Abstract
Background
Kinesiology tape has been advocated as a means of improving muscle flexibility, a potential modifiable risk factor for injury, over time. The epidemiology and etiology of hamstring injuries in sport have been well documented.
Purpose
To compare the temporal pattern of efficacy of kinesiology tape and traditional stretching techniques on hamstring extensibility over a five day period.
Study Design
Controlled laboratory study.
Methods
Thirty recreationally active male participants (Mean ± SD: age 20.0 ± 1.55 years; height 179.3 ± 4.94 cm; mass 76.9 ± 7.57 kg) completed an active knee extension assessment (of the dominant leg) as a measure of hamstring extensibility. Three experimental interventions were applied in randomized order: Kinesiology tape (KT), static stretch (SS), proprioceptive neuromuscular facilitation (PNF). Measures were taken at baseline, +1min, + 30mins, + 3days and +5days days after each intervention. The temporal pattern of change in active knee extension was modelled as a range of regression polynomials for each intervention, quantified as the regression coefficient.
Results
Hamstring ROM with KT application at +3days was significantly greater than baseline (129.18 ± 15.46%, p = 0.01), SS (106.99 ± 9.84%, p = 0.03) and PNF (107.42 ± 136.13%, p = 0.03) interventions. The temporal pattern of changes in ROM for SS and PNF were best modelled by a negative linear function, although the strength of the correlation was weak in each case. In contrast, the KT data was optimised using a quadratic polynomial function (r2 = 0.60), which yielded an optimum time of 2.76 days, eliciting a predicted ROM of 129.6% relative to baseline.
Conclusion
Each intervention displayed a unique temporal pattern of changes in active knee extension. SS was best suited to immediate improvements, and PNF to +30 minutes in hamstring extensibility, whereas kinesiology tape offered advantages over a longer duration, peaking at 2.76 days. These findings have implications for the choice of intervention, timing and duration to assist clinicians in both a sporting and clinical context.
Level of evidence
2c
Keywords: Flexibility, hamstring, kinesiology tape, stretching
INTRODUCTION
Recent investigations have examined the temporal efficacy of kinesiology taping (KT), finding that KT offered greater tissue response than PNF and static stretching over an acute time frame (30 minutes), peaking at 24.2 minutes.1 These findings may assist clinicians in determining the optimum application time for kinesiology tape to implement a positive tissue response prior to performance. Changes in tissue extensibility might be due to cutaneous receptor response, tissue deformation, and/or activation of the adhesive properties of the tape. Although manufacturers indicate KT can be worn for a three to five day period in order to have the optimum tissue response, there is currently minimal supporting empirical evidence.2,3 Several authors have considered the response to KT application (for up to 7 days) in pain, range of movement (ROM) and function in those with musculoskeletal pathologies with varying outcomes.4‐9
The complex physiological mechanisms underpinning the benefits of KT continue to be debated with both mechanical and sensory theories discussed.10 Suggested mechanical benefits include enhanced muscle extensibility, neuromuscular reflex stimulation (autogenic or reciprocal inhibition), stress‐strain relaxation, and tissue and plastic deformation.5,10‐13 However sensory tolerance and pain gate control theory may also influence the extensibility of the tissue.10,14
Muscle extensibility is one of many physical components that potentially influences injury, resulting in variations in muscle flexibility intervention strategies.15‐17 However direct comparison of interventions between studies is limited with methodological discrepancies in application, procedures, anatomical regions, recruitment criteria and sample size apparent.13,18‐21 Restricted hamstring flexibility is discussed as a potential precursor to injury, as a “modifiable” intrinsic risk factor, particularly in maximal speed activities due to the eccentric overload of the tissue.16,22‐26 Previously, static stretching (SS) was the common approach used to address flexibility in traditional musculoskeletal protocols,15,16,27,28 however evidence that demonstrates potential detrimental effects on strength and power associated with SS has resulted in a greater shift towards dynamic stretching and proprioceptive neuromuscular facilitation (PNF). 29‐33
The temporal efficacy of kinesiology taping on muscle extensibility over a three to five day period has been afforded little consideration, despite the common clinical suggestion for use over this time frame. Furthermore, the implications for sporting performance and musculoskeletal pathologies remain under researched. Immediate change in muscle extensibility post‐intervention using KT is likely to be through neuromuscular reflex stimulation, stress‐strain relaxation or stretch tolerance. 17 Thus static stretching and PNF would have an acute effect on hamstring extensibility, with PNF expected to show greater initial gains during and post stretch due to the potential for the contraction to impart an influence on the neuromuscular reflex response.38 However, over a prolonged period it could be hypothesised that KT could show an effect as the properties of the tape are activated over time, influencing cutaneous mechanoreceptor stimulation. Since KT application for muscle stretch is from the origin to insertion while in the lengthened position it could be hypothesised that through prolonged stress‐strain relaxation and viscoelastic deformation, applying a constant force over a period of time will assist tissue extensibility over a five‐day period. To be able to reduce a potential risk factor for injury, the efficacy of any technique for hamstring extensibility must be studied over longer periods of time in order to determine whether the extensibility is maintained through training and performance. The aim of the present study was to compare the immediate, 30 minute, three‐ and five‐day post‐intervention efficacy of KT to traditional stretching techniques on hamstring extensibility. This may assist practitioners in their choice of intervention to maintain muscle extensibility over a key time period. It was hypothesized that the temporal pattern of changes in hamstring extensibility will be unique to each intervention, given their discrete mechanistic influence.
