Abstract
Little research investigates whether sleep mediates the adverse effect of perceived discrimination on health and even less is known about whether sleep quality and sleep duration mediate the relationships in the same fashion. We applied a recently developed mediation analysis approach to a survey administered in 2008 in Philadelphia, PA, that includes 9042 adults. Health was measured with self-rated health, stress, and mental illness. Perceived discrimination was operationalized with self-reported discriminatory experience in two social contexts, namely health care system and housing market. Sleep quality and duration were measured with a five-point Likert scale and the self-reported sleep time at night, respectively. After controlling for one’s demographic, socioeconomic, and health-related characteristics, the mediation analysis quantified how much sleep quality and duration can account for the effect of perceived discrimination on these health outcomes. The key findings are: (a) sleep quality and duration accounted for approximately 15 to 25 % of the adverse effect of perceived discrimination. (b) Sleep quality is more important than sleep duration in mediating the relationship between perceived discrimination and health. (c) The proportion of the effect mediated by sleep differs by the social context where perceived discrimination occurred. It was confirmed that sleep mediates the relationship between perceived discrimination and health and the interventions to improve sleep, particularly sleep quality, should help to attenuate the effect of perceived discrimination on health.
Keywords: Sleep quality, Sleep duration, Perceived discrimination, Mediation analysis
Introduction
Discrimination refers to the unfair treatment an individual receives or perceives due to his/her personal characteristics, such as race/ethnicity, age, gender, sexual orientation, nationality, socioeconomic, and health status.1,2 Discrimination may occur in different social contexts (e.g., housing markets and health care systems)3 and social structure levels (e.g., institutional and interpersonal discrimination).4 While, in contrast to five decades ago, acts of discrimination have been less visible and less common, discrimination remains a public concern and health researchers have found that an individual’s perceived discriminatory experience affects health outcomes.3–6 One major explanation for the effect of perceived discrimination on health is drawn from social stress theory 7 and treats the perceived discriminatory experience as a social stressor, which may trigger both psychosocial and physiological reactions and then lead to compromised health.8 More recently, a growing interest is focused on expanding the knowledge of “how” perceived discrimination gets under the skin by identifying the potential mechanisms from discrimination to health.9–11
It should be noted that perceived discrimination may not correctly reflect actual discrimination because individuals may misinterpret or misunderstand the discriminatory events. However, perceived discrimination itself carries important implications,3 and whether individuals report discriminatory experience depends on one’s socioeconomic status and demographics.12 That is, even when an actual discrimination event occurs, not all individuals may perceive discrimination. The subjective feeling of being discriminated against remains crucial and has been found to affect one’s health.1 Investigating the pathways linking perceived discrimination and health provides insights into intervention studies that aim to minimize the adverse impacts of perceived discrimination on health.
A recent study reviewed 17 articles published between 1971 and 2014 that directly investigated the associations between health and various characteristics of sleep, such as sleep quality and duration.13 The authors suggested that “further research is needed to evaluate sleep as a mechanism linking discrimination to poorer health” (p.5). Therefore, it becomes crucial to understand how much the effect of discrimination on health could be explained by the mechanism impacted by sleep. The existing literature on health and perceived discrimination does not provide a clear picture of how sleep mediates the relationship between perceived discrimination and health. Moreover, even less is known about whether the mediating mechanisms change along with the characteristics of sleep.
Why can sleep serve as a mediator between perceived discrimination and health? Following the social stress perspective, discriminatory experience is a stressor and without adequate coping responses, such as reasoning with the offender or emotional distractions, perceived discrimination may be translated into feelings of being threatened, vigilance, anxiety, anger, and hostility.14–16 These emotional reactions can further lead to biological changes (e.g., sympathetic nervous system hyperactivation) that undermine an individual’s sleep quality and/or duration.17 Should sleep deprivation or sleep interruption continue, a range of adverse health outcomes may be observed, including self-rated health 18,19, psychological distress,19 depression,20 obesity,21,22 hypertension,21,23 and cardiovascular disease,21,24 among others. It should be noted that most of the health literature has investigated the connection between perceived discrimination and sleep and the linkage between sleep disorder (e.g., short duration and poor quality) and health, respectively, but relatively little research has established a framework centering on the mediating role of sleep between perceived discrimination and health.13
With respect to why different characteristics of sleep may have different mediating effects between perceived discrimination and health, it has been documented that sleep duration and quality are influenced by different social, cultural, demographic, behavioral, and psychological factors.25 One recent study in Philadelphia26 suggested that sleep quality and sleep duration work differently by gender. Specifically, it was found that men’s body mass indices (BMIs) were solely associated with sleep duration, and women’s BMIs were dependent on sleep quality and unrelated to sleep duration.26 Another review article25 used the meta-analysis approach to understand the effects of sleep quantity and quality on type 2 diabetes and found that, in general, the effects of sleep quality (e.g., maintaining uninterrupted sleep) on the emergence of type 2 diabetes were stronger than those of sleep duration. Similarly, Moore et al. found that sleep quality was more relevant to self-rated health and psychological stress than sleep quantity, adjusting for other individual characteristics.19 These findings suggest that when assessing sleep as a mediator between perceived discrimination and health, it should be necessary to distinguish sleep quality from sleep duration given the potential difference in their effects on health outcomes.
