Abstract
The transcription factor Nrf2 exerts protective effects in numerous experimental models of acute kidney injury, and is a promising therapeutic target in chronic kidney disease. To provide a detailed insight into the regulatory roles of Nrf2 in the kidney, we performed integrated transcriptomic and proteomic analyses of kidney tissue from wild-type and Nrf2 knockout mice treated with the Nrf2 inducer methyl-2-cyano-3,12-dioxooleano-1,9-dien-28-oate (CDDO-Me, also known as bardoxolone methyl). After 24 hours, analyses identified 2561 transcripts and 240 proteins that were differentially expressed in the kidneys of Nrf2 knockout mice, compared to wild-type counterparts, and 3122 transcripts and 68 proteins that were differentially expressed in wild-type mice treated with CDDO-Me, compared to vehicle control. In light of their sensitivity to genetic and pharmacological modulation of renal Nrf2 activity, genes/proteins that regulate xenobiotic disposition, redox balance, the intra/extracellular transport of small molecules, and the supply of NADPH and other cellular fuels were found to be positively regulated by Nrf2 in the kidney. This was verified by qPCR, immunoblotting, pathway analysis and immunohistochemistry. In addition, the levels of NADPH and glutathione were found to be significantly decreased in the kidneys of Nrf2 knockout mice. Thus, Nrf2 regulates genes that coordinate homeostatic processes in the kidney, highlighting its potential as a novel therapeutic target.
Keywords: Nrf2, Keap1, iTRAQ, ROS, oxidative stress
INTRODUCTION
Acute kidney injury (AKI) is a significant clinical problem, with more than 7% of patients developing some form of AKI following admission to hospital 1. Furthermore, as a result of the renal vasculature being exposed to approximately 25% of resting cardiac output 2, and given its role in the urinary excretion of conjugated reactive metabolites, the kidney often encounters relatively high levels of xenobiotics and their metabolites, of which a number are known to suppress renal function. A key mechanism underlying the nephrotoxicity of many xenobiotics (examples include cisplatin 3, ferric nitrilotriacetate 4 and streptozotocin 5) is their ability to induce the generation of reactive oxygen species (ROS) and consequent oxidative stress in specific regions of the kidney.
The transcription factor Nrf2 is widely regarded as the master regulator of defence against the deleterious effects of oxidative stress in mammalian cells 6. Under normal conditions, the level and activity of Nrf2 is restricted via its association with the cytosolic protein Keap1, which targets the transcription factor for ubiquitination and proteasomal degradation 6. In the presence of ROS and other potentially harmful stimuli, Nrf2 evades Keap1-mediated repression and accumulates in the nucleus, where it binds to antioxidant response elements (AREs) located in the promoter regions of cytoprotective genes, elevating expression of their products which serve to purge the toxic insult and minimise its damaging effects 6. As a result, there is considerable interest in targeting Nrf2 for therapeutic benefit, particularly in disease contexts in which ROS play an important role 7. Indeed, the triterpenoid Nrf2 inducer CDDO-Me (also known as bardoxolone methyl) had until recently shown promise as a novel therapy for chronic kidney disease (CKD) 8, when a phase III clinical trial was halted due to adverse cardiovascular events that are thought to be associated with an Nrf2-independent perturbation of endothelin signalling 9, 10. Recently, two new phase II trials of CDDO-Me (in CKD - NCT02316821, and pulmonary arterial hypertension - NCT02036970) were initiated with stricter exclusion criteria for patients with a history of cardiovascular disease.
We previously provided insights into the molecular mechanisms by which Nrf2 protects against drug-induced liver injury, by defining the constitutive Nrf2-regulated hepatic proteome 11. We demonstrated that the expression of a number of proteins responsible for the detoxification of acetaminophen and other drugs is markedly decreased in the livers of Nrf2−/− mice 11, consistent with the enhanced sensitivity of these animals to the hepatotoxicty provoked by these compounds 12, 13. In an extension to this study, we recently defined the biological processes that are sensitive to pharmacological modulation of Nrf2 in the liver by detailing the hepatic protein pool that is augmented in Nrf2+/+ mice, but not Nrf2−/− counterparts, in response to CDDO-Me 14. This work revealed that CDDO-Me is a highly selective inducer of Nrf2-regulated proteins in the liver, and identified six proteins (cytochrome P450 2A5, glutathione-S-transferases Mu 1 and Mu 3, ectonucleoside-triphosphate diphosphohydrolase, UDP-glucose-6-dehydrogenase and epoxide hydrolase) that were both downregulated in Nrf2−/− mice and upregulated by CDDO-Me in Nrf2+/+ mice 14.
In keeping with the role of Nrf2 as a key regulator of cell defence processes, it is known that Nrf2 protects against a number of nephrotoxic insults in experimental models, as we recently reviewed 15. For example, ischemic-reperfusion of the mouse kidney has been shown to stimulate Nrf2 signalling 16, whilst the associated renal injury is exacerbated in Nrf2−/− mice 17 and lessened in wild-type mice pre-treated with small molecule Nrf2 inducers 18, 19. Similar consequences of Nrf2 inhibition and induction have been noted in the context of cisplatin-induced proximal tubular cell damage 3. Despite these and other studies supporting a role for Nrf2 in protection against AKI 15, a global analysis of the biological processes that are regulated by Nrf2 in the kidney in vivo has yet to be performed. To address this knowledge gap, we have performed integrated transcriptomic and proteomic analyses of kidney homogenates from Nrf2+/+ and Nrf2−/− mice, treated or not with CDDO-Me. Our findings support a role for Nrf2 in regulating the expression of a battery of genes/proteins that contribute to the maintenance of renal homeostasis.
