Abstract
The number of personnel providing in-home health care services is increasing substantially. The unique configuration of environmental hazards in individual client homes has a significant impact on the safety and health of home health care providers (HHPs). This mixed-methods study used data from a standardized questionnaire, focus groups, and individual interviews to explore environmental health and safety hazards encountered by HHPs in client homes. The participant sample (N = 68) included nurses, aides, therapists, and owners/managers from a variety of geographic locations. The most often-reported hazards were trip/slip/lift hazards, biohazards, and hazards from poor air quality, allergens, pests and rodents, and fire and burns. Frequency of identified key hazards varied by room, that is, kitchen (e.g., throw rugs, water on floor), bathroom (e.g., tight spaces for client handling), bedroom (e.g., bed too low), living room (e.g., animal waste), and hallway (e.g., clutter). Findings indicate the need for broader training to enable HHPs to identify and address hazards they encounter in client homes.
Keywords: occupational hazards, research, health surveillance, occupational health, occupational safety, workforce
The demand for home health care services is escalating in step with the aging population, resulting in an ever-growing number of paid caregivers providing in-home services for individuals with illnesses and disabilities. The number of home health aides and personal attendants is expected to increase by about 50% between 2008 and 2018, substantially more than the average increase for all other occupations (Bureau of Labor Statistics, 2014). The unique physical environment of each home offers significant challenges when providing health care to clients while protecting caregivers’ health and safety. Data from the Oregon Home Care Commission (2008-2010) indicated that home health care providers (HHPs) in publically funded programs incurred 352 lost time injuries per 10,000 full-time workers (Wipfli, Olson, Wright, Garrigues, & Lees, 2012). Multiple types of home hazards have been identified by diverse types of HHPs, including nurses, aides and technicians, administrators, social workers, physical therapists, and occupational therapists (Brillhart, Kruse, & Heard, 2004; Darragh, Campo, & King, 2012; Howard & Adams, 2010; Kendra, 2002; Sitzman & Leiss, 2009; Taylor & Donnelly, 2006). Homes can harbor a variety of hazards, including throw rugs, pests, tobacco smoke, mold, sharps, inadequate lighting, cluttered hallways and rooms, and inaccessible bathrooms (Markkanen et al., 2007; Sherman et al., 2008). Despite high rates of work-related injuries and the identification of a variety of hazards, scant research describes hazards by specific locations in the home.
Hazards also negatively affect job performance, job satisfaction, and health (Berg, Clausson, & Bokberg, 2012; Denton, Zeytinoğlu, & Davies, 2002; Sherman et al., 2008). In the only published study describing specific locations in the home of injuries incurred by HHPs, Czuba, Sommerich, and Lavender (2012) found that 60% of home health aide injuries occurred inside client homes, with the most common locations being the bedroom (24%), bathroom (18%), and kitchen (9%). Half of the injuries were associated with client handling, 8% with specific objects (e.g., needles, pets), 8% with cleaning, 4% with lifting objects, 2% with trash disposal, and 28% were unspecified. Client handling tasks that resulted in injury included moving clients in bed, bathing, and transferring clients.
In summary, despite the prevalence and significance of home health hazards for worker safety and health, limited research to date has identified specific hazards most often encountered in the frequently accessed areas of client homes where workers provide home health care services. The purposes of this study were to describe hazards encountered by HHPs from a variety of disciplines, identify the specific locations in client homes where hazards are located, and use the findings to design more effective approaches for training HHPs to assess and manage hazards.
Research Question 1: What environmental health and safety hazards are encountered by HHPs in client homes?
Research Question 2: How are the hazards distributed across specific rooms within client homes?
Method
This mixed-methods study included participant responses to a structured questionnaire and then to open-ended questions in focus groups and interviews. This study was part of a larger project using an interdisciplinary, participatory approach to develop and test the efficacy of an interactive virtual simulation training system to improve the safety of HHPs. Eight focus groups with two to five participants and 37 interviews with one to three participants were completed. Interviews were conducted in-person (43%) or via online meeting software (57%). The study and procedures were approved by The Ohio State University and University of Louisville Institutional Review Boards.
Participants
Participants were identified through informational flyers and emails distributed by home health care agencies and professional organizations. A $50 department store gift card was provided to each participant. Sixty-eight workers, 59 (95%) females and 3 (5%) males, participated in the study (Table 1). Participants worked primarily in home health care and were able to converse, read, and write in English. A majority of participants were registered nurses (31%), aides or homemakers (21%), administrators or educators (19%), or physical or occupational therapists (19%).
Table 1.
