You are an attending physician in the medical intensive care unit and receive a call from the charge nurse. She tells you that the senior resident has been unable to place the central line that was discussed on rounds. You call the resident to get more information. The resident tells you that he has had multiple opportunities to place a central line with limited success. You are particularly stunned, not only because you assume that every postgraduate year 3 resident should be able to place a central line without direct supervision, but also because this resident has demonstrated outstanding knowledge of pulmonary physiology and ventilator management. With this realization, what are the implications for your program's teaching and supervision paradigms?
The Accreditation Council for Graduate Medical Education (ACGME) Common Program Requirements place significant emphasis on supervision of residents and codify the levels of supervision,1 yet offer little guidance on identification of the level of supervision for any particular task or skill. Many program leaders have expressed frustration when attempting to construct a conceptual model for supervision in the context of progressive responsibility.
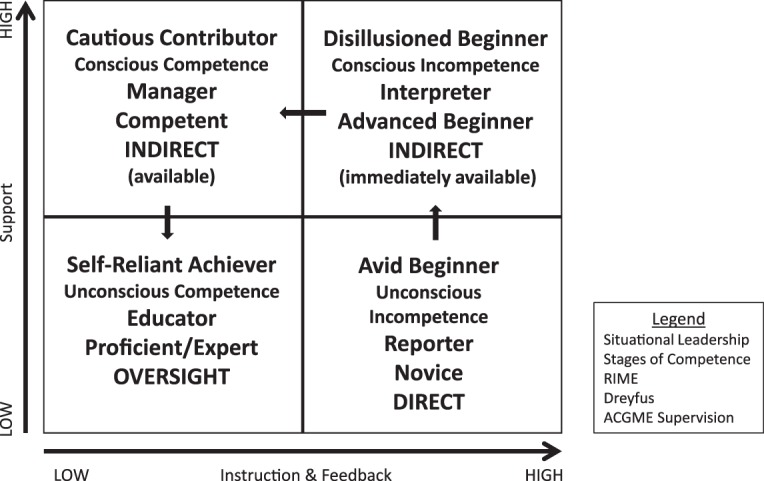
In this perspective, we review several models of learning and skill development: the Hersey-Blanchard Situational Leadership model,2 the Stages of Competence model,3 the RIME model,4 and the Dreyfus model.5 We demonstrate that these models provide a structured framework for conceptualizing supervision of residents at various stages in their development, which parallel the ACGME concept of progressive responsibility. Our aim is to provide readers with models to help guide the design of a supervision structure for their programs that both categorizes residents at each level of supervision and operationalizes that supervision for faculty.
The Situational Leadership Model
The Situational Leadership model was described by Paul Hersey in the 1980s2 and by Ken Blanchard in the 1990s.2 The model (figure 1) presents 4 levels of learner development: avid beginner, disillusioned beginner, reluctant learner/cautious contributor, and expert/self-reliant achiever.
FIGURE 1.
Supervision Model
Avid beginners are described as motivated, enthusiastic, and excited about the opportunity to do something new. This individual is already motivated, requiring only limited “support” from his or her supervisor. With disillusioned beginners, the initial excitement has worn off, and some aspects of learning have proved more difficult than originally anticipated. At this stage, learners need performance feedback that is sincere, specific, and timely, with acknowledgment of progress toward the desired goal. Cautious contributors can successfully complete a task, but have not had sufficient time to gain confidence in their abilities. Supervisors need to encourage learners at this stage to repeat their performance, while still being available to observe demonstrations by others. Self-reliant achievers have demonstrated competence and commitment, and have essentially become self-managed.
According to this model, the resident in this scenario is a self-reliant achiever in ventilator management, but a disillusioned beginner in the line placement task.
The Stages of Competence Model
The Stages of Competence model (figure 1) was introduced by Noel Burch in the 1970s.3 Similar to the Situational Leadership model, learners in the Stages of Competence model fall into 1 of 4 stages: unconscious incompetence, conscious incompetence, conscious competence, or unconscious competence. Conceptually, the Stages of Competence and the Situational Leadership models are parallel.
The Stages of Competence model implies that all learners proceed in a sequential, somewhat predictable, fashion through the 4 stages. At the unconscious incompetence stage, the individual does not understand or know how to do something, and does not necessarily recognize the deficit. Conscious incompetence is when the learner does not understand or know how to do something, but now he or she recognizes the deficit. Conscious competence is when the individual understands or knows how to do something; however, demonstrating the knowledge or skill requires concentration. At the level of unconscious competence, the individual has had so much practice with the skill that it requires little thought and can be performed while executing other tasks such as teaching.
In this model, the resident is at the level of unconscious competence in ventilator management but is consciously incompetent in line placement.
The RIME Model
Many readers are familiar with Pangaro's RIME model4 (figure 1), which describes 4 levels of learners: reporter, interpreter, manager, and educator. Reporters can identify most clinical information but do not integrate it with their basic science knowledge to formulate a diagnosis. Interpreters can identify the information and articulate the problem. Managers can identify the problem and design a therapeutic plan. Finally, educators can perform all of the functions above, and identify and share novel approaches for accomplishing the task.
The resident here is an educator in ventilator management, but a reporter in performing line placements.
The Dreyfus Model
The Dreyfus model was first introduced as a 5-stage model of skill acquisition.5 The stages are as follows: novice, advanced beginner, competent, proficient, and expert. These stages are eloquently described in an article by Carraccio et al6 and excerpted below.
