Abstract
The incidence of HIV/AIDS in India is increasing drastically, and truck drivers are seen as critical sources of HIV transmission due to their high rates of unprotected sex with multiple partners. An intervention based on the Information-Motivation-Behavioral (IMB) model was compared to an information-based control condition in a randomized trial. IMB constructs were assessed among 250 male truck drivers immediately prior to and following administration of the intervention which consisted or workshops which focused on motivating respondents to use condoms and a series of 5 interactive activities designed to address IMB conflicts. Condom use behavior was assessed approximately 10 months later. Findings showed mixed support for the effectiveness of the intervention. There was an effect of the IMB intervention on attitudes, norms, behavioral skills, and intentions specific to condom use with marital partners, but no effects on constructs related to non-marital partners. There was some evidence of greater condom use with marital and non-marital partners at behavioral follow-up for participants in the IMB condition, and effects on condom use with marital partners were mediated by changes in IMB constructs. These findings provide initial evidence for the effectiveness of theoretically-based approaches to HIV prevention in India.
Keywords: HIV/AIDS, Information-Motivation-Behavioural Model, prevention intervention, truck drivers, India
The first case of HIV infection in India was diagnosed in 1986 in a commercial sex worker in Chennai, Tamil Nadu (Dakar & Dakar, 2001). HIV has since spread dramatically throughout the country, with cases having been reported in all States and Union Territories. Although the overall HIV prevalence in India is believed to be less than 1%, India has one of the largest HIV-positive populations in the world, with 5.21 million infected individuals (NACO, 2006). This represents nearly 15% of the world’s HIV-infected population (UNAIDS, 2006) and 80% of Southeast Asia’s infected population (World Bank, 2005).
Heterosexual transmission is the main route of HIV transmission in India, and long distance truck drivers are seen as critical sources of HIV risk and transmission (Manjunath, Thappa, & Jaisankar, 2002). They account for as much as 12% of the HIV-infected adult population, with an infection rate that is up to 10 times higher than the national average (Lane, 2005). There are an estimated 3 to 5 million long distance truck drivers and “helpers” (apprentice truck drivers) in India, who spend extended periods of time away from their families, often stopping at “dhabas,” or roadside eateries, where it is quite common for them to pick up a sex worker, have sex with her, and then drop her off at the next dhaba. Anywhere from 70% to 90% of long distance truck drivers have multiple sexual partners, and only a very small percentage of them use condoms (Bryan, Fisher, & Benziger, 2001; Manjunath, Thappa, & Jaisankar, 2002; Rao, Pilli, Rao, & Chalam, 1999). Through their high risk sexual behavior, truck drivers not only put themselves and sex workers at risk for HIV, but also the general population when they return home and have sex with their primary and secondary partners (Bharat & Aggleton, 1999). Recent surveillance data have indicated that the epidemic is indeed spreading from high risk groups to the general population (NACO, 2005a, 2006; UNAIDS, 2004).
Although long distance truck drivers have long been implicated in the spread of HIV in India (Bansal & Nia, 1998), there has been relatively little use of behavioral science theory to develop theory-based HIV prevention interventions for this high risk population. There are several HIV prevention interventions currently being implemented with truck drivers (e.g., Healthy Highways Project – Family Health International, 2001; Operation Lighthouse – Population Services International, 2005), but most of them are atheoretical and focus primarily on disseminating information, not on increasing motivation and providing behavioral skills training. The majority has not been rigorously evaluated for their effectiveness, and when they are it is typically a process evaluation, where only the number of individuals participating in the intervention, not the degree of behavior change, is assessed. Those interventions that have been evaluated for their impact on risk behavior have used pre- and post-measures with no comparison group (e.g., Family Health International, 2001), making it virtually impossible to draw any definitive conclusions about the interventions’ effects (Cook & Campbell, 1979; Shadish, Cook, & Campbell, 2002). It is thus critically important to develop theory-based interventions that have empirically demonstrated effectiveness in reducing sexual risk behavior.
The current study employed the Information-Motivation-Behavioral Skills (IMB) model of HIV preventive behavior (J. Fisher & Fisher, 1992, 2000, 2002; W. Fisher & Fisher, 1993; W. Fisher, Fisher, & Harman, 2003) as the basis for the development, implementation, and evaluation of an intervention to reduce sexual risk behavior among Indian truck drivers. The IMB model asserts that HIV prevention information, motivation, and behavioral skills are the fundamental determinants of HIV preventive behavior. HIV prevention information includes facts about how HIV is transmitted and prevented, HIV prevention heuristics (e.g., “Any woman who is not married must be HIV-negative.”), and implicit theories of HIV risk, which hold that one can detect and avoid HIV by assessing a partner’s dress, demeanor, and social associations. HIV prevention motivation includes motivation constructs drawn from the Theory of Reasoned Action (Ajzen & Fishbein, 1980) (e.g., attitudes towards performing specific HIV preventive acts, perceptions of social support for performing HIV preventive acts, and behavioral intentions to engage in HIV preventive acts). The behavioral skills component of the model is composed of an individual’s objective ability and perceived self-efficacy for the performance of HIV-preventive behaviors (Bandura, 1989, 1994; J. Fisher & Fisher, 1992; W. Fisher & Fisher, 1993; Kelly & St. Lawrence, 1988). This model has been extensively validated in over 15 years of research with diverse populations in cross-cultural settings (see J. Fisher & Fisher, 2000).
Our IMB-based HIV prevention intervention for Indian truck drivers addressed the specific information, motivation, and behavioral skills deficits that were identified in elicitation research previously conducted with truck drivers in India (Bryan, Fisher, & Benziger, 2001). The intervention was implemented in the city of Chennai (population ~5 million), the leading industrial and commercial port in southern India. Chennai is the capital of Tamil Nadu, the state with the largest number of AIDS cases and one of the highest HIV prevalence rates in India (NACO, 2005b).