Participant Characteristics (N = 68)
| Characteristic | % |
|---|---|
| Sex (n = 62) | |
| Female | 59 (95.2) |
| Male | 3 (4.8) |
| Race (n = 50) | |
| White | 45 (71.4) |
| Other | 5 (7.9) |
| State (n = 68) | |
| Ohio | 22 (42.3) |
| Kentucky | 13 (25.0) |
| Minnesota | 4 (7.7) |
| Colorado | 3 (5.8) |
| Illinois | 3 (5.8) |
| Florida | 1 (1.9) |
| Indiana | 1 (1.9) |
| Iowa | 1 (1.9) |
| North Carolina | 1 (1.9) |
| South Carolina | 1 (1.9) |
| Washington | 1 (1.9) |
| Wyoming | 1 (1.9) |
| Age (n = 61; M = 49 years, SD = 11.8) | |
| 22-30 years | 6 (9.8) |
| 31-40 years | 10 (16.4) |
| 41-50 years | 15 (24.6) |
| 51-60 years | 19 (31.1) |
| 61-73 years | 11 (18.0) |
| Home health care position (n = 68) | |
| Registered Nurse | 21 (30.9) |
| Licensed practical nurse | 5 (7.4) |
| Physical therapist | 6 (8.8) |
| Occupational therapist | 7 (10.3) |
| Other specialists | 2 (2.9) |
| Aide/homemaker/assistant | 14 (20.6) |
| Administrator/educator | 13 (19.1) |
| Home health care experience (n = 61) | |
| <5 years | 13 (21.3) |
| 5-10 years | 23 (37.7) |
| 11+ years | 25 (41.0) |
| Type of agency (n = 43) | |
| For profit | 22 (51.2) |
| Not for profit | 21 (48.8) |
| Health history (n = 52) | |
| Asthma/allergies | 23 (37.7) |
| Arthritis/joint problems | 16 (30.8) |
| Overweight | 15 (23.8) |
| Back problems | 9 (24.3) |
| Hypertension | 7 (13.5) |
| Vision problems | 2 (3.8) |
| Depression | 2 (3.8) |
Procedures and Instruments
Prior to attending the focus group or interview, participants completed the Modified–Home Health Care Worker (M-HHCW) questionnaire. The 38-item M-HHCW includes demographic information, checklists of home health care tasks performed, injuries or adverse outcomes experienced in home health care situations, household hazards encountered in clients’ homes, and health history items. An open-ended question asked participants to indicate the most serious hazards they have encountered in homecare work. Parallel versions of M-HHCW questionnaires were constructed for various participant categories (registered nurses and home health aides, physical and occupational therapists, owners, managers, and home health care educators). The M-HHCW is written at a sixth-grade reading level and has been validated for face and content validity (Gershon, Canton, et al., 2008).
Each focus group and interview began with a discussion of hazards encountered by study participants in the homes of their clients. Although recognized as a significant hazard, participants were instructed to avoid discussing situations involving interpersonal violence as these hazards were generally outside the scope of the study and particularly outside the scope of the training system that was being developed as the main goal of the study. Focus group participants were then provided with separate floor plans of a bedroom, bathroom, kitchen, living room, and hallway (each participant was given a separate room) as well as cutouts of furniture/objects (e.g., bed, couch, sink) that generally belong in a given room. Participants were asked to reflect on their own homecare experience and to use the furniture and other objects to “furnish” a room as a room in a client’s home might be furnished. Participants then drew in the environmental health and safety concerns that immediately came to mind for that room. Once they completed identifying the hazards for the room, they passed their floor plan to the person next to them who reviewed the drawing and added additional hazards based on their experiences. This process continued until each participant provided input on each room drawing. Once the drawings were completed, the session moderator asked each participant to identify their top three priority hazards, using red adhesive stickers. Five additional adhesive dots were used to denote other, lower priority hazards. Following this hazard prioritization process, a discussion about the identified priorities in each room was facilitated by the moderator. Interview participants who interacted with a facilitator via a web-based meeting program or phone described the room-based hazards in several ways. Some dictated instructions to the facilitator, who furnished rooms, labeled hazards, and added “stickers” using a shared computer desktop. Others completed the drawings by themselves during the interview or verbally discussed hazards they had encountered in specific rooms in client homes. Interviews and focus groups lasted 45 minutes and two hours, respectively.
Data Analysis
All focus groups and interviews were digitally recorded, professionally transcribed, and independently verified. Focus group and interview transcripts were uploaded into Dedoose qualitative and mixed-methods analysis software (Dedoose Version 5.0.11, 2014) and content-analyzed. Transcripts were coded independently by two research team members (B.J.P., C.E.W.). Any discrepancies in coding were discussed and resolved to reach 100% agreement. Analysis of the transcripts was conceptualized in terms of density of response categories instead of frequency counts of content-coded categories. The analyzed responses could not be considered mutually exclusive responses as the focus groups and interviews were interactive discussions in which independent individual responses to questions were not gathered. The floor plan drawings were coded on a spreadsheet for hazards drawn by participants, and priority hazards were identified using adhesive dots. The M-HHCW questionnaire data were entered into an SPSS-PC database and analyzed descriptively. The open-ended M-HHCW item was content-analyzed.
Strategies to support validity and reliability focused on credibility and confirmability approaches. The researchers used multiple forms of triangulation, including triangulation of analysts, methods, and sources. As described above, two research team membeis coded the data separately and worked together to achieve 100% consensus. Data were collected from participants veibally and also by creating a visual depiction of in-home hazards. Data gathered from participants were corroborated through reviews of the literature. The research team used member checking to ensure hazards were correctly captured, and made adjustments when necessary. Seven participants representing all professional disciplines participated in member checking interviews. Participants reviewed the hazards and room analyses and provided feedback on and confirmation of the results.
Results
Hazards Encountered in Client Homes
Modified–Home Health Care Worker Questionnaire
Across client homes, participants reported encountering an average of 11 (SD = 5.4, median = 12, range = 0-19) environmental health and safety hazards from a list of 21 potential hazards (Table 2). The most common hazards cited were those pertaining to trip/slip/lift hazards (e.g., clutter, dangerous floors and stairs, throw rugs), biohazards (e.g., animal waste, infectious diseases), indoor air pollution (e.g., tobacco smoke, dust), alleigens (e.g., mold), and pests (mice and rats, insects). Other often-noted hazards were inadequate lighting, chemicals, and illicit drugs.
