SUMMARY
Drinking raw date palm sap is the primary route of Nipah virus (NiV) transmission from bats to people in Bangladesh; subsequent person-to-person transmission is common. During December 2010 to March 2011, we investigated NiV epidemiology by interviewing cases using structured questionnaires, in-depth interviews, and group discussions to collect clinical and exposure histories. We conducted a case-control study to identify risk factors for transmission. We identified 43 cases; 23 were laboratory-confirmed and 20 probable. Thirty-eight (88%) cases died. Drinking raw date palm sap and contact with an infected person were major risk factors; one healthcare worker was infected and for another case transmission apparently occurred through contact with a corpse. In absence of these risk factors, apparent routes of transmission included drinking fermented date palm sap. For the first time, a case was detected in eastern Bangladesh. Identification of new epidemiological characteristics emphasizes the importance of continued NiV surveillance and case investigation.
Keywords: Encephalitis, Nipah virus, nosocomial infection, outbreak
INTRODUCTION
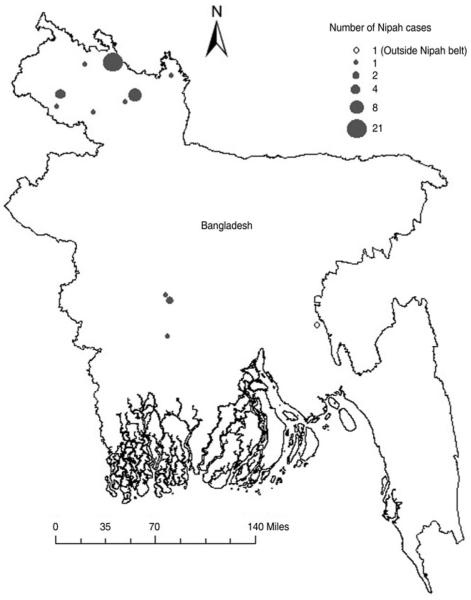
Nipah virus (NiV) is a zoonotic paramyxovirus that causes severe illness in humans often manifested as encephalitis [1]. Cases may also present with acute respiratory syndrome, manifested as cough with respiratory distress [1–5]. Nipah cases detected in Bangladesh through surveillance and outbreak investigations during 2001–2010 have all occurred during December–May in a geographically limited area in the northwestern and central parts of Bangladesh, often referred to as the ‘Nipah belt’ (Fig. 1) [4–9]. NiV infections in Bangladesh have a case-fatality ratio of >70% [8].
Fig. 1.
Geographical location of Nipah encephalitis cases identified during the 2010–2011 Nipah season in Bangladesh.
Outbreak investigations have identified drinking raw date palm sap, a delicacy in Bangladesh [10], as the most frequent route of transmission of NiV from bats to humans [6, 8, 11, 12]. Raw date palm sap is harvested during the winter months (December–March) [10], which is also the period when most of the Nipah cases are identified in Bangladesh [8, 10] and is therefore often referred to as the ‘Nipah season’ [9]. Studies using infrared cameras have shown that Pteropus fruit bats, the reservoir hosts of NiV [13], visit the date palm trees at night and contaminate the sap by licking the sap stream and urinating in the sap collection pot [14]. Another common pathway for NiV transmission to humans is through close contact with a person infected with NiV, most likely through contact with patient’s respiratory secretions [7, 8, 12, 15]. In Bangladesh, most of the cases that were infected through person-to-person transmission, were family caregivers who provided care to Nipah cases at home and in hospital [8]. Nosocomial transmission of NiV to healthcare providers has also been reported in India and Bangladesh [12, 16]. Corpse-to-human transmission of Nipah infection was also reported during an outbreak in March 2010 [12].
Since 2006, the Bangladesh Ministry of Health and Family Welfare’s Institute of Epidemiology, Disease Control and Research (IEDCR) and the International Centre for Diarrhoeal Diseases Research (icddr,b) have been jointly conducting hospital-based surveillance for cases and clusters of NiV infection [17].
From December 2010 to March 2011, a collaborative team of epidemiologists and qualitative investigators from IEDCR and icddr,b investigated multiple clusters and isolated cases of NiV infection in Bangladesh. The objectives of these investigations were to describe the NiV cases in terms of time, place and persons and to identify risk factors for transmission. Here we present the findings of epidemiological and anthropological investigations of NiV cases identified during the 2010–2011 Nipah season.