This study not only aims to heed the call for investigating sleep as a mediator13 but also for understanding whether the mechanisms through sleep quality and duration operate in similar fashion between perceived discrimination and health. Specifically, drawing from the discussion above, we propose two hypotheses that will be empirically tested in this study: (a) sleep quality and duration both mediate the adverse effect of perceived discrimination on health even after controlling for other individual features, and (b) sleep quality plays a more important role in mediating the negative impact of perceived discrimination on health than does sleep quantity.
Data and Methods
Data Source and Measures
To test the research hypotheses, we used the 2008 Public Health Management Corporation’s (PHMC) Southeastern Pennsylvania Household Health Survey, which collected information about respondents’ health status, behaviors, and access to and utilization of health care services.27 The PHMC survey targets all adult residents living in the Philadelphia metropolitan area with the institutionalized population excluded. It is worth noting that sleep disorder was not used as a selection criterion when the survey was administered so that the data could reflect the target population. The 2008 PHMC dataset has been found to be reliable and valid because the key socioeconomic indicators (e.g., poverty rate) and public health measures (e.g., obesity rate) drawn from the dataset were comparable with those obtained from other data sources maintained by federal agencies, such as the American Community Survey and Behavioral Risk Factor Surveillance System.9,26,28 The discriminatory experience was last collected in 2008, which is the reason for using the 2008 PHMC data.
We measured the concept of health with three different variables, namely self-rated health, self-rated stress, and mental illness. Respondents were asked to assess their overall health using one of the following four categories: excellent, good, fair, and poor. Following the conventional practice,29 self-rated health is dichotomized with those reporting fair and poor health being coded 1, otherwise 0. Self-rated stress is treated as a continuous variable that ranges from 1 to 10, where “no stress” was coded 1 and “extreme amount of stress” was coded 10. The subjective stress measure has been found to well reflect daily stress level30 and to properly evaluate overall mental health status. The last dependent variable, mental illness, is a binary variable where the respondents who have been clinically diagnosed with depression or other mental health conditions were coded 1, otherwise 0. Using three different health measures will help us to more thoroughly explore whether the mediating mechanisms change in response to different dependent variables.
The 2008 PHMC survey asked respondents whether they have “ever experienced discrimination, [or] been prevented from doing something or been hassled or made to feel inferior” due to race/ethnicity or color in the context of two social institutions: health care system and housing market. Drawing from this variable, we created two dichotomous perceived discrimination variables: discrimination when getting medical care (medical care discrimination, 1 = yes, 0 = no) and discrimination when finding housing (housing discrimination; 1 = yes, 0 = no).
With respect to the characteristics of sleep, the participants were asked to rate their quality of sleep on a scale from 1 (restless) to 5 (restful) and their answers (i.e., sleep quality) were treated as a continuous measure in the mediation analysis. Sleep quantity refers to how many hours of sleep an individual gets at night and the PHMC survey explained to the respondents that the answer to this question may be different from the number of hours spent in bed to better assess sleep quantity.27 These two measures have been adopted in previous research that explored whether sleep quality and duration mediated the relationships between income and psychological health.19
In addition to health, perceived discrimination, and sleep variables, we also control for an individual’s demographic, socioeconomic, and health-related covariates. All the control variables described below have been found to be associated with sleep.31 In order to clarify the mechanisms between perceived discrimination and health, it is necessary to consider these variables. Specifically, the demographic variables include gender, race/ethnicity, marital status, and age. Gender was coded 1 for males and 0 for females. Race/ethnicity was categorized into five groups: non-Hispanic White, non-Hispanic Black, Hispanics, Asians, and non-Hispanic other races. Four dummy variables were included in the analysis with non-Hispanic White as the reference group. Marital status was dichotomized into “married or living with a partner” and “other statuses”, such as single, widowed, and separated. The former is coded 1 and the latter is coded 0. Each respondent’s age (in years) is treated as a continuous variable.
Socioeconomic variables include poverty, employment status, educational attainment, home ownership, income, and presence of children under 18 in a household. Using the 2008 federal poverty line, those who lived below the poverty line were coded 1 in poverty, otherwise 0. There are three different employment statuses: full-time employed, part-time employed, and other employment statuses (e.g., retired or self-employed). We used full-time employment as the reference group to generate two dummy variables in the analysis. Educational attainment has five categories (i.e., four dummy variables): less than high school (reference group), high school graduate, some college education, college graduate, and post-college degree. Home owners were coded as 1 whereas renters were coded as 0. Income is divided into 19 groups with 1 indicating less than $10,400 and 19 representing more than $250,000. Given the nature of this variable, the income coding scheme is treated as an ordinal variable. The total number of children under 18 in a household is also considered as parenthood is a potential confounder of sleep.
We further take three health-related variables into account. Health insurance is defined as whether a participant has any health insurance coverage, and those without any insurance were coded 1, otherwise 0. An individual’s BMI is included in this study as BMI is related to physical activities and diet patterns. The last variable is whether a participant smokes cigarettes “every day or at least some days per week.” Smokers (i.e., those who answered yes) were coded 1 and non-smokers were coded 0.