METHODS
An a priori power analysis was performed for sample size estimation based on data and effect size was derived from a previous study.1 Using an alpha = 0.05 and power = 0.80, the projected sample size was nine for each experimental group. Given the potential for attrition over a five‐day testing period, a total of 30 male participants completed the study. Inclusion criteria required each participant to be male, over 18 years, participating in recreational sport four times a week, and asymptomatic from injury and with no history of previous hamstring injury. Exclusion criteria included history of lumbar or neurological symptoms, history of musculoskeletal disorders or injuries within the prior 12 months, medical conditions that may alter muscle flexibility and skin allergies or conditions. All participants were further screened and excluded if their straight leg raise was <70 degrees, potentially indicative of joint or tissue restriction or pathology. The 30 participants were randomly and evenly selected into three groups by intervention. Detailed information regarding the nature and purpose of the study was provided, and all participants provided written informed consent in accordance with the departmental and university ethical procedures and following the principles outlined in the Declaration of Helsinki. Ethical approval for the study was granted by the departmental research ethics committee.
Data Collection & Analysis
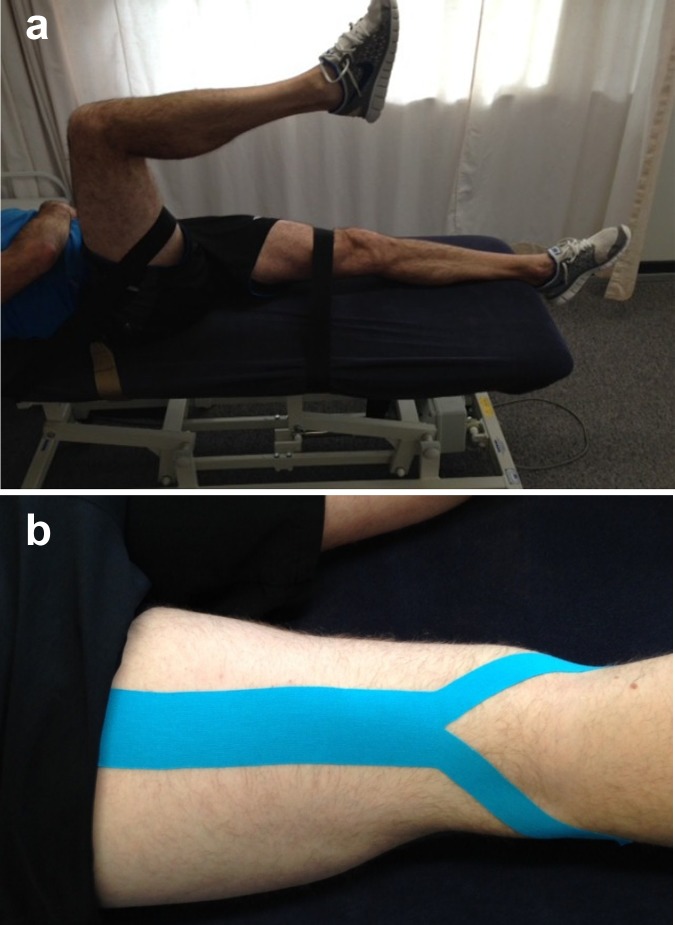
Consistent with a recent study,1 all participants completed a standardized five‐minute warm up on the cycle ergometer.29 Five centimetre (cm) seat belts were placed across ASIS and the non‐dominant leg at 20cm above tibial tuberosity in order to stabilize participants during the standardized Active Knee Extension (AKE) position34,35. The hip was placed at 908 and fixed using a seat belt, proximal to the popliteal crease (Figure 1a). All belts were marked for re‐measurement, and the dominant leg was measured for all participants. Dominant leg was identified as the preferred kicking leg.
