 33% and 20% of stress fractures in female and male distance runners, respectively.11
Risk factors for stress fractures can be classified as extrinsic or intrinsic.17 Extrinsic risk factors are causes that exist external to the individual affecting his or her risk of developing a condition, e.g., participation in activities or environmental features.17 Intrinsic risk factors are features that exist within the individual that impact his or her likelihood of contracting a condition, e.g., gender or biomechanics.17 Reported extrinsic risk factors for stress fractures include participation in running sports, military recruits’ participation in basic training, increased training intensity (speed or duration/number of training sessions), and participation in recreational running more than 25 miles per week.1,17 Intrinsic risk factors for stress fractures are reported to include female gender, amenorrhea, reduced caloric intake, reduced physical fitness, decreased bone mass, and previous history of stress fracture.1,17-19 In a recent meta‐analysis, Wright and colleagues18 reported that the two strongest risk factors for a LE stress fracture in runners are a history of a stress fracture (odds ratio [OR] 4.99; 95% confidence interval [CI] 2.91 to 8.56; p<0.001) and female gender (OR 2.31; 95% CI 1.24 to 4.29; p=0.008).
Diagnosis of stress fractures requires a careful review of an individual's activity including current and past exercise regimens.9 The history may reveal a recent change in exercise/training such as increased intensity or alteration in terrain.1,9 There is a high incidence of recurrence of stress fractures,18,20,21 thus, a history of previous musculoskeletal injuries should be explored.1,22 Pain may be constant or intermittent, depending on the severity of the fracture.1 Physical examination may reveal point tenderness on bones which are accessible to palpation.3,9 Active and passive joint movement may be painful if the fracture is close to a joint.3 Resistive muscle tests may be painful if the tested muscle is attached to the portion of bone with the stress fracture or if resistance causes movement of the fracture site.3 Soft tissue swelling and warmth may be present.9,19 However, tenderness to palpation, appreciable swelling, and palpable warmth may not be apparent in bones with extensive overlying soft tissue or for stress fractures that are less severe.3,15 Stress fractures in LE bones cause pain in stressful weight‐bearing activities such as running.2,15 More severe LE stress fractures may provoke pain during less stressful weight‐bearing, for example during walking.1,15,19 Stress fractures of the fibula are most common in its distal third and cause pain in the lateral distal third of the lower leg.2,15 Additional pathologies that may cause pain in this location include fibularis muscle strain or tendinopathy (particularly fibularis brevis) and lateral ankle ligament sprain.1
Ultrasound imaging (USI) has been used to examine musculoskeletal tissues,23-25 including diagnosis of fractures.26-29 Behrens and colleagues2 suggested that USI could be useful to diagnose stress fractures since it is non‐invasive and relatively easy to perform. The sensitivity and specificity of USI for diagnosis of early metatarsal stress fractures in persons with normal radiographs was reported to be 83% and 76%, respectively.30 Physical therapists (PTs) currently use USI to examine muscle, tendon, and other soft tissues to determine optimal rehabilitation strategies.24,25,31 Since USI may reveal bony changes consistent with fractures, PTs should be knowledgeable in USI findings for stress fractures. If present, these examination results may be signs used by the clinician in the decision to refer a patient to a medical physician. The purpose of this case report is to 1) describe the history, subjective examination, and objective examination findings of a fibular stress fracture, 2) describe the USI findings associated with a fibular stress fracture, and 3) describe the decision making process of a PT in the decision to refer the patient to a medical physician for further work‐up.
CASE DESCRIPTION: HISTORY AND SYSTEMS REVIEW
The subject was a 52‐year‐old female who participated in a “couch‐to‐5K” running training program. She self‐referred to a PT with a chief complaint of constant right lateral ankle pain that prevented her from participating in recreational running. The subject reported that she first felt mild pain towards the end of a 20‐minute run 19 days prior. The pain did not prevent her from finishing the run, was initially mild in intensity, and abated with completion of the run. But symptoms returned and became severe following her participation in a 5 kilometer (5K) run nine days prior to her physical therapy examination. She reported that the pain was severe and she was not able to tolerate normal weight‐bearing on the right LE during running. However, she continued to run and completed the 5K despite the pain. Although the pain had decreased in intensity since the 5K, the subject reported that she was concerned because it was still constant despite cessation of running.
The subject's chief complaint at the time of initial examination was constant right LE pain, localized posterior to the distal third of the fibula. Numeric pain rating was reported to be 2‐8 on a verbal scale of 0‐10 (10 = worst pain). The pain was worsened by weight‐bearing and palpation; pain was relieved by remaining non‐weight‐bearing. The subject's goals for physical therapy were to be able to return to running for fitness.