Table 2.
Hazards Encountered in Home Health Care as Reported in the Modified–Home Health Care Worker Questionnaire (n = 63)
| Exposure type | n (%) |
|---|---|
| Fall/trip/slip hazards | 56 (88.9) |
| Biohazards | 55 (87.3) |
| Air quality | 55 (87.3) |
| Allergens | 48 (76.2) |
| Pests/rodents | 47 (74.6) |
| Burning candles | 36 (62.1) |
| Poor lighting | 19 (32.8) |
| Chemicals | 18 (31.0) |
| Illicit drugs | 14 (24.1) |
Responses to the open-ended M-HHCW questionnaire item about the most serious hazards encountered in the home paralleled the checklist responses. Sixty of the 63 participants (95%) provided 127 written comments. Hazards related to trips/slips/lifts were the most common. Participants identified icy steps, stairs, lifting and transferring clients, clutter, and unsafe floois as specific, serious hazards. Exposure to biohazards, tobacco smoke, pests and rodents (bedbugs, mice), pets, inadequate ventilation and air quality, and the lack of proper equipment to assist clients were also noted as serious hazards encountered in clients' homes.
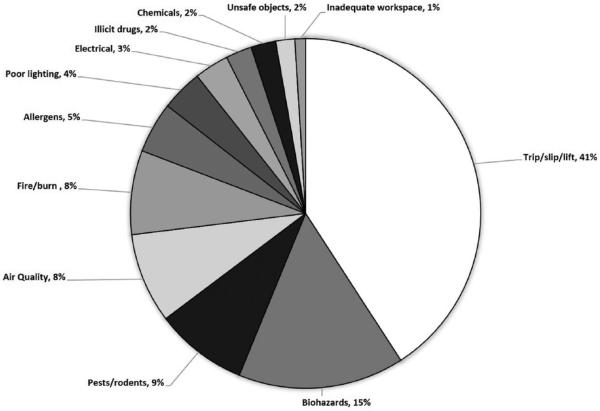
Focus groups and interviews
During the focus groups and interviews, participants talked about hazards they had encountered in clients' homes; from these discussions, 921 discrete comments were coded in the transcripts (see Table 3 for exemplars). Trip/slip/lift hazards were the most commonly reported hazards (41%; Figure 1). Participants indicated that lifting and moving clients, clutter and tight spaces, ice and snow, cords or tubing on the floor, and throw rugs were the primary reasons for potential musculoskeletal injuries from trips/slips/lifts. Biohazards, pests and rodents, air quality, and burn hazards were also often encountered by participants (15%, 9%, and 8%, respectively). The primary biohazards described included pet droppings and human waste. Bedbugs, mice and rats, and roaches were identified as the pests most frequently encountered in homes. Tobacco smoke and inadequate ventilation were the major causes of poor air quality. Smoking with an oxygen source turned on and using the stove for heating were the most common fire and burn hazards noted by participants. Additional identified hazards included allergens (e.g., mold), inadequate lighting, electrical hazards (e.g., faulty outlets), illicit drugs (e.g., marijuana), chemicals (e.g., pesticides; cleaning products), unsafe objects (e.g., furniture with sharp corneis), and homes in disrepair (e.g., falling ceilings). Inadequate workspace, specifically, the lack of adequate, clean space to place bags or other materials needed for HHPs to do their work was also mentioned as hazardous due to the need to assume awkward body postures or use inappropriate body mechanics during care activities.
Table 3.
Exemplar Quotes Illustrating Hazards Encountered by Home Health Care Providers
| Hazard type | Exemplar quotes |
|---|---|
| Trip/slip/lift hazards | |
| Trip–clutter | A lot of times you have people who are addicted to the shopping network, and they have boxes everywhere they’re opening, closing. I’ve had a couple patients like that. This one patient had newspapers all over the floor, and every time I’d come she’d ask me to pick them, but they were all over the floor, and you’d slide everywhere. Clothing, sometimes they can’t hang up the clothing so it’s all over the floor. Just about almost anything you could think of. |
| Slip/trip | Throw rugs. I think that’s with the older generation more. They seem to have to have rugs in front of everything∔in front of the stove, in front of the sink, in front of the refrigerator, in front of the doors all the time. And I help remind that these are dangerous; you could easily fall on them. “Yeah, I know. I should get rid of them.” But then you go back the next time and they still haven’t. |
| Lift | She didn’t want to have to be lifted with a Hoyer lift. And so people had to be able to lift∔because she was a quad, and she had a “trach” and it was ongoing, and so you had to be able to get her out of this electric wheelchair and get her in her bed. It was very challenging; it was hard. |
| Slip | I think the number one thing that’s happened to our staff is a lot of back injuries and falls on the ice, because most of your patients’ homes you go into, they’re homebound, so they can’t shovel the snow or anything. So by nature of that, you’re walking up to a house that’s already dangerous just in your own∔and you’re carrying a giant bag with you. |
| Biohazards | |
| Pet droppings | A lot of pet feces, urine, newspapers around, puppy pads around. They don’t clean them up, don’t think they need to. |
| Human waste | We have some patients who are incontinent so bad that the entire house smells of urine and yeah, bad, to the point of the ammonia smell hurting the staff. |
| Sharps | The table with all the papers and clutter, this is how we’ve gotten a lot of needle sticks. They will sit at the table to administer their medications and their shots and stuff. And the client did not dispose of the needle; it was laying there, and when the aide gathered up the papers, she sustained a needle stick. We have that one happen a lot. |
| Pests/rodents | |
| Pests | And then with all that clutter comes bugs∔lots and lots of bugs. That’s a big safety concern for everyone∔them and us, because we can bring them home with us. They’re living with them and they’re touching everything. |
| Pests/rodents | I’ve been in one particular home where I had to deal with mice nests, rat nests, droppings. I’ve been in various homes that I’ve had to deal with bedbugs and roaches. |
| Air quality | |