Figure 1.
(a) The Active Knee Extension testing position and (b) kinesiology tape Y‐cut application.
The measurement of AKE was taken once the participant extended the knee to their point of hamstring stretch tolerance (no pain and initial resistance) and at that point the calcaneus was supported to allow a baseline measurement to be recorded, via a standard goniometer (Myrin, Patterson Medical, North Ryde, Australia) at the tibiofemoral joint.30,36 The participant was then placed prone on the plinth with a pillow under the ankles to assist in relaxation of hamstrings.
Subsequent to this baseline measure, AKE measurements were completed immediately, 30 minutes, three‐ and five‐ days post intervention. Participant were instructed to continue normal daily activity through the duration of the study and requested to avoid any specific activity related to hamstring flexibility. For intervention in the SS the group, the barrier of resistance was found in AKE and a 30 sec hamstring stretch applied by the researcher at the initial point of resistance, with a 10 sec rest period between each stretch. This was repeated three times.1,31,37 The PNF group was placed in AKE position and the initial stretch barrier held for 10 secs, prior to 10 secs PNF hamstring contract‐relax resistance of 75% of their perceived maximum to assist muscle activation. There was a three second release from barrier prior to stretching to new resistance barrier for 10 secs, and this process was repeated three times.1,38 For KT application the distributors guidelines (RockTape®) were followed, with the area prepared and a Y‐cut piece of tape applied at 25% stretch from ischial tuberosity to head of fibula, and to the medial condyle of tibia to hamstring muscle insertion points with knee extension (Figure 1b). The KT application remained in place for the five‐day duration of the study. For all participants and for each intervention, the same therapist performed all procedures.
Statistical Analysis
A two factor (intervention × time) repeated measures general linear model was used to determine differences between interventions at the progressive time points. Where appropriate, post‐hoc pairwise comparisons using a Bonferroni correction factor were applied. Statistical significance was set at p ≤ 0.05. All measures are reported relative to the pre‐exercise score, which assigned 100% baseline for each participant. Data are presented as mean ± standard deviation.
In describing the temporal pattern of changes in ROM, a range of regression polynomials were applied to each intervention to determine the optimal model to describe temporal efficacy1. The strength of the regression was quantified using the r2 value.
RESULTS
The subject demographics for each intervention group are summarised in Table 1.
Table 1.
Subject Demographics (presented as group mean ± standard deviation).
| Group | Age (years) | Height (cm) | Mass (kg) |
|---|---|---|---|
| KT | 19.5 ± 0.70 | 177.6 ± 4.62 | 74.2 ± 5.84 |
| SS | 20.8 ± 2.15 | 181.6 ± 4.03 | 80.0 ± 6.38 |
| PNF | 20.2 ± 1.32 | 178.7 ± 5.64 | 76.6 ± 9.55 |
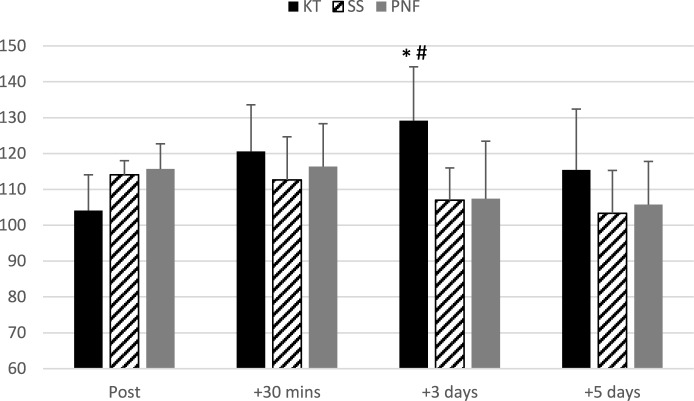
Table 2 summarises the change in ROM for each intervention over the five day period. The only significant changes observed in ROM occurred with KT application (relative to pre‐application baseline scores) at 30mins (p = 0.03) and 3 days (p = 0.01). At the three‐day post intervention measurement the KT trial also significantly outperformed the SS (p = 0.03) and PNF (p = 0.03) interventions. The SS and PNF interventions produced the greatest improvement in performance immediately post‐application but these changes were not statistically significantly different (p ∼ 0.10). The temporal pattern of changes in hamstring extensibility is shown in Figure 2.
