Abstract
Background
Although the resident candidate interview is costly and time-consuming for both applicants and programs, it is considered critically important for resident selection. Noncognitive attributes, including communication skills and professionalism, can be assessed by the personal interview.
Objective
We conducted a review of the literature on the residency interview to identify the interview characteristics used for resident selection and to ascertain to what extent the interview yields information that predicts future performance.
Methods
We searched PubMed and Scopus using the following search terms: residency, internship, interview, selection, and performance. We extracted information on characteristics of the interview process, including type of interview format, measures taken to minimize bias by interviewers, and testing of other clinical/surgical skills.
Results
We identified 104 studies that pertained to the resident selection interview, with highly varied interview formats and assessment tools. A positive correlation was demonstrated between a medical school academic record and the interview, especially for unblinded interview formats. A total of 34 studies attempted to correlate interview score with performance in residency, with mixed results. We also identified a number of studies that included personality testing, clinical skills testing, or surgical skills testing.
Conclusions
Our review identified a wide variety of approaches to the selection interview and a range of factors that have been studied to assess its effectiveness. More research needs to be done not only to address and ascertain appropriate interview formats that predict positive performance in residency, but also to determine interview factors that can predict both residents' “success” and program attrition.
Editor's Note: The online version of this article contains a list of the data extracted for each article.
Introduction
The year 2014 marked a record high of 26 678 postgraduate year (PGY)-1 positions offered in the United States. To achieve a Match rate of 96%, 17 374 US medical school seniors ranked a median of 11.5 programs, and often ranked more than 1 specialty.1 Residency programs screen large numbers of applications for a limited number of interview slots, and the residency selection process creates a significant expense for both applicants and programs. A recent survey of plastic surgery applicants found that interview costs ranged from $2,500 to $10,000,2 excluding the academic “cost” of lost days of medical education. The cost to residency programs is multifactorial, with the mean cost of recruiting 1 PGY-1 position estimated at $9,899.3
The screening, interview, and ranking processes are critical, as applicant selection has enduring consequences for the programs. Ideally, an applicant should be a good “fit” for the program, with a high likelihood of success and a low likelihood of problems. Poor performance in residency may require remediation, and resident attrition has been reported to be as high as 22% to 27% in general surgery programs,4–6 which can create significant workflow issues, reduce morale, and have a negative impact on future recruitment.
Academic qualifications of candidates are accessible via the electronic residency application service (ERAS) and include United States Medical Licensing Examination (USMLE) scores, clerkship and preclinical grades, and class rank. Although readily available, there is wide variation in grading, class rank, and academic honors among medical schools. Studies of the use of academic data in predicting future performance have produced mixed results. A recent meta-analysis of factors showed that examination-based selection strategies (eg, USMLE Step 1) had a strong positive association with in-service training examinations, whereas medical school grades had a less robust association with subjective outcomes such as resident performance evaluations.7 USMLE Part 1 may even have a negative correlation with future clinical performance and professionalism.8 Attributes such as leadership and professionalism are not assessable through standardized testing, but may be evident in a review of the curriculum vitae, personal statement, dean's letter, and letters of recommendation. A combination of cognitive and noncognitive factors was shown in 1979 by Keck et al9 to be the most predictive of postgraduate clinical performance compared with any individual variable, and it is unlikely that this paradigm has changed 36 years later.
The interview process allows for assessment of noncognitive factors, such as interpersonal and communication skills, maturity, interest in the field, dependability, and honesty.10,11 Program directors reported that the interview is the most important factor in determining resident selection.11–20 The interview may also identify negative applicant characteristics such as anxiety or aggression.21 Candidates value the interview process highly,22,23 and cite the quality of interactions with the program director24 and, most important, with the residents25–27 during the interview as important in their decision making. Applicants value the interaction with residents during an interview to assess resident morale,28 esprit de corps,29 and program “red flags” as perceived by applicants.30 Ultimately, program directors and residents have reported that their “gut feeling” is important in creating their respective rank lists.29,31
The resident selection interview also has been criticized for its “dubious value,”32 due to the lack of a standardized approach and low interrater reliability.27 During the interview, there is a strong potential for a “halo effect,” in which interviewers' prior knowledge about an applicant's academic record (grades, test scores) affect the outcome.33 Additionally, the interview can be a venue for unethical questioning regarding applicants' marital status, reproductive plans, and health, especially by faculty without adequate training.34–36
Given the high cost of the resident interview and its importance in resident selection, this review attempts to identify data-driven strategies to optimize resident interview processes. The objectives were (1) to identify interview characteristics utilized by residency programs to evaluate candidates for selection; (2) to establish a relationship between the interview score and applicant characteristics and rank-order position in blinded and unblinded interview formats; and (3) to examine associations between applicant interviews and trainee/physician performance.
Methods
Identifying and reviewing articles that met inclusion criteria involved 2 phases. During the first phase, we conducted a pilot search of articles to develop a data abstraction tool. This initial search yielded 107 articles in PubMed, using medical subject heading (MeSH) terms such as internship and residency, interviews as topic/methods, and personnel selection covering the period between 1966 and 2013. The tool was developed by a research team member (S.K.), with 1 revision after the pilot phase. A kappa value of 0.80 (for accuracy of data abstraction) was attained across 3 research team members (S.K., S.O., A.M.) who reviewed 5 articles. Subsequently, the team reviewed all 30 articles and completed the data abstraction tool with the addition of 2 added researchers (B.H., S.C.). A list of the data extracted for each article is provided as online supplemental material.
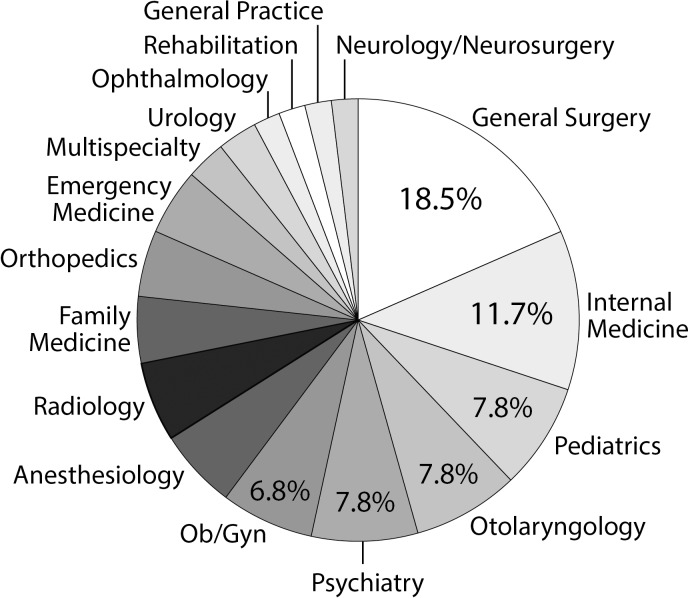
The second review phase involved an expanded search of articles with consultation from a health sciences librarian. A search for English-language articles from 1966 through October 2014 in PubMed used the following terms: (1) internship and residency (MeSH terms), (2) interview, and (3) selection or performance. The search strategy was repeated in Scopus, and we also reviewed references of identified articles. Figure 1 illustrates the article selection process. A full-text review of 264 articles was performed, which included the initial 30 studies. We excluded review articles, surveys of program directors or applicants, letters to the editor, and commentaries. Forty-seven additional articles focused on other aspects of resident selection and did not include data on the residency interview. A total of 104 articles contained program-level data on the interview processes for resident selection or as a predictor of future performance. The lead author (A.S-F.) completed the review of all 104 articles using the review process established during phase 1. Data analysis was performed using Stata version 13 (StataCorp LP) to generate descriptive statistics.