| Tobacco smoke | And there are people that smoke, and they don’t put down their cigarettes for you. And they’ll just keep smoking, and the house is full of∔you walk into kind of a stagnant∔and it’s not good for anyone, but they do it anyway. |
| Lack of ventilation |
There are many homes where there are very strong smells and there’s no ventilation at all. |
| Fire/burn hazards | |
| Smoking with oxygen in use |
I’m going to refer to is another client actually who was on oxygen and was a heavy, heavy smoker. So he was chronically smoking with big oxygen canister inside of his house. Actually, it was a tiny apartment, so it placed the entire apartment complex at risk. |
| Using stove for heat |
I was exposed to two patients recently that kept their burners on their stove for heat. And so I think that could be a hazard, especially if you accidentally lean on a stove without you knowing that it’s on. Because it was hard to see because they were gas burners. It was low, but it’s hard to see that. So that’s what they were doing to keep their heat going in their house. |
| Allergens | |
| Pet hair | And then we’ll have pets in the home and maybe a lot of pet hair or pet odor. |
| Mold/mildew | Mold was a biggie. A lot of houses that were in decayed condition, some of them where the floors were caving in, and people refused to move. The foundations were clearly rotted. And going back and into those homes when you would walk in the door, the mold’s smell would be overwhelming and hit you in the face. |
| Poor lighting | |
| Dim lighting | The lighting would be one I see a lot in the bedrooms. Poor lighting. People want to have their shades drawn and just the lamp on the bedside on. |
| Electrical hazards | |
| Inadequate outlets |
Electrical hazards, especially if we were bringing machinery equipment, say a pump to run tube feedings or something like that, some of the houses weren’t wired with the current outlets, current type of electricity you needed. And then they didn’t have the three-prong; they had two-prong. Sometimes people were using multiple extension cords to try and plug things in. |
| Faulty outlets | Faulty outlets. Just doing the care around the home. Every time you have to plug in the vacuum cleaner. But I see the outlet is hanging out. It’s dangerous. |
| Illicit drugs | |
| Marijuana smoke |
I’ve walked into homes just filled with marijuana smoke, just rolling out of the windows |
| Chemicals | |
| Pesticides | I have patients if they have ants or roaches, then they have sprays or powders and sometimes they’re sitting on the kitchen table. |
| Cleaning products |
And the chemicals on top, they’re like things that aren’t closed like bleach or a lot of these places have plugged up pipes so there’s like drain openers and cleaners they put down the toilet to try and keep them flowing. And they just leave them open because nine times out of ten there aren’t kids in the house. You stick a bedside commode on the top of the toilet because it’s not working and then you got this whole thing rocking and things start spilling and mixing together and∔I mean, fumes that will make you really sick. |
| Unsafe objects | |
| Penetrating objects |
Nails sticking out of the wall where they had pictures, but there’s not pictures anymore. |
| Unsafe furniture | One of the homes we went into, we actually saw that one of the legs was broken off, and they had taken a couple of concrete blocks to hold that side of the bed up. And they didn’t want to get rid of the bed because it was so sentimental; it meant so much to the family. And they didn’t replace the one leg that was broke. It was a four-poster bed and so the one poster leg was broken, so they had just taken concrete block and put it up underneath on that side. |
| Inadequate workspace | |
| Lack of clean surfaces |
I’ve had people who don’t part with anything just piled on all of these surfaces so that it makes it more difficult for you to find a clean surface to put your things on. Or if you’re doing a dressing change, where do you put your supplies and open them up on a safe place? And if the bed is dirty, they haven’t changed the sheets for a period of time, if they’ve been incontinent. |
Figure 1.
Environmental health and safety hazards encountered by home health care providers in client homes.
Hazards Encountered in Client Homes by Room
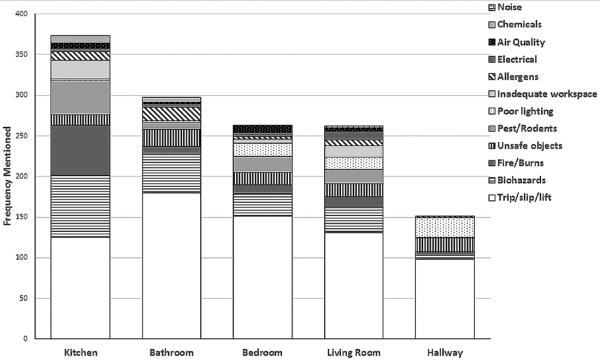
Kitchen
More kitchen hazards were mentioned by participants than hazards in any other room with trip/slip/lift hazards being the most frequently mentioned type of hazard (Figure 2). Throw rugs, water or grease on the floor, clutter, tight spaces, pets underfoot, faulty kitchen furniture, and damaged flooring comprised the most common types of kitchen trip/slip/lift hazards. Biohazards such as spoiled food on counters or in refrigerators were also frequently noted. Other kitchen biohazards included litter boxes and pet droppings, overflowing trash bags or containers, sharps in the trash or on counters, and dirt on counters, appliances, and tables. Fire and burn hazards related to using the oven as a heat source or combustible items or grease on or near a stovetop with a lit burner were often cited. Unsafe objects such as faulty appliances, sharp corners on kitchen counters, and broken legs on kitchen chairs were described and illustrated in floor plans. Kitchen hazards also included pests and rodents such as roaches and mice, alleigens (e.g., mold from a leaky ceiling or window), unlabeled and opened chemical cleaners, faulty electrical outlets, poor air quality from tobacco smoke or other odors, and inadequate clean, uncluttered space on which to place work items.
