Abstract
Effectiveness of a nurse educator in the pediatric oncology unit in Guatemala was assessed by measuring completion of an education course, chemotherapy and central line competency, continuing education, and cost. All newly hired nurses completed the education course. Of the nurses employed, 86% participated in the chemotherapy course, and 93% achieved competency; 57% participated in the central line course, and 79% achieved competency. The nurses completed a mean of 26 hours continuing education yearly. The annual direct cost of the educator ($244/nurse) was markedly less than other models. This is an effective sustainable means to educate nurses in low-income countries.
Keywords: Pediatric Oncology, Outcomes Research, Chemotherapy
Introduction
There is great disparity between the outcomes of children with cancer in high-income versus low-income countries, with a 5-year survival rate of 75% to 79% in the United States and Western Europe [1], but often less than 20% in low-income countries where most cases of childhood cancer occur [2]. As public health improves in low-income countries and common childhood diseases become less important contributors to mortality, childhood cancer becomes a more prominent cause of disease-related mortality [3]. A cornerstone of successful treatment of childhood cancer is the provision of specialized professional care in pediatric cancer units [4, 5]. Nurses, who comprise the largest group of health care professionals globally, are essential to successful treatment. Pediatric oncology nursing care requires advanced knowledge and clinical skills. Pediatric oncology nurses play a major role in managing disease-related complications, coordinating care for central-venous lines, administering chemotherapy, and educating patients and families [6]. Most hospitals in high-income countries provide extensive education and clinical training to newly hired pediatric oncology nurses and offer education classes on a continuing basis. In contrast, pediatric oncology education is generally unavailable for nurses in low-income countries. This lack of education likely contributes to the continued disparity in survival rates, as under-educated nurses are unable to meet the demands of pediatric cancer care [2, 7, 8]. The impact of nursing education on patient outcomes has been extensively researched. Several recent large-scale studies in high-income and low-income countries have suggested that nursing education contributes to improved patient outcomes, including reduced mortality [9–12].
Twinning, whereby a center in a high-income country partners with a center in a low-income country, can improve childhood cancer care significantly [2, 13]. Educating physicians and nurses is a priority of twinning programs aimed at developing sustainable pediatric cancer care and requires a long term commitment by the sponsoring center [14, 15]. Physician education is provided to partner sites through short-term fellowships, medical conferences, and online meetings to discuss patient care. Nursing education is a greater challenge. Travel to the sponsoring center for education is rarely feasible for several reasons: large numbers of nurses are required to support a center, work and family demands interfere, and language barriers often exist. Furthermore, nurses have little time during their work hours to attend online meetings, and many have limited computer access at home.
When the International Outreach Program (IOP) at St. Jude Children’s Research Hospital (St. Jude) began in 1993, the lack of nurses with pediatric oncology skills was a major impediment to the implementation of evidence-based oncology care at partner sites. Before 1998, nurses were educated through a series of lectures given by St. Jude nurses at partner sites. From 1998 to 2002, the IOP supported a residential training program in El Salvador for staff nurses from Latin America [8]. While both approaches met an important need, there were limitations: education was not universally available to nurses, continuing education remained unavailable, and the cost was unsustainable. In addition, both approaches employed St. Jude nurses as educators who were not fluent in Spanish or familiar with the culture.
In 2007, the IOP implemented a new nursing education model. Full-time nurse educator positions were established within partner-site pediatric oncology units, and experienced nurses were hired from inside the units. The nurse educator’s primary responsibilities included: providing pediatric oncology education for newly hired nurses, teaching courses in chemotherapy administration and central-venous line care, and providing continuing education classes and on-site mentoring. Training and ongoing support to the educators was provided by the St. Jude supported Latin American Center for Pediatric Oncology Nursing Education in Santiago, Chile and included: a 4-week comprehensive educator course, nursing education resources, and ongoing education via bimonthly online meetings [16].
A nurse dedicated exclusively to staff education for a specific unit within a hospital was a new concept at large public hospitals in low-income countries, which typically have only one nurse educator to serve the entire hospital. Since this concept had not been tested in low-income countries and a proven model for pediatric oncology nursing education was needed, we evaluated its effectiveness and cost at the National Pediatric Oncology Unit in Guatemala, where the nurse educator position was first established in January 2007. This study measured immediate and short term outcomes and constitutes the initial step in the process of comprehensive program evaluation [17].