Table 2.
Temporal changes in hamstring extensibility for each intervention.
| Group | Hamstring extensibility (% of baseline) | |||
|---|---|---|---|---|
| Post | + 30 mins | + 3 days | + 5 days | |
| KT | 104.06 ± 10.68 | 120.59 ± 13.41 | 129.18 ± 15.46 | 115.40 ± 18.54 |
| SS | 114.04 ± 3.86 | 112.67 ± 12.72 | 106.99 ± 9.83 | 103.32 ± 12.49 |
| PNF | 115.72 ± 7.18 | 116.36 ± 12.23 | 107.42 ± 16.13 | 105.81 ± 12.09 |
Figure 2.
The time history of changes in active knee extension with each intervention. *denotes significantly greater than baseline (p ≤ 0.05).
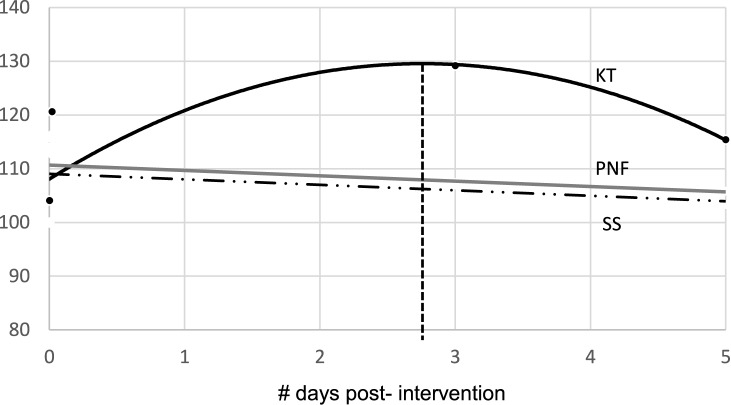
Figure 3 shows the temporal distribution in ROM plotted against a linear timeline, with the regression coefficients summarised in Table 3 for both linear and polynomial (quadratic) functions. The SS and PNF interventions were best modelled by a negative linear function, although the strength of the correlation was weak in each case. In contrast, the KT data produced a positive linear regression, but was optimized using a quadratic polynomial function (R2 = 0.60). The quadratic equation to describe the temporal pattern of change in ROM with KT application yields an optimum time of 2.76 days, eliciting a 129.6% ROM.
Figure 3.
The optimum correlational function to model the time history of changes in active knee extension for each intervention.
Table 3.
Linear and quadratic correlation coefficients to predict ROM from time post‐intervention.
| Linear regression | Quadratic regression | |
|---|---|---|
| KT | ROM = 2.55 days + 109.75 R2 = 0.24 | ROM = −2.83 days2 + 15.58 days + 108.07 R2 = 0.60 |
| SS | ROM = − 1.02 days + 109.04 R2 = 0.15 | ROM = −0.25 days2 + 0.15 days + 108.89 R2 = 0.14 |
| PNF | ROM = − 0.99 days + 110.66 R2 = 0.11 | ROM = 0.04 days2 – 1.16 days + 110.68 R2 = 0.10 |
DISCUSSION
The current study investigated the efficacy of KT on hamstring extensibility over a five‐day period in comparison with traditional stretching methods. There are a few studies (with notable methodological variance) whose authors have reported significant differences between KT and other treatment interventions,4,19,39 although research into the temporal benefits are limited.
While KT demonstrated a positive linear correlation with time post intervention, both SS and PNF presented a negative linear correlation. The findings have implications for the practitioner, since the choice of intervention might depend on the potential for immediate or longer‐term utilization for hamstring extensibility. Similar to previous literature, the findings indicate that if immediate and short term improvements are required PNF application is preferable.1,38 However if improvement in hamstring extensibility is required over a longer time period then KT offers potential benefits. KT application was best modelled as a quadratic function, predicting optimum yield at 2.76 days.