The subject's medical history was unremarkable related to LE injury. Prior to participation in the couch‐to‐5K program, she reported exercising at a fitness center two to three times per week including weight training and cardiopulmonary activities (elliptical or treadmill running). This included treadmill walk‐run interval training for 20‐30 minutes at approximately 3.0 ‐ 5.0 miles/hour for distances of 1.5 – 2.5 miles. The subject reported that she tried to alternate weeks of treadmill training and elliptical training for 20 – 30 minutes per session. Her weight training included use of exercise machines for LE and lower back strengthening, free weights for upper extremity resistance exercise, and planks and therapeutic exercise ball exercises for abdominal and back exercise. She reported no previous injuries from running or exercising. Medications included only a daily multivitamin.
CLINICAL IMPRESSION #1
The subject's primary problem was an inability to run and difficulty with full weight‐bearing on the right LE during ambulation due to moderately severe lateral lower leg/ankle pain. Given the location of symptoms and running as the mechanism of injury, the differential diagnosis list included fibularis muscle strain/tendinopathy and fibular stress fracture. The plan for the examination included a focused exam of the right LE including the selective tissue tension tests, palpation, and USI examination of the musculotendinous tissues. The PT was an experienced clinical researcher with five years of experience using USI for examination of degenerative and traumatic conditions of the Achilles tendon, gastroc‐soleus muscle group, plantar fascia, and other musculotendinous structures of the LE.
EXAMINATION
Physical examination began by observing the subject's gait while ambulating to the examination room. She ambulated without an assistive device with decreased stance time on the right LE, decreased left step length, a reduced heel rise at right terminal stance, and slow gait speed. Observation revealed a mild hallux abductovalgus deformity on the right foot. Non‐pitting edema at the right lateral distal lower leg and proximal lateral foot was present along with mild warmth to palpation. Right ankle active and passive motion did not alter symptoms and were nearly equal to the left ankle (plantarflexion, dorsiflexion, inversion, and eversion). Resisted tests of right ankle inversion and eversion were painless and 4+/5 strength on manual muscle testing, compared to 5/5 for the left LE. Sensation was intact to light touch in both distal LE. There was tenderness to palpation over the right fibularis brevis muscle posterior to the fibula and on the fibula approximately 6 cm proximal to the inferior border of the lateral malleolus. A firm enlargement over the fibula was palpable at the location of tenderness.
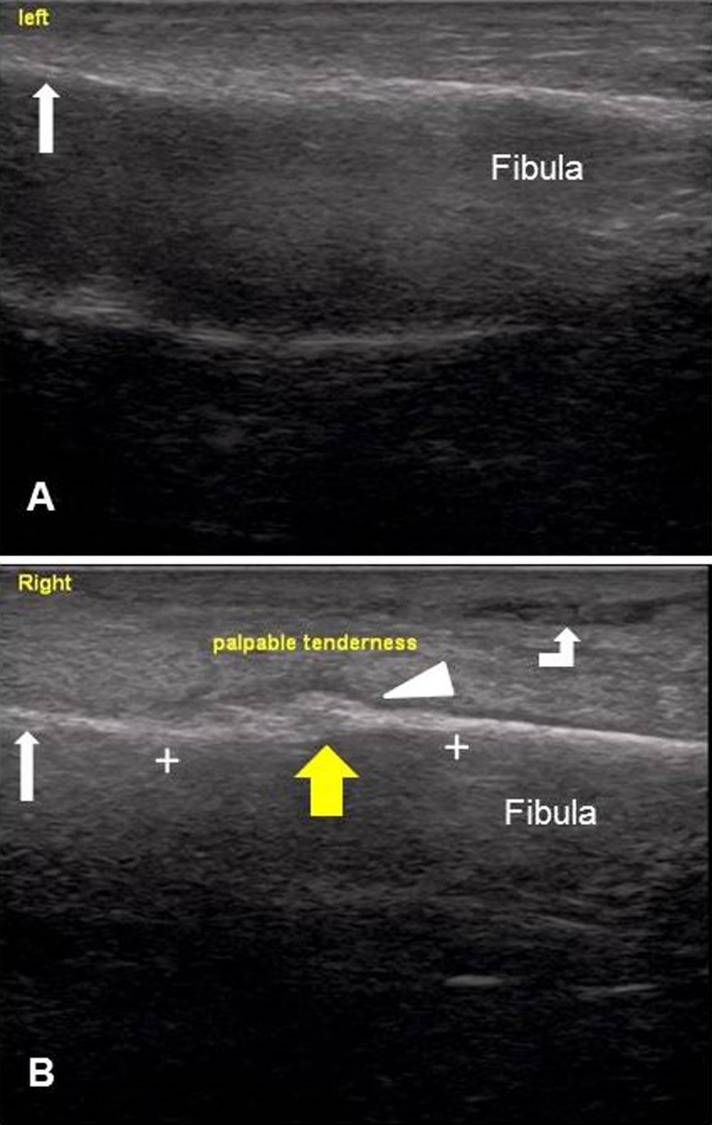
The PT performed an examination of the fibularis brevis muscle in the area of tenderness with comparison to the contralateral fibularis brevis muscle in order to determine if changes in muscle architecture were present. Longitudinal USI images of the distal fibulae and surrounding tissues were taken with a LOGIQR e USI system with a 7.5 MHz, 38 millimeter linear‐array probe (GE Healthcare, Wauwatosa, WI, USA). The USI settings were B mode, 10 MHz, depth 3.5 cm, image width 3.84 cm. Images were captured over the area of tenderness to palpation of the right distal fibula, approximately 4 cm – 8 cm superior to the inferior border of the lateral malleolus. This revealed an alteration of the normal contour of the right distal fibula at the location of tenderness (Figure 1). A 1.90 cm long hypoechoic area was visible overlying the normal hyperechoic surface of the bony cortex.