Figure 2.
Distribution of environmental health and safety hazards encountered by home health care providers across specific rooms in client homes.
Bathroom
Trip/slip/lift hazards were the most common type of bathroom hazard discussed by participants. Tight spaces due to small or overcrowded bathrooms were the primary trip/slip/lift concern followed closely by throw rugs, and lack of safety equipment such as grab bars, shower chairs, and non-slip bathtub mats. Inappropriately used items such as kitchen chairs placed in the tub as a shower chair and towel racks used as grab bais were illustrated in participants' floor plans. Trip/slip/lift hazards were often encountered while providing assistance to clients with toileting or bathing activities. These types of client handling activities are known to be physically hazardous (Czuba et al., 2012; Galinsky, Waters, & Malit, 2001) and are made more so under the adverse conditions described by participants (e.g., tight spaces, lack of appropriate assistive equipment, presence of slip/trip hazards). The slip hazards also included water on the floor, and trip hazards included floois in disrepair, especially in mobile homes. Bathroom biohazards primarily included human waste in and around the toilet and tub, dirt, lack of running water or soap in the bathroom or whole home, and pet droppings. Other bathroom hazards noted by participants included unsafe objects such as unsecured shelving and sharp vanity corneis, allergens from mold and mildew, space heaters in use (risk of tripping, fire, burns, electrical shock, and electrorution), water temperature settings that were too hot, pests and rodents, and unlabeled or leaking cleaning chemicals.
Bedroom
Trip/slip/lift hazards in the bedroom were primarily due to tight spaces and clutter (e.g., many pieces of furniture, medical equipment, clothing, magazines, or paper on the floor), moving clients in and out of bed, handling clients in the provision of care, and bed heights that were either too high or too low. Client care, including handling, was made more hazardous in the bedroom by furniture and other types of clutter that restricted or constrained workers' access to the client, forcing the HHP to work in awkward, stressful postures. Trip hazards posed by throw rugs, electrical cords, and oxygen tubing lying across the floor were also described and frequently appeared in the bedroom floor plans. Human waste in the bed or on the floor near a bedside commode was the most frequently identified biohazard in the bedroom. Bedroom biohazards also included pet droppings and aggressive pets (e.g., animal bite risk), spoiled food, dirt, soiled adult diapers, and unsheathed sharps. Inadequate lighting to perform tasks, bedbugs, unsafe objects such as a laige or heavy television on unstable furniture, fire hazards such as a client smoking in bed or smoking with oxygen in use, and missing smoke alarms were also cited as bedroom hazards.
Living room
Clutter from items such as magazines, papers, toys, and books, and tight spaces from large furniture, medical equipment, and a hospital bed in the living room were cited as slip/trip hazards as were rugs and electrical cords and oxygen tubing stretched across the floor. Participants often reported diffirulty in lifting clients from low furniture and moving clients due to clutter. Living room drawings often depicted throw rugs in the room along with mobility aides (i.e., walkers, wheelchairs); interactions between these posed additional hazards. Biohazards were also a major category of living room hazards, primarily from pet droppings, including living room rugs soiled with pet urine and feces. Annotations concerning human waste in a bedside commode appeared on the living room floor plans. Pests and rodents such as bedbugs in living room furniture were mentioned. Inadequate lighting was identified as a hazard in the living room, commonly from the lack of an overhead light or lack of light bulbs in lamps. Unsafe objects such as the ceiling falling down, sharp furniture, or sharp items, including syringes in rugs and furniture, were also identified as living room hazards. Inadequate workspace in the living room was mainly related to clutter and tight spaces. Fire, burns, and electrical hazards in the living room came from flammable clutter near a working space heater, careless smoking (as evidenced by burns in furniture and carpet), cigarette smoking while oxygen was in use, faulty or overloaded electrical outlets, and improper use of extension cords (i.e., extension cords used in series, aka daisy-chaining). The lack of an "oxygen in use" sign in a home was noted on several drawings as a hazard. Noise exposure due to loud televisions was mentioned as a hazard by several participants.
Hallway
Although the fewest hazards were identified in the hallway, trip/slip/lift hazards were the most common type of hallway hazard. Hallways cluttered with stored furniture, supplies, shoes and piles of clothes, mobility aids (i.e., walkers, wheelchairs), and litter boxes were hazardous to negotiate. Other trip hazards in hallways were throw or area rugs, damaged carpet, oxygen tubing running through or across a hallway, and pets underfoot. Frequently cited poor lighting compounded these hazardous conditions. Doorways off hallways were noted as being too narrow for the client's wheelchair, which contributed to potential overexertion exposure of workers who had to assist their clients through doorways without their wheelchairs. Unsafe objects such as falling ceilings and large picture frames with sharp edges hanging in hallways were also commonly mentioned.