METHODS
Case and cluster detection
Physicians in three sentinel Nipah surveillance hospitals investigated and reported all suspected cases and clusters of acute encephalitis admitted to the hospital during January–March to IEDCR. A suspected case of acute encephalitis was defined as a person with acute onset of fever and altered mental status or new onset of seizure or other neurological deficit. A cluster was defined as an occurrence of two or more cases of suspected acute encephalitis within 21 days which were within 30 min walking distance of each other. The physicians collected whole blood samples from suspected cases and serum was stored in liquid nitrogen and transported bi-weekly to the IEDCR virology laboratory and tested for Nipah IgM and IgG anti-bodies using an enzyme-linked immunosorbent assay [18]. We defined a confirmed case of Nipah as a suspected case of acute encephalitis with evidence of NiV antibodies in serum.
Physicians from public and private hospitals occasionally reported encephalitis cases to IEDCR and requested laboratory confirmation when, based on the geographical location or history of consumption of date palm sap they suspected that patients might have been infected by NiV.
We launched epidemiological investigations whenever a laboratory-confirmed Nipah case or a cluster of acute encephalitis was detected through any of these surveillance systems.
Case and cluster investigations
We visited each community where there was at least one confirmed case and asked family members, friends and neighbours of confirmed cases to identify suspected Nipah cases and clusters. We defined a suspected Nipah case as any resident in a village where a confirmed Nipah encephalitis case lived who developed fever within 21 days of onset of illness of the confirmed Nipah case. We collected blood samples from living suspected cases. Samples were centrifuged in the field, and sera were aliquoted and transported in liquid nitrogen to IEDCR’s virology laboratory. A suspected Nipah case with evidence of NiV antibodies in serum was defined as a confirmed case. Suspected Nipah cases who died before a sample could be obtained or who had no IgM against NiV in a serum sample that was collected within 8 days of onset of illness and who died before a follow-up serum sample could be obtained were defined as probable cases.
We used a structured questionnaire to collect age, gender, symptoms with date of onset and exposure history during 30 days prior to illness onset from each probable and confirmed case. We interviewed family members, friends or caregivers of cases as proxy respondents for those cases who were too sick to respond or had died.
During investigation of two large clusters, in Lalmonirhat and Rangpur districts, researchers trained in qualitative methods conducted in-depth interviews and informal group discussions with families and friends of confirmed and probable cases to explore cases’ history of food and drink consumption and exposure to sick persons during the 30 days prior to illness onset. The team stayed in the affected villages for a week, built a rapport with community residents and conducted interviews and group discussions. The team recorded the interviews using audio recorders. We transcribed and summarized the interviews and group discussion data. We reviewed the data carefully to identify and summarize common behaviours and experiences of cases.
Case-control study
To investigate exposures associated with the cases we conducted a case-control study. Using methods described by Sazzad et al. [12], we enrolled probable and confirmed cases as case-patients and four age-matched healthy neighborhood controls for each case in the case-control study.
Statistical analysis
We calculated frequencies of demographic and clinical characteristics of cases. We calculated odds ratios (OR) and 95% confidence intervals (CI) to estimate the association of each exposure with disease using univariate conditional logistic regression. To evaluate independent risk factors we included all variables with a P value of <0.10 from univariate analyses in conditional stepwise backward multivariate logistic regression. We considered an association statistically significant if the associated P value was <0.05. We assessed multicollinearity between independent variables using variance inflation factor.
Ethics
We obtained informed verbal consent from all participants or proxies. We obtained individual assent as well as parental consent for those aged <11 years. The human subjects review committee at icddr,b approved the protocol for Nipah surveillance and outbreak response.
RESULTS
Case and cluster detection
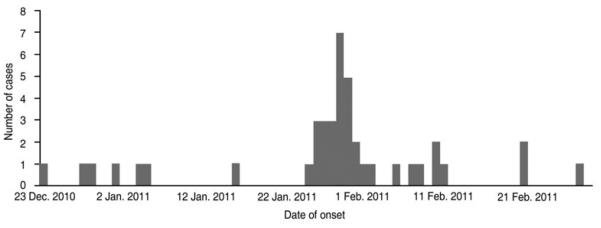
We identified 43 cases of Nipah encephalitis (23 confirmed, 20 probable) (Table 1). There were 37 cases in four clusters: three clusters occurred in three northern districts, Lalmonirhat (22 cases), Rangpur (eight cases), and Dinajpur (five cases), and the fourth cluster was in Rajbari District (two cases), in central Bangladesh (Fig. 1). All four clusters were detected through hospital-based Nipah surveillance. The remaining six cases were isolated, five of which were detected through hospital-based surveillance. The sixth was reported by physicians from a private hospital in Dhaka (Fig. 1). The onset of illness for the 43 cases was from 23 December 2010 to 1 March 2011 (Fig. 2).
Table 1.