FIGURE 1.
Selection Process for Included Studies
For the type of interview structure, we defined traditional or unstructured interviewing as the use of academic criteria and curricula vitae to generate questions that the interviewer determined to be relevant to the applicants' credentials. In contrast, structured interviews used predefined questions established by the selection committee prior to the interview and posed to all applicants. Behavioral interviews (also referred to as accomplishment interviews) are a type of structured interview in which applicants are asked to describe a past experience to provide an example of when they demonstrated characteristics desirable to the residency program. Multiple mini interviews include a timed circuit of stations to assess skills, including interpersonal communication, professionalism, and ethics.
Results
Interview Characteristics
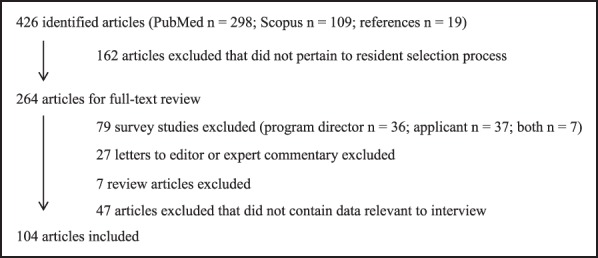
Of the 104 articles, 91 (88%) were from the United States or Canada; the remainder were from the United Kingdom (n = 8), Australia, Ireland, Thailand, and the United Arab Emirates. The specialties studied in the reviewed articles are shown in figure 2. Table 1 reports the key results of studies. Studies were predominantly single institution studies. Less than half (46%, 48 of 104) of the articles reported the interview format. Of the studies that provided data on the interview format, 54% (26 of 48) described using web- or video-based skills testing or multiple mini formats, 31% (15 of 48) reported a structured (including behavioral) interview, and 15% (7 of 48) used a traditional or unstructured format.
FIGURE 2.
Distribution of Specialties
TABLE 1.
Characteristics of Interviews (n = 104)
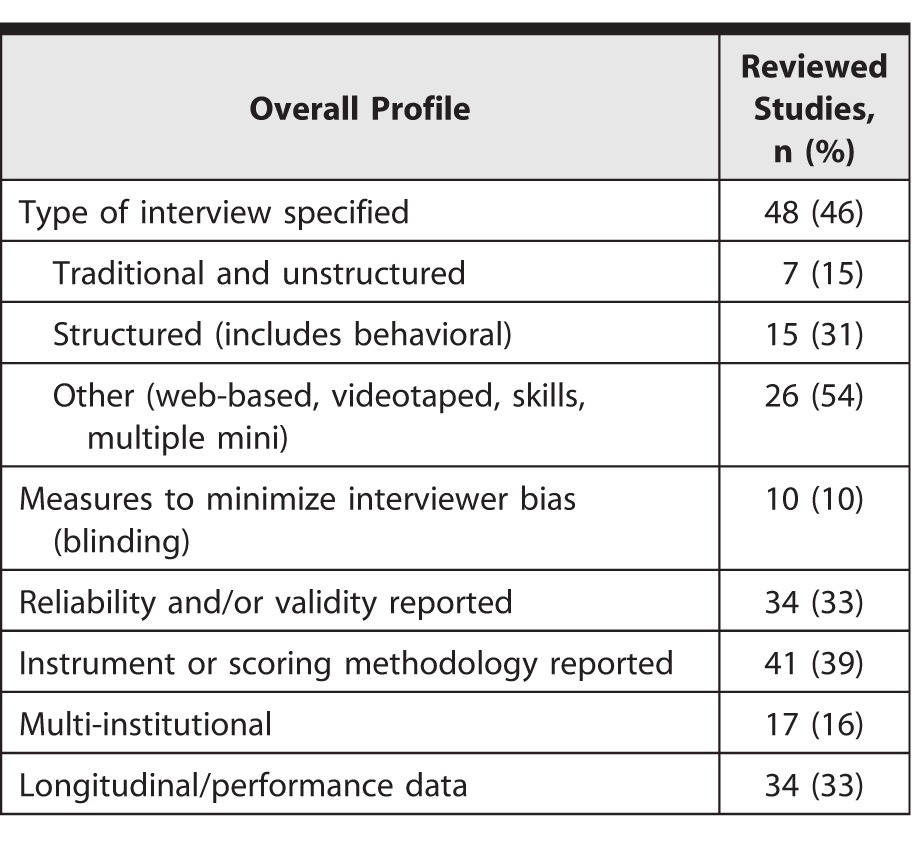
We found that most studies lacked substantial information regarding the scope and the format of the interview, the steps taken to reduce possible interview biases, and the psychometric evidence associated with the interview instrument, such as reliability and validity. Only one-third of studies tracked resident performance over time. The type and number of interviewers were not consistently reported. For studies that included this information, in addition to physician faculty, interviewers comprised of residents (n = 20), PhD faculty (n = 2), psychologists (n = 3), or other health professionals (n = 4).
Correlational Studies
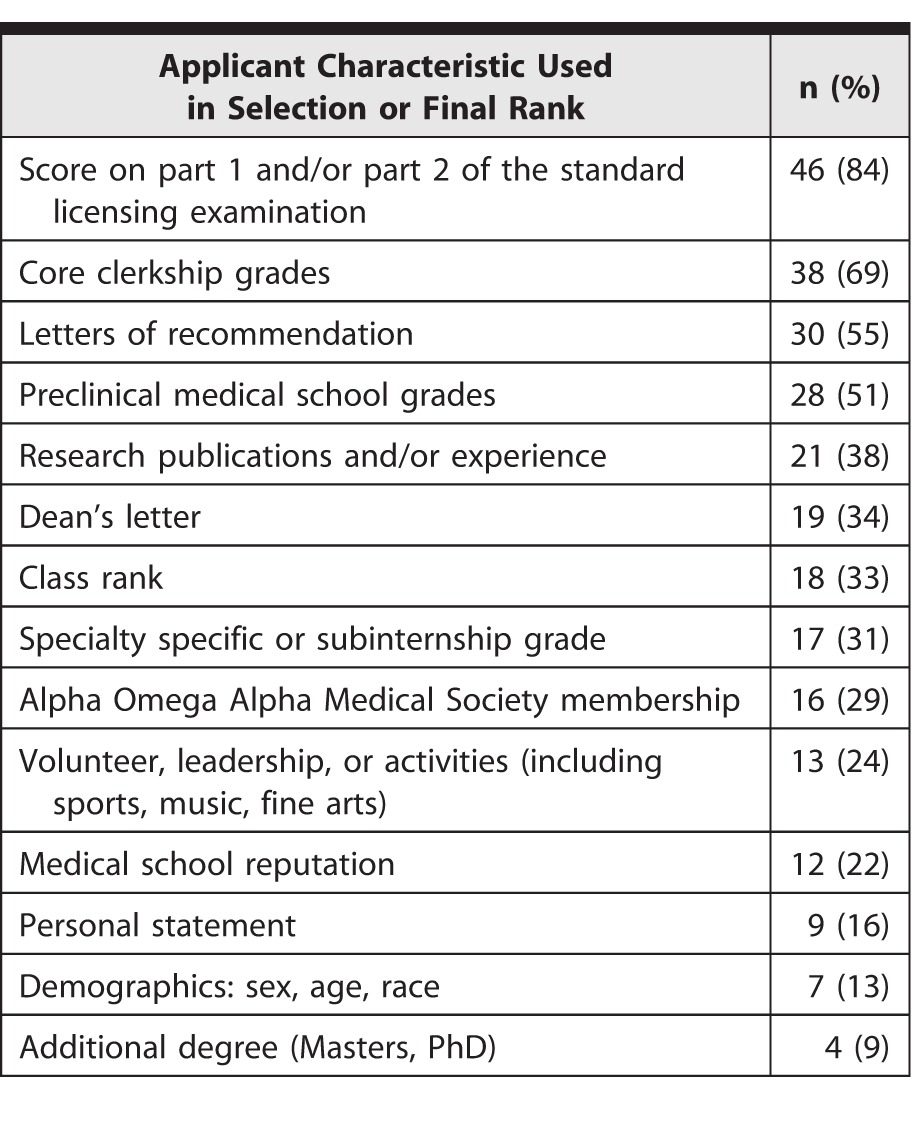
Studies frequently reported on the relationship of the interview score with academic criteria (USMLE, transcript, class rank, Alpha Omega Alpha Honor Medical Society, research publications), final rank, or match results. The cognitive and noncognitive criteria most commonly cited in studies as components of the final rank are shown in table 2. Many studies demonstrated a positive correlation among interview score, academic data, and final rank.32,37–43 One study found that the interview could so closely correlate with academic variables that the R2 values for final rank and preinterview academic rank were unchanged whether the interview score was added to the model or not.44 Three studies showed that the interview significantly changed the rank of some applicants, moving them both higher and lower (> 10 positions) than their preinterview rank.37,38,45 In a study using an interview format based on the CanMEDS competency-based framework (Communicator, Collaborator, Manager, Professional, Health Advocate, Medical Expert, Scholar), poor correlation was found between the interview and academic record, suggesting the interview was measuring factors other than academic performance.46
TABLE 2.
