Abstract
Background
Breast cancer patients commonly use the internet as an information resource. Our objective was to evaluate the quality of online information available to support patients facing a decision for breast surgery.
Methods
Breast cancer surgery-related queries were performed (Google and Bing), and reviewed for content pertinent to breast cancer surgery. The DISCERN instrument was used to evaluate websites’ structural components that influence publication reliability and ability of information to support treatment decision-making. Scores of 4/5 were considered “good”.
Results
45 unique websites were identified. Websites satisfied a median 5/9 content questions. Commonly omitted topics included: having a choice between breast conservation and mastectomy (67%) and potential for 2nd surgery to obtain negative margins after breast conservation (60%).
Websites had a median DISCERN score of 2.9 (range 2.0–4.5). Websites achieved higher scores on structural criteria (median 3.6 [2.1–4.7]), with 24% rated as “good”. Scores on supporting decision-making questions were lower (2.6 [1.3–4.4]), with only 7% scoring “good”.
Conclusion
Although numerous breast cancer-related websites exist, most do a poor job providing women with essential information necessary to actively participate in decision-making for breast cancer surgery. Providing easily-accessible, high-quality online information has the potential to significantly improve patients’ experiences with decision-making.
Keywords: Breast Cancer, Decision-Making, Internet, Information
INTRODUCTION
Each of the more than 250,000 women diagnosed annually with local-regional breast cancer will face the challenging decision between mastectomy and breast conservation.[1] Given that multiple randomized control trials have demonstrated equivalent survival between the two procedures, [2] patient preference is often a primary driver of surgical decision-making. Active participation in treatment decision-making has been shown to result in improved patient satisfaction with the decision-making process and greater perceived post-treatment quality of life.[3–6] However, in order to participate fully in the decision, patients need to be knowledgeable about the risks and benefits of each procedure including risk of local recurrence, recovery times associated with each procedure, cosmetic outcomes, and long-term quality of life. Further, most patients will need guidance on how to consider mastectomy versus breast conservation in the context of their personal values and long-term goals.
Not surprisingly, the internet is a very common resource that patients use to learn about their diagnosis and treatment options. 87% of the US population has internet access, and 72% of those users have searched for health information within the last year.[7] Given the ubiquitous presence of computers with high speed internet and mobile browsing devices, online materials represent a powerful avenue to educate patients of all ages about health care choices. However, in spite of this incredible potential, the Internet remains a daunting and often ineffective source of information due to a lack of intuitively designed consumer-level health care information, the inability to verify information reliability, and an often overabundance of information sources that makes finding high quality information challenging and time-consuming.[8–10] This is especially true for patients with lower health literacy (often those with lower socioeconomic status and/or less education) who arguably may benefit most from accessible, high-quality online information.[11] With this in mind, we sought to determine the quality of online information available to support patients with breast cancer who are facing a decision for type of breast surgery.
METHODS
We searched both Google™ (Mountain View, CA)[12] and Bing™ (Bellevue, WA)[13] with the following four phrases: Breast Cancer Surgery, Breast Cancer Treatment, Mastectomy, and Lumpectomy. These search terms were chosen based on the input from a convenience sample of women without a personal history of breast cancer. The search terms were kept purposely short, simple, and broad in order to reflect the practices of internet users of all abilities searching for information about breast cancer surgery. All searches were performed from the same location on 6/23/2014. The two search engines were chosen because at the time of our study, they were the most popular engines and together possessed 86% of the search engine market share in the US (Google 67.6%; Bing 18.7%).[14]
We reviewed sites that appeared within the first two pages of search results, as marketing data demonstrates that only 1.6% of users click on links from the third page of results or beyond.[15] Sites were excluded if they were not in English, if they were unrelated to breast cancer or its treatments, and if payment or registration was required for access. Any website that was an advertisement for products or specific surgeons/physicians/treatment centers were also excluded from the study even if they contained content that was otherwise related to breast cancer surgery. Websites that met the inclusionary criteria were then independently reviewed by two researchers (J.G.B. and J.L.T). Evaluations were performed using: 1) a list of content pertinent to breast cancer surgery that was derived from validated questionnaires as well as the literature[16] and 2) the DISCERN instrument (www.discern.org.uk). The DISCERN instrument is a validated questionnaire designed to assess the quality of patient targeted health information for treatment choices and is applicable for both printed and online resources.[17] It was designed to provide end-users (i.e. patients) with a reliable way of assessing the quality of an information source without requiring that they be experts in the subject matter. Further, it can be used by authors and publishers of information to improve the quality of their publications. It consists of a series of 16 questions, each of which are scored on a scale of 1–5; we considered 4–5 to be “good”, 3 “fair”, and 1–2 “poor”. The first 15 questions examine aspects of the source of the information or the information itself, while the 16th question is a subjective assessment by the reviewer of the overall quality of the website. Questions included in the DISCERN instrument fall into two main categories (Table 1): those that examined the structural characteristics of the site which impact quality or trustworthiness of the information source (seven questions), and those that examined how well the site supports shared decision-making (nine questions). Scores from questions within each of these groups were summarized, and then normalized out of 5 possible points. Inter-reviewer agreement was assessed by a calculated Kappa statistic (kappa 0.8) and descriptive statistics were performed.