Demographic and clinical characteristics of Nipah encephalitis cases by cluster identified during 2010–2011 Nipah season in Bangladesh (N = 43)
| Cluster/isolated case … Feature |
Lalmonirhat (N = 22) n (%) |
Dinajpur (N = 5) n (%) |
Rajbari (N = 2) n (%) |
Rangpur (N = 8) n (%) |
Isolated cases (N = 6) n (%) |
Total (N = 43) n (%) |
|---|---|---|---|---|---|---|
| Confirmed cases | 10 (45) | 2 (40) | 1 (50) | 4 (50) | 6 (100) | 23 (54) |
| Probable cases | 12 (55) | 3 (60) | 1 (50) | 4 (50) | 0 (0) | 20 (46) |
| Male | 18 (82) | 3 (60) | 6 (0) | 5 (63) | 4 (67) | 30 (70) |
| Median age, yr (range) | 18 (2–55) | 40 (23–50) | 16.2 (2.3–30) | 33.5 (5–45) | 19.5 (6–30) | 25 (2–55) |
| Fever | 22 (100) | 5 (100) | 2 (100) | 8 (100) | 6 (100) | 43 (100) |
| Altered consciousness | 21 (95) | 4 (80) | 2 (100) | 5 (63) | 6 (100) | 38 (88) |
| Headache | 19 (86) | 2 (40) | 1 (50) | 8 (100) | 5 (83) | 35 (81) |
| Severe weakness | 16 (73) | 4 (80) | 2 (100) | 8 (100) | 5 (83) | 35 (81) |
| Drowsiness | 15 (68) | 3 (60) | 1 (50) | 8 (100) | 5 (83) | 32 (74) |
| Difficulty breathing | 15 (68) | 1 (20) | 1 (50) | 5 (63) | 5 (83) | 27 (63) |
| Cough | 15 (68) | 2 (40) | 0 (0) | 5 (63) | 3 (50) | 25 (58) |
| Vomiting | 13 (59) | 0 (0) | 1 (50) | 4 (50) | 4 (67) | 22 (51) |
| Convulsion | 10 (45) | 2 (40) | 1 (50) | 4 (50) | 5 (83) | 22 (51) |
| Muscle pain | 8 (36) | 3 (60) | 1 (50) | 5 (63) | 3 (50) | 20 (47) |
| Change in personality | 9 (41) | 3 (60) | 1 (50) | 2 (25) | 2 (33) | 17 (40) |
| Diarrhoea | 9 (41) | 1 (20) | 1 (50) | 2 (25) | 2 (33) | 15 (35) |
| Joint pain | 7 (32) | 1 (20) | 1 (50) | 3 (38) | 2 (33) | 14 (33) |
| Paralysis of limb(s) | 1 (5) | 0 (0) | 0 (0) | 0 (0) | 1 (17) | 2 (5) |
| Number died | 21 (95) | 4 (80) | 2 (100) | 5 (63) | 6 (100) | 38 (88) |
| Median number of days from onset to death (range) |
5 (1–47) | 5 (3–8) | 5 (4–6) | 5 (4–8) | 10.5 (5–34) | 5.5 (1–47) |
Fig. 2.
Distribution of date of onset of illness of Nipah encephalitis cases identified during the 2010–2011 Nipah season in Bangladesh.
Case and cluster investigations
Of the 22 cases in the Lalmonirhat cluster, 21 lived in five adjacent villages and the other case was a healthcare worker in a referral hospital where cases from this cluster were admitted for treatment.
The healthcare worker was a laboratory-confirmed case and worked as a janitor in the hospital. She was assigned to work in the female medicine ward. During 6–11 days prior to her illness onset, the period of her potential exposure to the virus [5], there were no cases of known NiV infection admitted to that ward. However, 12 cases of Nipah infection from Lalmonirhat were admitted to the male medicine and paediatric wards during that time. We interviewed her colleagues regarding her potential exposures in the hospital but were unable to confirm her exposure to any of these known cases. However, her co-workers reported that janitors commonly worked outside their assigned units, such as assisting in transferring newly admitted patients from the emergency department to different wards or cleaning waste from another ward. According to her family members, she did not have any history of consuming date palm sap or of coming in contact with an encephalitis patient outside her workplace.
Fourteen (64%) of the 22 cases in the Lalmonirhat cluster reportedly consumed raw date palm sap in the month before their illness onset. Proxies responding for seven cases in this cluster could not confirm whether these cases had a history of consuming raw or fermented date palm sap or of coming into contact with a Nipah case. However, 20 (91%) of the 22 cases or their proxies reported observing fruit bats near their homes at night.