Methods
From January 2007 through September 2009, five outcome measures were assessed: 1) the rate of completion of a pediatric oncology nursing education course by newly hired nurses, 2) the rate of chemotherapy competency, 3) the rate of central-venous line care competency, 4) the hours of continuing education completed, and 5) the cost in comparison to three other education models used in low-income countries.
The pediatric oncology education course for newly hired nurses comprised 5 consecutive days of theoretical presentations and 5 consecutive days of clinical experience with a preceptor. A test score ≥ 70% was required for successful completion of the course. Competency in chemotherapy administration and central-venous line care required documented course completion and a test score ≥ 70%. Documentation included the course title, date, hours, and presenter.
Continuing education classes were offered weekly and included presentations on a broad range of topics relevant to pediatric oncology nursing. Education topics were prioritized based on interviews with the nursing staff and results of a nursing survey. Completion of continuing education required documented class attendance including class title, date, hours, topic, and presenter. A nursing quality assessment completed prior to the nurse educator intervention found no documentation of education or clinical training; therefore, it was not possible to compare educational outcomes before and after the nurse educator program was implemented. The study included all full-time professional staff nurses who worked in the pediatric oncology unit from January 1, 2007, when the nurse educator program began, to September 30, 2009. A staff nurse was defined as a full-time (30 hours or more per week) professional nurse who had worked for a minimum of six months in the unit and not in a management position. A professional nurse was defined as a graduate of a school of nursing, as documented by the hospital’s department of human resources. Their educational preparation included three to four years of training in a university or independent nursing school setting; graduates are considered professional nurses and able to take a licensure exam. Forty-nine nurses met these criteria and were included in the study. Their mean length of employment at the partner site was 3.5 years (range, 0.5 to 9.6 years); there were 46 females (94%) and 3 males (6%). Twenty-four nurses (51%) were hired before program implementation and 25 (49%) afterwards. This study was approved by the Institutional Review Boards of St. Jude, the University of Tennessee Health Science Center, and the Medical School of Francisco Marroquin University of Guatemala.
Results
Completion of the three basic courses
All 25 nurses newly hired during the study period successfully completed the pediatric oncology nursing education course. The mean (±SD) test score was 86% ± 7.4% (range, 70% to 97%). Of the 49 nurses who were employed by the oncology unit during the study period, 42 (86%) participated in the chemotherapy course, and 39 (93%) of those achieved competency. The mean score was 87% ± 9.7% (range, 62% to 100%). Of the 49 nurses, 28 (57%) participated in the central- venous line care course, and 22 (79%) of those achieved competency. The mean score was 78% ± 15% (range, 46% to 98%).
Continuing education
The 49 nurses completed 26 ± 8.3 (range, 6 to 41) mean annual hours of continuing education in pediatric oncology, which exceeded the 10 hours required to maintain pediatric oncology nurse certification in the U.S. [18].