Discussion
This study explored environmental health and safety hazards encountered by HHPs in clients’ homes and in specific rooms within those homes. Study strengths included the use of triangulated quantitative and qualitative methods, representation of diverse types of HHPs, and a room-by-room analysis of specific hazards. Integrating data from multiple data sources and professions lends confidence to the overall conclusion that HHPs are exposed to a variety of environmental health and safety hazards that can lead to costly injuries and illnesses. To the authors’ knowledge, this is the only study to date that has included a room-by-room analysis of these types of environmental health and safety hazards.
Consistent with other studies (Czuba et al., 2012; Darragh et al., 2012; Wipfli et al., 2012), trip/slip/lift hazards were the most commonly identified hazards, and the specific sources for these types of hazards varied, a key finding with implications for enhanced HHP training. Sprains and strains, commonly attributable to lifts, slips, and trips, have previously been documented to be the most frequent lost work-time injuries to HHPs, resulting in almost 1 month of lost work time (Centers for Disease Control and Prevention, 2010; Wipfli et al., 2012). Recommendations to reduce exposure to trip/slip/lift hazards include making changes in the work environment, (e.g., removing throw rugs, securing cords, providing adequate lighting), using assistive devices such as transfer or gait belts, participating in ergonomics training, and wearing sturdy shoes with slip-resistant soles (Centers for Disease Control and Prevention, 2010; Marrelli, 2008; Satink, 2007). These and other recommendations can be incorporated into specific training for HHPs on how to assess and manage trip/slip/lift hazards, especially for home health aides who have the most exposure.
Exposures to potential biohazards, such as human or pet waste and blood-borne pathogens, were commonly expressed concerns in this study as well as by other researchers (Gershon, Canton, et al., 2008; Gershon, Pogorzelska, Qureshi, & Sherman, 2008; Leiss, Sitzman, & Kendra, 2011; Markkanen et al., 2007; Wipfli et al., 2012). Occupational Safety and Health Administration (OSHA; 2011) regulations require agencies to have an exposure control plan and annual blood-borne pathogen training, but neither a control plan nor training is required for other biohazards. Most participants in this study (73%) indicated they received training on standard precautions and were supplied with gloves, but not other forms of personal protective equipment (PPE) such as face shields, goggles, or protective clothing. These findings highlight the need for agency- and policy-level changes to assure that HHPs have the protective equipment necessary for personal safety.
Air quality and allergen exposures from tobacco smoke, mold, and inadequate ventilation were considered highly hazardous by participants with asthma and allergies. Several participants commented that their agency had a tobacco smoking policy in which clients agreed not to smoke (nor allow others to smoke in their home) while the HHP was there. Although helpful, not all agencies have this type of policy and not all HHPs insist their agencies’ policies be followed. Although the consequences of exposure to secondhand tobacco smoke are well known (Centers for Disease Control and Prevention, 2014), the National Institute for Occupational Safety and Health (NIOSH) does not include this hazard in its 2010 Occupational Hazards in Home Care publication (Centers for Disease Control and Prevention, 2010). The findings of this study highlight the need for policy- and individual-level interventions to reduce risk of exposure to secondhand tobacco smoke. The U.S. Surgeon General has stated that no risk-free level of exposure to tobacco smoke exists (U.S. Department of Health and Human Services, 2006), so it is imperative that NIOSH and OSHA develop a standardized smoke-free policy template that can be adapted and implemented by home health agencies to protect their workers.
Participants in this study identified the most hazards in the kitchen, followed by the bedroom and the bathroom. These locations were also the primary locations where Czuba et al. (2012) reported that injuries occurred to home health aides. Although trip/slip/lift hazards were the most common hazard type reported in each room in the present study, with the exception of throw rugs, which pose a hazard in every room, the specific types of risks differed. Water and grease spills were described frequently on kitchen floors; tight spaces and missing equipment in bathrooms; clutter, tight spaces, and lifting hazards in the bedroom; electrical cords and oxygen tubing in the living room; and clutter in the hallway. Similar differences in the types of biohazards encountered in each room were identified. Pet droppings were key biohazards in the kitchen and living room; human waste was commonly noted as bathroom and bedroom hazards. The rooms in clients’ homes in which HHPs work varied by type of HHP and clients’ needs. For example, nurses may not go into a client’s bedroom or kitchen if client care is provided in the living room. By contrast, home health aides are often in all rooms if they provide cleaning, meal preparation, and personal care services. A key implication of these findings is that health care agencies should provide tailored training that addresses the different hazards HHPs are likely to encounter by room, also taking into account HHP job descriptions and client needs.
Limitations
Focus group and interview discussions sometimes also addressed items in the home that posed hazards to clients. In fact, HHPs tended to focus on hazards to clients unless specifically reoriented to HHP hazards. Discussions specifically focused on client hazards were not coded as HHP hazards, but it was not always clear who was the focus of individual comments. This finding may explain why spoiled food, which seems to be more of a hazard for the client than the worker, was included. The study also avoided focusing on interpersonal violence as a hazard. The authors acknowledge the importance of violence-related hazards, but determined that violence was outside the scope of this study.