Selection Criteria Reported by 55 Studies (53%)
Blinding Interviewers
Studies that evaluated the effect of blinding of interviewers to reduce bias consistently showed that an open or unblinded file resulted in higher interviewer ratings.33,42,47–49 Unblinded interviews correlated more closely to USMLE Step 1 scores,33,42,48 whereas 2 studies where interviewers were blinded to the applicant's academic record found a negative correlation with USMLE scores.33,42 One study found that 30% of the variance in interview scores was due to interviewer bias and concluded that unblinded interview scores were influenced significantly by other variables (USMLE scores, transcript, class rank, Alpha Omega Alpha), minimizing the weight of the interview in resident selection.47
Performance
Thirty-four studies attempted to evaluate whether the interview predicted performance. Outcomes studied included (1) clinical evaluations during residency by program directors, faculty, and/or chief residents; (2) global evaluation or ranking of residents; (3) in-training examination results; (4) attrition; or (5) problems with professionalism in residency or subsequently in their careers. The duration of follow-up ranged from 7 to 12 months for those outcomes that were assessed during the course of internship,50–53 and from 36 to 60 months for outcomes in residency. Results from these studies varied. Of the 34 studies (table 3), 17 showed that the interview did not predict subsequent clinical performance (weak positive, negative, or no correlation) in internship or residency, particularly with a traditional or unstructured interview format.41,50,53–67 Eleven studies showed a positive correlation between interview and subsequent performance.8,51,52,68–75 Performance metrics with a positive correlation included clinical evaluations, in-training examinations, licensing board examinations, and a composite score or rank of resident performance. Attrition from residency was not consistently predicted by the interview process in the 6 studies that assessed this variable.4–6,43,55,56 In a case control study of psychiatry residents, minor or major problems during residency may have only been associated with negative comments in the dean's letter and were not picked up in the interview.76 A longitudinal study from 1965 to 1999 showed that neither the residency interview nor the performance evaluations in a psychiatry program predicted long-term professionalism issues, resulting in referral to an impaired physician program.77
TABLE 3.
Prediction of Performance
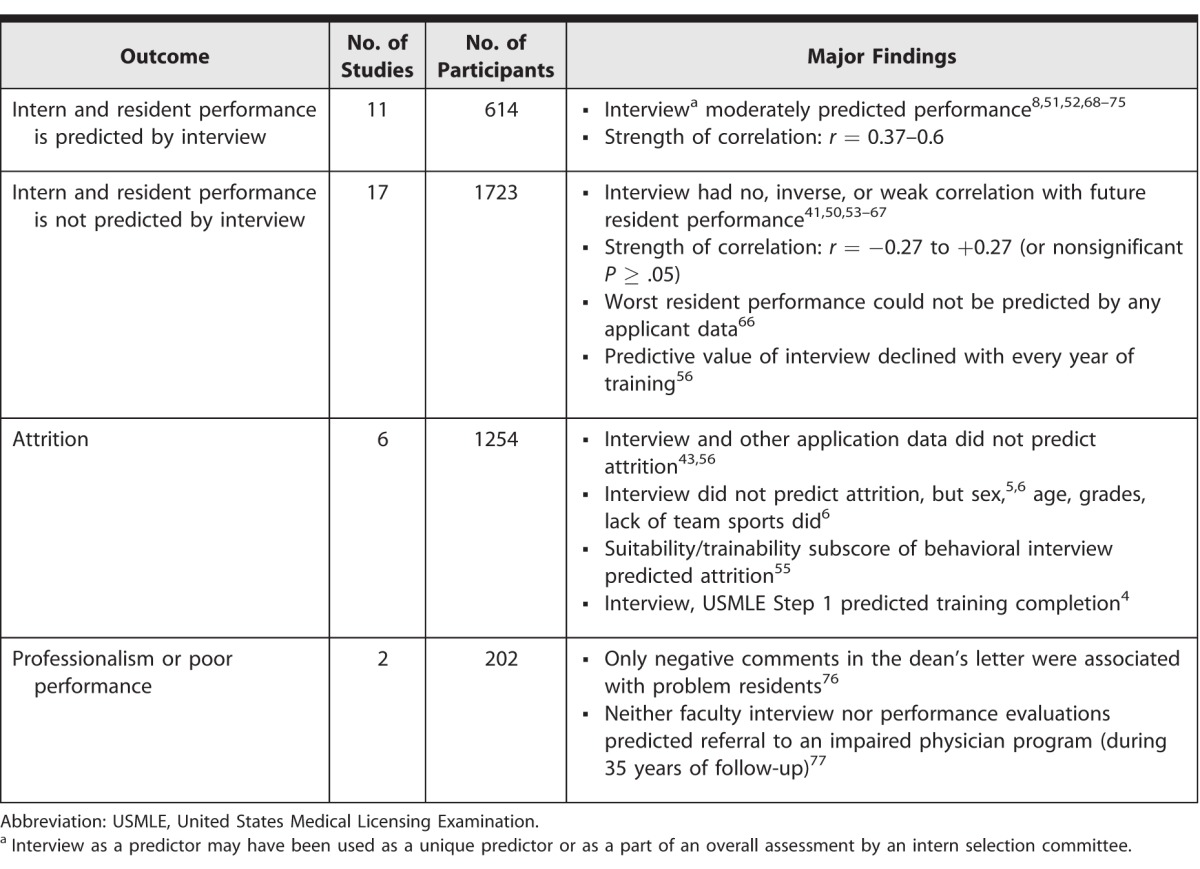
The behavioral or accomplishment interview was more predictive of subsequent residency performance evaluation than the traditional interview or other academic variables.54 Although 1 study did not find a correlation between the overall behavioral interview score and resident performance, a subscore for suitability/trainability was negatively associated with attrition.55 In another study, components of the accomplishment interview correlated with specific resident behaviors such as confidence with interpersonal skills (r = 0.38) or recognition of personal limits (r = −0.46).75
Clinical and Surgical Skills
The 7 studies that included an assessment of surgical skills as part of the interview or selection process showed mixed results.78–84 A soap carving task as part of an otolaryngology residency interview was not predictive of cognitive knowledge, visuospatial ability, manual dexterity, decision making, or overall resident performance.82 The use of surgical skills testing at an otolaryngology residency interview did not correlate with USMLE Step 1 scores,78 although in a larger cohort, it was predictive of faculty performance evaluation.79
Assessment of clinical skills in the form of an objective structured clinical examination or a multiple mini interview (MMI) to assess competencies desired by the program has been described for individual programs and regional assessment centers for selection of residents. Many of the studies examining validity evidence for the MMIs or multiple station interviews were identified in this review (MMI70,85–91 and competency center71,92–98). Several studies showed a positive correlation between multiple station interviews and future clinical examination testing.70,71,95 A study of the use of the MMI for emergency medicine interns at 3 institutions found that the results did not correlate with clerkship grades, medical school quality, or USMLE scores, but did correlate with emergency medicine clerkship grades. This suggests that the MMI may measure abilities that contribute to success in the specialty.91
Personality Testing
Eight studies explored the use of personality99–103 or emotional intelligence104–106 testing as part of resident selection. Use of the Myers-Briggs personality inventory for interviewers and applicants demonstrated that clinician faculty ranked candidates more favorably when they shared certain personality styles.103 Bohm et al106 evaluated a moral reasoning assessment tool in orthopedic resident applicants and found no association between moral reasoning and resident rank or USMLE scores.