Figure 1.
Longitudinal ultrasound images of the distal fibulae, taken 19 days following symptom onset. (A) Distal left fibula approximately 4 cm ‐ 8 cm superior to the lateral malleolus; malleolus on the left (white arrow). The bony cortex is visible as a horizontal hyperechoic line. (B) Distal right fibula approximately 4 cm ‐ 8 cm superior to the lateral malleolus; malleolus on the left (white arrow). A 1.90 cm long area of apparent periosteal thickening (wide yellow arrow) visible as a hypoechoic area (white arrowhead) overlying the hyperechoic bony cortex (between the white crosses). Inflammation in the soft tissues is visible as hypoechoic areas in the overlying soft tissue (bent arrow).
CLINICAL IMPRESSION #2
The initial impression of severe strain of the fibularis brevis muscle was ruled out by the lack of alteration of symptoms by active ankle motion, the strong, painless result from resisted tests of the ankle evertors, and the apparently normal results for USI assessment of the fibularis brevis musculotendinous unit.32,33 The findings of point tenderness of the distal fibula, warmth, edema, constant pain, increased pain with weight‐bearing, history of recently increased duration and frequency of running activity, and apparent unusual contour of the fibula on USI examination made the PT suspect a possible fibular stress fracture.1,15,19,34 The PT instructed the subject to contact a medical physician for further work‐up. Use of crutches for ambulation non‐weight‐bearing on the right LE was recommended; however, the subject declined. She reported that she had a straight cane and that she would use that to decrease weight‐bearing on the right LE. It was also recommended that she minimize ambulation and refrain from running until she was examined by a medical physician.
OUTCOME
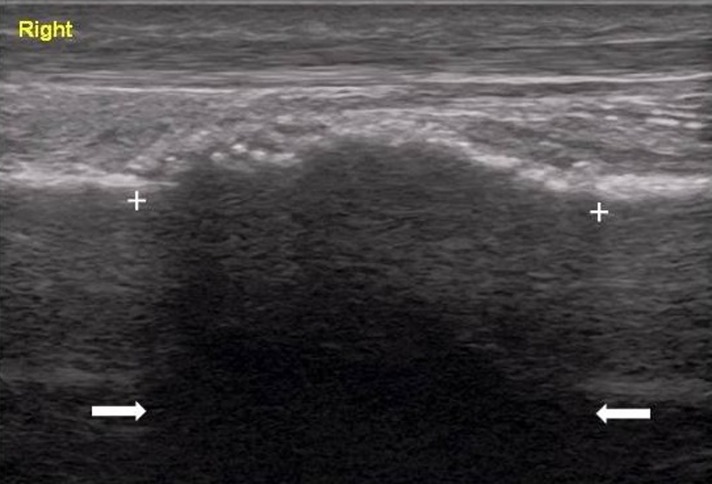
The subject's examination by a physician was delayed due to a previously planned trip. Due to persistent intermittent pain during ambulation, the subject made an appointment with a podiatrist following her return. Radiographs taken four weeks after her physical therapy examination revealed a healing stress fracture of the distal fibula (Figure 2). Since symptoms and ambulation were improving, the podiatrist recommended continued conservative management. This consisted of refraining from running until symptoms were completely abated, and then gradual resumption. The subject contacted the PT to relay the results of her examination by the podiatrist. Repeat USI revealed enlargement of the area of visible cortical irregularity (Figure 3). Eight weeks following the injury, the subject reported being pain‐free during ambulation. She was able to return to running on the treadmill and on an indoor cushioned track six months following the initial injury.