Due to the fact that long distance truck drivers are mobile and are rarely in one location for more than a few days, a single session workshop was developed that could be implemented where truckers congregate while they are waiting for their next assignment. In Chennai, truck drivers remain at the lorry sheds (locations where they park their trucks in between assignments) for one to three days before making their next delivery, so it was logical to conduct the intervention near these sheds. In order to reach the greatest number of truckers and to provide normative support for safer sexual practices, the intervention was offered in a group rather than an individual format. In order to ensure that the intervention was culturally appropriate to the target population of truck drivers and that it was feasible to implement in the chosen setting, the intervention was designed in close collaboration with the Benziger Foundation, a non-profit organization in Chennai that is dedicated to the eradication of HIV/AIDS in India. Effectiveness of the intervention was evaluated in a randomized controlled trial comparing the IMB-based intervention to an information-only control condition.
Method
Participants and Recruitment
Participants were recruited at the lorry booking offices throughout Chennai, India over a 6-week period in 2003 by two trained research staff (lay counselors) who worked for the Benziger Foundation. Truck drivers were individually approached and asked if they were interested in participating. Eligible participants were long distance drivers who resided in Tamil Nadu, were at least 18 years of age, and spoke fluent Tamil. The research staff described the study, and obtained informed consent from interested truckers. All participants were told that the study, entitled Truckers’ Health Project, involved completing 3 surveys about their sexual behavior and participating in a one-session group workshop about sexual health.
A total of 250 male participants were recruited for participation, with 125 participants in each condition (sample size was selected based on power of 0.80 to detect a small effect with estimated 25% attrition; Cohen, 1988). Participants ranged in age from 20 to 78 years, with a mean of 39. Most (78%) were lorry drivers who drove only in Tamil Nadu, and 92% were Hindu. Average monthly income ranged between 1,000 and 10,000 rupees, with a mean of 4870 rupees (approximately $100 U.S.). Most (98%) of the men were married (including all of the bisexual men), and had an average of 3 children. Most (95%) were heterosexual, and 5% were bisexual.
Procedures
This research protocol was approved by the Institutional Review Board (IRB) at the University of Connecticut, the Indian Council for Medical Research (ICMR), and by an IRB that was created specifically for this project in Chennai, India. Once participants consented to participate in the study, they were taken to a private location in the area of contact and administered a baseline survey by a member of the research staff. A second survey was administered immediately following the group workshop to assess changes in theoretical mediators (i.e., information, motivation, and behavioral skills), and a third behavioral survey was completed approximately 10 months later. At the 10-month follow-up, 194 participants (78%) had complete data that could be correctly linked to the baseline and immediate post-test surveys. Due to the low rates of literacy in India (Office of the Registrar General - India, 2001), all surveys were administered as structured, face-to-face individual interviews in Tamil. Participants were compensated 300 rupees ($6 to $7 U.S.) for each survey.
After completing the baseline measures, participants returned later in the day for the group workshop. A safe, private area was provided for each workshop through collaborations with the lorry booking offices. The workshops were randomly assigned to either the Information-Motivation-Behavioral Skills (IMB) intervention condition or to the Information-Only control condition. A total of 9 IMB intervention workshops and 8 control workshops were implemented with 11 to 16 truck drivers in each workshop. The workshops were each 4 hours long and co-facilitated in Tamil by two Masters level social workers.
Prior to intervention implementation, the social workers underwent an extensive 5-day training in either the IMB intervention or the information-only intervention (two social workers per intervention). The training included substantial role-play and rehearsal of the intervention protocol with detailed feedback on their individual performance. The social workers were not permitted to implement the protocol until they demonstrated that they could perform it to criteria; all four social workers met criteria. A fifth MSW who served as project manager for the study periodically observed the social workers and provided feedback as needed to ensure that the interventions were being delivered with fidelity.
IMB Intervention Workshop
The IMB intervention was developed based on the findings from the elicitation research (Bryan et al., 2001). Due to the high prevalence of extramarital sexual behavior among Indian truck drivers (Bryan et al., 2001; Manjunath et al., 2002; Rao et al., 1999), we believed that it would be extremely challenging to motivate them to be monogamous. Consequently, the intervention focused instead on motivating them to use condoms with all of their partners, consisting of 5 interactive activities that were designed to address each of the IMB constructs. Informational deficits were addressed in an activity entitled “Picture Your Health,” in which 19 flashcards with pictures of various objects, scenes, and people on them were used to stimulate discussion and educate truck drivers about the transmission and prevention of HIV/AIDS and other sexually transmitted infections (STIs), and to correct common misconceptions about them (e.g., the belief that engine heat adversely affects one’s sexual health and that penicillin injections taken prior to sex can prevent HIV and other STIs, etc.). This activity included information about the high prevalence of HIV among truck drivers and a discussion about how one cannot determine whether a person is infected by looking at them.
Negative attitudes about condoms were addressed in an activity entitled, “The Pros and Cons of Condom Use.” Participants were asked as a group to make a list of what they liked and disliked about condoms, and each negative attitude was countered with suggestions for how to decrease or minimize the negative aspects of condoms. With respect to behavioral skills, participants were taught through demonstration and rehearsal how to correctly store and use condoms. Each participant was provided with the opportunity to practice putting a condom on a model of a phallus, and they were given corrective feedback as they did so. During this activity, a variety of condoms were provided to participants, and they were informed where they could obtain free government condoms and purchase other brands. Safer sex communication skills were taught during a fourth activity in which participants were asked to role-play various scenarios in which they had to communicate with their partners (marital and non-marital) about sex and condom use. A fifth activity consisted of a discussion of the importance of getting tested for HIV and STIs, and participants were given a list of locations where they could do so.
Due to the fact that homosexual behavior is a taboo subject, highly stigmatizing (Reddy, 2005), and a punishable offense under The Indian Penal Code (1860; i.e., a person can be imprisoned for up to 10 years for engaging in sodomy), the intervention focused on sex between a man and a woman and avoided engaging in an explicit discussion about sex between men. There was concern that addressing male-to-male sex directly would alienate participants and inhibit our ability to have productive discussions about HIV prevention, and that it could put some of the participants at risk for severe legal and social repercussions. It should be noted, though, that intervention activities focused predominantly on behavior rather than on the gender of the partner, so that the intervention was relevant whether a participant’s partner was male or female.
