The Accreditation Council for Graduate Medical Education (ACGME) has called for improved assessment systems that better prepare residents for practice in the 21st century.1–3 As part of the milestone initiative, graduate medical education (GME) programs must convene clinical competency committees (CCCs) to synthesize assessments collected from evaluators in various clinical settings.4–6 These changes have prompted the GME community to critically review current assessment methods in order to identify workplace-based assessments that would provide meaningful data for CCC deliberations.7
This article reviews theoretical advantages of chart-stimulated recall (CSR), explores threats to validity due to construct underrepresentation and construct irrelevant variance using Messick's framework, and discusses possible solutions. The results can inform the GME community on considerations and potential solutions when implementing CSRs as part of an assessment system. We also identify areas for future research studies.
Chart-Stimulated Recall
CSR is a hybrid assessment format that combines chart review and an oral examination, with both based on a clinician's documented patient encounter. Faculty or the learner selects the clinical chart for a learner's patient to be used as a stimulus for questioning.8–16 Using the learner's own clinical chart situates the examination within a realistic context, adding to the authenticity and value of the exercise.17 Through a series of probing questions designed to inquire into the learner's clinical decision-making skills, the examinee is asked to reflect on and explain his or her rationale for clinical decisions. CSR has been used extensively in the United Kingdom and in Canada for the assessment of practicing physicians; in the United States it is predominantly used to assess trainees.
A variety of scoring forms have been developed for CSR, ranging from checklists with comment boxes to ordinal rating scales.11,18,19 Feedback usually is given to the learner at the end of the encounter11,20 and may include action plans to improve future clinical decision making.11,18,20–22 Despite evidence to support the use of CSR in assessing the competence of practicing physicians, its use for certification of physicians has diminished due to practical concerns, such as cost, time, and the need for experienced assessors.10,11,16,23
In the context of the new accreditation system and the milestones, CSR provides 2 meaningful contributions to the assessment of residents. First, inquiry focused on the specific case allows assessment of the learner's clinical decision making in a controlled, yet authentic, setting.24 Second, the formative feedback that a learner receives on a one-to-one basis provides individualized learning opportunities. CSR can fill a gap in the systematic assessment of clinical decision making; thus, a critical analysis of this assessment method is warranted.