Mediation Analysis Method
This study employs the method developed by Karlson, Breen, and Holm32,33 (KHB method hereafter) to examine whether sleep quality and quantity mediate the relationship between perceived discrimination experiences and health. In the traditional mediation analysis, the total effect of a certain variable on the outcome of interest cannot be decomposed into direct and indirect effects when using logit and probit models because the error variance in a nonlinear probability model varies across models.32,34 The KHB method, however, addresses this issue and can be applied to nonlinear probability models.33 The KHB method estimates all (i.e., direct, indirect, and total) effects on the same scale and the coefficients in logit/probit models are not affected by rescaling, particularly when the total effect is decomposed into the direct and indirect effects. This merit allows researchers to compare the coefficients without any scale identification issue. It should be noted that a Monte Carlo study reported that the KHB method is not sensitive to large sample size as the likelihood of committing a type I error does not increase with the sample size or the number of tests.35 This finding suggests that it is not necessary to adjust for the p values of the estimates.
Also, the KHB method can take potential confounding variables into consideration and these variables are not affected by the scale of coefficients either. The KHB method is able to investigate multiple mediators simultaneously because the KHB decomposition approach has been shown to maintain almost all the features of decomposing a linear model.35 Thus, the single mediator in a model can be replaced with a vector of mediators without any added complication.32 The additivity feature of the decomposition approach then allows users to quantify the contributions of each mediator to the total effect. The ability to handle multiple mediators remains a rare functionality in mediation analysis. The technical details and proofs are available elsewhere,32,33,35 and we opt not to include them here. The mediation analysis was implemented in Stata 13.
Results
The descriptive statistics of the variables used in this study were shown in Table 1 where the statistics specific to each perceived discrimination type were also presented. We summarized the notable findings as follows. First, overall, roughly 20 % of the respondents reported fair/poor health and almost one in five participants have been diagnosed with mental health issues (e.g., depression and anxiety). The average stress level was 5.27 with a standard deviation of 2.65, indicating that approximately 70 % of the PHMC respondents had a stress level between three and eight. More importantly, poor health was more prevalent among those reporting discriminatory experience across three health measures than their counterparts without any experience.
TABLE 1.
Descriptive statistics of the variables used in this study
| Overall | Medical care discrimination | VIF | Housing market discrimination | VIF | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Mean | SD | N | Mean | SD | N | Mean | SD | |||
| Self-rated health (fair/poor = 1) | 9042 | 20.3 % | 554 | 36.6 % | NA | 431 | 34.6 % | NA | |||
| Stress (no stress = 1, extreme = 10) | 9042 | 5.27 | 2.65 | 554 | 6.42 | 2.86 | NA | 431 | 6.37 | 2.81 | NA |
| Mental illness (= 1) | 9042 | 18.8 % | 554 | 29.2 % | NA | 431 | 27.8 % | NA | |||
| Medical care discrimination (= 1) | 9042 | 6.1 % | 554 | – | 1.07 | 431 | 37.1 % | NA | |||
| Housing market discrimination (= 1) | 9042 | 4.8 % | 554 | 28.9 % | NA | 431 | – | 1.08 | |||
| SLEEP quality (restless = 1, restful = 5) | 9042 | 3.62 | 1.29 | 554 | 3.19 | 1.47 | 1.36 | 431 | 3.24 | 1.42 | 1.36 |
| SLEEP quantity | 9042 | 6.55 | 1.43 | 554 | 5.98 | 1.82 | 1.36 | 431 | 5.94 | 1.63 | 1.36 |
| Gender (male = 1) | 9042 | 33.2 % | 554 | 29.2 % | 1.04 | 431 | 31.1 % | 1.04 | |||
| Race | |||||||||||
| Whites (not Latino) | 6152 | 68.0 % | 167 | 30.1 % | NA | 90 | 20.9 % | NA | |||
| Blacks (not Latino) | 2139 | 23.7 % | 286 | 51.6 % | 1.28 | 256 | 59.4 % | 1.29 | |||
| Latino | 438 | 4.8 % | 62 | 11.2 % | 1.13 | 52 | 12.1 % | 1.14 | |||
| Asian | 127 | 1.4 % | 6 | 1.1 % | 1.03 | 3 | 0.7 % | 1.03 | |||
| Others | 186 | 2.1 % | 33 | 6.0 % | 1.03 | 30 | 7.0 % | 1.03 | |||
| Age | 9042 | 52.02 | 15.60 | 554 | 47.09 | 14.17 | 1.81 | 431 | 46.64 | 13.31 | 1.80 |
| Poverty (= 1) | 9042 | 8.0 % | 554 | 18.4 % | 1.71 | 431 | 20.0 % | 1.71 | |||
| Main employment | |||||||||||
| Employed full-time | 5639 | 62.4 % | 295 | 53.2 % | NA | 242 | 56.1 % | NA | |||