To date the majority of KT studies have considered the immediate effects after application, while few studies have reviewed over the effects over a prolonged application. Those that have considered immediate or short term effects are associated with a variety of musculoskeletal pathologies including shoulder impingement,5,40 whiplash,19 plantar fasciitis,41 PFPS,5,39 achilles tendonosis42 and chronic lower back pain.6,8,43 Results from these studies should be viewed with caution as all have variance in both clinical and statistical outcomes. Importantly, those studies whose authors’ demonstrated improvements suffered from poor methodological quality.11,12,44,45 Any immediate KT benefits reported have not been maintained through the respective follow up periods which does not allow for advocating KT in preference over other interventions,8 rather, only that KT can be used as an alternative or adjunct intervention.39,40
The proposed physiological mechanisms for the beneficial effects of KT are numerous and complex, however the majority of authors suggesting three main mechanical theories; neuromuscular reflex stimulation (autogenic or reciprocal inhibition), stress‐strain relaxation, and tissue and plastic deformation.10‐12,46 The current findings suggest the proposed mechanical theories are more likely to influence the immediate change in muscle extensibility. The tissue response to KT application may influence plastic deformation and stress‐strain relaxation over a longer duration. The greatest initial gains attributed to PNF may be due to the co‐contraction theory through the neuromuscular reflex stimulation and subsequent latency to induce tissue relaxation and allow for a new end range to be established.10,47‐50 Previous researchers determined that post PNF intervention, muscle extensibility returned to 50% of baseline within one second and 90% in 10 seconds.51
The current findings suggest that KT was the preferential treatment over the five day duration, suggesting that the effects may be due to stress‐strain relaxation and viscoelastic deformation.17 The consistently applied stretch force at the end of range induced by the KT may reduce the viscoelastic energy and promote stress relaxation, so the muscles can experience strain relaxation (creep) resulting in a decline in passive resistance over time.17,52 Furthermore within the current study the larger muscle mass associated with hamstrings may induce greater improvements as passive elastic stiffness has positive correlation to the strength of muscles in comparison to other studies that utilized other muscles.53,54
The findings indicate the optimum post‐intervention time was 2.76 days, suggesting a combination of initial cutaneous mechanoreceptor stimulation, viscoelastic change and stress‐strain relaxation may assist in deformation over an approximate three day time period. However the results showed no statistically significant differences in ROM at day five, and a return to resting state by day six based on the regression equation, supporting the suggestion that viscoelastic deformation is transient and it's magnitude and duration are influenced by duration, intervention and load.10,55,56
It is important to note that additional mechanisms that influence muscle extensibility should be considered, including pain perception from the central and peripheral nervous systems,10 physiological changes in sarcomeres, the stimulation of the rearrangement of collagen,58 or psychological influences.47,57 Minimal literature exists to support alternative theories of plastic deformation and other mechanical mechanisms that consider the adaptive change within connective tissue. 10,31 Thus, future research could examine the tissue response to KT application reapplied at day three, recovery days prior to reapplication or methods to achieve greater longer term effects.
Similar to the recent study reviewing the efficacy of KT over 30 minutes to assist hamstring flexibility, KT can be potentially be utilized for technique improvement and performance facilitation.59 However, it is important to consider that an increase in muscle extensibility may be detrimental to power and performance, and may actually increase injury risk.27,51 Thus, findings of the current study cannot be generalized to a wider population that differs in age, gender and health of the subjects.
Understanding the possible mechanisms of influence of KT needs further consideration through other methods such as electromyography, ultrasound, and thermal imaging. The benefits of KT are likely to be influenced by a wide range of extrinsic factors such as therapist experience, the environment, the nature of injury, population, sporting demands, and physiological, psychological and biomechanical characteristics. Efficacy may also be directly related to the execution of the therapist experience, tape application and tape techniques chosen.51 Future studies should consider longitudinal and post application follow up studies, additional muscle groups, functional task assessment, and alternative tape application methods.
CONCLUSION
Each intervention displayed a unique temporal pattern of changes in active knee extension. For an immediate improvement in hamstring muscle flexibility PNF and SS both out‐performed KT, however for improvements over a longer duration kinesiology tape is advantageous. The optimum timing of kinesiology tape application was 2.76 days, eliciting a 30% improvement in hamastring ROM relative to baseline. These findings suggest that the choice of stretching intervention be informed by the clinical context.
REFERENCES
- 1.Farquharson C Greig M. Temporal efficacy of kinesiology tape vs. traditional stretching methods on hamstring extensibility. Int J Sports Phys Ther. 2015;10(1):45‐51. [PMC free article] [PubMed] [Google Scholar]
- 2.Kinesio® Taping Association. Kinesio® Taping Method Workbook – KT1. 2008 [Google Scholar]
- 3.RockTape® A users guide. http://rocktape.net/images/user_guide.pdf. Accessed 24/06/15.