Discussion
Our comprehensive review shows the complexity of the interview process in resident selection. The scope of this review, which included a broad range of medical and surgical specialties, provides an overview of the diverse characteristics of the interview in historical and contemporary resident selection. It suggests that the interview process varies greatly among programs and specialties, with regard to the assessment of interview format, logistics, characteristics of interviewers, and noncognitive skills.
Although 34 studies attempted to establish a relationship between the interview and future performance, the results are mixed as to whether the interview itself, or the interview combined with other data used in the application, predicted future “success” or “problems” for residency applicants. It was not possible to determine whether a specific interview format is superior for predicting performance.
It would be informative if selection strategies could predict subsequent resident performance, but quality data are limited and mixed. This is partly due to the lack of useful performance outcomes and limited power in small studies. Thus, longitudinal and multi-institution studies of performance during and after residency with clinically meaningful performance measures are needed to fully assess the predictability of various interview techniques or academic records. With improved specialty-specific trainee assessment tools, program directors may have a common language to assess overall performance and design interview processes that could predict more long-term physician success.
Gordon and Lincoln27 criticized the traditional interview for poor inter-interviewer reliability, content that varies from applicant to applicant, interviewer bias from stereotypes or idiosyncratic rapport, and the fact that questions may be anticipated or rehearsed by the applicant, resulting in a skewed view of an applicant's values and motivation. The box shows a series of recommendations to improve the reliability and value of the resident interview as a selection tool.
box Attributes of the Resident Interview That Improve Reliability
-
1
Explicit written description of the desired traits in an applicant/resident
-
2
Standardized questions to every applicant
-
3
Provision of behavior-specific anchors for rating scales for interviewers and using a scoring rubric to improve interrater and intrarater scoring
-
4
Use of multiple observers rather than a single interviewer
-
5
Training of interviewers in the format and scoring and including unethical and “illegal” question rules
-
6
Blinding of the interviewer to cognitive application data to minimize bias107
In the future, if the regional interview fair108 or web-based conference interview109,110 has additional evidence of validity, this may diminish the expense of interviewing to both programs and applicants. The major drawback will be the lack of interactions with resident and staff that an onsite interview provides.
This review has 2 limitations. The first is the heterogeneity of the source articles, which do not consistently report many of the variables of interest to the authors, limiting the ability to make interpretation of findings across studies. Additionally, a single author reviewed all included studies, which could have introduced bias in the data abstraction and conclusions raised in this study.
Conclusion
The interview in resident selection often is used to assess noncognitive factors and can provide information to assess the mutual fit of the applicant and the program. Ideally, the interview contributes to the final rank list by systematically assessing specialty-specific personal qualities, skills, and competencies. However, the selection interview does not predict clinical performance, problems with professionalism, or resident attrition. The predictive value of the interview may be limited due to “halo effects,” as interviewers base their assessment of candidates on academic criteria, especially in unblinded formats. Although there is insufficient evidence to recommend an optimal interview format to predict future performance, use of the unstructured, unblinded interview should be replaced with a more rigorous interview strategy.
Supplementary Material
Footnotes
Alyssa Stephenson-Famy, MD, is Assistant Professor and Associate Ob-Gyn Residency Program Director, University of Washington; Brenda S. Houmard, MD, PhD, is Associate Physician, SRM Spokane; Sidharth Oberoi, BS, is Co-Founder/President, Zaniac; Anton Manyak, BS, is a Medical Student, University of Vermont College of Medicine; Seine Chiang, MD, is Professor and Ob-Gyn Residency Program Director, University of Washington; and Sara Kim, PhD, is Research Professor and Associate Dean for Educational Quality Improvement, University of Washington.
Funding: The authors report no external funding source for this study.
Conflict of interest: The authors declare they have no competing interests.
This study was presented at the Council on Resident Education in Obstetrics and Gynecology and Association of Professors of Gynecology and Obstetrics Annual Meeting, in San Antonio, Texas, March 9–12, 2011.