| Employed part-time | 604 | 6.7 % | 51 | 9.2 % | 1.15 | 39 | 9.0 % | 1.15 | |||
| Unemployed/retired/disabled/homemaker/student | 2799 | 31.0 % | 208 | 37.5 % | 1.85 | 150 | 34.8 % | 1.85 | |||
| Completed education | |||||||||||
| <High school graduate | 617 | 6.8 % | 54 | 9.7 % | NA | 31 | 7.2 % | NA | |||
| High school graduate | 2882 | 31.9 % | 193 | 34.8 % | 4.30 | 145 | 33.6 % | 4.30 | |||
| Some college | 1828 | 20.2 % | 145 | 26.2 % | 3.75 | 110 | 25.5 % | 3.75 | |||
| College graduate | 2242 | 24.8 % | 109 | 19.7 % | 4.58 | 92 | 21.3 % | 4.58 | |||
| Post-college | 1473 | 16.3 % | 53 | 9.6 % | 3.78 | 53 | 12.3 % | 3.78 | |||
| Home ownership (= 1) | 9042 | 75.1 % | 554 | 56.3 % | 1.33 | 431 | 53.4 % | 1.33 | |||
| Income (1–19) | 7405 | 12.32 | 5.56 | 462 | 9.36 | 5.85 | 3.08 | 370 | 9.72 | 5.95 | 3.07 |
| Married/cohabitation (= 1) | 9042 | 55.8 % | 554 | 41.3 % | 1.41 | 431 | 42.9 % | 1.41 | |||
| Number of kids | 9042 | 0.62 | 1.10 | 554 | 0.73 | 1.26 | 1.25 | 431 | 0.80 | 1.32 | 1.25 |
| Health insurance (N = 1) | 9042 | 6.0 % | 554 | 15.5 % | 1.10 | 431 | 13.7 % | 1.10 | |||
| Body mass index | 9042 | 27.46 | 6.05 | 554 | 28.62 | 6.75 | 1.07 | 431 | 29.04 | 6.70 | 1.07 |
| Smoking (= 1) | 9042 | 20.0 % | 554 | 33.0 % | 1.11 | 431 | 29.0 % | 1.11 | |||
VIF variation inflation factor
Second, the prevalence of discriminatory experience was higher in the health care system (6.1 %) than in the housing market (4.8 %) and almost one in ten participants had experienced racial discrimination either when getting medical care or when obtaining housing. Over half of individuals who experienced discriminatory behaviors identified as non-Hispanic Black. Somewhat surprisingly, 30 % of individuals reporting discrimination when getting medical care were non-Hispanic White, and slightly over 20 % were non-Hispanic White among those who experienced discrimination in the housing market.
Third, the average sleep quality is 3.62 on a five-unit scale and our respondents reported 6.55 h of sleep at night. The standard deviations for these two variables are 1.29 and 1.43, respectively, and these numbers are highly comparable with those reported in the literature.19 For the overall samples, the distribution of sleep quality is slightly skewed to the right and the range of sleep hours is approximately between 3.5 and 9.5 h. In contrast to the overall samples, respondents with discrimination experience reported lower sleep quality (3.19 and 3.24, respectively) and shorter sleep duration (both less than 6 h). The standard deviations were also larger among respondents with discriminatory experience. These findings provided auxiliary evidence that perceived discrimination exerts an adverse impact on health outcomes and sleep has the potential to mediate this relationship.
It should be noted that we also conducted analyses, such as the chi-square test, to compare whether discriminatory experience varies by the key covariates and we found that perceived discrimination varied significantly (p < 0.001) by race/ethnicity and gender (p < 0.05). We reported the variation inflation factors (VIF) in Table 1. As a rule of thumb, a VIF greater than 10 indicates that multicollinearity exists among the independent variables. Given the fact that our largest VIF is smaller than 5, we concluded that multicollinearity should not be a concern.
Table 2 presents the mediation analysis results by the types of perceived discrimination and health outcomes (after controlling for demographic, socioeconomic, and health-related covariates). Two major findings are worth noting. First and foremost, including the characteristics of sleep into the analysis significantly reduced the effects of perceived discrimination, a pattern that was observed across different types of perceived discrimination and health outcomes. Using self-rated health as an example, the magnitude of the total effect of perceived discrimination when getting medical care was 0.46 (odds ratio [OR] = 1.59) when the characteristics of sleep were not included in the analysis. However, the magnitude decreased to 0.36 (i.e., direct effect; OR = 1.43) when sleep quality and sleep duration were considered. The difference in the magnitude of the effect (0.11) represents the mediating impact through the characteristics of sleep and was statistically significant. That being said, over 20 % (0.106/0.464 = 0.228) of the total effect of perceived discrimination on self-rated health went through the sleep-related mechanisms. Similar findings were obtained for those who experienced discrimination in housing markets.
TABLE 2.