This research was exempt from Institutional Review Board review.
RESULTS
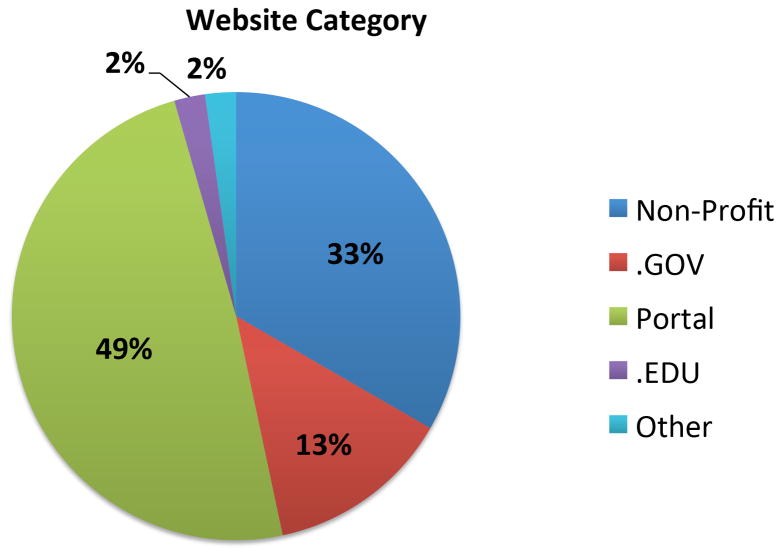
Our searches resulted in 182 total results. After excluding duplicate sites identified by each of the two search engines used, our final list included 45 unique websites which met the inclusion criteria. 49% of the websites reviewed were large information portals, a portion of which were health care specific (e.g. Wikipedia.org, about.com) (Figure 1). The remaining were maintained by non-profit foundations (e.g. Susan G. Komen, BreastCancer.org, 33%), sites of government or public health organizations (e.g. CDC, NIH, 13%), and university affiliated (2%). There were a small number of sites that consisted of articles or health guides that did not readily fall into any single category (e.g. New York Times Health Guide).
Figure 1.
Categorization of websites identified by search strategy
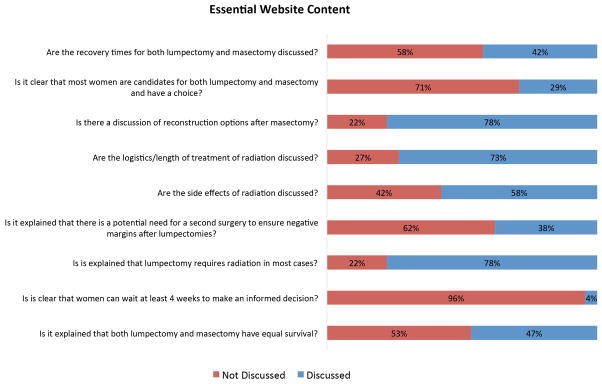
Websites addressed a median 5/9 (range 0–9) of the identified content questions, with only one website covering all topics felt to be pertinent to the decision for type of breast cancer surgery (Figure 2). Most websites did not discuss that most women can safely wait at least 4 weeks to make an informed treatment decision (96%), did not explicitly describe that most women are candidates for both mastectomy and breast conservation (71%), did not discuss the potential need for a 2nd procedure to ensure negative margins following breast conservation (62%), did not include post-surgery recovery times (58%), and did not state that mastectomy and breast conversation have equivalent survival (53%).