Of the eight cases in the Rangpur cluster, proxies of three probable cases reported that the cases regularly drank fermented date palm sap, a traditional liquor known locally as tari, from a common source. They consumed the drink daily during the 30 days prior to their illness onset. These probable cases did not have any history of drinking raw sap or of having contact with a Nipah case. Three confirmed cases became ill following close contact with one of these probable cases. Two other cases from this cluster, one confirmed and one probable, had no reported history of consuming raw or fermented date palm sap or contact with a Nipah case.
Of the five cases in the Dinajpur cluster, two probable cases had drunk raw date palm sap prior to illness onset. Two cases, one confirmed and one probable, came in contact with these probable cases. Another confirmed case was the sister of one of the primary cases. She visited her brother’s home after his death; she cried and held her brother’s corpse and touched his face and chest. Thirteen days later, she developed fever, severe weakness and drowsiness. She had no history of consuming date palm sap or contact with a living Nipah patient. She did not take part in preparing the body for funeral, as only men are allowed to take part in that ritual if the deceased person is male.
Both cases in the Rajbari cluster had drunk raw date palm sap within 3 weeks prior to their illness onset, but the second case (daughter of the first case) also came in contact with her mother after her onset of illness, which was 4 days prior to her onset of illness.
The case reported by a private hospital in Dhaka, was a patient from Comilla District, in the eastern part of the country, who was admitted to that hospital with encephalitis. Her physicians suspected NiV as a possible cause of her illness since she had consumed raw date palm sap and sent her sera to IEDCR for testing. She was confirmed as a case of Nipah encephalitis. She drank raw date palm sap harvested from a tree in the courtyard of her house within 2 weeks prior to her illness onset, and other members from her family and neighbours also drank from the same pot during that time. However, no one else who had shared the sap with her reported any illness. Five of the six isolated cases reported a history of consuming raw date palm sap. None of the isolated cases had contact with any encephalitis cases prior to illness onset.
Of the 43 cases, the first clinical manifestation of infection for 41 (95%) cases was fever; headache was the first symptom in two others (Table 1). Thirty-eight (88%) cases eventually developed altered mental status and unconsciousness. Twenty-seven (63%) cases developed difficulty breathing, and 10 of these developed difficult breathing prior to development of altered mental status.
Thirty-eight (88%) of the 43 cases died; the median duration from onset to death was 6 (range 1–47) days. Twenty-two (95%) of the 23 cases who drank raw or fermented date palm sap died, compared to two (33%) of the six cases who only had a history of coming into close contact with a Nipah case (risk ratio 2.9, 95% CI 0.9–8.9, P < 0.01).
Case-control study
We enrolled 40 cases in the case-control study. One hundred and fifty-five of 160 selected age-matched controls were available for interview. Mean age (±standard deviation) of cases was 24 ± 17.5 years and of controls 25 ± 15.6 years (t = 0.24, P = 0.81). For 35 (88%) of the 40 cases and 34 (22%) of the 155 controls, we interviewed proxy respondents (P < 0.01). In the univariate conditional logistic regression analysis, Nipah cases had higher odds of drinking raw date palm sap within 30 days prior the onset of illness compared to the controls during the same period [55% vs. 12%, matched OR (mOR) 9.6, 95% CI 4.0–22.9] (Table 2). Cases also had higher odds of touching or being in the same room with a person with fever and altered mental status (23% vs. 3%, mOR 10.3, 95% CI 2.8–38.4). Male gender and bats visiting trees within or around the household were also significantly associated with contracting NiV infection (Table 2). By multivariable analysis, none of the variance inflation factors were larger than 1.68, suggesting no problems with multicollinearity. Cases had a higher odds of drinking raw date palm sap (adjusted mOR 17.9, 95% CI 4.0–80.5), touching or being in the same room with a person with fever and altered mental status (adjusted mOR 24.3, 95% CI 3.0–197.0), bats visiting trees near the household at night (adjusted mOR 40.1, 95% CI 3.9–416.7) and bats visiting trees near the household during the day (adjusted mOR 6.5, 95% CI 1.1–37.5). While there was no association between eating other fruits and being a case, cases had a lower odds of eating plums (adjusted mOR 0.2, 95% CI 0.1–0.7) in multivariate analysis.
Table 2.