References
- 1.National Resident Matching Program. Charting outcomes in the match. 2014 5th ed. http://www.nrmp.org/wp-content/uploads/2014/09/Charting-Outcomes-2014-Final.pdf. Accessed July 21, 2015. [Google Scholar]
- 2.Wood JS, David LR. Outcome analysis of factors impacting the plastic surgery match. Ann Plast Surg. 2010;64(6):770–774. doi: 10.1097/SAP.0b013e3181b4bcf5. [DOI] [PubMed] [Google Scholar]
- 3.Brummond A, Sefcik S, Halvorsen AJ, Chaudhry S, Arora V, Adams M, et al. Resident recruitment costs: a national survey of internal medicine program directors. Am J Med. 2013;126(7):646–653. doi: 10.1016/j.amjmed.2013.03.018. [DOI] [PubMed] [Google Scholar]
- 4.Alterman DM, Jones TM, Heidel RE, Daley BJ, Goldman MH. The predictive value of general surgery application data for future resident performance. J Surg Educ. 2011;68(6):513–518. doi: 10.1016/j.jsurg.2011.07.007. [DOI] [PubMed] [Google Scholar]
- 5.Kelz RR, Mullen JL, Kaiser LR, Pray LA, Shea GP, Drebin JA, et al. Prevention of surgical resident attrition by a novel selection strategy. Ann Surg. 2010;252(3):537–541. doi: 10.1097/SLA.0b013e3181f27a50. discussion 541–543. [DOI] [PubMed] [Google Scholar]
- 6.Naylor RA, Reisch JS, Valentine RJ. Factors related to attrition in surgery residency based on application data. Arch Surg. 2008;143(7):647–651. doi: 10.1001/archsurg.143.7.647. discussion 651–652. [DOI] [PubMed] [Google Scholar]
- 7.Kenny S, McInnes M, Singh V. Associations between residency selection strategies and doctor performance: a meta-analysis. Med Educ. 2013;47(8):790–800. doi: 10.1111/medu.12234. [DOI] [PubMed] [Google Scholar]
- 8.Brothers TE, Wetherholt S. Importance of the faculty interview during the resident application process. J Surg Educ. 2007;64(6):378–385. doi: 10.1016/j.jsurg.2007.05.003. [DOI] [PubMed] [Google Scholar]
- 9.Keck JW, Arnold L, Willoughby L, Calkins V. Efficacy of cognitive/noncognitive measures in predicting resident-physician performance. J Med Educ. 1979;54(10):759–765. doi: 10.1097/00001888-197910000-00002. [DOI] [PubMed] [Google Scholar]
- 10.LaGrasso JR, Kennedy DA, Hoehn JG, Ashruf S, Przybyla AM. Selection criteria for the integrated model of plastic surgery residency. Plast Reconstr Surg. 2008;121(3):121e–125e. doi: 10.1097/01.prs.0000299456.96822.1b. [DOI] [PubMed] [Google Scholar]
- 11.Wagoner NE, Suriano JR, Stoner JA. Factors used by program directors to select residents. J Med Educ. 1986;61(1):10–21. doi: 10.1097/00001888-198601000-00002. [DOI] [PubMed] [Google Scholar]
- 12.Wagoner NE, Gray GT. Report on a survey of program directors regarding selection factors in graduate medical education. J Med Educ. 1979;54(6):445–452. doi: 10.1097/00001888-197906000-00001. [DOI] [PubMed] [Google Scholar]
- 13.Wagoner NE, Suriano JR. Program directors' responses to a survey on variables used to select residents in a time of change. Acad Med. 1999;74(1):51–58. [PubMed] [Google Scholar]
- 14.Melendez MM, Xu X, Sexton TR, Shapiro MJ, Mohan EP. The importance of basic science and clinical research as a selection criterion for general surgery residency programs. J Surg Educ. 2008;65(2):151–154. doi: 10.1016/j.jsurg.2007.08.009. [DOI] [PubMed] [Google Scholar]
- 15.Hirthler MA, Glick PL, Hassett JM, Jr, Cooney DR. Evaluation of the pediatric surgical matching program by the directors of pediatric surgical training programs. J Pediatr Surg. 1994;29(10):1370–1374. doi: 10.1016/0022-3468(94)90118-x. [DOI] [PubMed] [Google Scholar]
- 16.Makdisi G, Takeuchi T, Rodriguez J, Rucinski J, Wise L. How we select our residents—a survey of selection criteria in general surgery residents. J Surg Educ. 2011;68(1):67–72. doi: 10.1016/j.jsurg.2010.10.003. [DOI] [PubMed] [Google Scholar]
- 17.DeLisa JA, Jain SS, Campagnolo DI. Factors used by physical medicine and rehabilitation residency training directors to select their residents. Am J Phys Med Rehabil. 1994;73(3):152–156. doi: 10.1097/00002060-199406000-00002. [DOI] [PubMed] [Google Scholar]
- 18.Galazka SS, Kikano GE, Zyzanski S. Methods of recruiting and selecting residents for US family practice residencies. Acad Med. 1994;69(4):304–306. doi: 10.1097/00001888-199404000-00015. [DOI] [PubMed] [Google Scholar]
- 19.Nallasamy S, Uhler T, Nallasamy N, Tapino PJ, Volpe NJ. Ophthalmology resident selection: current trends in selection criteria and improving the process. Ophthalmology. 2010;117(5):1041–1047. doi: 10.1016/j.ophtha.2009.07.034. [DOI] [PubMed] [Google Scholar]
- 20.Taylor CA, Weinstein L, Mayhew HE. The process of resident selection: a view from the residency director's desk. Obstet Gynecol. 1995;85(2):299–303. doi: 10.1016/0029-7844(94)00388-T. [DOI] [PubMed] [Google Scholar]
- 21.Al Khalili K, Chalouhi N, Tjoumakaris S, Gonzalez LF, Starke RM, Rosenwasser R, et al. Programs selection criteria for neurological surgery applicants in the United States: a national survey for neurological surgery program directors. World Neurosurg. 2014;81(3–4):473–477.e2. doi: 10.1016/j.wneu.2013.08.019. [DOI] [PubMed] [Google Scholar]
- 22.Puscas L, Sharp SR, Schwab B, Lee WT. Qualities of residency applicants: comparison of otolaryngology program criteria with applicant expectations. Arch Otolaryngol Head Neck Surg. 2012;138(1):10–14. doi: 10.1001/archoto.2011.214. [DOI] [PubMed] [Google Scholar]
- 23.Simmonds AC, Robbins JM, Brinker MR, Rice JC, Kerstein MD. Factors important to students in selecting a residency program. Acad Med. 1990;65(10):640–643. doi: 10.1097/00001888-199010000-00009. [DOI] [PubMed] [Google Scholar]
- 24.Deiorio NM, Yarris LM, Gaines SA. Emergency medicine residency applicant views on the interview day process. Acad Emerg Med. 2009;16(suppl 2):67–70. doi: 10.1111/j.1553-2712.2009.00602.x. [DOI] [PubMed] [Google Scholar]
- 25.Schlitzkus LL, Schenarts PJ, Schenarts KD. It was the night before the interview: perceptions of resident applicants about the preinterview reception. J Surg Educ. 2013;70(6):750–757. doi: 10.1016/j.jsurg.2013.05.008. [DOI] [PubMed] [Google Scholar]
- 26.Love JN, Howell JM, Hegarty CB, McLaughlin SA, Coates WC, Hopson LR, et al. Factors that influence medical student selection of an emergency medicine residency program: implications for training programs. Acad Emerg Med. 2012;19(4):455–460. doi: 10.1111/j.1553-2712.2012.01323.x. [DOI] [PubMed] [Google Scholar]
- 27.Gordon MJ, Lincoln JA. Family practice resident selection: value of the interview. J Fam Pract. 1976;3(2):175–177. [PubMed] [Google Scholar]