Figure 2.
Assessment of website content pertinent to breast cancer surgery decision-making
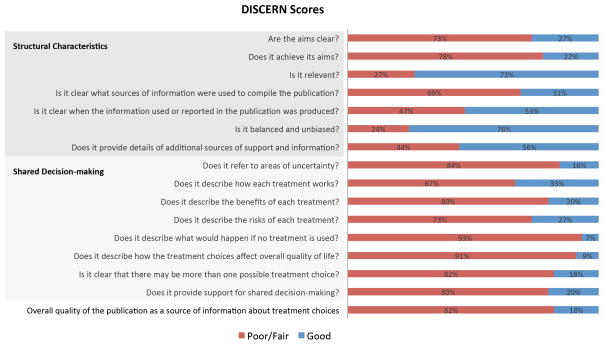
Scores from the evaluation using the DISCERN instrument revealed a number of deficiencies in both structural characteristics of the websites reviewed as well as their ability to support shared decision-making. Websites were rated as good on a median of 3/7 structural characteristics questions, with one website rated as good on all questions (Figure 3). Criteria where websites most commonly were considered to be poor/fair included not providing adequate documentation to the sources of the information presented (69%) and not displaying a date of publication, leaving readers unable to determine if the information was up-to-date (47%). On the 9 questions that examined support of shared decision-making, websites were rated as “good” on a median of 1/9 questions. No single website scored well on all of the shared decision-making questions, with 47% (21/45) failing to achieve a “good” score on any question. Questions most commonly rated as poor/fair included: not describing the consequences of disease progression if surgery were not performed (93%), not explaining the benefits of either one or both surgical treatments (80%), not adequately describing the risks of the procedures (73%), and not discussing details of how surgical treatments are carried out (67%). In addition, 91% of the sites did not describe how treatment could affect long-term quality of life. Due to these important shortcomings, reviewers rated 82% of the websites to be of inadequate quality to be used as a source of information about treatment choices and 80% of the websites to be insufficient to support shared decision-making.
Figure 3.
Assessment of website quality of treatment information as assessed by the DISCERN criteria
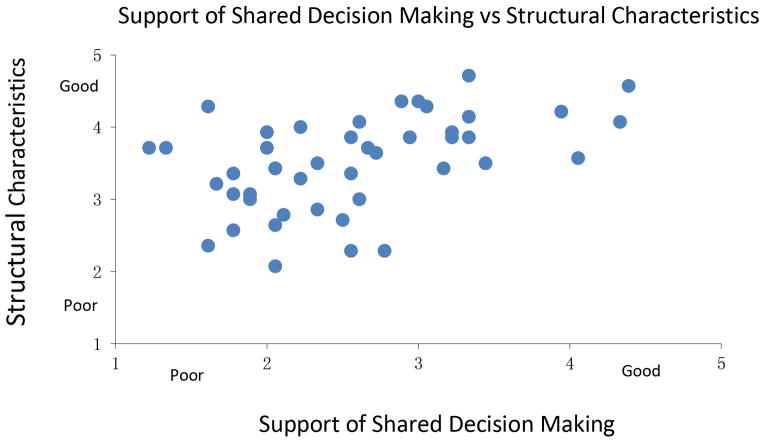
Figure 4 demonstrates how websites scored on Structural Characteristics relative to scores for Support of Shared Decision-Making. Significant differences in website performance across these two question categories were observed. Websites were more likely to score higher on questions examining structural characteristics [median 3.6 (2.1–4.7)] than on questions that assessed support of shared decision-making [median 2.6 (1.3–4.4)]. Four websites, all of which were hosted by cancer-focused non-profit organizations, stood out from the others with better performances in both structural characteristics [median 4.1 (3.6–4.6)] and support of shared decision-making [median 4.2 (3.9–4.4)].
Figure 4.
Assessment of websites’ DISCERN scores for the ability to supporting shared decision-making versus structural characteristics. Each website is represented by a dot on the graph.