RESULTS
Genetic and pharmacological modulation of Nrf2 in the kidney
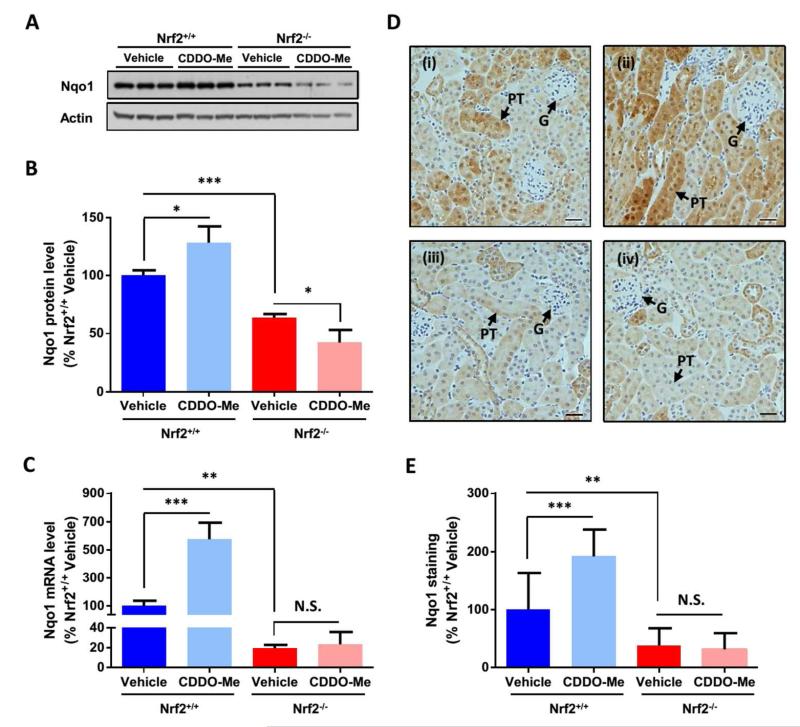
We first confirmed that CDDO-Me is an effective inducer of Nrf2 signalling in renal cells, through immunoblot and qPCR analysis of primary human proximal tubule epithelial cells following exposure to the compound, which provoked the accumulation of Nrf2 and upregulated the expression of the established Nrf2 target NAD(P)H dehydrogenase quinone 1 (Nqo1) at both protein and mRNA levels (Fig. S1). Nqo1 was also found to be expressed at a lower level following siRNA depletion of Nrf2, and at a higher level following transfection with Keap1 siRNA (Fig. S1), confirming that it is a robust marker of Nrf2 activity in renal cells. In light of these findings, we verified that the Nrf2 pathway could be pharmacologically modulated in the kidneys of Nrf2+/+ mice and was non-functional in Nrf2−/− mice, prior to conducting transcriptomic and proteomic analyses, by determining the expression level of Nqo1 in kidney homogenates from both genotypes, 24 h after dosing with vehicle or CDDO-Me 20. The level of Nqo1 protein (Fig. 1A-B) and mRNA (Fig. 1C) was significantly lower in the kidneys of vehicle-exposed Nrf2−/− mice, compared with Nrf2+/+ counterparts, consistent with loss of Nrf2 function. Moreover, whilst the Nrf2 inducer CDDO-Me provoked the induction of Nqo1 24 h after administration to Nrf2+/+ mice, this effect was abrogated in Nrf2−/− mice (Fig. 1A-C). Consistent with these findings, and the established role of Nrf2 in the protection of mice against pathological insults that target the cortical tubules 15, there was a significant decrease in Nqo1 immunohistochemical staining in the renal cortex, and particularly within the proximal tubules, of Nrf2−/− mice, compared with Nrf2+/+ counterparts (Fig. 1D-E). Furthermore, a significant increase in Nqo1 staining was observed in these structures in Nrf2+/+, but not Nrf2−/−, mice in response to CDDO-Me (Fig. 1D-E). Taken together, these data validate our model of genetic and pharmacological modulation of renal Nrf2 activity, and provide a platform for a global analysis of the regulatory roles of Nrf2 in the kidney.
Fig. 1. Genetic and pharmacological modulation of Nrf2 in the mouse kidney.
Mice of the indicated genotype were given a single i.p. injection of vehicle (DMSO) or CDDO-Me (3 mg/kg) and, 24 h later, Nqo1 levels were determined by (A-B) immunoblotting, (C) qPCR and (D-E) immunohistochemical analysis of whole kidney tissue. (B) Nqo1 band intensities were quantified by densitometry and normalized against those of β-actin. (C) Nqo1 mRNA levels were normalized to those of Ppia. (D-E) Nqo1 expression levels in the cortex of Nrf2+/+ mice treated with (i) DMSO or (ii) CDDO-Me, or Nrf2−/− mice treated with (iii) DMSO or (iv) CDDO-Me. G, glomerulus; PT, proximal tubule. Scale bars represent 50 μm. Data represent mean + S.D. of n=3 (A-C) or n=5 (D-E) animals per group. Statistical analysis was performed with an unpaired t test; *, P≤0.05; **, P≤0.01; ***, P≤0.001; N.S., non-significant.
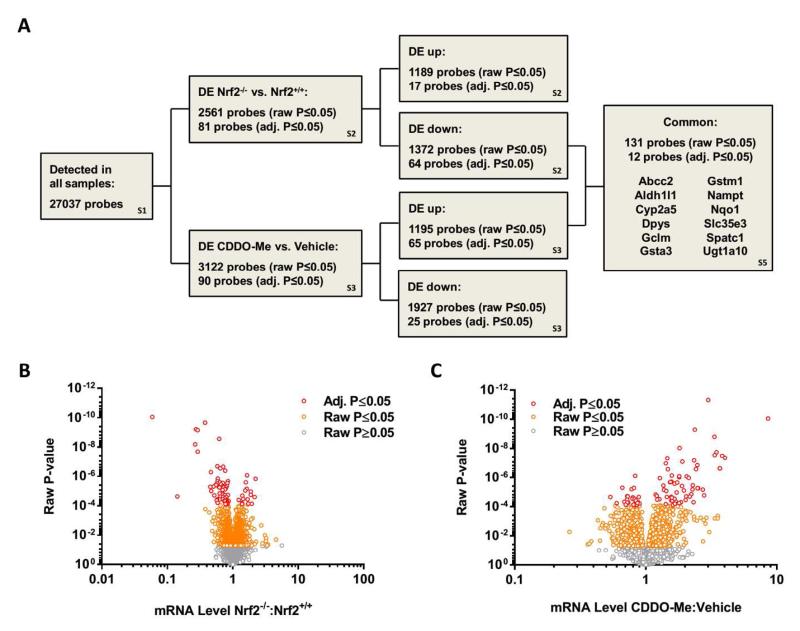
Definition of the Nrf2-regulated renal transcriptome
To characterise the regulatory roles of Nrf2 in the kidney, we performed microarray analyses on tissue homogenates from Nrf2+/+ and Nrf2−/− mice treated with vehicle or CDDO-Me for 24 h (Fig 2A). Of the 27037 probes recognised in all samples (Table S1), 2561 (raw P≤0.05) or 81 (adj. P≤0.05) probes were differentially expressed in the kidneys of Nrf2−/− mice, compared with Nrf2+/+ counterparts (Fig. 2B, Table S2), whilst 3122 (raw P≤0.05) or 90 (adj. P≤0.05) probes were differentially expressed in the kidneys of Nrf2+/+ mice treated with CDDO-Me, compared with vehicle control (Fig. 2C, Table S3). None of the probes that were significantly altered (adj. P≤0.05) in Nrf2+/+ mice treated with CDDO-Me were altered in Nrf2−/− mice treated with the compound (Table S3), demonstrating its relative specificity as an inducer of Nrf2. In keeping with this, Ingenuity Pathway Analysis (IPA) of the genes that were significantly down-regulated in the kidneys of Nrf2−/− mice, or significantly up-regulated in the kidneys of Nrf2+/+ mice treated with CDDO-Me, demonstrated that the ‘NRF2-mediated Oxidative Stress Response’ was the most significantly altered pathway in both cases (Table S4), supporting the genetic and pharmacological modulation of Nrf2 in our mouse model. Nine other pathways, including ‘Xenobiotic Metabolism Signaling’, ‘Aryl Hydrocarbon Receptor Signaling’, ‘PXR/RXR Activation’ and ‘Glutathione-mediated Detoxification’, were commonly affected by both genetic inhibition and pharmacological induction of Nrf2 (Table S4), highlighting the role of Nrf2 in regulating homeostatic signalling processes in the mouse kidney. Only two pathways were significantly up-regulated in the kidneys of Nrf2−/− mice, ‘VDR/RXR Activation’ and ‘β-Adrenergic Signalling’ (Table S4), whilst none were significantly down-regulated in the kidneys of Nrf2+/+ mice treated with CDDO-Me.