- 4.Thelen MD Dauber JA Stoneman PD. The clinical efficacy of Kinesio tape for shoulder pain: A randomized double blinded, clinical trial. J Orthop Sports Phys Ther. 2008;38:389‐395. [DOI] [PubMed] [Google Scholar]
- 5.Akbas E Atay AO Yuksel I. The effects of additional kinesio taping over exercise in the treatment of patellofemoral pain syndrome Acta Ortho et Trauma Turcica. 2011;45:335‐341. [DOI] [PubMed] [Google Scholar]
- 6.Castro‐Sanchez AM Lara‐Palomo IC Mataran‐Penarrocha GA, et al. Kinesio taping reduces disability and pain slightly in chronic non‐specific low back pain: A randomised trial. J Physiother. 2012;58:89‐95. [DOI] [PubMed] [Google Scholar]
- 7.Williams S Whatman C Hume PA et al. Kinesiotaping in treatment and prevention of sports injuries. A meta analysis of the evidence for its effectiveness. Sports Med. 2012;42(2):153‐164. [DOI] [PubMed] [Google Scholar]
- 8.Paoloni M Bernetti A Fratochhi G, et al. Kinesio Taping applied to lumbar muscles influence clinical and electromyographic characteristics in chronic low back pain patients. Eur J Phys Rehab Med. 2011;47:237‐44. [PubMed] [Google Scholar]
- 9.Garcia‐Muro F Rodgriguex‐Fernandez AL Herrero‐de‐Lucas A. Treatment of myofascial pain in the shoulder with Kinesio Taping. A case report. Man Ther. 2010;15(3):292‐95. [DOI] [PubMed] [Google Scholar]
- 10.Weppler C Magnusson P. Increasing muscle extensibility: A matter of increasing length or modifying sensation. Phys Ther. 2010;90:438‐449. [DOI] [PubMed] [Google Scholar]
- 11.Morris D Jones D Ryan H, et al. The clinical effects of Kinesio®Tex Taping: A systematic review. Physiother Theory Practice. 2013;29(4):259‐270. [DOI] [PubMed] [Google Scholar]
- 12.Mostafavifar M Wertz J Borchers J. A systematic review of the effectiveness of kinesio taping for musculoskeletal injury. Phys Sportsmed. 2012;40(4):33‐40. [DOI] [PubMed] [Google Scholar]
- 13.Gomez‐Soriano J Abian‐Vicen J Aparicio‐Garcia C, et al. The effect of kinesiology taping on muscle tone in healthy subjects: A double blind, placebo controlled cross over trial. Man Ther. 2014;19(5):508. [DOI] [PubMed] [Google Scholar]
- 14.Folpp H Deall S Harvey LA, et al. Can apparent increases in muscle extensibility with regular stretch be explained by changes in tolerance to stretch. Aust J Physiother. 2006;52:45‐50. [DOI] [PubMed] [Google Scholar]
- 15.Bahr R Holme I. Risk factors for sports injuries – a methodological approach. Br J Sports Med. 2003;37:384‐392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Witvrouw E Dannells L Asselman P, et al. Muscle flexibility as a risk factor for developing muscle injuries in male professional soccer players: a prospective study. Am J Sports Med. 2003;31(1):41‐46. [DOI] [PubMed] [Google Scholar]
- 17.Gajdosik R. Passive extensibility of skeletal muscle: review of the literature with clinical implications. Clin Biomech. 2001;16:87‐101. [DOI] [PubMed] [Google Scholar]
- 18.Merino‐Marban R Fernandez‐Rodriguez E Lopez‐Fernandez I, et al. The acute effect of kinesio taping on hamstring extensibility in university students. J of Phys Ed Sport. 2011;11(2);23‐27. [Google Scholar]
- 19.Gonzalez‐Iglesia J Fernandez‐De‐Las‐Penas C Cleland J, et al. Short term effects of cervical kinesiotaping on pain and cervical range of motion in patients with acute whiplash injury: a randomised clinical trial. J Orthop Sports Phys Ther. 2009;39(7):515‐21. [DOI] [PubMed] [Google Scholar]
- 20.Chen C Huang TS Chai HM, et al. Two stretching methods for the hamstrings: Proprioceptive Neuromuscular Facilitation versus Kinesio Taping. J Sport Rehab. 2013;22:59‐66. [DOI] [PubMed] [Google Scholar]
- 21.Williams JW Holleman DR Simel DL. Measuring shoulder function with the shoulder pain and disability index. J Rheum. 1995;22:727‐732. [PubMed] [Google Scholar]