Information-Only Control Workshop
The Information-Only workshop utilized a pre-written HIV prevention curriculum that had been used by numerous community-based organizations in Tamil Nadu with their clients. This 4-hour didactic and interactive group workshop provided information about nine different areas related to HIV/AIDS prevention, such as what HIV/AIDS is, the prevalence of AIDS in India and other parts of the world, how the immune system works, the different stages of HIV/AIDS, how HIV is and is not transmitted, how it is prevented, and other related information. The focus of the workshop was thus on providing information about HIV transmission and prevention, and not on increasing motivation or providing behavioral skills training. Condoms were also distributed at this workshop.
Outcome Measures
The measures of IMB constructs and risky sexual behavior were versions of previously validated instruments that were used with Indian truck drivers (Bryan et al., 2001). All survey measures were developed, piloted, revised, and translated into Tamil in collaboration with the Benziger Foundation.
Information
There were 18 information items answered on a “True,” “False,” or “Don’t Know,” scale. A participant’s score on the information scale consisted of the total number of correct responses out of 18 (“Don’t Know” was coded as incorrect). These items assessed participants’ beliefs about the proper use of condoms (e.g., “It is not safe to use condoms more than once.”), their beliefs about how to prevent HIV and other STIs (e.g., “Putting salt water or lemon juice, or both, on the genitals after having sex can keep you from getting sexually transmitted diseases.”), their misconceptions about how to cure HIV and other STIs (e.g., “Having intercourse with a virgin can cure sexually transmitted diseases.”), and the heuristics that they use to decide when it is safe to have unprotected sex with someone (“Once you trust your partner, you don’t need to use condoms with them.”).
Motivation to practice safer behavior was assessed as three separate dimensions: attitudes, norms, and behavioral intentions to engage in HIV preventive actions. All of the motivation items were assessed on 1–5 likert-type scales where each step on the scale was labeled appropriately for that question (e.g., most response options ranged from 1=“Disagree a Lot” to 5=“Agree a Lot”). Despite the fact that the measures had been validated in previous studies of the same population (Bryan et al., 2001), the items comprising each dimension of motivation unfortunately did not form reliable scales. Thus, in most cases individual items were either analyzed separately or combined into smaller subscales when it was conceptually appropriate to do so. In cases where subscales were formed, scores were computed as the mean of the items on that scale.
The items assessing attitudes toward condom use did not comprise a unitary scale, likely because the items addressed a wide variety of attitudes, such as attitudes about condoms (e.g., “Condoms are uncomfortable.”), about discussing safer sex (“Talking about condoms with any sexual partner would be embarrassing.”), and about having sex with people other than their wives (e.g., “I like having sex while I am on the road with women who are not my wife.”). Consequently, analyses were conducted on five subscales that conceptually addressed various aspects of attitudes: (1) attitudes toward condom use with non-marital partners (k = 2), (2) attitudes toward condom use with marital partners (k = 3), (3) attitudes regarding the naturalness of condoms (k = 2), (4) attitudes pertaining to perceived comfortableness of condoms (k = 2), and (5) attitudes toward buying and carrying condoms (k = 2).
Similarly, participants’ perceived norms for safer sexual behavior were assessed with 13 items that were broken down into five subscales of conceptually-related items: (1) norms for having sex outside of marriage (k = 3), (2) norms for condom use with non-marital partners (k = 3), (3) norms for condom use with marital partners (k = 1), (4) norms for talking to sexual partners about condom use (k = 3), and (5) norms for condom use being a man’s decision (k = 3). Finally, three separate aspects of intentions (within the time frame of “the next four months”) were assessed: (1) intentions to use condoms with non-marital partners (k = 2), (2) intentions to use condoms with marital partners (k = 1), and (3) intentions to buy condoms (k = 1).
Perceived behavioral skills for HIV prevention were assessed with 10 items that asked how “hard” or “easy” it was for patients to implement a variety of skills, including discussing sex and condom use with both marital and non-marital partners, and acquiring and using condoms. Response options ranged from 1=“Very Hard to Do” to 5=“Very Easy to Do.” The items were broken down into three conceptually-related subscales: (1) skills for talking about and using condoms with non-marital partners (k = 3), (2) skills for talking about and using condoms with marital partners (k = 3), and skills for buying and acquiring condoms (k = 4).
Risky sexual behavior
A number of questions pertaining to participants’ sexual behavior with their wives and non-marital partners (female and male) were asked at baseline and behavioral follow-up. The questions assessed frequency of vaginal and anal intercourse, number and types of partners (e.g., wife, sex worker, etc.), number of times condoms were used with marital and non-marital partners, frequency of condom use (as indicated on a 5-point scale ranging from “Never” to “Always”), use of other birth control methods (e.g., birth control pill, IUD, sterilization, and withdrawal), and alcohol use during sexual activity. An additional set of questions asked about any STIs participants had been diagnosed with in the past four months, and the treatment that they received for them. All of the behaviors were assessed with reference to “the past four months,” so that the baseline and follow-up measures of behavior would be equivalent.
Analytic Approach
First, we characterized the sample in terms of levels of baseline risky sexual behavior. The pretest equivalence of the two conditions on all measures was then examined, and univariate analyses of covariance (ANCOVA) examined the effect of intervention condition on the immediate post-test measures of IMB constructs and on risky sexual behavior at the long-term behavioral follow-up. Finally, a mediational model was estimated that examined the IMB constructs as mediators between intervention condition and condom use at behavioral follow-up. SAS Version 9.1 was used for all analyses, with the exception of the mediational model, in which Mplus Version 3.1 (Muthén & Muthén, 1998–2005) was used. Mplus includes the capability to test models using a full information (direct) maximum likelihood estimator (Arbuckle, 1996) to account for missing data.
Results
Description of sample
The total number of lifetime sexual partners ranged between 5 and 200 (M=41.99, mode=30). Number of sexual partners in the past four months ranged between 0 and 40 (M=12.71, mode=10). Most participants (93%) said they had had sex with someone who was not their wife in the past four months, and the average number of non-marital partners ranged between 2 and 40 (M=13.7, mode=12). Most men said they “never” (32.1%) and “rarely” (66.1%) used condoms with non-marital partners. The vast majority (96%) reported having intercourse with a commercial sex worker in the past four months. Birth control methods other than condoms with non-marital partners were extremely rare (e.g., fewer than 5% of participants reported using any alternative form of birth control). When asked how often they used a condom with marital partners in the past four months, 94% of the men said “never,” and none reported “always” using a condom with their wives. Instead of condoms, most married men reported either that no birth control was used with their wives (46%) or that their wives were sterilized (44%).