Fig. 2. Definition of the Nrf2-regulated renal transcriptome.
Microarray analysis was performed on kidney tissue from Nrf2+/+ or Nrf2−/− mice treated with vehicle (DMSO) or CDDO-Me for 24 h. (A) Overview of microarray analysis. DE; differentially expressed. The relevant supplementary tables are indicated in the boxes. (B-C) Volcano plots depicting differentially expressed genes in the kidneys of (B) Nrf2−/− mice, compared with Nrf2+/+ counterparts, and (C) Nrf2+/+ mice treated with CDDO-Me, compared to vehicle. Each point represents a single gene probe, with those shaded orange (raw P-value) and red (adjusted P-value) found to be significantly different between groups.
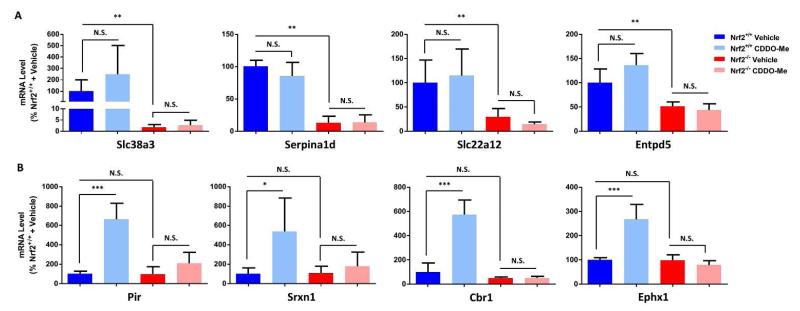
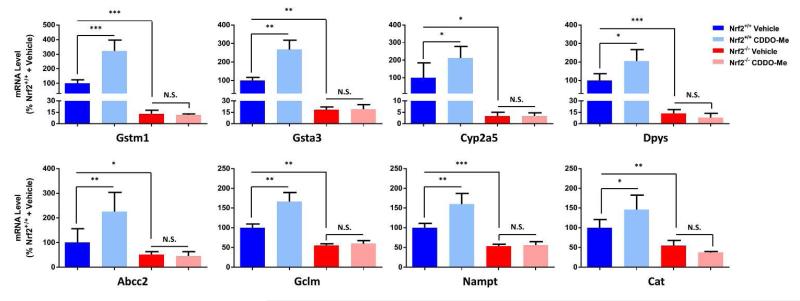
The 64 probes that were significantly downregulated (adj. P≤0.05) in the kidneys of Nrf2−/− mice represented 56 unique coding genes, whilst the 65 probes that were significantly upregulated (adj. P≤0.05) in the kidneys of Nrf2+/+ mice treated with CDDO-Me represented 57 unique coding genes. We confirmed the altered expression level of selected coding genes in the kidneys of Nrf2−/− mice and CDDO-Me -treated Nrf2+/+ mice by qPCR (Fig. 3). Given that seven genes encoding for transporters were found to be differentially expressed (adj. P≤0.05) in the kidneys of Nrf2−/− mice and/or CDDO-Me -treated Nrf2+/+ mice, we included solute carrier family 38 member 3 (Slc38a3) and Slc22a12 in this targeted analysis, which confirmed their lower expression in the kidneys of Nrf2−/− mice (Fig. 3A). Cross-referencing of the microarray data sets revealed that no probes were both upregulated in Nrf2−/− mice and downregulated in CDDO-Me -treated Nrf2+/+ mice, whilst twelve unique coding genes were found to be both downregulated in Nrf2−/− mice and upregulated in CDDO-Me -treated Nrf2+/+ mice (Fig. 2A, Tables 1 and S5). The differential expression of a sub-set of these twelve coding genes was verified by qPCR (Fig. 4), which showed good agreement with the microarray data. It is plausible that alterations of Nrf2 signalling in other tissues could indirectly affect the expression of the above genes in the kidneys of Nrf2−/− mice or CDDO-Me -treated Nrf2+/+ mice. However, bioinformatic analysis identified ARE-like sequences in many of the genes that were differentially expressed following genetic and/or pharmacological modulation of renal Nrf2 activity (Table S6), including those which have been shown previously, through integrated ChIP-Seq and qPCR analyses, to be bound by Nrf2 and/or differentially expressed in Nrf2−/− and Keap1−/− mouse embryonic fibroblasts (Table S7) 21. Together, these findings indicate a role for Nrf2 as a transcriptional regulator of the above genes in the kidney.
Fig. 3. Genes sensitive to genetic inhibition or pharmacological induction of Nrf2 in the mouse kidney.
qPCR validation of genes that were shown to be (A) significantly downregulated in the kidneys of Nrf2−/− mice, or (B) significantly upregulated in the kidneys of Nrf2+/+ mice treated with CDDO-Me. Gene expression levels are normalized to those of Ppia. Data represent mean + S.D. of n=5 animals per group. Statistical analysis of qPCR data was performed with an unpaired t test or Mann-Whitney test *, P≤0.05; **, P≤0.01; ***, P≤0.001; N.S., non-significant.
Table 1. Genes/proteins sensitive to genetic inhibition and pharmacological induction of Nrf2 in the mouse kidney.
Microarray and iTRAQ analyses were performed on kidney tissue from Nrf2+/+ or Nrf2−/− mice treated with vehicle (DMSO) or CDDO-Me for 24 h. The 12 genes shown above were shown to be both significantly downregulated in the kidneys of Nrf2−/− mice and significantly upregulated in the kidneys of Nrf2+/+ mice treated with CDDO-Me. From the iTRAQ analysis, 9 of the genes were also shown to be significantly downregulated at the protein level in the kidneys of Nrf2−/− mice. The remaining 3 genes were not detected (N.D.) at the protein level by iTRAQ. These 9 genes/proteins are therefore considered to be most sensitive to genetic inhibition and pharmacological induction of Nrf2 in the mouse kidney.