The KHB mediation analysis and decomposition results by discrimination types and health outcomesa
| Self-rated health | Medical care discrimination | Housing market discrimination | ||||
|---|---|---|---|---|---|---|
| Estimates | Robust SE | Mediation percentage | Estimates | Robust SE | Mediation percentage | |
| Total effect | 0.464*** | 0.119 | NA | 0.433** | 0.132 | NA |
| Direct effect | 0.358** | 0.119 | NA | 0.324* | 0.132 | NA |
| Mediating effect | 0.106*** | 0.021 | 22.84 | 0.109*** | 0.024 | 25.17 |
| Through | ||||||
| Sleep quality | 0.090*** | 0.020 | 84.11 | 0.090*** | 0.022 | 82.40 |
| Sleep duration | 0.017 | 0.010 | 15.89 | 0.019 | 0.011 | 17.60 |
| Self-rated stress | Estimates | Robust SE | Mediation percentage | Estimates | Robust SE | Mediation percentage |
| Total effect | 1.052*** | 0.119 | NA | 0.903*** | 0.132 | NA |
| Direct effect | 0.886*** | 0.119 | NA | 0.728*** | 0.133 | NA |
| Mediating effect | 0.167*** | 0.030 | 15.87 | 0.174*** | 0.033 | 19.27 |
| Through | ||||||
| Sleep quality | 0.116*** | 0.024 | 69.27 | 0.117*** | 0.027 | 66.89 |
| Sleep duration | 0.051*** | 0.013 | 30.73 | 0.058*** | 0.014 | 33.11 |
| Mental illness | Estimates | Robust SE | Mediation percentage | Estimates | Robust SE | Mediation percentage |
| Total effect | 0.500*** | 0.121 | NA | 0.424** | 0.140 | NA |
| Direct effect | 0.422** | 0.122 | NA | 0.345* | 0.140 | NA |
| Mediating effect | 0.079*** | 0.018 | 15.80 | 0.080*** | 0.020 | 18.87 |
| Through | ||||||
| Sleep quality | 0.084*** | 0.019 | 106.73 | 0.085*** | 0.021 | 106.77 |
| Sleep duration | −0.005 | 0.009 | −6.73 | −0.005 | 0.010 | −6.77 |
aAll the control variables are included in the analysis and only the mediation results were reported
*p < 0.05; **p < 0.01; ***p < 0.001
In contrast to self-rated health, the percentages of the total effects on self-rated stress and mental illness that were mediated by the characteristics of sleep were relatively smaller, ranging from 15 to 20 %. In addition, sleep quality and duration play a larger role in mediating the adverse effect of housing market discrimination on health than that of medical care discrimination because of the consistently larger mediation percentages in the former (e.g., 19.27 vs. 15.87 in self-rated stress).
Second, when assessing whether sleep quality and duration differently mediate the relationship between perceived discrimination and health, the results suggest that sleep quality is more important than sleep duration in mediating the adverse effect of perceived discrimination on health. For example, we found that more than 65 % of the mediating effect between perceived housing discrimination and self-rated stress came from the sleep quality mechanism and 35 % was attributable to the sleep duration mechanism. The findings were comparable to the relationship between medical care discrimination and self-rated stress (69.3 % via sleep quality and 30.7 % via sleep duration).
The importance of sleep quality is more profound in self-rated health and mental illness than it is in self-rated stress. Specifically, the decomposition results indicated that the mediating effects on self-rated health and self-rated stress via sleep duration were not statistically significant, suggesting that sleep quality should fully account for the mediating effect of perceived discrimination on self-rated health and mental illness, regardless of the social contexts where perceived discrimination occurred.
Discussion
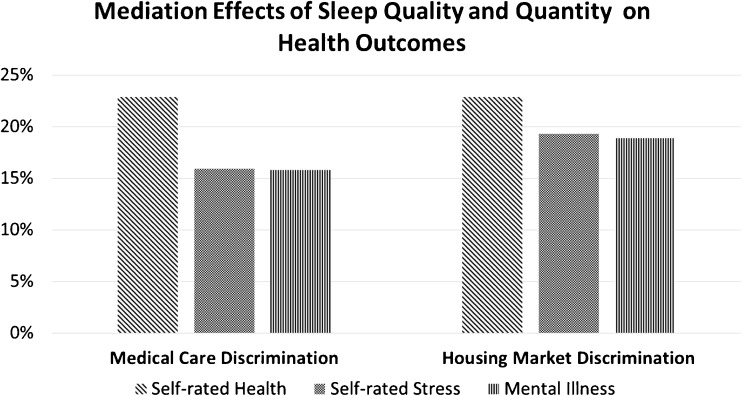
Our findings above directly speak to the recent call for exploring whether sleep mediates the detrimental effect of perceived discrimination on health13 and can be used to examine the research hypotheses. We first hypothesized that sleep quality and duration both mediate the adverse effect of perceived discrimination on health and this mediation holds true even after considering other individual characteristics. We found evidence to bolster this hypothesis as sleep quality and duration were found to jointly mediate 15 to 25% of the total effect of perceived discrimination on health. Moreover, following the recent literature,19,25,26 the second hypothesis stated that sleep quality plays a more important role than sleep duration and this hypothesis is substantiated by the analysis. Specifically, more than two thirds of the total mediation effect can be attributed to sleep quality and this pattern is consistent across models with different health outcomes. We summarized the percentages mediated by sleep quality and duration into Fig. 1 to illustrate the key findings.
FIG. 1.
Percentages of the total effects of perceived discrimination on health by social contexts.
By situating the discriminatory experience in the context of the health care system and housing market and using three health measures, we not only found evidence to support that sleep mediates the negative effect of perceived discrimination on health but also confirmed that the mediating role of sleep remains the same across different health measures and social contexts where individuals experienced discriminatory behaviors. Furthermore, the decomposition results suggested that sleep quality and sleep duration mediate the effects of perceived discrimination on health differently. The former plays a more important mediating role than the latter given that at least 80 % of the mediating effects on health were via sleep quality. This finding is similar to that reported by Moore et al. as they found that sleep quality is a more powerful predictor for mental and physical health,19 even after controlling for individual demographics and prior health status.