- 22.Lui H Garrett WE Moorman C, et al. (2012) Injury rate, mechanism, and risk factors of hamstring strain injuries in sports: A review of the literature. J Sport Health Sci. 2012;1(2):92‐101. [Google Scholar]
- 23.Brooks JHM Fuller CW Kemp SPT, et al. Incidence, risk and prevention of hamstring muscle injuries in professional rugby union. Am J Sports Med. 2006;34(8):1297‐1306. [DOI] [PubMed] [Google Scholar]
- 24.Woods C Hawkins RD Hulse M, et al. The Football Association Medical Research Programme: an audit of injuries in professional football – analysis of hamstring injuries. Br J Sports Med. 2004;38:36‐41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Clarke RA. Hamstring injuries: risk assessment and injury prevention. Ann Acad Med Singapore. 2008;37:341‐346. [PubMed] [Google Scholar]
- 26.Arnason A Andersen TE Holme I, et al. Prevention of hamstring strains in elite soccer: an intervention study. Scand J Med Sci Sports. 2008;18(1);40‐48. [DOI] [PubMed] [Google Scholar]
- 27.Peterson J Holmich P. Evidence based prevention of hamstring injuries in sport. Br J Sports Med. 2005;39:319‐323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Nelson RT Bandy WD. Eccentric training and static stretching improve hamstring flexibility of high school males. J Athl Train. 2004;39:254‐258. [PMC free article] [PubMed] [Google Scholar]
- 29.Bradley PS Olsen PD Portas MD. The effect of static, ballistic and proprioceptive neuromuscular facilitation on vertical jump performance. J Strength Cond Res. 2007;7(1):223‐226. [DOI] [PubMed] [Google Scholar]
- 30.Russell PJ Decoster LC Enea D. Effects of gastrocnemius, hamstring and combined stretching programmes on knee extensibility. Athl Train Sports Health Care. 2010;2(2):67‐73. [Google Scholar]
- 31.Feland JB Myrer JW Merrill RM. Acute changes in hamstring flexibility: PNF versus static stretching in Senior athletes. Phys Ther Sport. 2001;2:186‐193. [Google Scholar]
- 32.Kay AD, Blazevich AJ. Effect of acute static stretch on maximal muscle performance: A systematic review. Med Sci Sports Exerc. 2012;54‐164. [DOI] [PubMed] [Google Scholar]
- 33.Behm DG Button DC Butt JC Factors affecting force loss with prolonged stretching. Can J App Phys. 2001;26(3);262‐272. [PubMed] [Google Scholar]
- 34.Mendiguchia J Brughelli M. A return to sport algorithm for acute hamstring injuries. Phys Ther Sport. 2011;12:2‐14. [DOI] [PubMed] [Google Scholar]
- 35.Azevedo DC Melo RM Correa RVA, et al. Uninvolved versus target muscle contraction during contract relax proprioceptive neuromuscular facilitation stretching. Phys Ther Sport. 2011;12(3):117‐121. [DOI] [PubMed] [Google Scholar]
- 36.Panteleimon B Panagiotis I Fotis B. Evaluation of hamstring flexibility by using two different measuring instruments. Sport Logia. 2010;6:28‐32. [Google Scholar]
- 37.Yuktasir B Kaya F. Investigation into the long term effects of static and PNF stretching exercises on range of motion and jump performance. J Bodywork Movement Ther. 2009;13:11‐21. [DOI] [PubMed] [Google Scholar]
- 38.Funk DC Swank AM Mikla BM, et al. Impact of prior exercise on hamstring flexibility: a comparison of proprioceptive neuromuscular facilitation and static stretching. J Strength Cond Res. 2003;17(3):489‐492. [DOI] [PubMed] [Google Scholar]
- 39.Aytar A Ozunlus N Surenkok O, et al. Initial effects of kinesio taping in patients with patellofemorial pain syndrome: A randomized, double blind study. Isokin Exerc Sci. 2011;19:135‐142. [Google Scholar]
- 40.Kaya E Zinnuroglu M Tugcu I. Kinesio taping compared to physical therapy modalities for the treatment of shoulder impingement syndrome. Clin Rheumatol. 2011;30(2):201‐207. [DOI] [PubMed] [Google Scholar]
- 41.Tsai HJ Chang WD Lee JP. Effects of short‐term treatment with kinesio taping for plantar fasciitis. J Musculoskeletal Pain. 2010;18:71‐80. [Google Scholar]