- 28.Aagaard EM, Julian K, Dedier J, Soloman I, Tillisch J, Perez-Stable EJ. Factors affecting medical students' selection of an internal medicine residency program. J Natl Med Assoc. 2005;97(9):1264–1270. [PMC free article] [PubMed] [Google Scholar]
- 29.Parker AM, Petroze RT, Schirmer BD, Calland JF. Surgical residency market research—what are applicants looking for? J Surg Educ. 2013;70(2):232–236. doi: 10.1016/j.jsurg.2012.09.002. [DOI] [PubMed] [Google Scholar]
- 30.Yousuf SJ, Kwagyan J, Jones LS. Applicants' choice of an ophthalmology residency program. Ophthalmology. 2013;120(2):423–427. doi: 10.1016/j.ophtha.2012.07.084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Otero HJ, Erturk SM, Ondategui-Parra S, Ros PR. Key criteria for selection of radiology residents: results of a national survey. Acad Radiol. 2006;13(9):1155–1164. doi: 10.1016/j.acra.2006.06.012. [DOI] [PubMed] [Google Scholar]
- 32.Prager JD, Myer CM, 4th, Hayes KM, Myer CM, 3rd, Pensak ML. Improving methods of resident selection. Laryngoscope. 2010;120(12):2391–2398. doi: 10.1002/lary.21022. [DOI] [PubMed] [Google Scholar]
- 33.Smilen SW, Funai EF, Bianco AT. Residency selection: should interviewers be given applicants' board scores? Am J Obstet Gynecol. 2001;184(3):508–513. doi: 10.1067/mob.2001.109868. [DOI] [PubMed] [Google Scholar]
- 34.Slone RM. Resident selection: Part 3. The interview. Invest Radiol. 1991;26(4):396–399. doi: 10.1097/00004424-199104000-00027. [DOI] [PubMed] [Google Scholar]
- 35.Hern HG, Jr, Alter HJ, Wills CP, Snoey ER, Simon BC. How prevalent are potentially illegal questions during residency interviews? Acad Med. 2013;88(8):1116–1121. doi: 10.1097/ACM.0b013e318299eecc. [DOI] [PubMed] [Google Scholar]
- 36.Thurman RJ, Katz E, Carter W, Han J, Kayala E, McCoin N, et al. Emergency medicine residency applicant perceptions of unethical recruiting practices and illegal questioning in the match. Acad Emerg Med. 2009;16(6):550–557. doi: 10.1111/j.1553-2712.2009.00413.x. [DOI] [PubMed] [Google Scholar]
- 37.Christakis PG, Christakis TJ, Dziura J, Christakis JT. Role of the interview in admissions at the University of Toronto ophthalmology program. Can J Ophthalmol. 2010;45(5):527–530. doi: 10.3129/i10-041. [DOI] [PubMed] [Google Scholar]
- 38.Collins M, Curtis A, Artis K, Staib L, Bokhari J. Comparison of two methods for ranking applicants for residency. J Am Coll Radiol. 2010;7(12):961–966. doi: 10.1016/j.jacr.2010.06.020. [DOI] [PubMed] [Google Scholar]
- 39.Curtis DJ, Riordan DD, Cruess DF, Brower AC. Selecting radiology resident candidates. Invest Radiol. 1989;24(4):324–330. doi: 10.1097/00004424-198904000-00012. [DOI] [PubMed] [Google Scholar]
- 40.Davis JL, Platt LD, Sandhu M, Shapiro F. Evaluating factors in the selection of residents. Acad Med. 1995;70(3):176–177. doi: 10.1097/00001888-199503000-00004. [DOI] [PubMed] [Google Scholar]
- 41.Kandler H, Plutchik R, Conte H, Siegel B. Prediction of performance of psychiatric residents: a three-year follow-up study. Am J Psychiatry. 1975;132(12):1286–1290. doi: 10.1176/ajp.132.12.1286. [DOI] [PubMed] [Google Scholar]
- 42.Miles WS, Shaw V, Risucci D. The role of blinded interviews in the assessment of surgical residency candidates. Am J Surg. 2001;182(2):143–146. doi: 10.1016/s0002-9610(01)00668-7. [DOI] [PubMed] [Google Scholar]
- 43.Scott-Conner CEH, Rhodes RS, Aggarwal AK, Bass J. Selecting residents for a surgical residency: Are we doing what we say we are doing? Current Surgery. 1997;54(1):42–46. [Google Scholar]
- 44.Young MJ, Woolliscroft JO, Holloway JJ. Determining the policies of a residency selection committee. J Med Educ. 1986;61(10):835–837. doi: 10.1097/00001888-198610000-00009. [DOI] [PubMed] [Google Scholar]
- 45.Gong H, Jr, Parker NH, Apgar FA, Shank C. Influence of the interview on ranking in the residency selection process. Med Educ. 1984;18(5):366–369. doi: 10.1111/j.1365-2923.1984.tb01284.x. [DOI] [PubMed] [Google Scholar]
- 46.Hamel P, Boisjoly H, Corriveau C, Fallaha N, Lahoud S, Luneau K, et al. Using the CanMEDS roles when interviewing for an ophthalmology residency program. Can J Ophthalmol. 2007;42(2):299–304. [PubMed] [Google Scholar]
- 47.Robin AP, Bombeck CT, Pollak R, Nyhus LM. Introduction of bias in residency-candidate interviews. Surgery. 1991;110(2):253–258. [PubMed] [Google Scholar]
- 48.Swanson DB, Sawhill A, Holtzman KZ, Bucak SD, Morrison C, Hurwitz S, et al. Relationship between performance on part I of the American Board of Orthopaedic Surgery certifying examination and scores on USMLE steps 1 and 2. Acad Med. 2009;84(suppl 10):21–24. doi: 10.1097/ACM.0b013e3181b37fd2. [DOI] [PubMed] [Google Scholar]
- 49.Hauge LS, Stroessner SJ, Chowdhry S, Wool NL. Association for Surgical Education. Evaluating resident candidates: does closed file review impact faculty ratings? Am J Surg. 2007;193(6):761–765. doi: 10.1016/j.amjsurg.2007.01.020. [DOI] [PubMed] [Google Scholar]
- 50.Part HM, Markert RJ. Predicting the first-year performances of international medical graduates in an internal medicine residency. Acad Med. 1993;68(11):856–858. [PubMed] [Google Scholar]
- 51.Khongphatthanayothin A, Chongsrisawat V, Wananukul S, Sanpavat S. Resident recruitment: what are good predictors for performance during pediatric residency training? J Med Assoc Thai. 2002;85(suppl 1):302–311. [PubMed] [Google Scholar]
- 52.Olawaiye A, Yeh J, Withiam-Leitch M. Resident selection process and prediction of clinical performance in an obstetrics and gynecology program. Teach Learn Med. 2006;18(4):310–315. doi: 10.1207/s15328015tlm1804_6. [DOI] [PubMed] [Google Scholar]
- 53.Komives E, Weiss ST, Rosa RM. The applicant interview as a predictor of resident performance. J Med Educ. 1984;59(5):425–426. doi: 10.1097/00001888-198405000-00009. [DOI] [PubMed] [Google Scholar]
- 54.Altmaier EM, Smith WL, O'Halloran CM, Franken EA., Jr The predictive utility of behavior-based interviewing compared with traditional interviewing in the selection of radiology residents. Invest Radiol. 1992;27(5):385–389. doi: 10.1097/00004424-199205000-00013. [DOI] [PubMed] [Google Scholar]
- 55.Strand EA, Moore E, Laube DW. Can a structured, behavior-based interview predict future resident success? Am J Obstet Gynecol. 2011;204(5):446.e1–446.e13. doi: 10.1016/j.ajog.2011.02.019. [DOI] [PubMed] [Google Scholar]
- 56.Dubovsky SL, Gendel MH, Dubovsky AN, Levin R, Rosse J, House R. Can admissions interviews predict performance in residency? Acad Psychiatry. 2008;32(6):498–503. doi: 10.1176/appi.ap.32.6.498. [DOI] [PubMed] [Google Scholar]