Validity Threats Due to Construct Underrepresentation
Construct underrepresentation refers to the incorrect interpretation of test results based on inadequate sampling of that which is being measured.25 Examples of construct underrepresentation issues as they relate to CSR are outlined in the table. Construct underrepresentation is common in all clinical performance assessments,26 and may be overcome by increasing the representativeness of cases relative to an assessment blueprint.27 However, simply administering larger numbers of CSR sessions may not be feasible due to practical limitations. For example, if an average-sized internal medicine residency program has 64 residents who are examined 3 times a year with 20-minute encounters, then administering CSR will require approximately 64 hours of personnel time annually, excluding time for preparation and feedback.
TABLE.
Threats to Validity of Chart-Stimulated Recall (CSR)
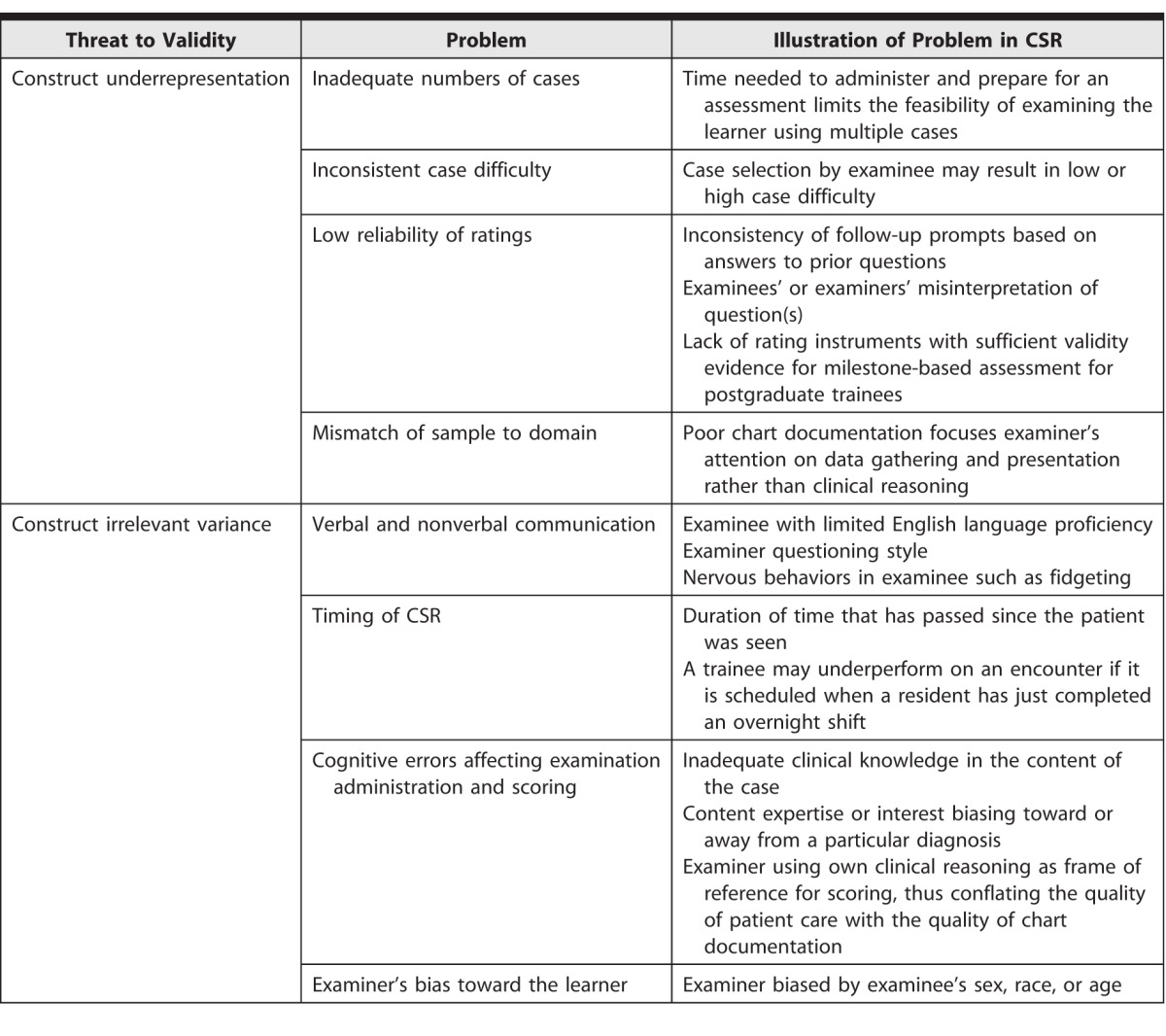
Case difficulty may additionally contribute to construct underrepresentation. Selection of straightforward cases that pose minimal challenges to clinical decision making, or complex cases selected for the purposes of receiving corrective instruction, may result in higher or lower ratings.
The format of the examination may also contribute to construct underrepresentation. Although open-ended questions provide evaluators some autonomy to probe examinees, such questions are also subject to interpretation, resulting in potential discrepancies between test administrations.28,29 In addition, there is considerable variation in available rating instruments and a paucity of recommendations for how to conduct rater training. There are no CSR rating instruments with validity evidence to use for generating scores in a milestone framework. Thus, this limits the ability of CCCs to interpret the results in the context of milestone-based assessments.
Validity Threats Due to Construct Irrelevant Variance
Construct irrelevant variance refers to external factors that contribute to systematic error of a measurement. While some construct irrelevant variance is unavoidable in any workplace-based assessments, CSR appears to be more prone to such errors because of the interactive nature of the examination. In particular, verbal and nonverbal communication may affect assessor scoring.30 For example, a non–native English-speaking resident may struggle to answer a question rapidly because of language challenges. An evaluator may misinterpret this delay as an indication of weak clinical decision-making skills.28,31,32 Furthermore, styles of questioning vary between evaluators. Learners may view some styles as overly aggressive, leading to heightened anxiety and nervous behaviors.33–35 Finally, an evaluator may harbor subconscious biases toward the learner based on age, sex, or ethnicity, among others.