Implications for Occupational Health Nursing Practice
Although home health care is not a traditional practice site for occupational health nurses, the recent significant growth in home health care, high incidence of injuries and illnesses among HHPs, and the breadth of hazards encountered by HHPs supports a need for home health care agencies to use or contract with occupational health nurses to improve occupational safety practices, thus preventing the adverse health events that can affect HHPs. This study provides critical information that occupational health nurses could use to effectively train home health care personnel to conduct thorough home hazard assessments to identify hazards that HHPs might encounter in their work. In addition, occupational health nurses can provide expert guidance to agencies and policy makers to develop and implement policies that assure a safe working environment for HHPs. Examples include a standardized smoke-free policy template previously discussed, as well as policies clearly outlining protocols with sequentially ordered management steps for HHPs to follow when potential hazards are encountered in client homes. These steps may range from securing assistance moving an obese homebound client, to informing a family member when a faulty electrical outlet is identified, to contacting the agency when evidence of pests such as cockroaches or mice are noted. Through training, education, and active involvement in policy development and implementation, occupational health nurses could make a significant safety and health impact on the working conditions of HHPs.
Conclusion
This study is unique in its focus on a room-by-room analysis of specific environmental hazards in clients’ homes. Trip/slip/lift hazards were the most common hazards throughout the home, but, with the exception of throw rugs, varied from room to room. Biohazards were most common in the kitchen and bathroom, and electrical and fire hazards were most common in the kitchen. Training for individual HHPs should include specific approaches to managing hazards that the HHPs can address at the point of care, as well as how to effectively engage assistance from their agencies. These findings can contribute to the development of evidence-based, efficacious, and engaging training programs using interactive virtual simulation approaches. This research also revealed opportunities for agency-level training to facilitate coordination and communication between HHPs and agency management.
Supplementary Material
Applying Research to Practice.
The number of home health care providers is increasing, and these workers are exposed to a variety of hazards in client homes. This study explored the environmental health and safety hazards encountered by home health care providers and how these hazards were distributed across specific rooms in client homes. Participants frequently described trip/slip/lift hazards, biohazards, and hazards from poor air quality, allergens, pests/rodents, and fire/burns. Hazard risk varied by room. Examples of kitchen hazards included throw rugs and water on the floor, a too low or too high bed was a hazard in the bedroom, human waste and tight spaces were frequent bathroom hazards, living rooms and hallways were often cluttered. There is a need for broader training to enable home health care providers to identify and address these hazards.
Acknowledgments
The authors would like to thank the research associates who provided invaluable assistance throughout this project: Carly Dufresne, Christine Gabrell, Chase Harber, and Jenna Vanderwall. We would also like to thank the home health care providers who spoke candidly with us during the focus groups and interviews.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by the National Institute for Occupational Safety and Health (NIOSH) of the Centers for Disease Control and Prevention under Award R01OH010425-02.
Biographies
Barbara J. Polivka, PhD, RN, is professor and Shirley B. Powers Endowed Chair for Nursing Research at the University of Louisville School of Nursing. Her research has focused on environmental health and health services research, with a specific focus in environmental exposures in homes for healthcare workers and residents.
Celia E. Wills, PhD, RN, is an associate professor at The Ohio State University College of Nursing. Her research program focuses on patient and health care provider judgment and decision-making on topics such as shared patient-provider treatment decision-making, nurses’ judgments of patient care safety errors, and health care provider decision-making about managing home health and safety hazards.
Amy Darragh, PhD, OTR/L, FAOTA, is an associate professor at The Ohio State University in the School of Health and Rehabilitation Sciences. She has a long history of research in occupational safety and health, with particular expertise in work-related musculoskeletal disorder prevention and safe patient handling and mobility.
Steven Lavender, PhD, CPE, is an associate professor at The Ohio State University in the Department of Integrated Systems Engineering and the Department of Orthopaedics. His research primarily focuses on ergonomic intervention development, ergonomic assessment methods, and occupational biomechanics.
Carolyn Sommerich, PhD, is an associate professor at The Ohio State University in the Department of Integrated Systems Engineering and the School of Health and Rehabilitation Sciences. Her research focus is ergonomics and occupational biomechanics, with special interests in the upper extremity, ergonomics in office and health care settings, and ergonomics issues affecting youth.
Donald Stredney, MA, is the Director of the Interface Lab at the Ohio Supercomputer Center. He has been involved in computational methods to represent biomedical structures and phenomenon for over 30 years. He collaborates closely with domain specialists including skull-base visualization, a functional endoscopy sinus surgery simulator, the temporal bone simulation, disaster preparedness, and home health hazards.
Footnotes
Conflict of Interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Berg A, Clausson EK, Bokberg C. Secondhand smoking in Swedish municipal home nursing: A qualitative pilot study. Public Health Nursing. 2012;29:525–533. doi: 10.1111/j.1525-1446.2011.01004.x. doi:10.1111/j.1525-1446.2011.01004.x. [DOI] [PubMed] [Google Scholar]
- Brillhart B, Kruse B, Heard L. Safety concerns for rehabilitation nurses in home care. Rehabilitation Nursing. 2004;29:227–229. [PubMed] [Google Scholar]
- Bureau of Labor Statistics Occupational outlook handbook. Home Health Aides. 2014 U.S. Department of Labor. Retrieved from http://www.bls.gov/ooh/healthcare/home-health-aides.htm.