| Microarray |
iTRAQ |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Nrf2−/− vs. Nrf2+/+ | CDDO-Me vs. Vehicle | Nrf2−/− vs. Nrf2+/+ | CDDO-Me vs. Vehicle | ||||||||
|
|
|
||||||||||
| Gene Symbol |
David ID |
RefSeq | Ratio | Adj. P-value | Ratio | Adj. P-value | Accession | Ratio | P-value | Ratio | P-value |
| Abcc2 | 451709 | NM_013806 | 0.77 | 9.43−03 | 1.46 | 2.79−04 | Q8VI47 | 0.79 | 6.66−03 | 1.22 | 4.76−03 |
| Aldh1l1 | 430403 | NM_027406 | 0.72 | 8.21−03 | 1.38 | 9.42−03 | Q8R0Y6 | 0.33 | 5.14−10 | 1.08 | 2.12−01 |
| Cyp2a5 | 420632 | NM_007812 | 0.27 | 6.17−05 | 2.04 | 2.01−02 | P20852 | N.D. | N.D. | N.D. | N.D. |
| Dpys | 425658 | NM_001164466 | 0.29 | 8.53−06 | 1.67 | 4.28−02 | Q9EQF5 | 0.66 | 3.78−02 | 1.04 | 7.75−01 |
| Gclm | 425831 | NM_008129 | 0.76 | 1.40−03 | 1.28 | 2.96−03 | O09172 | 0.81 | 2.06−02 | 1.05 | 5.59−01 |
| Gsta3 | 423583 | NM_001077353 | 0.27 | 8.20−06 | 2.13 | 2.89−03 | P30115 | 0.16 | 8.62−08 | 0.90 | 3.42−01 |
| Gstm1 | 443311 | NM_010358 | 0.38 | 3.81−06 | 1.90 | 4.37−04 | P10649 | 0.09 | 1.14−10 | 1.16 | 5.82−02 |
| Nampt | 465583 | NM_021524 | 0.70 | 1.08−02 | 1.44 | 1.07−02 | Q99KQ4 | 0.61 | 8.19−03 | 1.22 | 1.14−01 |
| Nqo1 | 481143 | NM_008706 | 0.29 | 1.45−04 | 3.47 | 1.39−04 | Q64669 | 0.28 | 1.66−07 | 1.36 | 1.02−03 |
| Slc35e3 | 443078 | NM_029875 | 0.84 | 3.44−02 | 1.22 | 1.96−02 | Q6PGC7 | N.D. | N.D. | N.D. | N.D. |
| Spatc1 | 429270 | NM_028852 | 0.63 | 1.68−02 | 1.80 | 2.38−03 | Q148B6 | N.D. | N.D. | N.D. | N.D. |
| Ugt1a10 | 446962 | NM_201641 | 0.58 | 9.04−04 | 1.45 | 2.12−02 | Q6ZQM8 | 0.25 | 6.18−05 | 1.09 | 5.50−01 |
Fig. 4. Genes sensitive to both genetic inhibition and pharmacological induction of Nrf2 in the mouse kidney.
qPCR validation of genes that were shown to be both significantly downregulated in the kidneys of Nrf2−/− mice and significantly upregulated in the kidneys of Nrf2+/+ mice treated with CDDO-Me. Gene expression levels are normalized to those of Ppia. Data represent mean + S.D. of n=5 animals per group. Statistical analysis of qPCR data was performed with an unpaired t test or Mann-Whitney test; *, P≤0.05; ***, P≤0.001; N.S., non-significant.
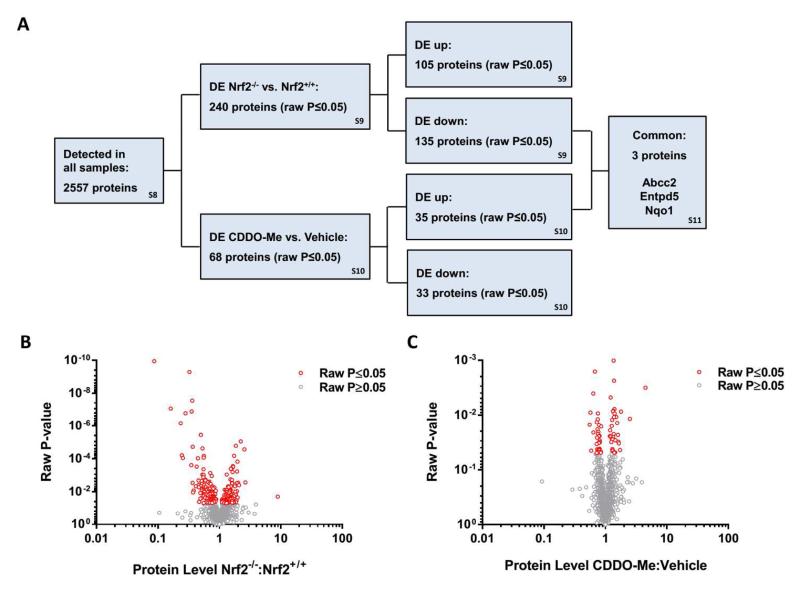
Definition of the Nrf2-regulated renal proteome
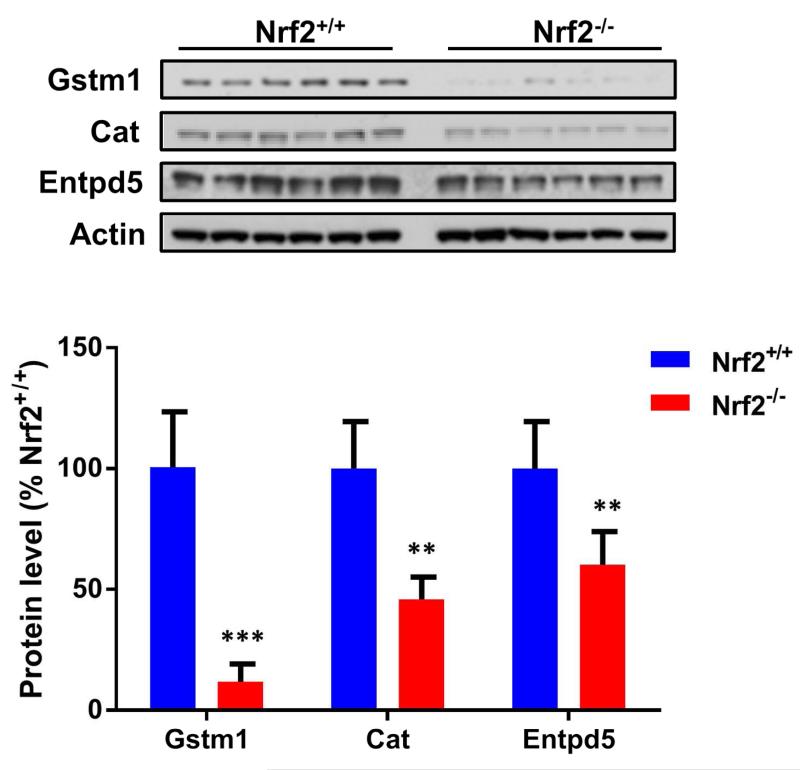
To complement our transcriptomic analysis of the kidneys of Nrf2+/+ and Nrf2−/− mice treated with vehicle or CDDO-Me, we performed isobaric tags for relative and absolute quantification (iTRAQ) - based proteomic analyses on the same tissues (Fig. 5A). Of the 2557 proteins quantified in at least four samples from each group at a false discovery rate of 1 % (Table S8), 240 were differentially expressed (P≤0.05) in the kidneys of Nrf2−/− mice, compared with Nrf2+/+ counterparts (Fig. 5B, Table S9). Three of the most substantially down-regulated proteins in the kidneys of Nrf2−/− mice, glutathione-S-transferase Mu 1 (Gstm1; 11.5-fold lower in Nrf2−/− vs. Nrf2+/+ mice), catalase (Cat; 4.3-fold lower) and ectonucleoside-triphosphate diphosphohydrolase (Entpd5; 2.8-fold lower), were also shown by immunoblotting of tissue homogenates to be expressed at a lower level in the absence of Nrf2 (Fig. 6), demonstrating the robustness of our proteomic analysis. We also confirmed that the DMSO vehicle had little effect on the expression levels of Nrf2-regulated proteins by performing an independent iTRAQ analysis of kidney homogenates from untreated Nrf2+/+ and Nrf2−/− mice (Fig. S2), which showed excellent agreement with the primary data set.