Evaluators' cognitive biases and clinical knowledge may affect both administration of the CSR and examination scoring.36,37 Evaluators must have high levels of competence and familiarity with the clinical subject matter. Moreover, the evaluator's area of clinical expertise may alter the examination. For example, when faced with a case of dyspnea, a cardiologist may gravitate toward a diagnosis of congestive heart failure and lead the questioning in this direction, while a pulmonologist may gravitate toward emphysema. Therefore, it is possible that raters' markings of the learner are influenced by a bias toward a particular diagnosis.
The reliance on chart documentation creates another potential source of construct irrelevant variance. Poor chart documentation may divert an evaluator's attention away from clinical decision making and toward clinical documentation, effectively converting CSR into an assessment of the resident's documentation skills.
Recommendations
The various threats to validity we have described prevent the use of CSR as a single assessment measure for high-stakes summative assessment decisions. However, CSR can play a useful role as part of multiple sources of assessment for CCC decisions regarding resident performance. CSR's contribution, by facilitating the assessment of learners' clinical decision-making skills and allowing the provision of individualized feedback, is important and may not be captured in other assessment methods. CSRs are interactive, decoupled from the daily time pressures of clinical care, allowing for structured reflection on one's practice. Furthermore, CSR provides a venue for trainees to receive individualized face-to-face instruction, feedback, and assessment from an experienced clinician. In order to fully realize the potential of CSR, it is essential to pay close attention to the development of the instrument, the training of evaluators, and the preparation of examinees.38
An important step toward improving the quality of CSR assessment is robust faculty development in 2 areas: (1) how to conduct the examination, and (2) how to select the content to be examined. To mitigate rater (evaluator) cognitive errors, faculty development should include measures to ensure that raters' clinical knowledge is up-to-date. Recommendations for future research to enhance the quality of CSR are displayed in the box.
box Future Directions for Investigation
-
•
Determining the optimal frequency and timing of chart-stimulated recall assessments to ensure adequate interrater reliability and to minimize construct underrepresentation
-
•
Developing standardized prompts to minimize construct irrelevant variance due to variations in rater questioning
-
•
Developing a defensible scoring rubric and composite score interpretation
-
•
Studying the impact of evaluator training
-
•
Identifying how cases should be selected
-
•
Improving the feasibility of the examination process
-
•
Measuring the impact of feedback on trainees' performance
Summary
CSR is a promising assessment method that provides important feedback to learners and can inform CCC deliberations, yet additional research is needed before it can be used for summative assessments in GME. Clarity and recommendations for mitigating threats to the validity of CSR are still largely lacking—answers to these challenges will help health profession educators determine how CSR should fit into an assessment system in the new accreditation system and its relative benefit to opportunity cost with respect to other assessment methods. Faculty rater development for CSR assessment is an important element of improving the validity and utility of this tool.
Footnotes
Shalini T. Reddy, MD, is Professor of Internal Medicine, University of Chicago Pritzker School of Medicine, and Associate Program Director, Internal Medicine Residency, Mercy Hospital Chicago; Justin Endo, MD, is Assistant Professor, Department of Dermatology, University of Wisconsin; Shanu Gupta, MD, is Assistant Professor and Director of Education, Rush University Hospitalists; Ara Tekian, PhD, MHPE, is Professor and Director of the International Program, Department of Medical Education, University of Illinois at Chicago; and Yoon Soo Park, PhD, is Assistant Professor, Department of Medical Education, University of Illinois at Chicago.