- 57.Bell JG, Kanellitsas I, Shaffer L. Selection of obstetrics and gynecology residents on the basis of medical school performance. Am J Obstet Gynecol. 2002;186(5):1091–1094. doi: 10.1067/mob.2002.121622. [DOI] [PubMed] [Google Scholar]
- 58.Bent JP, Colley PM, Zahtz GD, Smith RV, Parikh SR, Schiff B, et al. Otolaryngology resident selection: do rank lists matter? Otolaryngol Head Neck Surg. 2011;144(4):537–541. doi: 10.1177/0194599810396604. [DOI] [PubMed] [Google Scholar]
- 59.Borowitz SM, Saulsbury FT, Wilson WG. Information collected during the residency match process does not predict clinical performance. Arch Pediatr Adolesc Med. 2000;154(3):256–260. doi: 10.1001/archpedi.154.3.256. [DOI] [PubMed] [Google Scholar]
- 60.Chole RA, Ogden MA. Predictors of future success in otolaryngology residency applicants. Arch Otolaryngol Head Neck Surg. 2012;138(8):707–712. doi: 10.1001/archoto.2012.1374. [DOI] [PubMed] [Google Scholar]
- 61.Daly KA, Levine SC, Adams GL. Predictors for resident success in otolaryngology. J Am Coll Surg. 2006;202(4):649–654. doi: 10.1016/j.jamcollsurg.2005.12.006. [DOI] [PubMed] [Google Scholar]
- 62.Dawkins K, Ekstrom RD, Maltbie A, Golden RN. The relationship between psychiatry residency applicant evaluations and subsequent residency performance. Acad Psychiatry. 2005;29(1):69–75. doi: 10.1176/appi.ap.29.1.69. [DOI] [PubMed] [Google Scholar]
- 63.Oldfield Z, Beasley SW, Smith J, Anthony A, Watt A. Correlation of selection scores with subsequent assessment scores during surgical training. ANZ J Surg. 2013;83(6):412–416. doi: 10.1111/ans.12176. [DOI] [PubMed] [Google Scholar]
- 64.Metro DG, Talarico JF, Patel RM, Wetmore AL. The resident application process and its correlation to future performance as a resident. Anesth Analg. 2005;100(2):502–505. doi: 10.1213/01.ANE.0000154583.47236.5F. [DOI] [PubMed] [Google Scholar]
- 65.McGreevy JM, Kollmorgen DR. Medical school performance does not predict success in a surgery residency. Curr Surg. 1997;54(7):438–441. [Google Scholar]
- 66.Fryer JP, Corcoran N, George B, Wang E, Darosa D. Does resident ranking during recruitment accurately predict subsequent performance as a surgical resident? J Surg Educ. 2012;69(6):724–730. doi: 10.1016/j.jsurg.2012.06.010. [DOI] [PubMed] [Google Scholar]
- 67.George JM, Young D, Metz EN. Evaluating selected internship candidates and their subsequent performances. Acad Med. 1989;64(8):480–482. doi: 10.1097/00001888-198908000-00013. [DOI] [PubMed] [Google Scholar]
- 68.Geissler J, VanHeest A, Tatman P, Gioe T. Aggregate Interview Method of ranking orthopedic applicants predicts future performance. Orthopedics. 2013;36(7):e966–e970. doi: 10.3928/01477447-20130624-30. [DOI] [PubMed] [Google Scholar]
- 69.Grewal SG, Yeung LS, Brandes SB. Predictors of success in a urology residency program. J Surg Educ. 2013;70(1):138–143. doi: 10.1016/j.jsurg.2012.06.015. [DOI] [PubMed] [Google Scholar]
- 70.Eva KW, Reiter HI, Trinh K, Wasi P, Rosenfeld J, Norman GR. Predictive validity of the multiple mini-interview for selecting medical trainees. Med Educ. 2009;43(8):767–775. doi: 10.1111/j.1365-2923.2009.03407.x. [DOI] [PubMed] [Google Scholar]
- 71.Thordarson DB, Ebramzadeh E, Sangiorgio SN, Schnall SB, Patzakis MJ. Resident selection: how we are doing and why? Clin Orthop Relat Res. 2007;(459):255–259. doi: 10.1097/BLO.0b013e31805d7eda. [DOI] [PubMed] [Google Scholar]
- 72.Ozuah PO. Predicting residents' performance: a prospective study. BMC Med Educ. 2002;2:7. doi: 10.1186/1472-6920-2-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Shiroma PR, Alarcon RD. Selection factors among international medical graduates and psychiatric residency performance. Acad Psychiatry. 2010;34(2):128–131. doi: 10.1176/appi.ap.34.2.128. [DOI] [PubMed] [Google Scholar]
- 74.Warrick SS, Crumrine RS. Predictors of success in an anesthesiology residency. J Med Educ. 1986;61(7):591–595. doi: 10.1097/00001888-198607000-00007. [DOI] [PubMed] [Google Scholar]
- 75.Wood PS, Smith WL, Altmaier EM, Tarico VS, Franken EA., Jr A prospective study of cognitive and noncognitive selection criteria as predictors of resident performance. Invest Radiol. 1990;25(7):855–859. doi: 10.1097/00004424-199007000-00018. [DOI] [PubMed] [Google Scholar]
- 76.Brenner AM, Mathai S, Jain S, Mohl PC. Can we predict “problem residents”? Acad Med. 2010;85(7):1147–1151. doi: 10.1097/ACM.0b013e3181e1a85d. [DOI] [PubMed] [Google Scholar]
- 77.Dubovsky SL, Gendel M, Dubovsky AN, Rosse J, Levin R, House R. Do data obtained from admissions interviews and resident evaluations predict later personal and practice problems? Acad Psychiatry. 2005;29(5):443–447. doi: 10.1176/appi.ap.29.5.443. [DOI] [PubMed] [Google Scholar]
- 78.Carlson ML, Archibald DJ, Sorom AJ, Moore EJ. Under the microscope: assessing surgical aptitude of otolaryngology residency applicants. Laryngoscope. 2010;120(6):1109–1113. doi: 10.1002/lary.20914. [DOI] [PubMed] [Google Scholar]
- 79.Moore EJ, Price DL, Van Abel KM, Carlson ML. Still under the microscope: can a surgical aptitude test predict otolaryngology resident performance? Laryngoscope. 2015;125(2):e57–e61. doi: 10.1002/lary.24791. [DOI] [PubMed] [Google Scholar]
- 80.Krespi YP, Levine TM, Einhorn RK, Mitrani M. Surgical aptitude test for otolaryngology-head and neck surgery resident applicants. Laryngoscope. 1986;96(11):1201–1206. doi: 10.1002/lary.1986.96.11.1201. [DOI] [PubMed] [Google Scholar]
- 81.Panait L, Larios JM, Brenes RA, Francher TT, Ajemian MS, Dudrick SJ, et al. Surgical skills assessment of applicants to general surgery residency. J Surg Res. 2011;170(2):189–194. doi: 10.1016/j.jss.2011.04.006. [DOI] [PubMed] [Google Scholar]
- 82.Tang CG, Hilsinger RL, Jr, Cruz RM, Schloegel LJ, Byl FM, Jr, Rasgon BM. Manual dexterity aptitude testing: a soap carving study. JAMA Otolaryngol Head Neck Surg. 2014;140(3):243–249. doi: 10.1001/jamaoto.2013.6456. [DOI] [PubMed] [Google Scholar]
- 83.Gallagher AG, Leonard G, Traynor OJ. Role and feasibility of psychomotor and dexterity testing in selection for surgical training. ANZ J Surg. 2009;79(3):108–113. doi: 10.1111/j.1445-2197.2008.04824.x. [DOI] [PubMed] [Google Scholar]
- 84.Gallagher AG, Neary P, Gillen P, Lane B, Whelan A, Tanner WA, et al. Novel method for assessment and selection of trainees for higher surgical training in general surgery. ANZ J Surg. 2008;78(4):282–290. doi: 10.1111/j.1445-2197.2008.04439.x. [DOI] [PubMed] [Google Scholar]