Conditional univariate logistic regression analysis of exposures for Nipah encephalitis during December 2010-March 2011 Nipah season in Bangladesh
| Cases (N = 40) |
Controls (N = 155) |
|||||
|---|---|---|---|---|---|---|
| Risk factors | n | % | n | % | mOR (95% CI) | P value |
| Male | 29 | 73 | 81 | 52 | 2.6 (1.2–5.7) | 0.02 |
| Climbed a tree | 7 | 18 | 26 | 17 | 1.12 (0.4–3.2) | 0.83 |
| Drank raw date palm sap | 22 | 55 | 18 | 12 | 9.6 (4.0–22.9) | <0.01 |
| Sap harvester by profession | 3 | 8 | 0 | 0 | Undefined | 1.00 |
| Touched someone with fever and altered mental status or were in the same room with someone with those symptoms |
9 | 23 | 5 | 3 | 10.3 (2.8–38.4) | <0.01 |
| Contact with living animals | ||||||
| Cows | 16 | 40 | 80 | 51 | 0.6 (0.3–1.3) | 0.17 |
| Goats | 18 | 45 | 64 | 41 | 1.2 (0.6–2.7) | 0.61 |
| Sheep | 1 | 3 | 0 | 0 | Undefined | |
| Pigs | 1 | 3 | 0 | 0 | Undefined | |
| Dogs | 3 | 8 | 4 | 3 | 4.2 (0.7–26.1) | 0.13 |
| Cats | 3 | 8 | 7 | 5 | 1.8 (0.4–7.2) | 0.13 0.42 |
| Fruit bats | 0 | 0 | 0 | 0 | Undefined | |
| Contact with sick animal | ||||||
| Cow | 0 | 0 | 5 | 3 | Undefined | |
| Goat | 2 | 5 | 5 | 3 | 1.7 (0.3–9.4) | 0.56 |
| Pig | 0 | 0 | 0 | 0 | Undefined | |
| Ate meat of a sick animal | 6 | 15 | 16 | 10 | 1.6 (0.6–4.5) | 0.39 |
| Report of seeing bat during the day near home | 9 | 23 | 10 | 7 | 4.4 (1.6–11.9) | <0.01 |
| Report of seeing a bat at night near home | 36 | 90 | 71 | 46 | 45.7 (6.1–345.1) | <0.01 |
| Ate fruit | ||||||
| Plums | 21 | 53 | 102 | 66 | 0.5 (0.2–1.1) | 0.08 |
| Bananas | 23 | 58 | 93 | 60 | 0.9 (0.4–2.0) | 0.81 |
| Papayas | 18 | 45 | 53 | 34 | 1.6 (0.8–3.3) | 0.20 |
| Sapodillas | 1 | 3 | 5 | 3 | 0.6 (0.0–12.4) | 0.77 |
| Carambolas | 7 | 18 | 38 | 25 | 0.6 (0.2–1.6) | 0.32 |
| Guavas | 7 | 18 | 44 | 28 | 0.5 (0.2–1.3) | 0.16 |
| Ate fruit fallen onto ground | ||||||
| Plums | 14 | 35 | 48 | 31 | 1.3 (0.6–3.1) | 0.52 |
| Papayas | 3 | 8 | 4 | 3 | 3.0 (0.8–13.4) | 0.15 |
| Carambolas | 4 | 10 | 14 | 9 | 1.2 (0.3–4.1) | 0.82 |
| Guavas | 4 | 10 | 12 | 8 | 1.4 (0.4–5.3) | 0.62 |
mOR, Matched odds ratio; CI, confidence interval.
DISCUSSION
During the 2010–2011 Nipah season in Bangladesh, as in previous Nipah seasons, drinking raw date palm sap and having contact with a case of Nipah encephalitis were identified as the two most common risk factors for Nipah infection and 72% of cases reported one of these exposures during their incubation period. Additional evidence of healthcare and corpse-to-human transmission in Bangladesh was also found [12].
We also identified a new potential pathway of NiV transmission, drinking fermented date palm sap. In the absence of other known potential risk factors, drinking fermented date palm sap appeared to be the most plausible potential pathway of transmission for three probable cases in the Rangpur cluster. Drinking fermented date palm sap has not previously been recognized as a transmission source for NiV, therefore this was not included as a risk factor in the case-control study. Prior to the 2010–2011 Nipah season, there were no reported cases of NiV infection following drinking fermented date palm sap in Bangladesh, although this was also not explored as a potential risk factor for NiV infection. However, in a cluster of NiV infection reported from India during 2007, the index case developed NiV infection following drinking traditional liquor made from date palm sap [19]. Paramyxoviruses are considered susceptible to alcohol, but the alcohol concentration required to act as a disinfectant is 60–70%, while the alcohol concentration of traditional liquor in the Indian subcontinent has been reported to be around 4% [20]. This suggests that NiV may remain viable in fermented sap and be transmitted to humans who drink this sap. Possible transmission of NiV through drinking fermented date palm sap suggests the need to include this as a potential risk factor in future risk factor studies to statistically examine the association between drinking fermented date palm sap and NiV infection.