Fig. 5. Definition of the Nrf2-regulated renal proteome.
iTRAQ analysis was performed on kidney tissue from Nrf2+/+ or Nrf2−/− mice treated with vehicle (DMSO) or CDDO-Me for 24 h. (A) Overview of iTRAQ findings. DE; differentially expressed. The relevant supplementary tables are indicated in the boxes. (B-C) Volcano plots depicting differentially expressed proteins in the kidneys of (B) Nrf2−/− mice, compared with Nrf2+/+ counterparts, and (C) Nrf2+/+ mice treated with CDDO-Me, compared to vehicle. Each point represents a single protein, with those shaded red found to be significantly different (raw P-value) between groups.
Fig. 6. Proteins sensitive to genetic inhibition of Nrf2 in the mouse kidney.
Immunoblot validation of Gstm1, Cat and Entpd5 as proteins with decreased expression in the kidneys of Nrf2−/− mice. Immunoreactive band intensities were quantified by densitometry and normalized against those of β-actin. Data represent mean + S.D. of n=6 animals per group. Statistical analysis of immunoblot data was performed with an unpaired t test; **, P≤0.01 ***, P≤0.001.
Compared to its effects on gene expression, the acute effects of a single 24 h exposure to CDDO-Me were less evident at the protein level, with 68 proteins found to be differentially expressed (P≤0.05) in the kidneys of Nrf2+/+ mice treated with CDDO-Me, compared with vehicle control (Fig. 5C, Table S10). Indeed, only ATP-binding cassette sub-family C member 2 (Abcc2), Entpd5 and Nqo1 were both significantly downregulated in the kidneys of Nrf2−/− mice and significantly up-regulated in the kidneys of Nrf2+/+ mice treated with CDDO-Me (Table S11). Whilst the relatively short timeframe used for this experiment (24 h) may not have been sufficient to provoke significant changes in the wider battery of Nrf2-regulated proteins, a targeted analysis revealed minimal additional changes in the expression of Nqo1, Gstm1, Cat and Entpd5 (which were sensitive to genetic inhibition of Nrf2 in the mouse kidney; Table S8) at earlier or later time points, or at different doses of CDDO-Me (Fig. S3).
IPA interrogation of the proteins that were significantly down-regulated in the kidneys of Nrf2−/− mice, or significantly up-regulated in the kidneys of Nrf2+/+ mice treated with CDDO-Me, again demonstrated that the ‘NRF2-mediated Oxidative Stress Response’ was one of the most significantly represented pathways in both cases (Table S12). Examination of the proteomic data also revealed that modulation of renal Nrf2 activity was associated with significant alterations in the expression level of proteins known to regulate core metabolic processes, including the pentose phosphate pathway (glucose-6-phosphate 1-dehydrogenase X, G6pdx; 6-phosphogluconate dehydrogenase decarboxylating, Pgd; transketolase, Tkt), the synthesis and recycling of amino acids (cysteine sulfinic acid decarboxylase, Csad; cystathionine gamma-lyase, Cth; threonine synthase-like 2, Thnsl2), and the metabolism of lipids/fatty acids (acetyl-coenzyme A acetyltransferase 1, Acat1; peroxisomal acyl-coenzyme A oxidase 3, Acox3; peroxisomal multifunctional enzyme type 2, Hsd17b4). These findings further indicate that Nrf2 regulates the expression of genes/proteins that coordinate renal homeostatic processes.
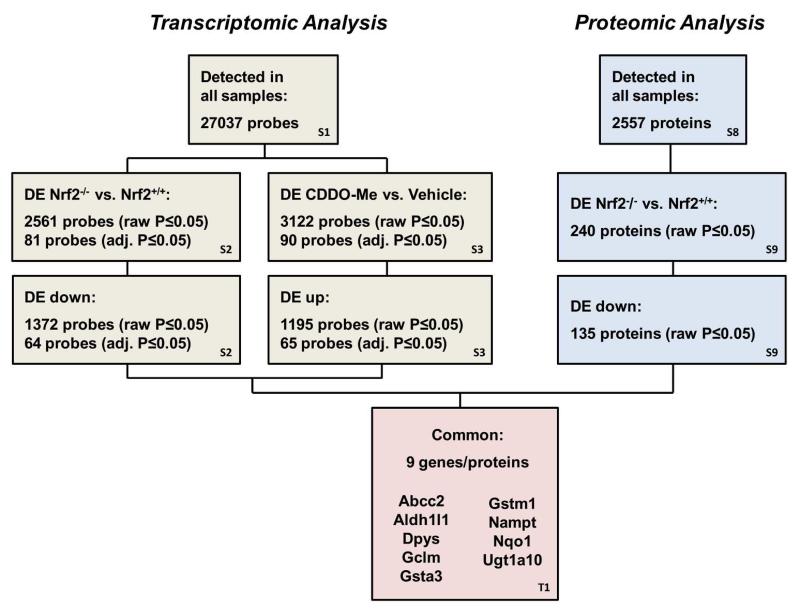
Comparison of transcriptomic and proteomic data
There was a good level of agreement between our transcriptomic and proteomic data sets (Fig. 7). Indeed, IPA examination of the data from Nrf2−/− mice identified twelve pathways that were commonly altered at both gene and protein expression levels (Tables S4 and S12). In keeping with this, of the twelve coding genes that were both significantly downregulated (adj. P≤0.05) in the kidneys of Nrf2−/− mice and upregulated in the kidneys of Nrf2+/+ mice treated with CDDO-Me according to our microarray analysis, nine were also found in our proteomic analysis to be significantly (P≤0.05) downregulated at the protein level in the kidneys of Nrf2−/− mice, whilst the remaining three proteins were not detected (Table 1). These data highlight this panel of genes/proteins as sensitive markers of Nrf2 activity in the mouse kidney. Most likely due to their low abundance in whole tissue homogenates, only 23 of the 72 transporters that were detected in our microarray analysis of the mouse kidney were also present in the iTRAQ data set (Table S13). Of the seven transporters that were differentially expressed (adj. P≤0.05) at the mRNA level in the kidneys of Nrf2−/− mice and/or CDDO-Me -treated Nrf2+/+ mice, three were detected in our iTRAQ analysis, with two of these (Abcc2 and Slc22a12) found to have significantly altered expression in response to genetic and/or pharmacological modulation of Nrf2 activity (Table S13).
Fig. 7. Correlation of transcriptomic and proteomic analyses of Nrf2 activity in the mouse kidney.
Microarray and iTRAQ analyses were performed on kidney tissue from Nrf2+/+ or Nrf2−/− mice treated with vehicle (DMSO) or CDDO-Me for 24 h. DE; differentially expressed. The relevant tables are indicated in the boxes. From the microarray analysis, 12 genes were shown to be both significantly downregulated in the kidneys of Nrf2−/− mice and significantly upregulated in the kidneys of Nrf2+/+ mice treated with CDDO-Me. From the iTRAQ analysis, 9 of the genes were also shown to be significantly downregulated at the protein level in the kidneys of Nrf2−/− mice (the remaining 3 genes were not detected at the protein level by iTRAQ). These 9 genes/proteins are therefore considered to be most sensitive to genetic inhibition and pharmacological induction of Nrf2 in the mouse kidney.