As suggested by the social stress perspective, regardless of where perceived discrimination occurs, it can be regarded as a stressor14,15,36 and lead to negative mood or emotional reactions,37 which may trigger biological reactions, such as increased blood pressure38 and nervous system hyperactivation.17 These reactions may hinder one’s sleep quality and duration17 and ultimately health.9 Little is known about how important the mediating role of sleep is between perceived discrimination and health. Our findings indicate that approximately 20 % of the total effect of perceived discrimination on health can be mediated through sleep, particularly better sleep quality. Several actions can be taken to improve sleep quality, such as music-assisted relaxation39 exercise,40 or diet pattern changes.41 These activities are part of the emotion-focused coping techniques and can distract individuals with perceived discrimination.7,30 In contrast to that of sleep quality, the mediating role of sleep duration is less clear. More specifically, sleep duration was only found to mediate the relationship between perceived discrimination and self-rated stress. One plausible explanation is that sleep duration changes over life course and the relationship between sleep duration and health may not be linear.42 To test that our findings are valid and reliable, we dichotomized sleep duration by coding those reporting 7 or 8 h as 1, otherwise 0, and then conducted the same mediation analyses. We found similar patterns in that sleep quality still accounts for over 75% of the mediation effect (results available upon request). The additional analyses (not shown) also suggested that without sleep quality, sleep duration could mediate roughly 7–15% of the total effect, however, when sleep quality was included, sleep duration became less important. This echoes our conclusion that sleep quality is more important than sleep duration in mediating the adverse effect of perceived discrimination on health. All these sensitivity analyses indicated that our findings reported in the result section do not change by how we measure sleep duration.
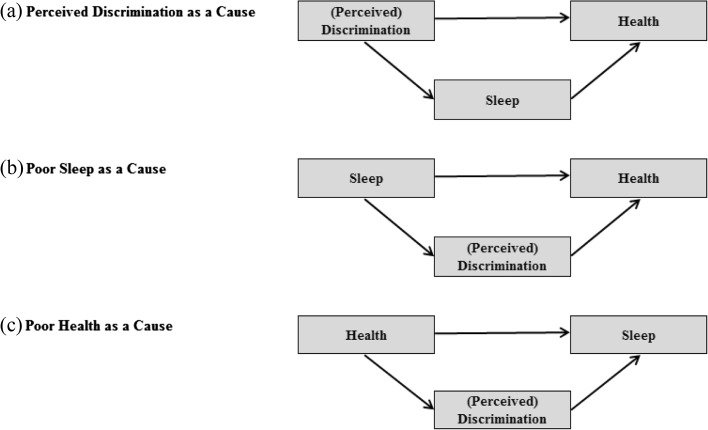
The analytic framework of this study assumes that perceived discrimination is the root cause of poor sleep quality/duration and health (Fig. 2a). It is also possible that perceived discrimination serves as the mediator between sleep and health (Fig. 2b, c). We examined the two frameworks with the same data and methods and found that the mechanisms in Fig. 2b, c can only account for 2~7 % of the total effects (detailed results are not shown but available upon request). In other words, while it is statistically possible that perceived discrimination can serve as the mediator, this argument carries little substantive implication in contrast to our framework where sleep quality and duration mediate approximately 20 % of the adverse impact of perceived discrimination on health. More importantly, this study is driven by the social stress theory7 and the recommendation of a recent review article.13 To justify Fig. 2b, c, it may be necessary to consider a different set of literature or theoretical arguments and this is beyond the scope of this study.
FIG. 2.
Alternative analytic frameworks.
This study has several limitations. First, while it has been argued that the mediation analysis approach of this study can be used to draw causal relationships,43 the cross-sectional nature of our data makes it impossible to determine the causal relationships among perceived discrimination, sleep, and health. While we examined two other alternative models to show that the analytic framework of this study may be better (see the previous paragraph), longitudinal data are still needed to clarify the causal relationships. Second, the characteristics of sleep and discrimination are both subjective. Though subjective measures may be more appropriate for stress-related research,30 future efforts are warranted to adopt objective sleep and/or discrimination measures. Third, it should be cautioned against generalizing our findings to other areas or populations as the PHMC data only reflect the population in the Philadelphia metropolitan area.
Conclusions
This study contributes to the literature by (a) confirming the role of sleep between perceived discrimination and three health outcomes, namely self-rated health, self-rated stress, and mental illness; (b) suggesting that sleep quality outweighs sleep duration in terms of mediating the pernicious effect of perceived discrimination on health; and (c) quantifying the sleep-related mechanisms that were found to account for roughly 20 % of the total effect of perceived discrimination on health. To our knowledge, our research framework is among the first to center on sleep in extensively examining whether sleep mediates the relationship between perceived discrimination (in different contexts) and health.
Acknowledgments
We acknowledge the assistance from the Center for Social and Demographic Analysis at the University at Albany, State University of New York, which receives core funding from NICHD [R24-HD044943].
Contributor Information
Tse-Chuan Yang, Email: tyang3@albany.edu.