The janitor identified with Nipah encephalitis was the second healthcare worker in a Nipah surveillance hospital in Bangladesh to be confirmed with Nipah infection [12]. Although we could not identify the specific case to which she was exposed, admission of 12 cases of Nipah infection in that hospital during her period of exposure and absence of a history of consuming date palm sap, suggests that she was probably exposed to the cases in her workplace while performing her janitorial duties. Reports suggesting nosocomial transmission of Nipah encephalitis during two consecutive Nipah seasons further underscore the risk for healthcare workers. During the large Nipah outbreak in Malaysia and in subsequent studies there was limited evidence of nosocomial transmission of NiV [21, 22], but during an outbreak in India, in 2001, 45 of the 66 Nipah encephalitis cases had a history of hospital exposure [16]. In Bangladesh, there is an insufficient supply of personal protective equipment to permit healthcare workers to follow recommended practices. Hand-washing facilities are absent or inadequate in many hospitals and isolation wards frequently are either absent or non-functioning [23], all of which are crucial in preventing person-to-person or possible fomite-borne transmission of NiV. Sustained person-to-person transmission of an infectious disease requires that each case infects, on average, at least one new case; otherwise, the outbreak will eventually stop. Previous Nipah outbreaks in Bangladesh were self-limiting and the majority of cases did not transmit to anyone else; on average, cases infected fewer than one person each (R0 = 0.48) [24]. Emerging zoonotic infections that are transmitted from human to human, but are not sustained, such as NiV, are concerning for global public health because each new spillover of these pathogens into humans and subsequent transmission between people provides an opportunity for the virus to better adapt to humans and become more efficient in transmission from person-to-person [25]. Therefore, improving respiratory precautions in hospital settings is not only important to reduce the burden of healthcare-associated infections in Bangladesh, but also to limit opportunities for this pathogen to develop more efficient person-to-person transmissibility.
We identified a case of apparent corpse-to-human transmission. Frequent isolation of NiV from respiratory secretions of Nipah cases and evidence of corpse-to-human transmission in this outbreak investigation suggests that contact with secretions or body fluids of deceased Nipah cases is an important risk for transmission [12, 26]. The secondary case likely came in contact with the body fluids of the primary case when she cried while holding the body of the deceased. In Bangladeshi culture, the rituals following the death of a person often involve close contact with the corpse. The ritual purification of the body is accomplished by cleaning and washing the skin surface and body orifices without wearing any protective clothing [12], thereby creating opportunities for transmission of NiV. Public health action following the detection of Nipah cases or clusters should include communication messages targeting family members and those who will have close contact with the corpse of a Nipah case, discouraging touching the deceased’s face, especially respiratory secretions. Messages should emphasize covering the face while coming in close contact with the deceased and washing hands with soap after performing the ritual bath. However, such reactive strategies will still fail to prevent person-to-person transmission of infection from the primary cases since these cases often remain undiagnosed when in hospital unless they are part of a cluster or are detected later when secondary cases appear. Therefore, research should be undertaken to identify the system barriers in implementing interventions in the hospitals to reduce person-to-person or corpse-to-human transmission as a whole, such as respiratory precaution and hand washing and ways to overcome those barriers.
The isolated case from Comilla District is the first confirmed case of Nipah encephalitis from the eastern part of Bangladesh. While the reasons for the relative lack of occurrence of NiV infection in eastern districts are unknown, detection of this isolated Nipah encephalitis case, who had a history of drinking raw date palm sap, suggests that other undetected isolated NiV cases and clusters may occur outside of the previously described ‘Nipah belt’ [9]. However, considering routine reports and investigation of outbreaks of disease around the country, it is unlikely that a large number of cases remain undetected in that part of the country.
Those who developed the disease following drinking raw or fermented date palm sap had a higher casefatality proportion compared to those who developed the disease following exposure to a Nipah case. This is consistent with the findings from previous Nipah outbreaks in Bangladesh where cases who developed illness following person-to-person transmission had a lower case-fatality proportion compared to those who were infected through date palm sap consumption [6, 7, 11, 15, 27]. Similarly, in experimental studies golden hamsters exposed to a higher dose of NiV had higher case fatality [28]. Therefore, this variation in casefatality proportion could be related to the route of transmission or to the difference in dose of exposure to NiV.
Use of proxy respondents in a larger proportion of cases compared to the controls might result in a differential recall of exposures between the cases and controls. Although we interviewed multiple family members, friends or family caregivers as proxies, they may have had incomplete knowledge of exposures of the deceased cases. Therefore, a higher proportion of proxy respondents in cases compared to controls might have resulted in attenuation of the association between risk factors and the outcome. The apparent protective effect of eating plums, which is a common fruit during the winter, might be the result of such bias. This finding could also be due to chance, as there is no known plausible biological mechanism to support a protective effect. The independent association between bats visiting trees near households and being a Nipah case might indicate possible additional unknown pathways of NiV transmission from bats to humans.