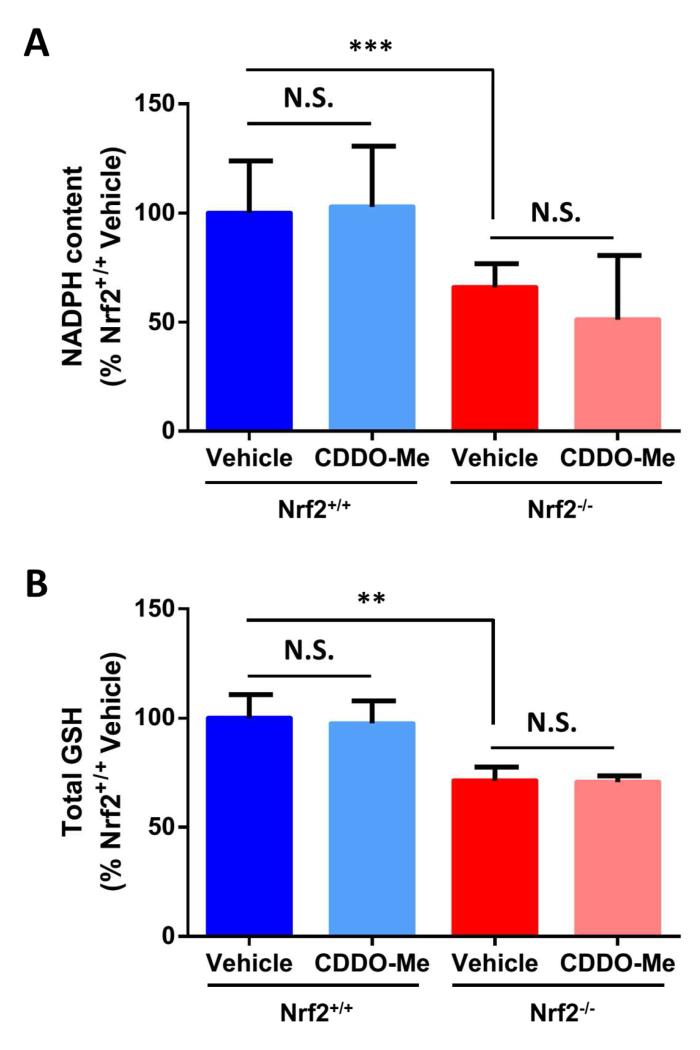
Nrf2 regulates the provision of NADPH and glutathione in the kidney
The transcriptomic and proteomic data sets demonstrated that genes/proteins that are known to regulate the synthesis and metabolism of NADPH and glutathione were downregulated in the kidneys of Nrf2−/− mice. Consistent with these observations, the levels of NADPH (Fig. 8A) and glutathione (Fig. 8B) were found to be significantly lower in the kidneys of vehicle-treated Nrf2−/− mice, compared to Nrf2+/+ counterparts. The levels of NADPH and glutathione were not altered by CDDO-Me in Nrf2+/+ or Nrf2−/− mice (Fig. 8A-B), in keeping with the minimal effects of CDDO-Me at the protein level at 24 h. Taken together, these data confirm that Nrf2 contributes to the provision of NADPH and glutathione, which serve as important cofactors in a number of homeostatic processes, in the kidney.
Fig. 8. Nrf2 regulates the provision of NADPH and glutathione in the kidney.
The (A) NADPH and (B) glutathione contents of kidney tissue from Nrf2+/+ or Nrf2−/− mice treated with vehicle (DMSO) or CDDO-Me for 24 h. (A) NADPH content is normalized to protein content and expressed as a percentage of vehicle-treated Nrf2+/+ mice. (B) Glutathione content is normalized to tissue weight and expressed as a percentage of vehicle-treated Nrf2+/+ mice. All data represent mean + S.D. of n=6 animals per group. Statistical analysis was performed using an unpaired t test; **, P≤0.01; ***, P≤0.001; N.S., non-significant.
DISCUSSION
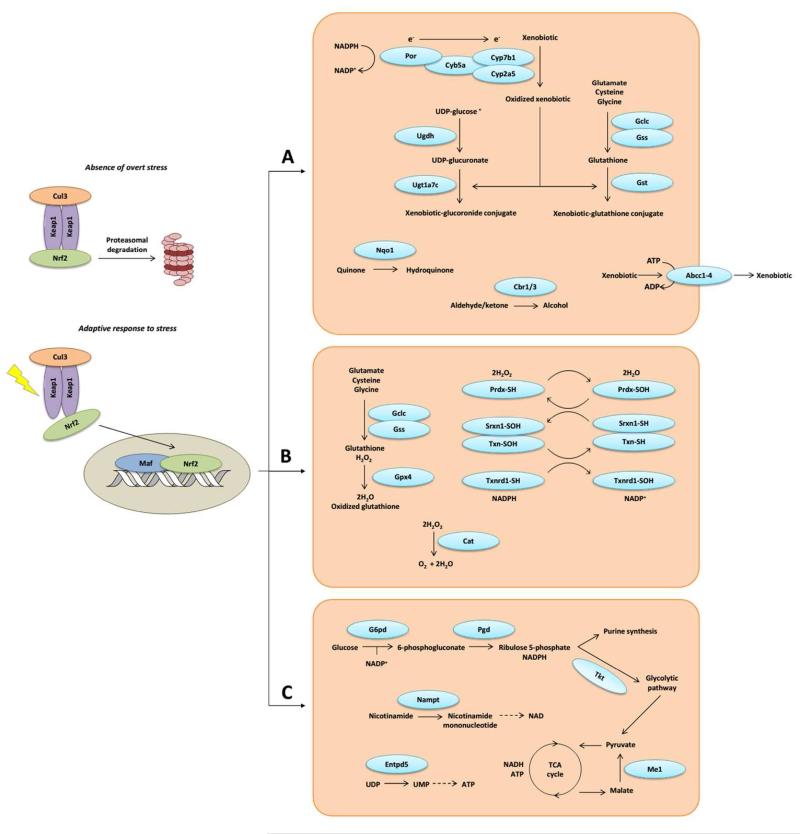
Delineating the biological processes that are regulated by Nrf2 in the kidney is critical to understand the mechanisms by which Nrf2 protects against nephrotoxic insults 22, and to rationalise the pharmacodynamic effects associated with therapeutic Nrf2 inducers in the kidney 23. Previous work has demonstrated the role of Nrf2 in regulating the expression of selected cytoprotective genes in the kidney in vivo and in renal cells cultured in vitro 17, 24. However, prior to this study, a global analysis of the biological processes that are regulated by Nrf2 in the kidney in vivo had not been performed. Using an integrated transcriptomic and proteomic approach, we have demonstrated that the kidneys of Nrf2−/− mice are deficient in the expression of genes/proteins that coordinate the synthesis and conjugation of glutathione, maintain cellular redox balance, control the metabolism and disposition of a wide range of xenobiotics, and regulate the supply of NADPH and other cellular fuels (Fig. 9). Consistent with these observations, we have also shown that Nrf2 influences the provision of NADPH and glutathione in the kidney in vivo. These findings demonstrate the role of Nrf2 in regulating the expression of genes/proteins that contribute to the maintenance of renal homeostasis.