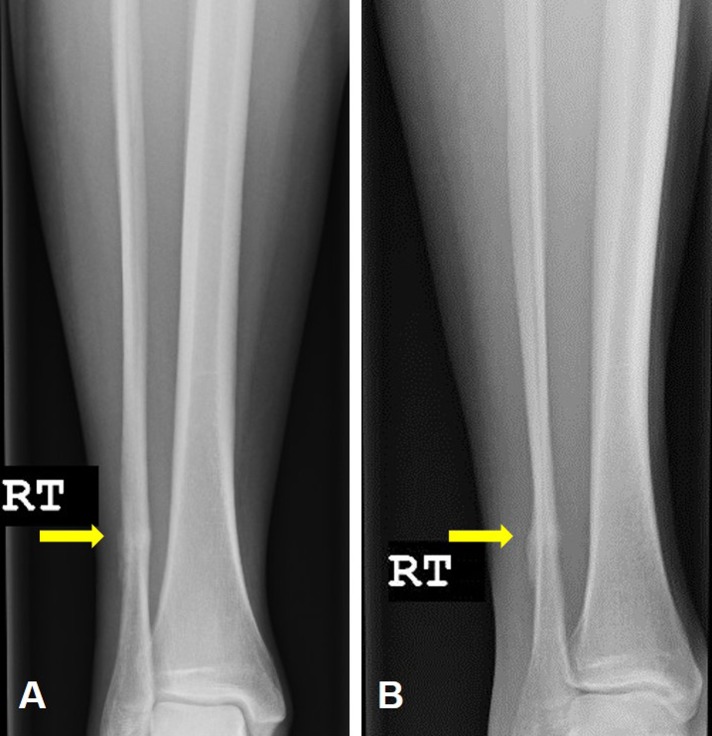
Figure 2.
Radiographs of the right lower leg, taken 47 days following symptom onset. (A) Anterior‐posterior view of the right lower leg and ankle. Distal fibular stress fracture confirmed by bone callus at the area of symptoms (yellow arrow). (B) Oblique view of the right lower leg and ankle. Fibular bone callus evident (yellow arrow); improved visualization of callus in oblique view as compared to anterior‐posterior view.
Figure 3.
Longitudinal ultrasound image of the right distal fibula, taken 53 days following symptom onset. Ultrasound settings: B mode, 10 MHz, depth 3.5 cm, image width 3.84 cm. Fibular bone callus evident as a 2.30 cm long area of cortical irregularity with a mixed hypoechoic‐hyperechoic appearance (between the white crosses). Posterior acoustic shadowing from the bone callus visible (between the white arrows).
The couch‐to‐5K program in which the subject participated included walk‐run interval training sessions three times per week that began with 20 minutes of 60‐second jog intervals alternated with 90‐second walk intervals bounded by five‐minute warm‐up and cool‐down walks (Run for God, Varnell, Georgia, USA). The program progressively increases jogging time while decreasing walking time for a total time of 30 minutes for 10 weeks. During week 11 the running time was 30 minutes with five‐minute walking warm‐ups and cool‐downs. Running based upon distance began in week 12 with two‐mile jogs and finally three‐mile jogs. The 5K race was following week 12. The subject reported that she first felt symptoms at the end of week nine of training in which she ran approximately 2.5 miles three times. She developed constant pain when she participated in a 5K at the end of week 10 of training.
DISCUSSION
This case report has shown how the results of portable USI were useful in the decision making process to refer a 52‐year‐old female recreational runner to a physician for a suspected fibular stress fracture. Physical therapists have been reported to use therapeutic ultrasound to screen for the presence of stress fractures.35 Although it is currently not common practice for PTs to use USI to diagnose fractures, the clinical use of USI by PTs to make qualitative assessments of muscle architecture in rehabilitation is growing.36,37 Physical therapists have been reported to use USI to assess the trunk muscles in persons with low back pain, the infraspinatous muscle in persons with shoulder impingement syndrome, the scapular muscles in persons with lateral epicondylalgia, and the levator ani muscles in persons with pelvic floor dysfunction.24,25,38-42 Ultrasound imaging provides visualization of muscle tissue and is able to provide dynamic images of muscle during contraction and activity.37 Since abnormal findings of bony structures may be visible with USI, PTs should be knowledgeable of normal versus abnormal bony architecture to aid in clinical decision making.