We could not confirm 20 probable cases by laboratory tests, but the clinical manifestations in these previously healthy individuals were consistent with confirmed Nipah cases. Moreover, occurrence of these cases at the same time and place as the confirmed cases, similar exposure or frequent history of contact with the confirmed cases and the fatal outcome in all of them suggest that these cases probably had Nipah encephalitis.
Evidence regarding established risk factors such as drinking raw date palm sap and close contact with a Nipah case indicates the continued need for interventions to minimize the risks of such exposures to prevent human cases. While raising awareness to stop drinking raw date palm sap could be one approach to reduce zoonotic transmission of NiV, this recommendation may not be universally followed because drinking raw date palm sap is a long practised tradition in rural Bangladesh [29]. Therefore, preventing contamination of the date palm sap might be a more acceptable intervention. Protective bamboo skirts that prevent bats’ access to date palm sap might be effective in reducing transmission of NiV through drinking raw date palm sap [30]. On the other hand, prevention of person-to-person transmission of NiV infection would require a general improvement in infection prevention practices in patient care, such as implementation of respiratory and personal protective precautions and hand washing. Encephalitis is a common clinical condition caused by multiple pathogens, so development of a rapid diagnostic test to identify suspected Nipah cases early could be useful to identify patients at higher risk of transmitting the fatal infection and so permit increased attention by providers to reducing risk. Evidence generated during the Nipah season in 2010–2011 in Bangladesh highlights the importance of ongoing surveillance and thorough outbreak investigations, as we continue to learn about new transmission pathways and the epidemiological characteristics of Nipah in Bangladesh.
ACKNOWLEDGEMENTS
We thank the family members of study participants for their constant support and the volunteers from the outbreak village for their participation in the investigation. We acknowledge Diana DiazGranados for her helpful review of this manuscript.
The study was funded by CDC, Atlanta, GA, USA, cooperative agreement no. 5U01CI000628-01, the US National Institutes of Health (NIH), grant no. 07-015-0712-52200 (Bangladesh-NIH/Emerging Infectious Disease), and National Science Foundation/NIH Ecology and Evolution of Infectious Diseases grant no. 2R01-TW005869 from the Fogarty International Center. icddr,b also acknowledges with gratitude the commitment of CDC, NIH, and the Government of Bangladesh to its research efforts. icddr,b is also grateful to the Governments of Australia, Bangladesh, Canada, Sweden, and the United Kingdom for providing core/unrestricted support.
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Footnotes
DECLARATION OF INTEREST
None.
REFERENCES
- 1.Bellini WJ, et al. Nipah virus: an emergent paramyxo-virus causing severe encephalitis in humans. Journal of NeuroVirology. 2005;11:481–487. doi: 10.1080/13550280500187435. [DOI] [PubMed] [Google Scholar]
- 2.Goh KJ, et al. Clinical features of nipah virus encephalitis among pig farmers in Malaysia. New England Journal of Medicine. 2000;342:1229–1235. doi: 10.1056/NEJM200004273421701. [DOI] [PubMed] [Google Scholar]
- 3.Paton NI, et al. Outbreak of nipah-virus infection among abattoir workers in Singapore. Lancet. 1999;354:1253–1256. doi: 10.1016/S0140-6736(99)04379-2. [DOI] [PubMed] [Google Scholar]
- 4.Hsu VP, et al. Nipah virus encephalitis reemergence, Bangladesh. Emerging Infectious Diseases. 2004;10:2082–2087. doi: 10.3201/eid1012.040701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hossain MJ, et al. Clinical presentation of Nipah virus infection in Bangladesh. Clinical Infectious Diseases. 2008;46:977–984. doi: 10.1086/529147. [DOI] [PubMed] [Google Scholar]
- 6.Luby SP, et al. Foodborne transmission of Nipah virus, Bangladesh. Emerging Infectious Diseases. 2006;12:1888–1894. doi: 10.3201/eid1212.060732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gurley ES, et al. Person-to-person transmission of Nipah virus in a Bangladeshi community. Emerging Infectious Diseases. 2007;13:1031–1037. doi: 10.3201/eid1307.061128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Luby SP, Gurley ES, Hossain MJ. Transmission of human infection with Nipah virus. Clinical Infectious Diseases. 2009;49:1743–1748. doi: 10.1086/647951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stone R. Epidemiology. Breaking the chain in Bangladesh. Science. 2011;331:1128–1131. doi: 10.1126/science.331.6021.1128. [DOI] [PubMed] [Google Scholar]