Alcohol use during sexual intercourse was quite high with both marital and non-marital partners: 80% of participants reported being under the influence of alcohol at the last intercourse episode with marital partners, and 82% reported being under the influence of alcohol at last intercourse with non-marital partners. There were few diagnosed cases of HIV and other STIs, likely because of low rates of testing (WHO/WPRO, 2005). Only 4.4% reported having been tested for an STI in the prior four months, with 4.2% being diagnosed with an STI; 2.2% reported ever having been tested for HIV, and none reported being HIV-positive.
Pretest equivalence of condition
The equivalence of the IMB and control groups at pretest was examined using t-tests for all continuous measures and χ2 difference tests for all categorical variables. Several significant differences between conditions at pretest were observed. Those in the IMB condition had a significantly higher number of children, lifetime sexual partners and number of partners in the prior four months. They were more likely to have had intercourse with non-marital partners in the prior four months, were less likely to masturbate when traveling, were less likely to have a sterilized wife, and were more likely to be under the influence of alcohol when having sex with non-marital partners. None of these constructs related to risky sexual behavior, however, so they were not included as covariates in subsequent analyses (West, Biesanz, & Pitts, 2000). The primary behavioral outcome of condom use with marital and non-marital partners did not differ by condition.
In terms of IMB model constructs, those in the IMB condition were less knowledgeable about HIV prevention-related information, expressed less favorable attitudes about the naturalness of condoms, and were more likely to endorse norms for having sex outside of marriage and for condom use being a man’s decision. Regardless of whether the pretest scores differed by condition, pretest scores on each outcome variable of interest were included as covariates for all subsequent analyses.
Posttest intervention outcomes
Univariate ANCOVAs were conducted to assess the effect of condition on each IMB construct at immediate posttest, covarying the pretest scores. Table 1 shows the effect of condition on post-test scores of information, attitudes, norms, intentions, and behavioral skills.1
Table 1.
Pretest and posttest means on program components and tests of group differences at pretest and posttest
| Program Component |
Experimental Means |
Control Means |
Pretest Differences (F-value) |
Posttest Effect of Condition (F-value) |
Cohen’s d Effect Size |
|---|---|---|---|---|---|
| Information: | |||||
| HIV-prevention information scores | |||||
| Pretest | 13.55 | 14.58 | 11.90*** | ||
| Posttest | 14.84 | 15.15 | 2.34 | −.26 | |
| Attitudes: | |||||
| Condoms with marital partners | |||||
| Pretest | 2.25 | 2.19 | .44 | ||
| Posttest | 2.58 | 2.21 | 10.79*** | .37 | |
| Condoms with non-marital partners | |||||
| Pretest | 2.59 | 2.59 | .0004 | ||
| Posttest | 2.63 | 2.79 | 1.44 | −.16 | |
| Naturalness of condoms | |||||
| Pretest | 2.89 | 3.33 | 10.50*** | ||
| Posttest | 3.60 | 3.66 | .19 | −.05 | |
| Comfortableness of condoms | |||||
| Pretest | 3.55 | 3.57 | .02 | ||
| Posttest | 3.30 | 3.20 | .42 | .09 | |
| Buying and carrying condoms | |||||
| Pretest | 2.88 | 2.73 | 2.28 | ||
| Posttest | 2.90 | 2.75 | 2.18 | .15 | |
| Norms: | |||||
| Using condoms with marital partners | |||||
| Pretest | 2.38 | 2.44 | .14 | ||
| Posttest | 3.24 | 2.83 | 4.68* | .40 | |
| Using condoms with non-marital partners | |||||
| Pretest | 2.86 | 2.73 | 1.23 | ||
| Posttest | 2.52 | 2.57 | .16 | −.05 | |
| Sex outside of marriage | |||||
| Pretest | 2.69 | 2.41 | 6.0* | ||
| Posttest | 2.86 | 2.93 | .34 | −.06 | |
| Talking about condoms | |||||
| Pretest | 3.33 | 3.26 | .36 | ||
| Posttest | 3.16 | 3.07 | .76 | .09 | |
| Condoms as a man’s decision | |||||
| Pretest | 2.79 | 2.45 | 6.45* | ||
| Posttest | 2.84 | 3.04 | 2.18 | −.16 | |
| Behavioral intentions: | |||||
| Intentions to use condoms with marital partners | |||||
| Pretest | 2.85 | 2.51 | 3.65 | ||
| Posttest | 2.51 | 2.15 | 4.10* | .36 | |
| Intentions to use condoms with non-marital partners | |||||
| Pretest | 2.59 | 2.61 | .02 | ||
| Posttest | 2.48 | 2.36 | .82 | .11 | |
| Intentions to buy condoms | |||||
| Pretest | 2.50 | 2.41 | .29 | ||
| Posttest | 3.17 | 2.70 | .7.91** | .48 | |
| Behavioral skills: | |||||
| Skills related to condom use with marital partners | |||||
| Pretest | 2.51 | 2.50 | .004 | ||
| Posttest | 2.53 | 2.10 | 18.26*** | .43 | |
| Skills related to condom use with non-marital partners | |||||
| Pretest | 2.48 | 2.49 | .006 | ||
| Posttest | 2.72 | 2.58 | 1.89 | .14 | |
| Skills for buying condoms | |||||
| Pretest | 2.63 | 2.53 | 2.04 | ||
| Posttest | 2.55 | 2.55 | .01 | .01 | |
Note.
p<.10,
p<.05,
p<.01,
p<.001
Effect size represents an estimate of Cohen’s d adjusted for pretest scores and can be evaluated in terms of the standard recommendations put forth by Cohen (1988) in which small, medium, and large effects are .20, .50, and .80, respectively. The numerator is the difference between means (μT − μC) so that negative effect size values indicate larger means in the control condition. The denominator term adjusts for pretest scores in that it is a function of the proportion of variance not accounted for after considering the correlation between pretest and posttest scores.