The fibular stress fracture developed by this recreational runner was initially not suspected as the cause of her symptoms due to her relatively small amount of running. Although the subject did recently increase her running mileage and frequency, this was done over a period of nine weeks. Her reported weekly mileage was much less than 25 miles per week, the amount reported to be an extrinsic risk factor for stress fractures.1 She reported exercising several times per week prior to beginning the “couch‐to‐5K” running training program. The training program utilized interval training, which was found to be protective of running related injuries in a prospective study of recreational runners.43 Although a 10% rule for a graded progression of exercise volume is commonly recommended, there is insufficient evidence to the beneficial effects of such a program.44,45 But in light of the diagnosis, it is apparent that several risk factors for a stress fracture were present including female gender, altered training regimen for both amount and surface of running terrain, and a possible biomechanical risk factor related to the foot structure of the patient's right foot.1,17,18 It is possible that additional factors may have contributed to development of the stress fracture including hormonal influences, older age, nutritional deficiencies, reduced physical fitness, reduced bone mass, and being a novice runner.17,46 Lower estrogen levels in amenorrheic female athletes was reported to interfere with the ability of bone to adapt to increased mechanical loading due to disruption of the osteoclast/osteoblast activity.9,17 It may be that perimenopausal female recreational athletes are at increased risk of stress fractures due to lower estrogen levels, amenorrhea, and reduced caloric intake for weight loss. A recent meta‐analysis found that novice runners were at greater risk for running‐related injuries versus regular recreational runners.46
Although fibular stress fractures have been reported, this is the first case reporting the use of USI findings of a distal fibular stress fracture.47-49 A systematic review concluded that USI was accurate for diagnosis of long bone fractures in the emergency department setting.26 Ultrasound imaging has also been used at the hospital bedside for diagnosis of pediatric long bone fractures.29 Metatarsal and tibial stress fracture cases diagnosed with USI have been reported.34,50,51 A case series of primarily metatarsal stress fractures included one case of an adolescent male with a proximal fibular stress fracture.49 Importantly, comparison of USI findings to MRI for detection of early metatarsal stress fractures in persons with negative radiographs demonstrated sensitivity of 83%, specificity of 76%, a positive likelihood ratio of 3.45, and a negative likelihood ratio of 0.22.30 A recent systematic review of studies examining diagnostic imaging for LE stress fractures reported that USI has higher sensitivity than specificity.52 The authors recommended that the best use may be to rule out a LE stress fracture when USI findings are negative; magnetic resonance imaging is the current recommended “gold standard” to diagnose a LE stress fracture.52
The USI image cortical irregularity overlying the stress fracture in this case is similar to the reported findings of earlier case reports involving the tibia and the metatarsals. This case has a few additional findings of interest, notably visible periosteal elevation demonstrated by the hypoechoic area overlying the hyperechoic area of the bony cortex and hypoechoic areas in the soft tissues, which are fluid from inflammation.51 Ultrasound imaging signs reported to indicate a stress fracture include periosteal elevation, fluid in the soft tissue surrounding the bone, increased acoustic shadowing posterior to the stress fracture, and increased vascularization due to healing (visible on Doppler color USI).49,53,54 The follow‐up USI illustrates posterior acoustic shadowing and the mixed hypoechoic‐hyperechoic character of healing bone callus, visible on the subject's radiograph taken a few days prior.28,49,51,53 It may be that the tender, firm enlargement palpated by the PT over the subject's fibula was a healing bone callus at the site of the stress fracture. Physical therapists using gray‐scale USI to assess muscle morphology should be alert for signs of cortical irregularity, increased posterior shadowing, increased vascularization, and hypoechoic areas overlying normal hyperechoic bone as possible signs of occult stress fractures.49,53 If color Doppler USI is used, the PT should be alert for signs of increased vascularization as an early indication of bone healing in a suspected stress fracture.54
Ultrasound imaging is being used more frequently for assessment of muscle morphology and motor control in rehabilitation and for clinical diagnosis.23,26,29,55 Reported benefits to USI as an imaging modality are: it does not expose a patient to radiation, it is inexpensive, it may be portable, it is becoming readily available, and it is easy to perform.1,29,53 Physical therapists are using USI to assess musculoskeletal structures for clinical decision making in designing the rehabilitation program.25,41,42,56 In response to the growing clinical use of USI by PTs, recommendations regarding its use by PTs have been published.55,57 This case report suggests that USI may be useful to assist clinicians with clinical decision making as a screening tool for the need to refer.26,34 Although fibular stress fractures are considered low risk injuries since they are not likely to progress to complete fracture or to develop nonunion or delayed union, they still may result in significant morbidity if not managed properly.9,16 Importantly, USI may be useful for examination of other bones in which stress fractures are considered high risk, such as the femur.9,15,16 If PTs have access to this diagnostic imaging device, the images collected may be useful to send with a patient when referring him/her to a medical physician. This is only a case report; however, so firm conclusions cannot be made. Future research is needed to evaluate the sensitivity and specificity of USI for the detection of early stress fractures.30,52
CONCLUSIONS
This case report has shown the use of USI results in the decision making process of a PT to refer a recreational female runner for a suspected fibular stress fracture. The abnormal bony findings of the right fibula, coupled with the patient history, age, gender, constant pain, and physical examination findings indicated that referral to a medical physician was necessary. This case illustrates the importance of a PT being familiar with bony findings on USI since they may be signs of an occult stress fracture. This may be particularly important for those PTs examining patients who are self‐referred or for patients who have only been examined with plain radiography.