- 42.Lee JH Yoo WG. Treatment of chronic Achilles tendon pain by Kinesio taping in an amateur badminton player. Phys Ther Sport. 2012;13(2):115‐119. [DOI] [PubMed] [Google Scholar]
- 43.Yoshida A Kahanov L. The effect of kinesiotaping on lower trunk range of motions. Res Sports Med. 2007;15(2):103‐112. [DOI] [PubMed] [Google Scholar]
- 44.Ernst E Pittler MH. Re‐analysis of previous meta‐analysis of clinical trials in homeopathy. J Clin Epidemiology. 2000;53:1188. [DOI] [PubMed] [Google Scholar]
- 45.Schultz KF Chalmers I Hayes RJ, et al. Dimensions of methodological quality associated with estimates of treatment effects in controlled trials. JAMA. 1995;273(5):408‐412. [DOI] [PubMed] [Google Scholar]
- 46.Sharman M Cresswell A Riek S. Proprioceptive Neuromuscular Facilitation stretching mechanisms and clinical application. Sports Med. 2006;36(11):929‐939. [DOI] [PubMed] [Google Scholar]
- 47.De Weijer VC Goeken LN Shamus E. The effect of static stretching and warm up exercise on hamstring length over the course of 24 hours. J Orthop Sports Phys Ther. 2003;33:727‐733. [DOI] [PubMed] [Google Scholar]
- 48.Chalmers G. Re‐examination of the possible role of golgi tendon organ and muscle spindle reflexes in proprioceptive neuromuscular facilitation muscle stretching. Sports Biomech. 2004;3:159‐183. [DOI] [PubMed] [Google Scholar]
- 49.Hindle KB Whitcomb TJ Briggs WO, et al. Proprioceptive Neuromuscular Facilitation (PNF): Its mechanisms and effects on range of motion and muscular function. J Hum Kinetics. 2012;31:105‐113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.O’Hora J Cartwright A Wade CD, et al. Efficacy of static stretching and proprioceptive neuromuscular facilitation stretch on hamstring length after a single session. J Strength Cond Res 2011;25(6):1586‐1591. [DOI] [PubMed] [Google Scholar]
- 51.Moore MA Kukulka CG. Depression of Hoffman Reflexes following voluntary contraction and implications for proprioceptive neuromuscular facilitation therapy. Phys Ther. 1991;71:321‐329. [DOI] [PubMed] [Google Scholar]
- 52.Magnusson SP Simonsen EB Aagard P, et al. Viscoelastic response to repeated static stretching in the human hamstring muscle. Scand J Med Sci Sports. 1995;5:342‐347. [DOI] [PubMed] [Google Scholar]
- 53.Klinge K Magnusson SP Simonsen EB, et al. The effect of strength and flexibility training on skeletal muscle electromyographic activity, stiffness and viscoelastic stress relaxation response. Am J Sports Med. 1997;25(5):710‐716. [DOI] [PubMed] [Google Scholar]
- 54.McHugh MP Kremenic IJ Fox MB, et al. The role of mechanical and neural restraints to joint range of motion during passive stretch. Med Sci Sports Exerc. 1998;30(6):928‐932. [DOI] [PubMed] [Google Scholar]
- 55.Magnusson SP Simonsen EB Aagaard P, et al. Biomechanical responses to repeated stretches in human hamstring muscle in vivo. Am J Sports Med. 1996;24:622‐628. [DOI] [PubMed] [Google Scholar]
- 56.Magnusson SP Aagaard P Nielson JJ. Passive energy return after repeated stretches of the hamstring muscle‐tendon unit. Med Sci Sports Exerc. 2000;32(1);1160‐1164. [DOI] [PubMed] [Google Scholar]
- 57.Franettovich M Chapman A Blanch P, et al. A physiological and psychological basis for anti‐pronation taping from a critical review of the literature. Sports Med. 2008;38(8):617‐631. [DOI] [PubMed] [Google Scholar]
- 58.Ben M Harvey LA. Regular stretch does not increase muscle extensibility: A randomised control trial. Scand J Med Sci Sport. 2010;20(1):136‐144. [DOI] [PubMed] [Google Scholar]
- 59.Vithoulk I Beneka A Malliou P, et al. The effects of kinesiotaping on quadriceps strength during isokinetic exercise in healthy non athlete women. Isokinetics Exerc Sci. 2010;18(1):1‐6. [Google Scholar]