HIV-prevention information
As shown in Table 1, there was no significant effect of condition on information scores at post-test, as information scores increased in both the control and IMB conditions. This is not surprising, however, given that HIV-prevention information was provided in both conditions. It is notable that information scores across both conditions were, overall, quite high at both pretest and posttest. For example, all pretest questions, with the exception of four items, were answered correctly by 74%–98% of participants across conditions. The four items on which there were substantial deficits in knowledge [(1) oral sex is less risky than vaginal intercourse for transmitting HIV, (2) oil-based lubricants should not be used with condoms, (3) there is no cure for AIDS, and (4) taking antibiotics cannot keep you from getting sexually transmitted diseases] were answered correctly by 33%–58% of participants at pretest, and these percentages improved slightly to 38%–61% at posttest.
Motivation
Of the five subscales addressing attitudes, the only significant effect of condition was on attitudes toward condom use with marital partners (see Table 1). Similarly, there was a significant effect of condition on norms for using condoms with marital partners, but no effects on any of the other norm subscales. There was a significant effect of condition on intentions to buy condoms and to use condoms with marital partners, but no effect on intentions to use condoms with non-marital partners.
Behavioral skills
There was a significant effect of condition on skills related to condom use with marital partners, but not on skills related to condom use with non-marital partners, or buying and carrying condoms (see Table 1).
Effects of condition on behavior at follow-up
The effect of condition on later behavior was analyzed via univariate ANCOVAS for continuous outcomes (covarying pretest scores on each variable) and by χ2 tests for dichotomous items. Two broad categories of behavior were examined: sexual behavior (e.g., number of non-marital sexual partners) and condom use behavior with marital and non-marital partners.
Effects on sexual behavior
There were no effects of condition on whether participants had sex with someone other than their wife in the previous four months. At pretest, 93% of participants in both conditions had sex with someone other than their wife in the past four months. At follow-up, 89% in the control condition and 90% in the IMB condition had sex with someone other than their wife in the past four months, χ2 (1) = .05, p=.82. At pretest there was no difference between the IMB (97%) and control (94%) groups in the percentage of participants who had sex with a commercial sex worker in the previous four months (χ2 (1) = .58, p=.45). At follow-up, however, significantly fewer participants from the IMB condition (83%) than from the control condition (94%) had sex with a commercial sex worker, χ2 (1) = 4.61, p < .05. Finally, there was a significant effect of condition on total number of non-marital sexual partners in the prior four months, F (2, 168) = 10.63, p < .001; M = 18.81 in control; M = 15.91 in IMB.
Effect of condition on condom use behavior
Condom use behavior with both marital and non-marital partners was assessed at follow-up. Two types of questions were asked for each: (1) the total number of times condoms were used with each type of partner (e.g., In the past four months, how many times did you use condoms when you had sex with your wife?), and (2) frequency of condom use with marital and non-marital partners (e.g., How often did you and your wife use condoms when you had sexual intercourse, ranging from “never” to “always.”).
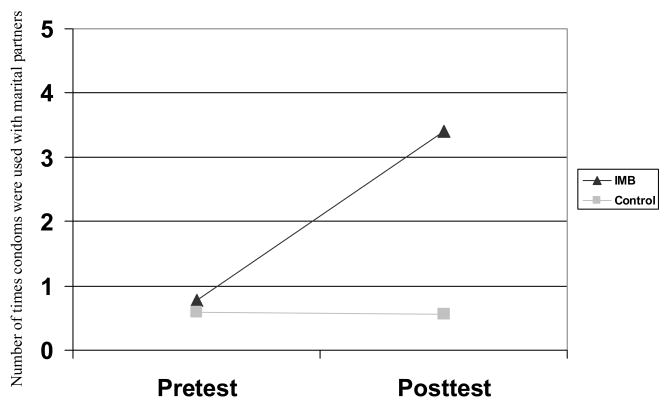
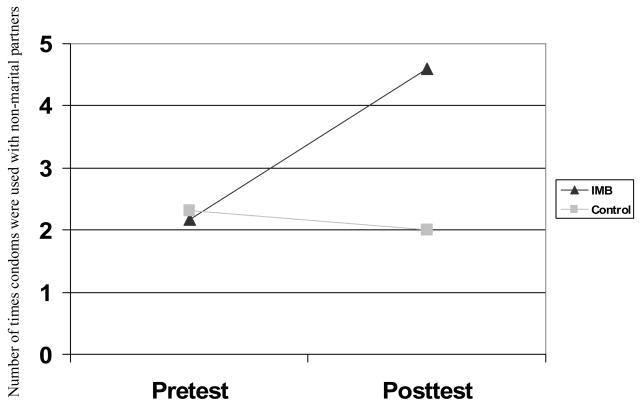
The ANCOVA showed a significant effect of condition on total number of times condoms were used with marital partners in the previous four months, F (1,133) = 21.21, p<.001 (see Figure 1). Specifically, condom use did not differ by condition at pretest (M = .59 in control; M = .77 in IMB), but did at follow-up (M = .56 in control; M = 3.40 in IMB). The distribution of frequency of condom use with marital partners was extremely skewed such that the vast majority of participants “never” used condoms with their wives. Thus, this variable was dichotomized to compare any condom use versus no condom use with wives. At pretest, there was no significant difference between IMB (9%) and control (5%) participants who said they had used condoms with their wives in the previous four months, χ2 (1) = .94, p=.33. At follow-up, however, significantly more participants from the IMB condition (14%) than from the control condition (3%) said they had used condoms with their wives in the previous four months, χ2 (1) = 5.75, p<.05. There was also a significant effect of condition on number of times condoms were used with non-marital partners, F (1,157) = 30.93, p < .001 (see Figure 2), with a significant difference between conditions at follow-up (M = 2.01 in control; M = 4.60 in IMB) but not at pretest (M = 2.31 in control; M = 2.17 in IMB). The effect of condition on frequency of condom use with non-marital partners approached significance, F (2, 167) = 3.71, p=.056; M = 1.64 in control; M = 1.74 in IMB, again favoring the IMB condition.
Figure 1.
Effect of condition on number of times condoms were used with marital partners, F (1,133) = 21.21, p<.001. Possible range: 0 and higher.
Figure 2.
Effect of condition on number of times condoms were used with non-marital partners, F (1,157) = 30.93, p < .001. Possible range: 0 and higher.