REFERENCES
- 1.Patel DS Roth M Kapil N. Stress fractures: Diagnosis, treatment, and prevention. Am Fam Physician. 2011;83(1):39‐46. [PubMed] [Google Scholar]
- 2.Behrens SB Deren ME Matson A Fadale PD Monchik KO. Stress fractures of the pelvis and legs in athletes: A review. Sports Health. 2013;5(2):165‐174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Brukner P Bradshaw C Khan KM White S Crossley K. Stress fractures: A review of 180 cases. Clin J Sport Med. 1996;6(2):85‐89. [PubMed] [Google Scholar]
- 4.Iwamoto J Takeda T. Stress fractures in athletes: Review of 196 cases. J Orthop Sci. 2003;8(3):273‐278. [DOI] [PubMed] [Google Scholar]
- 5.Niva MH Sormaala MJ Kiuru MJ Haataja R Ahovuo JA Pihlajamaki HK. Bone stress injuries of the ankle and foot: An 86‐month magnetic resonance imaging‐based study of physically active young adults. Am J Sports Med. 2007;35(4):643‐649. [DOI] [PubMed] [Google Scholar]
- 6.Macleod MA Houston AS Sanders L Anagnostopoulos C. Incidence of trauma related stress fractures and shin splints in male and female army recruits: Retrospective case study. BMJ. 1999;318(7175):29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bhatnagar A Kumar M Shivanna D Bahubali A Manjunath D. High incidence of stress fractures in military cadets during training: A point of concern. J Clin Diagn Res. 2015;9(8):RC01‐3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bennell KL Brukner PD. Epidemiology and site specificity of stress fractures. Clin Sports Med. 1997;16(2):179‐196. [DOI] [PubMed] [Google Scholar]
- 9.McCormick F Nwachukwu BU Provencher MT. Stress fractures in runners. Clin Sports Med. 2012;31(2):291‐306. [DOI] [PubMed] [Google Scholar]
- 10.Gaeta M Mileto A Ascenti G Bernava G Murabito A Minutoli F. Bone stress injuries of the leg in athletes. Radiol Med. 2013;118(6):1034‐1044. [DOI] [PubMed] [Google Scholar]
- 11.Snyder RA Koester MC Dunn WR. Epidemiology of stress fractures. Clin Sports Med. 2006;25(1):37‐52, viii. [DOI] [PubMed] [Google Scholar]
- 12.Bennell KL Malcolm SA Thomas SA Wark JD Brukner PD. The incidence and distribution of stress fractures in competitive track and field athletes. A twelve‐month prospective study. Am J Sports Med. 1996;24(2):211‐217. [DOI] [PubMed] [Google Scholar]
- 13.Brunet ME Cook SD Brinker MR Dickinson JA. A survey of running injuries in 1505 competitive and recreational runners. J Sports Med Phys Fitness. 1990;30(3):307‐315. [PubMed] [Google Scholar]
- 14.Matheson GO Clement DB McKenzie DC Taunton JE Lloyd‐Smith DR MacIntyre JG. Stress fractures in athletes. A study of 320 cases. Am J Sports Med. 1987;15(1):46‐58. [DOI] [PubMed] [Google Scholar]
- 15.Fredericson M Jennings F Beaulieu C Matheson GO. Stress fractures in athletes. Top Magn Reson Imaging. 2006;17(5):309‐325. [DOI] [PubMed] [Google Scholar]
- 16.Kahanov L Eberman LE Games KE Wasik M. Diagnosis, treatment, and rehabilitation of stress fractures in the lower extremity in runners. Open Access J Sports Med. 2015;6:87‐95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Warden SJ Burr DB Brukner PD. Stress fractures: Pathophysiology, epidemiology, and risk factors. Curr Osteoporos Rep. 2006;4(3):103‐109. [DOI] [PubMed] [Google Scholar]
- 18.Wright AA Taylor JB Ford KR Siska L Smoliga JM. Risk factors associated with lower extremity stress fractures in runners: A systematic review with meta‐analysis [published online ahead of print July 17, 2015]. Br J Sports Med. doi:10.1136/bjsports‐2015‐094828. [DOI] [PubMed] [Google Scholar]
- 19.Chen YT Tenforde AS Fredericson M. Update on stress fractures in female athletes: Epidemiology, treatment, and prevention. Curr Rev Musculoskelet Med. 2013;6(2):173‐181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Changstrom BG Brou L Khodaee M Braund C Comstock RD. Epidemiology of stress fracture injuries among US high school athletes, 2005‐2006 through 2012‐2013. Am J Sports Med. 2015;43(1):26‐33. [DOI] [PubMed] [Google Scholar]