- 10.Nahar N, et al. Date palm sap collection: Exploring opportunities to prevent Nipah transmission. EcoHealth. 2010;7:196–203. doi: 10.1007/s10393-010-0320-3. [DOI] [PubMed] [Google Scholar]
- 11.Rahman MA, et al. Date palm sap linked to Nipah virus outbreak in Bangladesh, 2008. Vector Borne and Zoonotic Diseases. 2012;12:65–72. doi: 10.1089/vbz.2011.0656. [DOI] [PubMed] [Google Scholar]
- 12.Sazzad HMS, et al. Nipah virus infection outbreak with nosocomial and corpse-to-human transmission, Bangladesh. Emerging Infectious Diseases. 2013;19:210–217. doi: 10.3201/eid1902.120971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Epstein JH, et al. Henipavirus infection in fruit bats (Pteropus giganteus), India. Emerging Infectious Diseases. 2008;14:1309–1311. doi: 10.3201/eid1408.071492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Khan MS, et al. Use of infrared camera to understand bats’ access to date palm sap: Implications for preventing Nipah virus transmission. EcoHealth. 2010;7:517–525. doi: 10.1007/s10393-010-0366-2. [DOI] [PubMed] [Google Scholar]
- 15.Homaira N, et al. Nipah virus outbreak with person-to-person transmission in a district of Bangladesh, 2007. Epidemiology and Infection. 2010;138:1630–1636. doi: 10.1017/S0950268810000695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chadha MS, et al. Nipah virus-associated encephalitis outbreak, Siliguri, India. Emerging Infectious Diseases. 2006;12:235–240. doi: 10.3201/eid1202.051247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Naser AM, et al. Integrated cluster- and case-based surveillance for detecting stage III zoonotic pathogens: an example of Nipah virus surveillance in Bangladesh. Epidemiology and Infection. 2015;143:1922–1930. doi: 10.1017/S0950268814002635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Daniels P, Ksiazek T, Eaton BT. Laboratory diagnosis of Nipah and Hendra virus infections. Microbes and Infection. 2001;3:289–295. doi: 10.1016/s1286-4579(01)01382-x. [DOI] [PubMed] [Google Scholar]
- 19.Arankalle VA, et al. Genomic characterization of Nipah virus, West Bengal, India. Emerging Infectious Diseases. 2011;17:907–909. doi: 10.3201/eid1705.100968. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chandrasekhar K, et al. A review on palm wine. International Journal of Research in Biological Sciences. 2012;2:33–38. [Google Scholar]
- 21.Mounts AW, et al. A cohort study of health care workers to assess nosocomial transmissibility of Nipah virus, Malaysia, 1999. Journal of Infectious Diseases. 2001;183:810–813. doi: 10.1086/318822. [DOI] [PubMed] [Google Scholar]
- 22.Gurley ES, et al. Risk of nosocomial transmission of Nipah virus in a Bangladesh hospital. Infection Control and Hospital Epidemiology. 2007;28:740–742. doi: 10.1086/516665. [DOI] [PubMed] [Google Scholar]
- 23.Rimi NA, et al. Infrastructure and contamination of the physical environment in three Bangladeshi hospitals: Putting infection control into context. PLoS ONE. 2014;9 doi: 10.1371/journal.pone.0089085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Luby SP, et al. Recurrent zoonotic transmission of Nipah virus into humans, Bangladesh, –. Emerging Infectious Diseases. 2009;15:1229–1235. doi: 10.3201/eid1508.081237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Antia R, et al. The role of evolution in the emergence of infectious diseases. Nature. 2003;426:658–661. doi: 10.1038/nature02104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lo MK, et al. Characterization of nipah virus from outbreaks in Bangladesh, 2008–2010. Emerging Infectious Diseases. 2012;18:248–255. doi: 10.3201/eid1802.111492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Homaira N, et al. Cluster of Nipah virus infection, Kushtia district, Bangladesh, 2007. PLoS ONE. 2010;5:e13570. doi: 10.1371/journal.pone.0013570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Rockx B, et al. Clinical outcome of henipavirus infection in hamsters is determined by the route and dose of infection. Journal of Virology. 2011;85:7658–7671. doi: 10.1128/JVI.00473-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Blatter EB. The Palms of British India and Ceylon. Periodical Experts Book Agency; 1978. [Google Scholar]
- 30.Nahar N, et al. Piloting the use of indigenous methods to prevent nipah virus infection by interrupting bats’ access to date palm sap in Bangladesh. Health Promotion International. 2013;28:378–386. doi: 10.1093/heapro/das020. [DOI] [PubMed] [Google Scholar]