Kiwoong Park, Email: kpark5@albany.edu.
References
- 1.Pascoe EA, Smart RL. Perceived discrimination and health: a meta-analytic review. Psychol Bull. 2009;135(4):531. doi: 10.1037/a0016059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Larson LK. Employee Health--AIDS Discrimination. Employment Discrimination. Vol 10. Matthew Bender; 2014.
- 3.Pager D, Shepherd H. The sociology of discrimination: racial discrimination in employment, housing, credit, and consumer markets. Annu Rev Sociol. 2008;34:181. doi: 10.1146/annurev.soc.33.040406.131740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Gee GC. A multilevel analysis of the relationship between institutional and individual racial discrimination and health status. Am J Public Health. 2002;92(4):615–623. doi: 10.2105/AJPH.92.4.615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Finch BK, Kolody B, Vega WA. Perceived discrimination and depression among Mexican-origin adults in California. J Health Soc Behav. 2000;41(3):295–313. doi: 10.2307/2676322. [DOI] [PubMed] [Google Scholar]
- 6.Williams DR, Mohammed SA. Discrimination and racial disparities in health: evidence and needed research. J Behav Med. 2009;32(1):20–47. doi: 10.1007/s10865-008-9185-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aneshensel CS. Social stress: theory and research. Annu Rev Sociol. 1992;18:15–38. doi: 10.1146/annurev.so.18.080192.000311. [DOI] [Google Scholar]
- 8.Selye H. Stress in Health and Diseases. Boston, MA: Butterworth; 1976.
- 9.Chen D, Yang T-C. The pathways from perceived discrimination to self-rated health: an investigation of the roles of distrust, social capital, and health behaviors. Soc Sci Med. 2014;104:64–73. doi: 10.1016/j.socscimed.2013.12.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Steffen PR, Bowden M. Sleep disturbance mediates the relationship between perceived racism and depressive symptoms. Ethn Dis. 2006;5(6):8–11. [PubMed] [Google Scholar]
- 11.Williams DR, Neighbors HW, Jackson JS. Racial/ethnic discrimination and health: findings from community studies. Am J Public Health. 2003;93(2):200–208. doi: 10.2105/AJPH.93.2.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Borrell LN, Kiefe CI, Williams DR, Diez-Roux AV, Gordon-Larsen P. Self-reported health, perceived racial discrimination, and skin color in African Americans in the CARDIA study. Soc Sci Med. 2006;63(6):1415–1427. doi: 10.1016/j.socscimed.2006.04.008. [DOI] [PubMed] [Google Scholar]
- 13.Slopen N, Lewis TT, Williams DR. Discrimination and sleep: a systematic review. Sleep Medicine. 2015 doi: 10.1016/j.sleep.2015.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Brondolo E, Gallo LC, Myers HF. Race, racism and health: disparities, mechanisms, and interventions. J Behav Med. 2009;32(1):1–8. doi: 10.1007/s10865-008-9190-3. [DOI] [PubMed] [Google Scholar]
- 15.Brondolo E, Hausmann LR, Jhalani J, et al. Dimensions of perceived racism and self-reported health: examination of racial/ethnic differences and potential mediators. Ann Behav Med. 2011;42(1):14–28. doi: 10.1007/s12160-011-9265-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Noh S, Kaspar V. Perceived discrimination and depression: moderating effects of coping, acculturation, and ethnic support. Am J Public Health. 2003;93(2):232–238. doi: 10.2105/AJPH.93.2.232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Buckley TM, Schatzberg AF. On the interactions of the hypothalamic-pituitary-adrenal (HPA) axis and sleep: normal HPA axis activity and circadian rhythm, exemplary sleep disorders. J Clin Endocrinol Metabol. 2005;90(5):3106–3114. doi: 10.1210/jc.2004-1056. [DOI] [PubMed] [Google Scholar]
- 18.Magee CA, Caputi P, Iverson DC. Relationships between self-rated health, quality of life and sleep duration in middle aged and elderly Australians. Sleep Med. 2011;12(4):346–350. doi: 10.1016/j.sleep.2010.09.013. [DOI] [PubMed] [Google Scholar]
- 19.Moore PJ, Adler NE, Williams DR, Jackson JS. Socioeconomic status and health: the role of sleep. Psychosom Med. 2002;64(2):337–344. doi: 10.1097/00006842-200203000-00018. [DOI] [PubMed] [Google Scholar]
- 20.Tsuno N, Besset A, Ritchie K. Sleep and depression. J Clin Psychiatry. 2005;66(10):1254–1269. doi: 10.4088/JCP.v66n1008. [DOI] [PubMed] [Google Scholar]
- 21.Buxton OM, Marcelli E. Short and long sleep are positively associated with obesity, diabetes, hypertension, and cardiovascular disease among adults in the United States. Soc Sci Med. 2010;71(5):1027–1036. doi: 10.1016/j.socscimed.2010.05.041. [DOI] [PubMed] [Google Scholar]
- 22.Cappuccio FP, Taggart FM, Kandala N-B, Currie A. Meta-analysis of short sleep duration and obesity in children and adults. Sleep. 2008;31(5):619. doi: 10.1093/sleep/31.5.619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gangwisch JE, Heymsfield SB, Boden-Albala B, et al. Short sleep duration as a risk factor for hypertension analyses of the first national health and nutrition examination survey. Hypertension. 2006;47(5):833–839. doi: 10.1161/01.HYP.0000217362.34748.e0. [DOI] [PubMed] [Google Scholar]
- 24.Ayas NT, White DP, Manson JE, et al. A prospective study of sleep duration and coronary heart disease in women. Arch Intern Med. 2003;163(2):205–209. doi: 10.1001/archinte.163.2.205. [DOI] [PubMed] [Google Scholar]
- 25.Cappuccio FP, D'Elia L, Strazzullo P, Miller MA. Quantity and quality of sleep and incidence of type 2 diabetes: a systematic review and meta-analysis. Diabetes Care. 2010;33(2):414–420. doi: 10.2337/dc09-1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yang T-C, Matthews SA, Chen VY-J. Stochastic variability in stress, sleep duration, and sleep quality across the distribution of body mass index: insights from quantile regression. Int J Behav Med. 2014;21(2):282–291. doi: 10.1007/s12529-013-9293-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Public Health Management Corporation (PHMC). Household Health Survey Documentation. Philadelphia, PA; 2008.