DISCUSSION
Access to the internet has rapidly increased over the past decade, with an estimated 87% of adults using the internet as of 2014.[7] Many of these internet users will search the internet for health-related information. Disparities exist with regards to who uses the internet, with most studies suggesting that internet users tend to be younger, more affluent and more highly educated.[7,18] However, the rates of internet use have increased in all subgroups, and disparities due to inequalities in access appear to be decreasing.[18] More concerning is that disparities have also been observed in online information seeking, especially in patients with lower health literacy.11,18–22 Online information seeking requires skills beyond our usual conception of health literacy to include concepts such as computer literacy and information literacy (i.e. how to frame an appropriate search strategy and filter results to obtain relevant information).[19] Giving the growing abundance of information available on the internet, disparities in online information seeking are likely to increase as patients must sort through an increasingly large volume of information in search of high quality information.
The findings of the current study support this concern, as we found that identifying accurate, high-quality internet information on breast cancer surgery is challenging, even for individuals with high health literacy. We found that most patients will encounter serious challenges in identifying high-quality sources of information that will support them in being informed participants in treatment decision-making. While we did find that most websites were unbiased (76%) and contained information relevant to breast cancer and its treatments (73%), deficiencies in content areas felt to be essential for informed patient decision-making clearly highlight a fundamental incongruity between what information breast cancer patients may need and what is easily attainable online.
Only four websites were identified by our review as being of higher quality, with median DISCERN scores above 4 (the threshold for a “good” score). These websites represent the best sources of breast cancer surgery information currently available. However, when reviewed in further detail, even these websites were considered by the research team to be insufficient to meet the needs of newly diagnosed breast cancer patients seeking information. In general, these websites contained voluminous information that was not written for diverse patient populations with differing levels of health literacy. In addition, figures that facilitate comparisons of the two primary surgical treatments of breast cancer (important for patient decision-making) were sparse or not present. Perhaps most importantly, there were far too few patient prompts that encouraged patients to examine their treatment options in the context of their thoughts, feelings, fears, and goals. By our review, even the “best” available websites are insufficient to provide women with all of the knowledge they needed to be an equal partner with their physician in treatment decision-making for breast cancer surgery.
Our study does have some limitations. In this study, we attempted to recreate how the average patient would use the internet to find surgical treatment information after receiving a breast cancer diagnosis. Although our search terms have face validity, they may not reflect the true search practices of patients. Further, we undertook this study to assess, using a validated questionnaire, the ability of current online information to support patient decision-making for breast cancer surgery. However, this may not have been the original goal of website development and it is possible that some websites reviewed poorly in our study are actually doing a good job achieving the goal they were originally designed for. Finally, although we used a validated questionnaire specifically designed to assess the quality of patient targeted health information for treatment choices, there are other potentially important elements of website design that could meaningfully impact the user experience and patient education that we did not assess, such as effective use of interactive elements, attractiveness of layout, or personalized content.
CONCLUSIONS
Online health care information is an increasingly common way for breast cancer patients to gain knowledge about their disease and surgical treatment options. However, although numerous online sources of breast cancer information exist, our results found that it may be challenging for women to identify high quality sites that will provide them with essential information needed to play an active role in treatment decision-making. Our findings suggest that some simple steps that could be taken to facilitate assessment of the quality of information presented on a website include listing a date of publication to document that a site is up-to-date and citing references for the original sources of information. More extensive changes will be necessary to ensure that information included in a website is user-friendly and can support patient decision-making for breast cancer surgery. Examples include minimizing the amount of information communicated through text versus other media sources (i.e. video clips), designing sites to be intuitive for patients to navigate, and utilizing figures and pictures to highlights potential benefits and risk of various treatment options and facilitating direct comparisons. Although these changes would benefit all women, those with less education or of lower socioeconomic status may experience the most benefit given known disparities in online information-seeking. Providing easily-accessible, high quality online information that meets the needs of patients with diverse backgrounds has the potential to significantly improve the experiences of breast cancer patients facing a decision for breast cancer surgery.
Synopsis.
Current online sources of breast cancer information do not provide women with essential information necessary to actively participate in decision making for breast cancer surgery. Providing easily-accessible, high-quality online information has the potential to significantly improve patients’ experiences with decision-making.
Acknowledgments
Funding Sources: This project was funded with support from the Building Interdisciplinary Research Careers in Women’s Health Scholar Program (NIH K12 HD055894). Additional support came from the University of Wisconsin School of Medicine and Public Health Shapiro Summer Research Program.
Footnotes
No conflicts of interest.