References
- 1.Nasca TJ. ACGME initiatives in concert with Institute of Medicine recommendations. J Grad Med Educ. 2014;6(4):809–810. doi: 10.4300/JGME-06-04-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Nasca TJ, Philibert I, Brigham T, Flynn TC. The next GME accreditation system—rationale and benefits. N Engl J Med. 2012;366(11):1051–1056. doi: 10.1056/NEJMsr1200117. [DOI] [PubMed] [Google Scholar]
- 3.Swing SR, Clyman SG, Holmboe ES, Williams RG. Advancing resident assessment in graduate medical education. J Grad Med Educ. 2009;1(2):278–286. doi: 10.4300/JGME-D-09-00010.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Carraccio CL, Benson BJ, Nixon LJ, Derstine PL. From the educational bench to the clinical bedside: translating the Dreyfus developmental model to the learning of clinical skills. Acad Med. 2008;83(8):761–767. doi: 10.1097/ACM.0b013e31817eb632. [DOI] [PubMed] [Google Scholar]
- 5.Dreyfus HL, Dreyfus SE. Mind Over Machine. New York, NY: Simon and Schuster;; 2000. [Google Scholar]
- 6.Carraccio C, Sectish TC. Report of colloquium II: the theory and practice of graduate medical education—how do we know when we have made a “good doctor”? Pediatrics. 2009;123(suppl 1):17–21. doi: 10.1542/peds.2008-1578F. [DOI] [PubMed] [Google Scholar]
- 7.Schuwirth L. From structured, standardized assessment to unstructured assessment in the workplace. J Grad Med Educ. 2014;6(1):165–166. doi: 10.4300/JGME-D-13-00416.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Goulet F, Jacques A, Gagnon R, Bourbeau D, Laberge D, Melanson J, et al. Performance assessment: family physicians in Montreal meet the mark! Can Fam Physician. 2002;48:1337–1344. [PMC free article] [PubMed] [Google Scholar]
- 9.Hayden SR, Dufel S, Shih R. Definitions and competencies for practice-based learning and improvement. Acad Emerg Med. 2002;9(11):1242–1248. doi: 10.1111/j.1553-2712.2002.tb01584.x. [DOI] [PubMed] [Google Scholar]
- 10.Miller PA, Nayer M, Eva KW. Psychometric properties of a peer-assessment program to assess continuing competence in physical therapy. Phys Ther. 2010;90(7):1026–1038. doi: 10.2522/ptj.20080137. [DOI] [PubMed] [Google Scholar]
- 11.Schipper S, Ross S. Structured teaching and assessment: a new chart-stimulated recall worksheet for family medicine residents. Can Fam Physician. 2010;56(9):958–959. e352–e354. [PMC free article] [PubMed] [Google Scholar]
- 12.Maatsch JL, Krome RL, Sprafka S, Maclean CB. The Emergency Medicine Specialty Certification Examination (EMSCE) JACEP. 1976;5(7):529–534. doi: 10.1016/s0361-1124(76)80289-4. [DOI] [PubMed] [Google Scholar]
- 13.Maatsch JL. Assessment of clinical competence on the Emergency Medicine Specialty Certification Examination: the validity of examiner ratings of simulated clinical encounters. Ann Emerg Med. 1981;10(10):504–507. doi: 10.1016/s0196-0644(81)80003-0. [DOI] [PubMed] [Google Scholar]
- 14.Maatsch JL, Huang R. An evaluation of the construct validity of four alternative theories of clinical competence. Res Med Educ. 1986;25:69–74. [PubMed] [Google Scholar]
- 15.Munger BS, Krome RL, Maatsch JC, Podgorny G. The certification examination in emergency medicine: an update. Ann Emerg Med. 1982;11(2):91–96. doi: 10.1016/s0196-0644(82)80304-1. [DOI] [PubMed] [Google Scholar]
- 16.Salvatori P, Baptiste S, Ward M. Development of a tool to measure clinical competence in occupational therapy: a pilot study? Can J Occup Ther. 2000;67(1):51–60. doi: 10.1177/000841740006700108. [DOI] [PubMed] [Google Scholar]
- 17.Carraccio C, Burke AE. Beyond competencies and milestones: adding meaning through context. J Grad Med Educ. 2010;2(3):419–422. doi: 10.4300/JGME-D-10-00127.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Norman GR, Davis DA, Lamb S, Hanna E, Caulford P, Kaigas T. Competency assessment of primary care physicians as part of a peer review program. JAMA. 1993;270(9):1046–1051. [PubMed] [Google Scholar]
- 19.Academy of Medical Royal Colleges. Improving Assessment, 2009. http://www.aomrc.org.uk/doc_view/49-improving-assessment. Accessed May 11, 2015. [Google Scholar]