- 85.Ahmed A, Qayed KI, Abdulrahman M, Tavares W, Rosenfeld J. The multiple mini-interview for selecting medical residents: first experience in the Middle East region. Med Teach. 2014;36(8):703–709. doi: 10.3109/0142159X.2014.907875. [DOI] [PubMed] [Google Scholar]
- 86.Campagna-Vaillancourt M, Manoukian J, Razack S, Nguyen LH. Acceptability and reliability of multiple mini interviews for admission to otolaryngology residency. Laryngoscope. 2014;124(1):91–96. doi: 10.1002/lary.24122. [DOI] [PubMed] [Google Scholar]
- 87.Dore KL, Kreuger S, Ladhani M, Rolfson D, Kurtz D, Kulasegaram K, et al. The reliability and acceptability of the Multiple Mini-Interview as a selection instrument for postgraduate admissions. Acad Med. 2010;85(suppl 10):60–63. doi: 10.1097/ACM.0b013e3181ed442b. [DOI] [PubMed] [Google Scholar]
- 88.Finlayson HC, Townson AF. Resident selection for a physical medicine and rehabilitation program: feasibility and reliability of the multiple mini-interview. Am J Phys Med Rehabil. 2011;90(4):330–335. doi: 10.1097/PHM.0b013e31820f9677. [DOI] [PubMed] [Google Scholar]
- 89.Hofmeister M, Lockyer J, Crutcher R. The acceptability of the multiple mini interview for resident selection. Fam Med. 2008;40(10):734–740. [PubMed] [Google Scholar]
- 90.Hofmeister M, Lockyer J, Crutcher R. The multiple mini-interview for selection of international medical graduates into family medicine residency education. Med Educ. 2009;43(6):573–579. doi: 10.1111/j.1365-2923.2009.03380.x. [DOI] [PubMed] [Google Scholar]
- 91.Hopson LR, Burkhardt JC, Stansfield RB, Vohra T, Turner-Lawrence D, Losman ED. The multiple mini-interview for emergency medicine resident selection. J Emerg Med. 2014;46(4):537–543. doi: 10.1016/j.jemermed.2013.08.119. [DOI] [PubMed] [Google Scholar]
- 92.Brown CA, Wakefield SE, Bullock AD. The selection of GP trainees in the West Midlands: audit of assessment centre scores by ethnicity and country of qualification. Med Teach. 2001;23(6):605–609. doi: 10.1080/01421590120091069. [DOI] [PubMed] [Google Scholar]
- 93.Brown CA, Wakefield SE, Bullock AD. The selection of GP trainees in the West Midlands: second audit of assessment centre scores by ethnicity and country of qualification. Med Teach. 2003;25(6):649–653. doi: 10.1080/0142159031000137445. [DOI] [PubMed] [Google Scholar]
- 94.Onyon C, Wall D, Goodyear HM. Reliability of multi-station interviews in selection of junior doctors for specialty training. Med Teach. 2009;31(7):665–667. doi: 10.1080/01421590802578236. [DOI] [PubMed] [Google Scholar]
- 95.Randall R, Davies H, Patterson F, Farrell K. Selecting doctors for postgraduate training in paediatrics using a competency based assessment centre. Arch Dis Child. 2006;91(5):444–448. doi: 10.1136/adc.2005.076653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Randall R, Stewart P, Farrell K, Patterson F. Using an assessment centre to select doctors for postgraduate training in obstetrics and gynaecology. Obstet Gynaecol. 2006;8(4):257–262. [Google Scholar]
- 97.Rao R. The Structured Clinically Relevant Interview for Psychiatrists in Training (SCRIPT): a new standardized assessment tool for recruitment in the UK. Acad Psychiatry. 2007;31(6):443–446. doi: 10.1176/appi.ap.31.6.443. [DOI] [PubMed] [Google Scholar]
- 98.Smith PE, Dunstan FD, Wiles CM. Selecting specialist registrars by station interview. Clin Med. 2006;6(3):279–280. doi: 10.7861/clinmedicine.6-3-279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Tulsky A, Aultman JM, Zirwas MJ. Personality testing in resident selection. Virtual Mentor. 2012;14(12):937–945. doi: 10.1001/virtualmentor.2012.14.12.ecas2-1212. [DOI] [PubMed] [Google Scholar]
- 100.Merlo LJ, Matveevskii AS. Personality testing may improve resident selection in anesthesiology programs. Med Teach. 2009;31(12):e551–e554. doi: 10.3109/01421590903390593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Bell RM, Fann SA, Morrison JE, Lisk JR. Determining personal talents and behavioral styles of applicants to surgical training: a new look at an old problem, part II. J Surg Educ. 2012;69(1):23–29. doi: 10.1016/j.jsurg.2011.05.017. [DOI] [PubMed] [Google Scholar]
- 102.Bell RM, Fann SA, Morrison JE, Lisk JR. Determining personal talents and behavioral styles of applicants to surgical training: a new look at an old problem, part I. J Surg Educ. 2011;68(6):534–541. doi: 10.1016/j.jsurg.2011.05.016. [DOI] [PubMed] [Google Scholar]
- 103.Quintero AJ, Segal LS, King TS, Black KP. The personal interview: assessing the potential for personality similarity to bias the selection of orthopaedic residents. Acad Med. 2009;84(10):1364–1372. doi: 10.1097/ACM.0b013e3181b6a9af. [DOI] [PubMed] [Google Scholar]
- 104.Lin DT, Kannappan A, Lau JN. The assessment of emotional intelligence among candidates interviewing for general surgery residency. J Surg Educ. 2013;70(4):514–521. doi: 10.1016/j.jsurg.2013.03.010. [DOI] [PubMed] [Google Scholar]
- 105.Talarico JF, Varon AJ, Banks SE, Berger JS, Pivalizza EG, Medina-Rivera G, et al. Emotional intelligence and the relationship to resident performance: a multi-institutional study. J Clin Anesth. 2013;25(3):181–187. doi: 10.1016/j.jclinane.2012.08.002. [DOI] [PubMed] [Google Scholar]
- 106.Bohm KC, Van Heest T, Gioe TJ, Agel J, Johnson TC, Van Heest A. Assessment of moral reasoning skills in the orthopaedic surgery resident applicant. J Bone Joint Surg Am. 2014;96(17):e151. doi: 10.2106/JBJS.M.00706. [DOI] [PubMed] [Google Scholar]
- 107.Lee AG, Golnik KC, Oetting TA, Beaver HA, Boldt HC, Olson R, et al. Re-engineering the resident applicant selection process in ophthalmology: a literature review and recommendations for improvement. Surv Ophthalmol. 2008;53(2):164–176. doi: 10.1016/j.survophthal.2007.12.007. [DOI] [PubMed] [Google Scholar]
- 108.Grober ED, Matsumoto ED, Jewett MA, Chin JL. Canadian Urology Program Directors. The Canadian Urology Fair: a model for minimizing the financial and academic costs of the residency selection process. Can J Surg. 2003;46(6):458–462. [PMC free article] [PubMed] [Google Scholar]
- 109.Pasadhika S, Altenbernd T, Ober RR, Harvey EM, Miller JM. Residency interview video conferencing. Ophthalmology. 2014;119(2):426–426.e5. doi: 10.1016/j.ophtha.2011.09.032. [DOI] [PubMed] [Google Scholar]
- 110.Shah SK, Arora S, Skipper B, Kalishman S, Timm TC, Smith AY. Randomized evaluation of a web based interview process for urology resident selection. J Urol. 2012;187(4):1380–1384. doi: 10.1016/j.juro.2011.11.108. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.