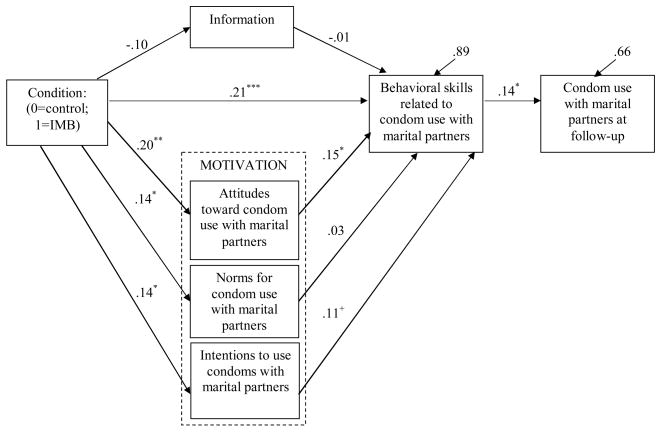
Mediation
Because there were program effects on IMB constructs that were specific to condom use with marital partners, a single mediational model was specified to examine whether these effects mediated the relationships between condition and condom use with marital partners at follow-up (see Figure 3). Pretest scores on each model construct were included as covariates. Consistent with the IMB model, it was expected that the effects of condition, information, and motivation on condom use would be completely mediated by behavioral skills.
Figure 3.
Mediational model demonstrating IMB constructs as mediators between program condition and condom use with marital partners at follow-up. Model Fit: χ2 (35) = 59.59, p < .01, CFI=.85, RMSEA=.05, SRMR=.05; +p<.10, * p<.05, **p<.01, ***p<.001.
As shown, and consistent with the univariate ANCOVAs, there was a significant effect of condition on attitudes, norms, intentions, and behavioral skills for condom use with marital partners. Attitudes significantly and intentions marginally predicted behavioral skills which, in turn, predicted condom use with marital partners at the behavioral follow-up (β = .14, p < .05). The model accounted for 34% of the variance in condom use at follow-up, and 11% of the variance in behavioral skills. There was adequate fit of the model to the data (χ2 (35) = 59.59, p < .01, CFI=.85, RMSEA=.05, SRMR=.05). Examination of the significance of the mediated effect showed that there was a significant total indirect effect of condition on condom use through the combination of IMB constructs (z = 1.95, p = .05) and that the specific indirect effect of condition on condom use through behavioral skills approached significance (z = 1.84, p = .07).
Attrition
Differential rates of attrition between the IMB and control groups was assessed by calculating the interaction between attrition at follow-up (0=retained; 1=not retained) and condition (0=control; 1=IMB) on all pretest measures (Jurs & Glass, 1971). Of the 31 tests conducted (17 IMB constructs; 6 demographic variables; 8 behavioral variables), the only significant interaction was on knowledge scores at pretest, F(3, 246) = 4.44, p < .05, such that those in the IMB condition who were lost to attrition demonstrated lower knowledge scores at pretest than participants in the other three conditions. Although this pattern could have been problematic, information was not impacted by the intervention, nor did it predict behavioral skills or condom use. Furthermore, given the sheer number of tests conducted, this single significant interaction might also be attributed to chance.
Discussion
A single-session IMB model-based HIV risk reduction intervention that targeted truck drivers in Chennai, India was developed, implemented, and evaluated relative to an information-only control. Consistent with previous findings (Bryan et al., 2001), participants in this study reported high levels of risky sexual behavior at baseline. Findings confirmed that those exposed to the IMB-based intervention demonstrated more positive attitudes toward, perception of greater normative support for, greater self-efficacy for, and greater intentions toward use of condoms with marital partners. Surprisingly, there were no effects on motivation or behavioral skills for condom use with non-marital partners.
Follow-up data showed greater condom use among marital and non-marital partners observed 10 months later in the IMB condition. Importantly, program effects on condom use with marital partners were mediated by changes to IMB constructs, and the model accounted for 34% of the variance in condom use at follow-up. This provides initial evidence that implementing an intervention that provides the necessary informational, motivational, and behavioral skills content can significantly impact truck drivers’ risky sexual practices.
There is still a great deal of variance unaccounted for, however, indicating that there are additional factors that need to be identified and addressed in order to more effectively reduce risky sexual behavior. As an example, a substantial number of participants indicated drinking alcohol while engaging in risky sexual activity. Future programs might do well to include IMB components that address HIV prevention while under the influence of alcohol. Futhermore, because there were no significant effects of the IMB intervention on participants’ motivation or behavioral skills regarding condom use with non-marital partners, the mechanisms underlying changes to condom use behavior with non-marital partners remain unknown.
The finding that the IMB intervention was most effective on the IMB constructs and on condom use specific to marital partners is somewhat counterintuitive. At the inception of this study, it was anticipated that it might be more difficult for men to introduce condoms into marital than non-marital relationships because of the possible conflict it could create (i.e., wives might question the need to use condoms in a monogamous relationship). Gender role norms in India could potentially explain these findings. For men in India, an essential part of their masculine identity is the role of provider (Anandhi & Jeyaranjan, 2002; Kimar, Gupta, & Abraham, 2002). A man who is not able to adequately protect his wife is considered unmanly, and thus infecting her with HIV or other STI could damage his masculine self-esteem. The IMB intervention encouraged condom use with both martial and non-marital partners as a means of protecting the truck drivers’ own health and the health of their wives. It may be that in their role as “protector,” men chose to use condoms with their wives as the most direct way to protect them. Additional research is needed to better understand the dynamics of risk behavior with marital versus non-marital partners and to determine how best to motivate truck drivers to use condoms with their non-marital partners.
Although the IMB-based intervention resulted in a significant increase in condom use with marital partners, it is important to note that condom use remained very low. Considering the high number of extramarital partners, the infrequent use of condoms, and the strong normative support for these behaviors, it is not surprising that a single session intervention was not associated with larger effects. The fact that a single session intervention impacted behavior at all, however, is noteworthy, particularly given the 10-month time lag between assessments. The duration of these effects suggest that an IMB-based intervention that provides additional dosages of the intervention may have even greater impact on truck drivers’ sexual behavior, particularly if the additional sessions can more fully address the practice of safer sex while under the influence of alcohol and negotiating safer sex with non-marital partners. This is supported by literature demonstrating that multi-session HIV/STI prevention interventions result in greater behavior change than single session interventions (IOM, 2001; Johnson-Masotti, Laud, Hoffman, Hayat, & Pinkerton, 2001; Kalichman, Carey, & Johnson, 1996). The challenge for working with truck drivers, however, is that they are extremely mobile, and it would be virtually impossible to maintain the same group members from session to session. Consequently, any multi-session group workshop would have to be designed so that the membership of a particular group could change.