Cost comparison with other nursing education models
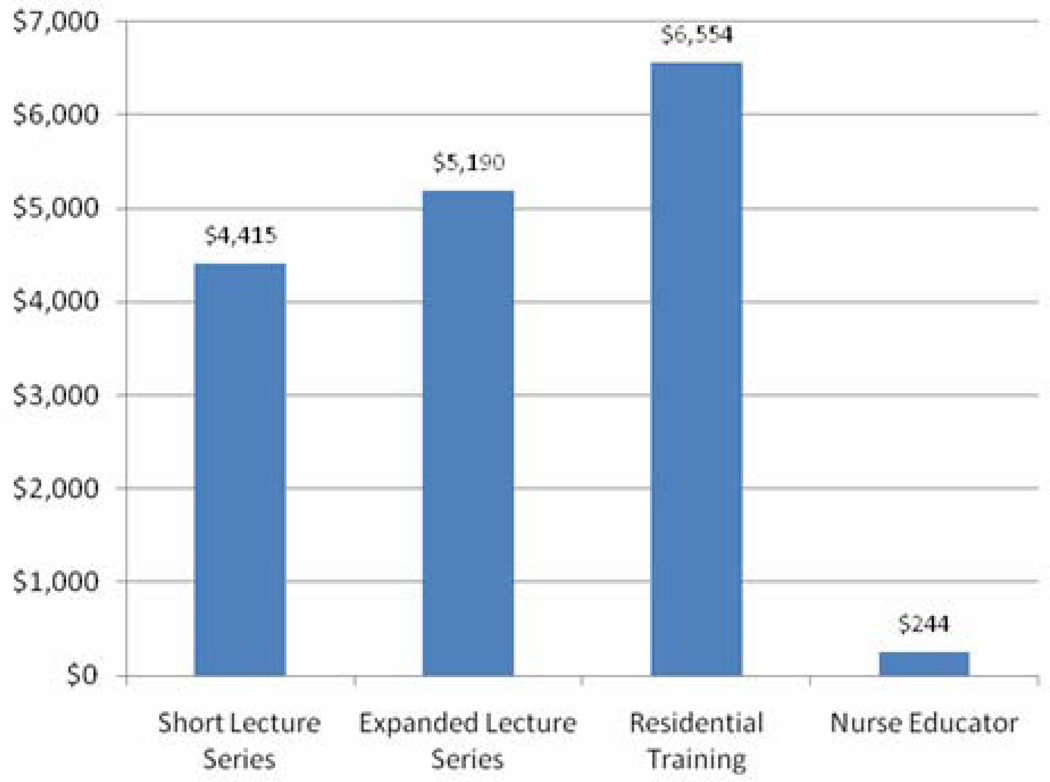
Wilimas et al. [8] described the direct costs in U.S. dollars (adjusted to 2009 values by using the consumer price index) of three single-intervention models previously used by the St. Jude IOP to educate pediatric oncology nurses: brief (1–2 week) lecture series at partner sites ($4,415/nurse), expanded (12-week) lecture series at partner sites ($5,190/nurse) and 3-month residential training ($6,554/nurse). The direct costs (salary and benefits) of a full time nurse educator who provided education to 49 staff nurses over the study time period was $244/nurse annually (Fig. 1). Neither start-up costs, such as that of the 4-week education course in Chile for the nurse educator ($3,670), nor time spent by St. Jude staff members developing the program were included in the costs of any of the educational models.
Figure 1.
Average educational cost per pediatric oncology nurse by educational model
Discussion
As previously reported [19], a 2006 nursing quality assessment found no documentation of theoretical or clinical training for nurses within the Guatemalan National Pediatric Oncology Unit. Numerous factors contributed to this deficiency. There was no organized approach to education in the pediatric oncology unit, and nurses were not provided time or support for educational activities. The unit’s head nurse was responsible for educating newly hired nurses, but her many other responsibilities left little time to do so. Further, specialized training for nurses was not perceived as a high priority by the institutional leadership, and as a result financial support was unavailable.
This study demonstrated that a full-time nurse educator positively impacts pediatric oncology nursing education outcomes and offers a sustainable model for providing initial and ongoing pediatric oncology education to nurses in Guatemala. By October 2009, of the 49 nurses, 42 (86%) had participated in the chemotherapy course, and 39 (93%) of those achieved competency, and 28 (57%) participated in the in central-venous line care course, and 22 (79%) of those achieved competency. Chemotherapy competency was initially considered a priority and the course was offered more frequently than the central- venous line care course and thus contributed to the higher participation rate. Of the 25 nurses hired after January 2007, all completed a 2-week pediatric oncology course; whereas, the 24 nurses hired before that date had received no clinical or theoretical education. Their training had comprised an unpaid 15-day trial period shadowing a busy staff nurse. The 26 mean annual hours of continuing education completed was considerably greater than the 10 hours required for pediatric oncology nursing certification and was crucial to compensate for the previous lack of oncology-specific education. Most important, the nurse educator remained available to mentor staff nurses on a daily basis and to assess the effects of the education program. Finally, the per capita cost of the nurse educator model, determined by the educator’s salary divided by the number of nurses educated annually is not expected to increase significantly. The salary of the nurse educator will increase over time, but the educator will continue to provide continuing education and clinical training to the entire staff of 49 nurses. The number of nurses educated will remain stable or increase as new positions are created.