Novices use analytic reasoning and rules to link cause and effect, with little ability to filter or prioritize information. Synthesis is difficult, and the big picture is elusive. Advanced beginners use both analytic reasoning and pattern recognition to solve problems, and are able to abstract from concrete and specific information to more general aspects of a problem. At the level of competent, learners see the big picture, yet complex or uncommon problems still require reliance on analytic reasoning. Proficient learners still need to occasionally fall back to methodical and analytic reasoning for managing problems. Finally, experts are open to notice the unexpected and are perceptive in discriminating features that do not fit a recognizable pattern. The first 4 stages described in the Dreyfus model parallel the 4 stages of all the previously described models (figure 1).
In this model, the resident is proficient in ventilator management, but an advanced beginner in line placement.
Developing a Structured Model of Supervision
The 4 models presented describe learners as they progress through stages of development, and to some degree, suggest the type of instruction, feedback, and support appropriate for each stage. We propose that supervision can be operationalized as instruction, feedback, and support. The synthesis of the models can help us identify the level of supervision necessary for each stage. In addition, the 4 models can define what supervision should look like at each level (figure 1). For example, the avid beginner/unconsciously incompetent/reporter/novice learner requires direct supervision with high levels of feedback and instruction. In contrast, the self-reliant/unconsciously competent/educator/proficient learner would only require oversight with minimal ongoing feedback and instruction. Accordingly, from a sampling of different skill acquisition models, we can describe what a learner should look like to determine what level of supervision is required. In addition, we can operationalize the characteristics of the supervision.
In our scenario, the resident has characteristics of a disillusioned beginner and a novice learner, suggesting a need for direct supervision and instruction in line placement. At the same time, his knowledge of ventilator management suggests he needs only oversight. Accordingly, learners need varying levels of supervision for different areas of competence, and identifying competencies based on postgraduate year level becomes less relevant.
The next step in this process (using the specialty-specific milestones as a foundation) would be for each specialty to reach a consensus about what a resident should look like in each quadrant of the composite model for skills and content areas in that specialty. Figure 2 illustrates an example using the skills from our scenario. A similar schema could be developed for each skill or milestone. This would give program directors the necessary tools to determine what level of supervision their learners need, and how best to supervise them, based on an analysis of each individual's learning and the skill or competency being taught. These frameworks create multiple research opportunities to further describe optimal supervision.
FIGURE 2.
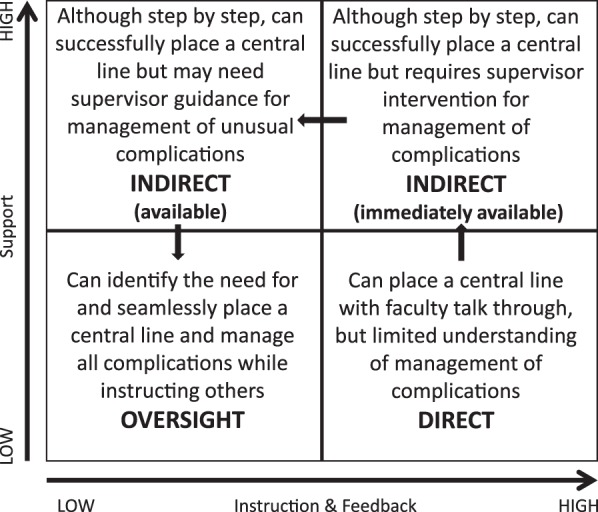
Supervision of Central Line Insertion
Footnotes
Both authors are at the University of Texas Health Science Center at San Antonio. Jennifer L. Peel, PhD, is Assistant Dean for Graduate Medical Education and Professor, Anesthesiology; and Robert J. Nolan, MD, is Associate Dean for Graduate Medical Education and Associate Chair, Pediatrics.
References
- 1.Accreditation Council for Graduate Medical Education. ACGME Common Program Requirements. 2015 http://www.acgme.org/acgmeweb/Portals/0/PFAssets/ProgramRequirements/CPRs2013.pdf. Accessed June 22. [Google Scholar]
- 2.Leadership-Central.com. Hersey-Blanchard Situational Leadership Theory. 2015 http://www.leadership-central.com/situational-leadership-theory.html#axzz3OpFIn2L3. Accessed July 31. [Google Scholar]
- 3.Adams L. Gordon Training International. Learning a new skill is easier said than done. 2015 http://www.gordontraining.com/free-workplace-articles/learning-a-new-skill-is-easier-said-than-done. Accessed July 31. [Google Scholar]
- 4.Pangaro L. A new vocabulary and other innovations for improving descriptive in-training evaluations. Acad Med. 1999;74(11):1203–1207. doi: 10.1097/00001888-199911000-00012. [DOI] [PubMed] [Google Scholar]
- 5.Dreyfus H, Dreyfus S. A Five-Stage Model of the Mental Activities Involved in Direct Skill Acquisition: Operations Research Center Report. Berkeley: University of California Press;; 1980. [Google Scholar]
- 6.Carraccio CL, Benson BJ, Nixon LJ, Derstine PL. From the educational bench to the clinical bedside: translating the Dreyfus Development Model to the learning of clinical skills. Acad Med. 2008;83(8):761–767. doi: 10.1097/ACM.0b013e31817eb632. [DOI] [PubMed] [Google Scholar]