One limitation of this study was that the items assessing attitudes, perceived norms, and behavioral skills did not comprise unitary scales, and the subscales comprised of conceptually-related items were assessed by a limited number of items (1 to 4 items). These limitations with regard to measurement underscore some of the difficulties in conducting international research. A second limitation was the significant baseline differences between conditions on several variables. These differences may have been due to groups rather than individuals being randomized to condition. A third limitation was the fact that the information-only intervention was less interactive and more didactic than the IMB intervention, potentially causing participants to be less engaged in the control intervention and thus less likely to make behavioral changes. Finally, attrition and reliance on self-reports of sexual behavior also limit our findings.
Recommendations for future research include exploring how to most effectively and safely address the HIV prevention needs of truck drivers who have sex with men in India, identifying the number of workshop sessions needed to maximize change and minimize attrition among truck drivers, and determining how to motivate truck drivers to use condoms with their non-marital partners. Additional research is also needed to explore the relationship between alcohol use and HIV prevention-related information, motivation, and behavioral skills, and how to incorporate those relationships into an effective prevention intervention. With their high levels of risk behavior and multiple sexual partners, it is critically important to develop optimally effective interventions with truck drivers as a means of stemming the spread of HIV in India.
Acknowledgments
The authors acknowledge with thanks the assistance of T. Joseph Benziger and his staff at the Benziger Foundation in conducting this research.
Footnotes
It was possible that the independence of observations assumption was violated because the control and IMB programs were administered in groups. To examine the extent to which observations were non-independent, intraclass correlation values were calculated and ranged from .00 to .35. Given that a few intraclass correlation values exceeded an acceptable cut-off, all analyses were redone in a mixed model framework to account for group membership. The conclusions were the same for every measure, with the exception of norms for using condoms with marital partners, F (1, 15) = 2.01, p = .18, and intentions to use condoms with marital partners, F (1, 15) = 1.85, p = .19. The direction of findings remained the same for both of these outcomes, but there were drops in significance.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Dr. Deborah H Cornman, Email: deborah.cornman@uconn.edu, University of Connecticut Storrs, CT UNITED STATES.
Sarah J Schmiege, Email: Sarah.Schmiege@colorado.edu, University of Colorado at Boulder
T. Joseph Benziger, Benziger Foundation at Chennai, India.
Angela Bryan, Email: angela.bryan@colorado.edu, University of Colorado at Boulder
Jeffrey D Fisher, Email: jeffrey.fisher@uconn.edu, University of Connecticut
References
- Ajzen I, Fishbein M. Understanding attitudes and predicting social behavior. Englewood Cliffs, NJ: Prentice-Hall; 1980. [Google Scholar]
- Anandhi S, Jeyaranjan J. Men, masculinity and domestic violence in India: Summary report of four studies. Washington, DC: International Center for Research on Women; 2002. Masculinity and domestic violence in a Tamil Nadu village; pp. 6–15. [Google Scholar]
- Arbuckle JL. Full information estimation in the presence of incomplete data. In: Marcoulides GA, Schumacker RE, editors. Advanced Structural Equation Modeling: Issues and Techniques. Mahwah, NJ: Erlbaum; 1996. pp. 243–277. [Google Scholar]
- Bandura A. Perceived self-efficacy in the exercise of control over AIDS infection. In: Mays VM, Albee GW, Schneider SM, editors. Primary prevention of AIDS. Newbury Park, CA: Sage; 1989. pp. 128–41. [Google Scholar]
- Bandura A. Social cognitive theory and exercise of control over HIV infection. In: DiClemente RJ, Peterson JL, editors. Preventing AIDS: Theories and methods of behavioral interventions. New York: Plenum; 1994. pp. 25–59. [Google Scholar]
- Bansal RK, Nia AB. Truck crew and risk of contraction of STDS, including HIV: Encouraging the use of condoms by the method of applying theories. Indian Journal of Medical Science. 1998;52(6):253–264. [PubMed] [Google Scholar]
- Bharat S, Aggleton P. Facing the challenge: Household responses to HIV/AIDS in Mumai, India. AIDS Care. 1999;11:31–44. doi: 10.1080/09540129948180. [DOI] [PubMed] [Google Scholar]
- Bryan AD, Fisher JD, Benziger TJ. Determinants of HIV risk behavior among Indian truck drivers. Social Science and Medicine. 2001;53:1413–1426. doi: 10.1016/s0277-9536(00)00435-4. [DOI] [PubMed] [Google Scholar]
- Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale, NJ: Lawrence Erlbaum Associate; 1988. [Google Scholar]
- Cook TD, Campbell DT. Quasi-experimentation: Design and analysis issues for field settings. Chicago: Rand McNally; 1979. [Google Scholar]
- Dakar DN, Dakar SN. Combating AIDS in the 21st century: Issues and challenges. New Delhi, India: Sterling Publishers Private Limited; 2001. [Google Scholar]
- Family Health International. Summary report: Behavioural surveillance survey in Healthy Highway Project, India. 2001. Retrieved March 9, 2006 from, http://www.fhi.org/en/HIVAIDS/pub/survreports/BSSHealthyHwy/index.htm.