The nurse educator program was effective for several reasons. The educator was provided education, resources, and professional support for this new role. The educator was an experienced nurse at the partner site but had received no formal pediatric oncology education and had limited experience in teaching. After the educator was hired in 2007, the educator completed a 4-week comprehensive educator course at the Latin American Center for Pediatric Oncology Nursing Education. Professional peer support and continuing pediatric oncology education was consistently provided via bimonthly online meetings hosted by www.Cure4Kids.org. Basic management principles also played a role in the educator’s effectiveness. The role was clearly defined, and education responsibilities were closely monitored. Language and cultural barriers were limited because the educator was hired from within the partner site country and education and support was provided primarily by the Latin American Center for Pediatric Oncology Nursing Education [15].
The size and composition of the staff sample was a strength of the study. Forty-nine nurses met the defining criteria for professional staff nurse, and all were included in the study. The detailed documentation available during the 2009 assessment was another positive attribute of the study. Each of the 49 nurses had an individual education record that included documentation of the education provided and copies of the scored evaluation tests. There were also study limitations. Scheduling time away from patient care was a challenge, and all professional nurses were not able to participate in the chemotherapy and central- venous line care courses. After a 2009 site visit, the administrative director agreed to give the nurses more dedicated time to attend classes each month, and 12 months after completion of the study, the nurse educator reported that the chemotherapy course was provided to 5 of the 10 nurses who had not achieved competency and the central-venous line care course was provided to 22 of the 27 nurses who had not achieved competency. Only professional nurses were included in this study; however, the same educational content was provided to technical nurses because of their similar patient care roles. Although their roles are similar, technical nurses have 10 to 12 months of education as opposed to 3 to 4 years for the professional nurse. Future studies should include an evaluation of educational outcomes for both professional and technical nurses.
A logical progression in research would be to replicate this study at other pediatric oncology hospitals in low-income countries and include clinical outcomes. Nurse educators have been established in El Salvador, Chile, Mexico (3 sites), Colombia, and Honduras. Close monitoring of their work suggests initial success; however, a quantitative evaluation is needed. Large-scale studies in both high-income and low-income countries have suggested that nursing education contributes to improved patient outcomes, including reduced mortality [9–12]. Although this study measured short term outcomes, it was a necessary first step in the process of a comprehensive program evaluation [17]. The next phase of program evaluation will include the measurement of nurse-sensitive clinical outcomes such as nosocomial infection rates and central-venous line and chemotherapy complications.
Providing education to pediatric oncology nurses in low-income countries is an important factor in closing the survival gap and one that has been given little attention. This is the first study to evaluate defined outcomes of pediatric oncology nursing education in a low-income country. Although long term clinical outcomes are yet to be determined, our findings suggest that a full time nurse educator is an effective, affordable, and sustainable solution to meet pediatric oncology educational needs of nurses in Guatemala and similar countries. Pediatric oncology professionals in high-income countries take for granted the high level of nurse education, but our findings are remarkable in a low-income country, particularly when one considers that the educator position was a newly created nursing role in Guatemala, the educator did not have experience in teaching or formal training in pediatric oncology, and the unit had no history of providing nursing education. Two keys for success warrant emphasis: 1) the educator was dedicated solely to staff education and clinical training without the competing responsibilities of providing direct patient care, and 2) the educator received education, resources, and professional support on an ongoing basis. This model is not limited to use within pediatric oncology settings and could easily be adapted to other subspecialties in low-income countries.
Acknowledgements
We thank Chong Wang MS and Jie Yang PhD for assistance with data analysis and Sharon Naron MPA, MLS for editorial support.
Funding: National Cancer Institute (Grant CA21765; Bethesda MD, USA) and American Lebanese Syrian Associated Charities (ALSAC; Memphis, TN, USA).
Footnotes
Conflict of Interest
The authors declare no conflict of interest.