Fig. 9. Schematic overview of biological processes regulated by Nrf2 in the mouse kidney.
Integrated transcriptomic and proteomic analyses reveal that Nrf2 controls the expression of genes/proteins that contribute to the maintenance of normal kidney function, by (a) coordinating xenobiotic disposition, (b) maintaining redox balance, and (c) mediating the supply of NAPDH and other cellular fuels.
As we recently reviewed, genetic and pharmacological modulation of Nrf2 activity has been shown to alter the threshold for sensitivity to a number of experimental nephrotoxins 15. For example, cisplatin-induced renal injury is exacerbated in Nrf2−/− mice and ameliorated in Nrf2+/+ (but not Nrf2−/−) mice by pre-treatment with CDDO-Im, a structural analogue of CDDO-Me 3. The primary structural targets of cisplatin-induced kidney injury are the cortical tubules, and especially proximal tubule epithelial cells 25. Our IHC data demonstrates that Nrf2 activity is relatively high in the cortical tubules, in keeping with a report in healthy cynomolgus monkeys in which 28 day administration of CDDO-Me was shown to upregulate Nqo1 expression predominantly in these structures 26. Notably, Keap1 is also reported to be expressed at a much higher level in human renal cortex compared to medulla 27. These findings are consistent with the ability of Nrf2 and Nqo1 to directly protect against cisplatin nephrotoxicity in mice 3, 28, 29. Although further work is needed to define the contribution of other proteins and processes to the nephro-protective effects of Nrf2 in vivo, it is likely that the decreased expression of the gene battery reported here, and resulting lowered capacity to adapt to changes in local redox conditions via the provision of NADPH and glutathione, at least partly contributes to the enhanced sensitivity to renal insult associated with downregulation of Nrf2 signalling.
One third of the proteins that we recently showed to be sensitive to genetic inhibition or pharmacological induction of Nrf2 in the mouse liver 14 were found here to be similarly regulated by Nrf2 in the kidney, demonstrating that there is a degree of overlap in the regulatory roles of Nrf2 across different tissues. Indeed, consistent with our findings in the kidney, a recent report demonstrated that Nrf2 influences the provision of NADPH in the liver 30. However, several proteins found here to be sensitive to modulation of Nrf2 activity in the kidney were previously shown to be unaltered in the liver, and vice versa, under the same experimental conditions 14. We also noted that some Nrf2-regulated genes were downregulated to a greater degree in the kidney, compared to the liver, of Nrf2−/− mice, and vice versa. For example, Gstm1 protein levels were found to be 11.4 and 4.1 -fold lower in the kidneys and livers, respectively, of Nrf2−/− mice compared to wild type counterparts 14. Given that our IHC data indicates that Nrf2 activity is relatively high in the cortical tubules of the kidney, and that our transcriptomic and proteomic analyses have been conducted on whole tissue homogenates, it will be important to define the biological actions of Nrf2 in specific regions and cell types within the kidney, in order to better understand its roles in renal physiology and disease.
Chronic kidney disease in patients is characterised by a progressive decline in renal function, reduced metabolic capacity and an increased burden of oxidative stress 36, 37. Notably, several animal studies have provided evidence for a downregulation of the Nrf2 pathway during the pathogenesis of chronic kidney disease 22. Indeed, Vaziri and colleagues have observed a higher burden of oxidative stress and a lower level of expression of Nrf2 and its target genes, linked to an increase in the level of Keap1, in rat models of spontaneous focal glomerulosclerosis 38, surgical nephrectomy 39 and tubulo-interstitial nephropathy 40. The data reported here show that the Slc38a3 gene, which codes for the sodium-coupled neutral amino acid transporter 3 (Snat3), is expressed at a dramatically lower level in the kidneys of Nrf2−/− mice. Under physiological conditions, renal Snat3 protein expression is low (consistent with the absence of Slc38a3/Snat3 in our iTRAQ data sets) but is dramatically increased as part of the adaptive response to metabolic acidosis 34, 35. The dysregulation of Snat3 could render Nrf2−/− mice unable to adapt efficiently to metabolic acidosis, which is associated with multiple forms of kidney disease and causes neurological or cardiovascular complications in patients. We are currently testing this hypothesis.
CDDO-Me and its analogues have previously been shown to induce Nrf2 signalling and protect against experimental renal disease in animal models 3, 19, 31, 32. Here, CDDO-Me augmented the expression of numerous cytoprotective genes in the mouse kidney, although the pharmacodynamic impact of a single acute exposure to the compound was less pronounced at the protein level, even up to 72 h post-administration (Fig. S3). Consistent with this, the ability of CDDO-Me and its analogues to protect against experimental AKI provoked by ferric nitrilotriacetate 31, cisplatin 3, aristolochic acid 32 and ischaemia reperfusion 19 has only been demonstrated following repeated daily dosing of the triterpenoids, implying that chronic stimulation is necessary to provoke meaningful changes in the expression of Nrf2-regulated proteins in the kidney. As a result, further work is needed to define the effects of repeated administration of CDDO-Me on the renal Nrf2-regulated gene battery. In addition, Yates et al. have provided evidence for the differential induction of Nqo1 mRNA in various tissues of mice following a single 6 h exposure to CDDO-Me or its structural analogues 33. Such a phenomenon could be influenced by drug disposition, and it will therefore be important to determine whether intraperitoneal injection (as used here) and oral administration (as used clinically) of CDDO-Me and other small molecule inducers provoke different magnitudes of Nrf2 pathway response in the kidney, and indeed other organs.
CDDO-Me improves estimated glomerular filtration rate (eGFR) in both cancer and early-stage CKD patients 8, whilst structural analogues enhance eGFR 41 and renal function 42 in rats. Recent work has shown that selected Nrf2 target genes are upregulated in the glomeruli of Keap1 hypomorphic knockdown mice 43. However, the direct role of Nrf2 in the improved eGFR observed in patients and animals receiving CDDO-Me or related triterpenoids is currently unclear. Our microarray data reveals that none of the transcripts that are significantly altered by CDDO-Me in Nrf2+/+ mice are similarly altered in Nrf2−/− KO mice (see Table S3), demonstrating the relative specificity of the compound as an acute inducer of Nrf2 in the kidney. However, it is possible that during chronic exposure CDDO-Me alters other renal signalling pathways, or has indirect effects on kidney function through stimulation of Nrf2 activity in other organs, such as the liver. Therefore, further work is needed to understand the pharmacological mechanisms that underlie the beneficial effect of CDDO-Me on eGFR, in order to support the development of potent, specific and safe Nrf2 inducers that may represent promising candidates for the treatment of CKD, for which new drugs are urgently required.