References
- 1.Howlader N, Noone AM, Krapcho M, et al. SEER Cancer Statistics Review, 1975–2010. Bethesda, MD: National Cancer Institute; 2012. http://seer.cancer.gov/csr/1975_2010/, based on November 2012 SEER data submission, posted to the SEER web site, 2013. [Google Scholar]
- 2.Waljee JF, Rogers MA, Alderman AK. Decision aids and breast cancer: do they influence choice for surgery and knowledge of treatment options? Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2007;25:1067–1073. doi: 10.1200/JCO.2006.08.5472. [DOI] [PubMed] [Google Scholar]
- 3.Mandelblatt J, Kreling B, Figeuriedo M, Feng S. What is the impact of shared decision making on treatment and outcomes for older women with breast cancer? Journal of clinical oncology : official journal of the American Society of Clinical Oncology. 2006;24:4908–4913. doi: 10.1200/JCO.2006.07.1159. [DOI] [PubMed] [Google Scholar]
- 4.Holmes-Rovner M, Valade D, Orlowski C, et al. Implementing shared decision-making in routine practice: barriers and opportunities. Health expectations : an international journal of public participation in health care and health policy. 2000;3:182–191. doi: 10.1046/j.1369-6513.2000.00093.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Graham ID, Logan J, O’Connor A, et al. A qualitative study of physicians’ perceptions of three decision aids. Patient education and counseling. 2003;50:279–283. doi: 10.1016/s0738-3991(03)00050-8. [DOI] [PubMed] [Google Scholar]
- 6.O’Connor AM, Llewellyn-Thomas HA, Flood AB. Modifying unwarranted variations in health care: shared decision making using patient decision aids. Health Aff (Millwood) 2004;(Suppl Variation):VAR63–72. doi: 10.1377/hlthaff.var.63. [DOI] [PubMed] [Google Scholar]
- 7.Fox S, Duggan M. Health. Washington, D.C: Pew Research Center; 2013. Health Online 2013. [Google Scholar]
- 8.Morahan-Martin JM. How internet users find, evaluate, and use online health information: a cross-cultural review. Cyberpsychology & behavior : the impact of the Internet, multimedia and virtual reality on behavior and society. 2004;7:497–510. doi: 10.1089/cpb.2004.7.497. [DOI] [PubMed] [Google Scholar]
- 9.Webb TL, Joseph J, Yardley L, Michie S. Using the internet to promote health behavior change: a systematic review and meta-analysis of the impact of theoretical basis, use of behavior change techniques, and mode of delivery on efficacy. Journal of medical Internet research. 2010;12:e4. doi: 10.2196/jmir.1376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.McInnes N, Haglund BJ. Readability of online health information: implications for health literacy. Informatics for health & social care. 2011;36:173–189. doi: 10.3109/17538157.2010.542529. [DOI] [PubMed] [Google Scholar]
- 11.Lee CJ, Ramirez AS, Lewis N, et al. Looking beyond the Internet: examining socioeconomic inequalities in cancer information seeking among cancer patients. Health communication. 2012;27:806–817. doi: 10.1080/10410236.2011.647621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Google. In.
- 13.Bing. In.
- 14.comScore. U.S. Search Engine Rankings. Reston, VA: comScore, Inc; 2014. Releases April 2014. [Google Scholar]
- 15.Ghita M, Loiz D, Petrescu P. Google Organic CTR Study 2014. Craiova, Romania: Caphyon Advanced Web Ranking; 2014. [Google Scholar]
- 16.Lee CN, Dominik R, Levin CA, et al. Development of instruments to measure the quality of breast cancer treatment decisions. Health expectations : an international journal of public participation in health care and health policy. 2010;13:258–272. doi: 10.1111/j.1369-7625.2010.00600.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Charnock D, Shepperd S, Needham G, Gann R. DISCERN: an instrument for judging the quality of written consumer health information on treatment choices. Journal of epidemiology and community health. 1999;53:105–111. doi: 10.1136/jech.53.2.105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hesse BW, Gaysynsky A, Ottenbacher A, et al. Meeting the healthy people 2020 goals: using the Health Information National Trends Survey to monitor progress on health communication objectives. Journal of health communication. 2014;19:1497–1509. doi: 10.1080/10810730.2014.954084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Norman CD, Skinner HA. eHealth Literacy: Essential Skills for Consumer Health in a Networked World. Journal of medical Internet research. 2006;8:e9. doi: 10.2196/jmir.8.2.e9. [DOI] [PMC free article] [PubMed] [Google Scholar]