- 20.Williamson J, Osborne A. Critical analysis of case based discussions. BJMP. 2012;5(2):a514. [Google Scholar]
- 21.Mehta F, Brown J, Shaw NJ. Do trainees value feedback in case-based discussion assessments? Med Teach. 2013;35(5):e1166–e1172. doi: 10.3109/0142159X.2012.731100. [DOI] [PubMed] [Google Scholar]
- 22.Jennett P, Affleck L. Chart audit and chart stimulated recall as methods of needs assessment in continuing professional health education. J Cont Educ Health. 1998;18(3):163–171. [Google Scholar]
- 23.Cunnington JP, Hanna E, Turnhbull J, Kaigas TB, Norman GR. Defensible assessment of the competency of the practicing physician. Acad Med. 1997;72(1):9–12. [PubMed] [Google Scholar]
- 24.Chaudhry SI, Holmboe E, Beasley BW. The state of evaluation in internal medicine residency. J Gen Intern Med. 2008;23(7):1010–1015. doi: 10.1007/s11606-008-0578-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Downing SM. Validity: on the meaningful interpretation of assessment data. Med Educ. 2003;37(9):830–837. doi: 10.1046/j.1365-2923.2003.01594.x. [DOI] [PubMed] [Google Scholar]
- 26.Norcini JJ. Current perspectives in assessment: the assessment of performance at work. Med Educ. 2005;39(9):880–889. doi: 10.1111/j.1365-2929.2005.02182.x. [DOI] [PubMed] [Google Scholar]
- 27.Downing SM, Haladyna TM. Validity threats: overcoming interference with proposed interpretations of assessment data. Med Educ. 2004;38(3):327–333. doi: 10.1046/j.1365-2923.2004.01777.x. [DOI] [PubMed] [Google Scholar]
- 28.Memon MA, Joughin GR, Memon B. Oral assessment and postgraduate medical examinations: establishing conditions for validity, reliability and fairness. Adv Health Sci Educ Theory Pract. 2010;15(2):277–289. doi: 10.1007/s10459-008-9111-9. [DOI] [PubMed] [Google Scholar]
- 29.Turnbull J, Danoff D, Norman G. Content specificity and oral certification examinations. Med Educ. 1996;30(1):56–59. doi: 10.1111/j.1365-2923.1996.tb00718.x. [DOI] [PubMed] [Google Scholar]
- 30.Burchard KW, Rowland-Morin PA, Coe N, Garb JL. A surgery oral examination: interrater agreement and the influence of rater characteristics. Acad Med. 1995;70(11):1044–1046. doi: 10.1097/00001888-199511000-00026. [DOI] [PubMed] [Google Scholar]
- 31.Roberts C, Sarangi S, Southgate L, Wakeford R, Wass V. Oral examinations-equal opportunities, ethnicity, and fairness in the MRCGP. BMJ. 2000;320(7231):370–375. doi: 10.1136/bmj.320.7231.370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wakeford R, Southgate L, Wass V. Improving oral examinations: selecting, training, and monitoring examiners for the MRCGP. Royal College of General Practitioners. BMJ. 1995;311(7010):931–935. doi: 10.1136/bmj.311.7010.931. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Weingarten M, Polliack M, Tabenkin H, Kahan E. Variations among examiners in family medicine residency board oral examinations. Med Educ. 2000;34(1):13–17. doi: 10.1046/j.1365-2923.2000.00408.x. [DOI] [PubMed] [Google Scholar]
- 34.Thomas CS, Mellsop G, Callender K, Crawshaw J, Ellis PM, Hall A, et al. The oral examination: a study of academic and non-academic factors. Med Educ. 1993;27(5):433–439. doi: 10.1111/j.1365-2923.1993.tb00297.x. [DOI] [PubMed] [Google Scholar]
- 35.Rowland-Morin PA, Burchard KW, Garb JL, Coe NP. Influence of effective communication by surgery students on their oral examination scores. Acad Med. 1991;66(3):169–171. doi: 10.1097/00001888-199103000-00011. [DOI] [PubMed] [Google Scholar]
- 36.Gingerich A, Kogan J, Yeates P, Govaerts M, Holmboe E. Seeing the “black box” differently: assessor cognition from three research perspectives. Med Educ. 2014;48(11):1055–1068. doi: 10.1111/medu.12546. [DOI] [PubMed] [Google Scholar]
- 37.Kogan JR, Conforti LN, Iobst WF, Holmboe ES. Reconceptualizing variable rater assessments as both an educational and clinical care problem. Acad Med. 2014;89(5):721–727. doi: 10.1097/ACM.0000000000000221. [DOI] [PubMed] [Google Scholar]
- 38.Raj JM, Thorn PM. A faculty development program to reduce rater error on milestone-based assessments. J Grad Med Educ. 2014;6(4):680–685. doi: 10.4300/JGME-D-14-00161.1. [DOI] [PMC free article] [PubMed] [Google Scholar]