- 28.Yang T-C, Matthews SA, Hillemeier MM. Effect of health care system distrust on breast and cervical cancer screening in Philadelphia, Pennsylvania. Am J Public Health. 2011;101(7):1297–1305. doi: 10.2105/AJPH.2010.300061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Idler EL, Benyamini Y. Self-rated health and mortality: a review of twenty-seven community studies. J Health Soc Behav. 1997;38(1):21–37. doi: 10.2307/2955359. [DOI] [PubMed] [Google Scholar]
- 30.Lazarus RS. Theory-based stress measurement. Psychol Inq. 1990;1(1):3–13. doi: 10.1207/s15327965pli0101_1. [DOI] [Google Scholar]
- 31.Krueger PM, Friedman EM. Sleep duration in the United States: a cross-sectional population-based study. Am J Epidemiol. 2009;169(9):1052–1063. doi: 10.1093/aje/kwp023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Breen R, Karlson KB, Holm A. Total, direct, and indirect effects in logit and probit models. Sociol Methods Res. 2013;42(2):164–191. doi: 10.1177/0049124113494572. [DOI] [Google Scholar]
- 33.Karlson KB, Holm A. Decomposing primary and secondary effects: a new decomposition method. Res Soc Stratification Mobil. 2011;29(2):221–237. doi: 10.1016/j.rssm.2010.12.005. [DOI] [Google Scholar]
- 34.MacKinnon DP, Dwyer JH. Estimating mediated effects in prevention studies. Eval Rev. 1993;17(2):144–158. doi: 10.1177/0193841X9301700202. [DOI] [Google Scholar]
- 35.Karlson KB, Holm A, Breen R. Comparing regression coefficients between same-sample nested models using logit and probit a new method. Sociol Methodol. 2012;42(1):286–313. doi: 10.1177/0081175012444861. [DOI] [Google Scholar]
- 36.Brondolo E, Rieppi R, Kelly KP, Gerin W. Perceived racism and blood pressure: a review of the literature and conceptual and methodological critique. Ann Behav Med. 2003;25(1):55–65. doi: 10.1207/S15324796ABM2501_08. [DOI] [PubMed] [Google Scholar]
- 37.Broudy R, Brondolo E, Coakley V, et al. Perceived ethnic discrimination in relation to daily moods and negative social interactions. J Behav Med. 2007;30(1):31–43. doi: 10.1007/s10865-006-9081-4. [DOI] [PubMed] [Google Scholar]
- 38.Krieger N, Sidney S. Racial discrimination and blood pressure: the CARDIA study of young black and white adults. Am J Public Health. 1996;86(10):1370–1378. doi: 10.2105/AJPH.86.10.1370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.De Niet G, Tiemens B, Lendemeijer B, Hutschemaekers G. Music‐assisted relaxation to improve sleep quality: meta‐analysis. J Adv Nurs. 2009;65(7):1356–1364. doi: 10.1111/j.1365-2648.2009.04982.x. [DOI] [PubMed] [Google Scholar]
- 40.King AC, Oman RF, Brassington GS, Bliwise DL, Haskell WL. Moderate-intensity exercise and self-rated quality of sleep in older adults: a randomized controlled trial. J Am Med Assoc (JAMA) 1997;277(1):32–37. doi: 10.1001/jama.1997.03540250040029. [DOI] [PubMed] [Google Scholar]
- 41.Peuhkuri K, Sihvola N, Korpela R. Diet promotes sleep duration and quality. Nutr Res. 2012;32(5):309–319. doi: 10.1016/j.nutres.2012.03.009. [DOI] [PubMed] [Google Scholar]
- 42.Ferrie JE, Shipley MJ, Cappuccio FP, et al. A prospective study of change in sleep duration: associations with mortality in the Whitehall II cohort. Sleep. 2007;30(12):1659. doi: 10.1093/sleep/30.12.1659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hayes AF. Introduction to mediation, moderation, and conditional process analysis: a regression-based approach. New York, NY: Guilford Press; 2013.