- Centers for Disease Control and Prevention . NIOSH Hazard Review: Occupational Hazards in Home Healthcare. Author; Cincinnati, OH: 2010. [Google Scholar]
- Centers for Disease Control and Prevention . Prevalence of smokefree home rules—United States, 1992-1993 and 2010-2011. Author; Atlanta, GA: 2014. [Google Scholar]
- Czuba LR, Sommerich CM, Lavender SA. Ergonomic and safety risk factors in home health care: Exploration and assessment of alternative interventions. Work. 2012;42(3):1–12. doi: 10.3233/WOR-2012-1433. [DOI] [PubMed] [Google Scholar]
- Darragh AR, Campo M, King P. Work-related activities associated with injury in occupational and physical therapists. Work. 2012;42:373–384. doi: 10.3233/WOR-2012-1430. doi:10.3233/WOR-2012-1430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- W.P. f. M , analyzing, and presenting qualitative and mixed method research data. SocioCultural Research Consultants; Los Angeles, CA: 2014. Dedoose Version 5.0.11. Available from Retrieved from http://www.dedoose.com/ [Google Scholar]
- Denton MA, Zeytinoğlu IU, Davies S. Working in clients’ homes: The impact on the mental health and well-being of visiting home care workers. Home Health Care Services Quarterly. 2002;21(1):1–27. doi: 10.1300/J027v21n01_01. [DOI] [PubMed] [Google Scholar]
- Galinsky T, Waters T, Malit B. Overexertion injuries in home health care workers and the need for ergonomics. Home Health Care Services Quarterly. 2001;20(3):57–73. doi: 10.1300/J027v20n03_04. [DOI] [PubMed] [Google Scholar]
- Gershon RRM, Canton AN, Raveis VH, Silver A, Chen CC, Qureshi KA, Stone PW. Household-related hazardous conditions with implications for patient safety in the home health care sector. Journal of Patient Safety. 2008;4:227–234. doi:10.1097/PTS.0b013e31818936e3. [Google Scholar]
- Gershon RRM, Pogorzelska M, Qureshi KA, Sherman M. Home health care registered nurses and the risk of percutaneous injuries: A pilot study. American Journal of Infection Control. 2008;36:165–172. doi: 10.1016/j.ajic.2007.04.278. doi:10.1016/j.ajic.2007.04.278. [DOI] [PubMed] [Google Scholar]
- Howard N, Adams D. An analysis of injuries among home health care workers using the Washington State Workers’ Compensation Claims Database. Home Health Care Services Quarterly. 2010;29:55–74. doi: 10.1080/01621424.2010.493435. doi:10.1080/01621424.2010.493435. [DOI] [PubMed] [Google Scholar]
- Kendra MA. Perception of risk by administrators and home health aides. Public Health Nursing. 2002;19:86–93. doi: 10.1046/j.1525-1446.2002.19203.x. [DOI] [PubMed] [Google Scholar]
- Leiss JK, Sitzman KL, Kendra MA. Provision and use of personal protective equipment among home care and hospice nurses in North Carolina. American Journal of Infection Control. 2011;39:123–128. doi: 10.1016/j.ajic.2010.05.021. doi:10.1016/j.ajic.2010.05.021. [DOI] [PubMed] [Google Scholar]
- Markkanen P, Quinn M, Galligan C, Chalupka S, Davis L, Laramie A. There’s no place like home: A qualitative study of the working conditions of home health care providers. Journal of Occupational and Environmental Medicine. 2007;49:327–337. doi: 10.1097/JOM.0b013e3180326552. [DOI] [PubMed] [Google Scholar]
- Marrelli T. Home health aide guidelines for care: A handbook for care giving at home. 2nd Marrelli and Associates; Boca Grande, FL: 2008. [Google Scholar]
- Occupational Safety and Health Administration OSHA fact sheet: OSHA’s bloodborne pathogens standard. 2011 Retrieved from https://www.osha.gov/OshDoc/data_BloodborneFacts/bbfact01.pdf.
- Satink F. Integrating occupational safety into home health operations. Caring. 2007;26(2):40–44. [PubMed] [Google Scholar]
- Sherman MF, Gershon RRM, Samar SM, Pearson JM, Canton AN, Damsky MR. Safety factors predictive of job satisfaction and job retention among home healthcare aides. Journal of Occupational and Environmental Medicine. 2008;50:1430–1441. doi: 10.1097/JOM.0b013e31818a388e. doi: 10.1097/JOM.0b013e31818a388e. [DOI] [PubMed] [Google Scholar]
- Sitzman KL, Leiss JK. Documentation of incidental factors affecting the home healthcare work environment. Home Healthcare Nurse. 2009;27:516–521. doi: 10.1097/01.NHH.0000361921.20388.5b. doi:10.1097/01.NHH.0000361921.20388.5b. [DOI] [PubMed] [Google Scholar]
- Taylor BJ, Donnelly M. Risks to home care workers: Professional perspectives. Health, Risk & Society. 2006;8:239–256. [Google Scholar]
- U.S. Department of Health and Human Services . The health consequences of involuntary exposure to tobacco smoke: A report of the Surgeon General. Author; Atlanta, GA: 2006. [PubMed] [Google Scholar]
- Wipfli B, Olson R, Wright RR, Garrigues L, Lees J. Characterizing hazards and injuries among home care workers. Home Healthcare Nurse. 2012;30:387–393. doi: 10.1097/NHH.0b013e31825b10ee. doi:10.1097/NHH.0b013e31825b10ee. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.