- Fisher JD, Fisher WA. Changing AIDS risk behavior. Psychological Bulletin. 1992;111:455–474. doi: 10.1037/0033-2909.111.3.455. [DOI] [PubMed] [Google Scholar]
- Fisher JD, Fisher WA. Theoretical approaches to individual-level change in HIV-Risk Behavior. In: Peterson J, DiClemente R, editors. HIV prevention handbook. New York: Plenum; 2000. pp. 3–55. [Google Scholar]
- Fisher JD, Fisher WA. The information-motivation-behavioral skills model. In: DiClemente R, Crosby R, Kegler R, editors. Emerging Promotion Research and Practice. San Francisco, CA: Josey Bass Publishers; 2002. pp. 40–70. [Google Scholar]
- Fisher WA, Fisher JD. Understanding and promoting AIDS preventive behavior: A conceptual model and educational tools. The Canadian Journal of Human Sexuality. 1993;1:99–106. [Google Scholar]
- Fisher WA, Fisher JD, Harman JJ. The information-motivation-behavioral skills model: A general social psychological approach to understanding and promoting health behavior. In: Suls J, Wallston KA, editors. Social psychological foundations of health and illness. Walden, MA: Blackwell Publishing; 2003. pp. 82–106. [Google Scholar]
- Ruiz MS, Gable AB, Kaplan EH, Stoto MA, Fineberg HV, Trussell J, editors. Institute of Medicine (IOM) No time to lose: Getting more from HIV prevention. Washington, DC: National Academy Press; 2001. [PubMed] [Google Scholar]
- Johnson-Masotti AP, Laud PW, Hoffman RG, Hayat MJ, Pinkerton SD. Probabilistic cost-effectiveness analysis of HIV prevention: Comparing a Bayesian approach with traditional deterministic sensitivity analysis. Evaluation Review. 2001;25(4):474–502. doi: 10.1177/0193841X0102500404. [DOI] [PubMed] [Google Scholar]
- Jurs SG, Glass GV. The effect of experimental mortality on the internal and external validity of the randomized comparative experiment. Journal of Experimental Education. 1971;40:62–66. [Google Scholar]
- Kalichman SC, Carey MP, Johnson BT. Prevention of sexually transmitted HIV infection: A meta-analytic review of the behavioral outcome literature. Annals of Behavioral Medicine. 1996;18:6–15. doi: 10.1007/BF02903934. [DOI] [PubMed] [Google Scholar]
- Kelly JA, St Lawrence JS. AIDS prevention and treatment: Psychology’s role in the health crisis. Clinical Psychology Review. 1988;8:255–284. [Google Scholar]
- Kimar CS, Gupta SD, Abraham G. Men, masculinity and domestic violence in India: Summary report of four studies. Washington DC: International Center for Research on Women; 2002. Masculinity and violence against women in marriage: An exploratory study in Rajasthan; pp. 6–15. [Google Scholar]
- Lane E. Sex education steers India’s truckers away from AIDS highway. Agence France-Presse. 2005. Feb 6, Retrieved March 9, 2006, from http://www.aegis.com/NEWS/AFP/2005/AF050212.html.
- Manjunath JV, Thappa DM, Jaisankar TJ. Sexually transmitted diseases and sexual lifestyles of long-distance truck drivers: A clinico-epidemiologic study in south India. International Journal of STDs and AIDS. 2002;13(9):612–617. doi: 10.1258/09564620260216317. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. 3. Los Angeles, CA: Muthén & Muthén; 1998–2005. [Google Scholar]
- NACO. Facts & figures: An overview of the spread and prevalence of HIV/AIDS in India. Ministry of Health & Family Welfare, Government of India; 2005a. Retrieved March 9, 2006, from http://www.nacoonline.org/facts_overview.htm. [Google Scholar]
- NACO. Facts & Figures: Observed HIV prevalence levels state wise: 1998–2004. Ministry of Health & Family Welfare, Government of India; 2005b. Retrieved March 9, 2006, from http://www.nacoonline.org/facts_statewise.htm. [Google Scholar]
- NACO. HIV/AIDS epidemiological surveillance & estimation report for the year 2005. Ministry of Health & Family Welfare, Government of India; 2006. Apr, Retrieved September 19, 2006, from http://www.nacoonline.org/fnlapil06rprt.pdf. [Google Scholar]
- Office of the Registrar General, India. Literacy Rate: India. Census of India 2001. 2001. Retrieved March 9, 2006, from http://www.censusindia.net/results/provindia3.html.
- Population Services International. India’s Operation Lighthouse. 2005. Retrieved March 9, 2006 from http://www.psi.org/resources/pubs/OPL.pdf.
- Rao KS, Pilli RD, Rao AS, Chalam PS. Sexual lifestyle of long distance lorry drivers in India: Questionnaire survey. British Medical Journal. 1999;318:162–163. doi: 10.1136/bmj.318.7177.162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reddy G. Geographies of contagion: Hijras, kothis, and the politics of sexual marginality in Hyderabad. Anthropology & Medicine. 2005;12(3):255–270. doi: 10.1080/13648470500291410. [DOI] [PubMed] [Google Scholar]
- Shadish WR, Cook TD, Campbell DT. Experimental and Quasi- Experimental Designs for Generalized Causal Inference. Boston: Houghton-Mifflin; 2002. [Google Scholar]
- The Indian Penal Code. 1860. Retrieved September 19, 2006, from http://www.indialawinfo.com/bareacts/ipc.html.
- UNAIDS. UNAIDS India: HIV epidemic in India. 2004. Retrieved March 9, 2006, from http://www.unaids.org.in/displaymore.asp?itemid=56&chkey=76&subchkey=0&chname=HIV%20Epidemic%20in%20India.
- UNAIDS. 2006 report on the global AIDS epidemic. 2006. Retrieved September 19, 2006, from http://www.unaids.org/en/HIV_data/2006GlobalReport/default.asp.
- West SG, Aiken LS. Toward understanding individual effects in multicomponent prevention programs: Design and analysis strategies. In: Bryant KJ, Windle M, West SG, editors. The science of prevention: Methodological advances from alcohol and substance abuse research. Washington, DC: American Psychological Association; 1997. [Google Scholar]
- West SG, Biesanz JC, Pitts SC. Causal inference and generalization in field settings: Experimental and quasi-experimental designs. In: Reis HT, Judd CM, editors. Handbook of research methods in social and personality psychology. New York: Cambridge University Press; 2000. pp. 40–84. [Google Scholar]
- World Bank. HIV/AIDS in South Asia. 2005. May, Retrieved March 9, 2006, from http://siteresources.worldbank.org/INTSOUTHASIA/Resources/HIV-AIDS-brief-05-2005a.pdf.
- World Health Organization/Regional Office for the Western Pacific (WHO/WPRO) Training manual on STD case management: The syndromic approach for primary health care settings. HIV/AIDS and sexually transmitted infections. 2005. Retrieved March 9, 2006, from http://www.wpro.who.int/sites/hsi/documents/Training+Manual+on+STD+Case+Manageent.htm.