- 21.Tenforde AS Sayres LC McCurdy ML Sainani KL Fredericson M. Identifying sex‐specific risk factors for stress fractures in adolescent runners. Med Sci Sports Exerc. 2013;45(10):1843‐1851. [DOI] [PubMed] [Google Scholar]
- 22.Sanderlin BW Raspa RF. Common stress fractures. Am Fam Physician. 2003;68(8):1527‐1532. [PubMed] [Google Scholar]
- 23.Grzelak P Podgorski MT Stefanczyk L Domzalski M. Ultrasonographic test for complete anterior cruciate ligament injury. Indian J Orthop. 2015;49(2):143‐149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Koppenhaver S Harris D Harris A, et al. The reliability of rehabilitative ultrasound imaging in the measurement of infraspinatus muscle function in the symptomatic and asymptomatic shoulders of patients with unilateral shoulder impingement syndrome. Int J Sports Phys Ther. 2015;10(2):128‐135. [PMC free article] [PubMed] [Google Scholar]
- 25.Thibault‐Gagnon S Gentilcore‐Saulnier E Auchincloss C McLean L. Pelvic floor ultrasound imaging: Are physiotherapists interchangeable in the assessment of levator hiatal biometry? Physiother Can. 2014;66(4):340‐347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Joshi N Lira A Mehta N Paladino L Sinert R. Diagnostic accuracy of history, physical examination, and bedside ultrasound for diagnosis of extremity fractures in the emergency department: A systematic review. Acad Emerg Med. 2013;20(1):1‐15. [DOI] [PubMed] [Google Scholar]
- 27.Marshburn TH Legome E Sargsyan A, et al. Goal‐directed ultrasound in the detection of long‐bone fractures. J Trauma. 2004;57(2):329‐332. [DOI] [PubMed] [Google Scholar]
- 28.Craig JG Jacobson JA Moed BR. Ultrasound of fracture and bone healing. Radiol Clin North Am. 1999;37(4):737‐51, ix. [DOI] [PubMed] [Google Scholar]
- 29.Cross KP. Bedside ultrasound for pediatric long bone fractures. Clin Pediatr Emerg Med. 2011;12(1):27‐36. [Google Scholar]
- 30.Banal F Gandjbakhch F Foltz V, et al. Sensitivity and specificity of ultrasonography in early diagnosis of metatarsal bone stress fractures: A pilot study of 37 patients. J Rheumatol. 2009;36(8):1715‐1719. [DOI] [PubMed] [Google Scholar]
- 31.Suydam SM Buchanan TS Manal K Silbernagel KG. Compensatory muscle activation caused by tendon lengthening post‐Achilles tendon rupture. Knee Surg Sports Traumatol Arthrosc. 2015;23(3):868‐874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dutton M. Patient/client management. In: Dutton's Orthopaedic Examination, Evaluation, and Intervention. 3rd ed. New York, NY: The McGraw‐Hill Companies, Inc.; 2012:151‐191. [Google Scholar]
- 33.Dutton M. The ankle and foot. In: Dutton's Orthopaedic Examination, Evaluation, and Intervention. 3rd ed. New York, New York: The McGraw‐Hill Companies, Inc.; 2012:943‐1034. [Google Scholar]
- 34.Khy V Wyssa B Bianchi S. Bilateral stress fracture of the tibia diagnosed by ultrasound. A case report. J Ultrasound. 2012;15(2):130‐134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Romani WA Perrin DH Dussault RG Ball DW Kahler DM. Identification of tibial stress fractures using therapeutic continuous ultrasound. J Orthop Sports Phys Ther. 2000;30(8):444‐452. [DOI] [PubMed] [Google Scholar]
- 36.Potter CL Cairns MC Stokes M. Use of ultrasound imaging by physiotherapists: A pilot study to survey use, skills and training. Man Ther. 2012;17(1):39‐46. [DOI] [PubMed] [Google Scholar]
- 37.Teyhen DS. Rehabilitative ultrasound imaging for assessment and treatment of musculoskeletal conditions. Man Ther. 2011;16(1):44‐45. [DOI] [PubMed] [Google Scholar]
- 38.Brenner AK Gill NW Buscema CJ Kiesel K. Improved activation of lumbar multifidus following spinal manipulation: A case report applying rehabilitative ultrasound imaging. J Orthop Sports Phys Ther. 2007;37(10):613‐619. [DOI] [PubMed] [Google Scholar]
- 39.Stokes M Hides J Elliott J Kiesel K Hodges P. Rehabilitative ultrasound imaging of the posterior paraspinal muscles. J Orthop Sports Phys Ther. 2007;37(10):581‐595. [DOI] [PubMed] [Google Scholar]