References
- 1.Jemal A, Siegel R, Ward E, et al. Cancer statistics. CA Cancer J Clin. 2007;57:43–66. doi: 10.3322/canjclin.57.1.43. [DOI] [PubMed] [Google Scholar]
- 2.Barr RD, Ribeiro RC, Agarwal BR, et al. Pediatric oncology in countries with limited resources. In: Pizzo PA, Poplack DG, editors. Principles and practice of pediatric oncology. Philadelphia: Lippincott, Williams and Wilkins; 2006. pp. 1604–1616. [Google Scholar]
- 3.Howard SC, Marinoni M, Castillo L, et al. Improving outcomes for children with cancer in low-income countries in Latin America: A report on the recent meetings of the Monza International School of Pediatric Hematology/Oncology (MISPHO)-Part I. Pediatr Blood Cancer. 2007;48:364–369. doi: 10.1002/pbc.21003. [DOI] [PubMed] [Google Scholar]
- 4.Wagner HP, Antic V. The problem of pediatric malignancies in the developing world. Ann NY Acad Sci. 1997;824:193–204. doi: 10.1111/j.1749-6632.1997.tb46222.x. [DOI] [PubMed] [Google Scholar]
- 5.McGregor LM, Metzger ML, Sanders R, et al. Pediatric cancers in the new millennium: Dramatic progress, new challenges. Oncology (Williston Park) 2007;21:809–820. [PubMed] [Google Scholar]
- 6.Hockenberry MJ, Kline NE. Nursing support of the child with cancer. In: Pizzo PA, Poplack DG, editors. Principles and practice of pediatric oncology. Philadelphia: Lippincott, Williams and Wilkins; 2006. pp. 1380–1396. [Google Scholar]
- 7.Sheldon LK. International cancer care: What is the role of oncology nursing? Clin J Onco. 2010;14:539–541. doi: 10.1188/10.CJON.539-541. [DOI] [PubMed] [Google Scholar]
- 8.Wilimas JA, Donahue N, Chammas G, et al. Training subspecialty nurses in developing countries: Methods, outcome, and cost. Med Pediatr Oncol. 2003;41:136–140. doi: 10.1002/mpo.10242. [DOI] [PubMed] [Google Scholar]
- 9.Aiken LH, Clarke SP, Cheung RB, et al. Educational levels of hospital nurses and surgical patient mortality. JAMA. 2003;290:1617–1623. doi: 10.1001/jama.290.12.1617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chomba E, McClure EM, Wright LL, et al. Effect of WHO newborn care training on neonatal mortality by education. Ambul Pediatr. 2008;8:300–304. doi: 10.1016/j.ambp.2008.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Elixhauser A, Steiner C, Fraser I. Volume thresholds and hospital characteristics in the United States. Health Aff (Millwood) 2003;22:167–177. doi: 10.1377/hlthaff.22.2.167. [DOI] [PubMed] [Google Scholar]
- 12.Estabrooks CA, Midodzi WK, Cummings GG, et al. The impact of hospital nursing characteristics on 30-day mortality. Nurs Res. 2005;54:74–84. doi: 10.1097/00006199-200503000-00002. [DOI] [PubMed] [Google Scholar]
- 13.Wilimas JA, Ribeiro RC. Pediatric hematology-oncology outreach for developing countries. Hematol Oncol Clin North Am. 2001;15:775–787. doi: 10.1016/s0889-8588(05)70246-x. [DOI] [PubMed] [Google Scholar]
- 14.Kellie SJ, Howard SC. Global child health priorities: What role for paediatric oncologists. Eur J Cancer. 2008;44:2388–2396. doi: 10.1016/j.ejca.2008.07.022. [DOI] [PubMed] [Google Scholar]
- 15.Eden T. Translation of cure for acute lymphoblastic leukaemia to all children. Brit J Haematol. 2002;118:945–951. doi: 10.1046/j.1365-2141.2002.03670.x. [DOI] [PubMed] [Google Scholar]
- 16.Day SW, Segovia L, Viveros P, et al. Development of a Latin American center for pediatric oncology nursing education. Pediatr Blood Cancer. 2011;56:5–6. doi: 10.1002/pbc.22856. [DOI] [PubMed] [Google Scholar]
- 17.Weiss CH. Evaluation. 2nd ed. New Jersey: Prentice Hall; 1998. [Google Scholar]
- 18.Oncology Nursing Certification Corporation. Retrieved December 10, 2010 from http://www.oncc.org.
- 19.Day SW, Dycus PM, Chismark EA, McKeon L. Quality assessment of pediatric oncology nursing care in a Central American country: Findings, recommendations, and preliminary outcomes. Pediatr Nurs. 2008;34:367–373. [PubMed] [Google Scholar]