- 40.Hebert JJ Koppenhaver SL Parent EC Fritz JM. A systematic review of the reliability of rehabilitative ultrasound imaging for the quantitative assessment of the abdominal and lumbar trunk muscles. Spine. 2009;34(23):E848‐56. [DOI] [PubMed] [Google Scholar]
- 41.Koppenhaver SL Hebert JJ Parent EC Fritz JM. Rehabilitative ultrasound imaging is a valid measure of trunk muscle size and activation during most isometric sub‐maximal contractions: A systematic review. Aust J Physiother. 2009;55(3):153‐169. [DOI] [PubMed] [Google Scholar]
- 42.Day JM Bush H Nitz AJ Uhl TL. Scapular muscle performance in individuals with lateral epicondylalgia. J Orthop Sports Phys Ther. 2015;45(5):414‐424. [DOI] [PubMed] [Google Scholar]
- 43.Hespanhol Junior LC Pena Costa LO Lopes AD. Previous injuries and some training characteristics predict running‐related injuries in recreational runners: A prospective cohort study. J Physiother. 2013;59(4):263‐269. [DOI] [PubMed] [Google Scholar]
- 44.Buist I Bredeweg SW van Mechelen W Lemmink KA Pepping GJ Diercks RL. No effect of a graded training program on the number of running‐related injuries in novice runners: A randomized controlled trial. Am J Sports Med. 2008;36(1):33‐39. [DOI] [PubMed] [Google Scholar]
- 45.Bredeweg SW Zijlstra S Bessem B Buist I. The effectiveness of a preconditioning programme on preventing running‐related injuries in novice runners: A randomised controlled trial. Br J Sports Med. 2012;46(12):865‐870. [DOI] [PubMed] [Google Scholar]
- 46.Videbaek S Bueno AM Nielsen RO Rasmussen S. Incidence of running‐related injuries per 1000 h of running in different types of runners: A systematic review and meta‐analysis. Sports Med. 2015;45(7):1017‐1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bertrand AS Leroux J Cellier C Abu Amara S Vivier PH. Stress fracture of the fibula. J Radiol. 2011;92(12):1139‐1142. [DOI] [PubMed] [Google Scholar]
- 48.Greenberg EM Gohn N Grady M. Fibular stress fracture in a high school athlete. J Orthop Sports Phys Ther. 2013;43(1):29. [DOI] [PubMed] [Google Scholar]
- 49.Bodner G Stockl B Fierlinger A Schocke M Bernathova M. Sonographic findings in stress fractures of the lower limb: Preliminary findings. Eur Radiol. 2005;15(2):356‐359. [DOI] [PubMed] [Google Scholar]
- 50.Banal F Etchepare F Rouhier B, et al. Ultrasound ability in early diagnosis of stress fracture of metatarsal bone. Ann Rheum Dis. 2006;65(7):977‐978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Battaglia PJ Kaeser MA Kettner NW. Diagnosis and serial sonography of a proximal fifth metatarsal stress fracture. J Chiropr Med. 2013;12(3):196‐200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wright AA Hegedus EJ Lenchik L Kuhn KJ Santiago L Smoliga JM. Diagnostic accuracy of various imaging modalities for suspected lower extremity stress fractures: A systematic review with evidence‐based recommendations for clinical practice [published online ahead of print March 24, 2015]. Am J Sports Med. doi: 10.1177/0363546515574066. [DOI] [PubMed] [Google Scholar]
- 53.Moran DS Evans RK Hadad E. Imaging of lower extremity stress fracture injuries. Sports Med. 2008;38(4):345‐356. [DOI] [PubMed] [Google Scholar]
- 54.Caruso G Lagalla R Derchi L Iovane A Sanfilippo A. Monitoring of fracture calluses with color Doppler sonography. J Clin Ultrasound. 2000;28(1):20‐27. [DOI] [PubMed] [Google Scholar]
- 55.Teyhen D Koppenhaver S. Rehabilitative ultrasound imaging. J Physiother. 2011;57(3):196. [DOI] [PubMed] [Google Scholar]
- 56.Tragord BS Bui‐Mansfield LT Croy T Shaffer SW. Suprascapular neuropathy after distal clavicle resection and coracoclavicular ligament reconstruction: A resident's case problem. J Orthop Sports Phys Ther. 2015;45(4):299‐305. [DOI] [PubMed] [Google Scholar]
- 57.Bailey LB Beattie PF Shanley E Seitz AL Thigpen CA. Current rehabilitation applications for shoulder ultrasound imaging. J Orthop Sports Phys Ther. 2015;45(5):394‐405. [DOI] [PubMed] [Google Scholar]