METHODS
Animals and dosing
Non-fasted male Nrf2+/+ and Nrf2−/− mice (C57BL/6 background, generation and genotyping described previously 44, 45) of 10-12 weeks of age were utilised throughout the study, which was conducted according to the Animals (Scientific Procedures) Act 1986 and University of Liverpool local guidelines. Mice were housed at 19-23 °C on a 12 h light/dark cycle, and given free access to food and water. Mice were administered a single intraperitoneal dose of vehicle (DMSO, 100 μL/mouse) or CDDO-Me (3 mg/kg), and sacrificed 24 h later by exposure to a rising concentration of CO2 followed by cardiac puncture. The renal capsule and fat were removed from excised kidneys, which were then snap frozen, along with other organs, and stored at −80 °C.
Microarray analysis and bioinformatics
RNA was isolated from kidney tissue (n=5 per group) using the Direct-Zol RNA MiniPrep kit (Zymo Research, Germany) including on-column DNAse treatment. RNA concentration was assessed using a NanoDrop ND 1000 (Thermo Scientific, Switzerland) and RNA integrity was determined using a Bioanalyzer RNA 6000 Chip (Agilent, USA). DNAse-treated total RNA (270 ng) was subjected to cDNA target synthesis using the Ambion WT Expression kit (Life Technologies, Switzerland) following standard recommendations. Fragmentation and labelling of amplified cDNA were performed using the WT Terminal Labeling Kit (Affymetrix, UK) and a TProfessionnal TRIO PCR machine (Biometra, Germany). A volume of 85 μL cocktail (23.4 ng/μl labeled DNA) was loaded on Mouse Gene 2.0 ST arrays (Affymetrix) and hybridized for 17 h (45 °C, 60 rpm) in a hybridization oven 645 (Affymetrix). The arrays were washed and stained on a Fluidics Station 450 (Affymetrix) by using the Hybridization Wash and Stain kit (Affymetrix) under the FS450_0002 protocol. The GeneChips were scanned with an Affymetrix GeneChip Scanner 3000 7G. DAT images and CEL files of the microarrays were generated using Affymetrix GeneChip Command Control (version 4.0). CEL files were normalized according to RMA method 46 and data were log2-transformed. To select differentially expressed genes a two-way ANOVA model, using method of moments 47, was applied. The FDR-adjusted P-values were computed from raw P-values as described by Benjamini and Hochberg 48. Probes with transcript IDs but no associated gene assignment, gene symbol or RefSeq were excluded from bioinformatic analysis of the microarray data. To identify coding genes, probes that represented predicted genes, pseudogenes, uncharacterized cDNAs, Riken cDNAs and those without an identifier were excluded. Cross-referencing to the iTRAQ data set was facilitated by assignment of a DAVID identifier (http://david.abcc.ncifcrf.gov/conversion.jsp) to relevant coding genes.
iTRAQ analysis
Individual whole kidneys (n=6 per group) were homogenised in 0.5 M triethylammonium bicarbonate/0.1% SDS and subjected to a 1 h freeze-thaw cycle, followed by 3 × 10 sec bursts of sonication (3 μm amplitude). Samples were centrifuged (12,000 g, 10 min, 4 °C) and supernatants retained for iTRAQ and immunoblot analysis. iTRAQ labelling, mass spectrometry and data analysis were performed as described 14. Reported proteins were detected in at least 4 of 6 animals per treatment group. Differential expression (P≤0.05) was determined using the limma package within the R programming environment 49, enabling simultaneous comparisons between multiple treatments using design and contrast matrices via a linear regression model. Cross-referencing to the microarray data set was facilitated by assignment of a DAVID identifier to relevant proteins.
Ingenuity Pathway analysis and identification of ARE-like sequences
Ingenuity Pathway Analysis (IPA; www.ingenuity.com) of the microarray and iTRAQ data sets was performed to reveal biological pathways that were perturbed under the various conditions. Pathways represented by a single gene/protein were excluded for robustness. Regulatory Sequence Analysis Tools (RSAT) software (http://rsat.ulb.ac.be/rsat/) 50 was used to identify ARE sequences in the 5′-flanking regions upstream of putative Nrf2-regulated genes. 5′-flanking sequences (5000 bp upstream of the start codon) were retrieved directly from the ENSEMBL database from within the RSAT package. Promoter sequences were then interrogated for ARE or ARE-like sequences using a string-based analysis with the sub-programme ‘dna search’ available within RSAT. The search terms used were TMAnnRTGABnnnGCR and TGABnnnGC (where M = A/C, R = A/G, B = G/C/T, and N = any nucleotide). Consensus ARE sequences were taken from 51.
qPCR analysis
For relative quantification of selected genes, cDNA generated for microarray analysis of kidney tissue (n=5 per group) was analysed, using KAPA SYBR FAST qPCR reagent (Kapa Biosystems, USA) on a Rotor-Gene 3000A qPCR machine (Corbett Research, Australia), and normalized to Ppia. Gene-specific primers are detailed in Table S14.
Immunoblotting
Tissue homogenates (20 μg protein, n=6 per group) were separated by SDS-PAGE as previously described 11. The Nqo1 (ab2346), Gstm (ab53942), Entpd5 (ab92542), Cat (ab16731) and β-actin (ab6276) antibodies were from Abcam (UK). Immunoreactive band volumes were quantified using TotalLab 100 software (Nonlinear Dynamics, UK) and normalized to β-actin, which was probed as a loading control.
Quantification of NADPH and glutathione
Whole kidney tissue from Nrf2+/+ or Nrf2−/− mice dosed with DMSO or CDDO-Me (n=6 per group) was homogenised, and NADPH or glutathione levels were determined using NADP/NADPH-Glo or GSH-Glo assay kits (Promega), as per the manufacturer’s instructions, with the exception that NADPH and GSH were quantified after 5 and 2 min incubations, respectively, of the homogenates with the relevant detection reagents. NADPH was normalized to total protein content. Glutathione content was normalized to tissue weight.
Immunohistochemistry and image analysis
Whole kidneys from Nrf2+/+ or Nrf2−/− mice dosed with DMSO or CDDO-Me (n=5 per group) were fixed in 10 % neutral buffered formalin, then longitudinally trimmed and embedded in paraffin. Serial 4 μm-thick sections were cut and placed on polylysine-coated slides, rehydrated through serial passages in solutions at decreasing concentration of alcohol and moved to tris buffered saline Tween (TBST) solution, before quenching endogenous peroxidase activity through incubation in 0.3 % hydrogen peroxide. After blocking non-specific labelling using a 30 min incubation at room temperature with 20 % normal goat serum, the rabbit polyclonal anti-Nqo1 antibody (HPA007308, Sigma-Aldrich) was diluted 1:100 in TBST and applied overnight at 4 °C,. Negative control staining was performed by replacing the primary antibody with normal rabbit serum (X0902, Dako; see Fig. S4) or by omitting the primary antibody. Finally, after washing in TBST, anti-rabbit HRP EnVision™ polymer detection system (K4011, Dako) was applied for 30 min at room temperature. After 30 min incubation with appropriate secondary antibodies, slides were washed with TBST and 3,3′-diaminobenzidine was added as chromogen for 10 min. Slides were counterstained with Papanicolaou haematoxylin and mounted. For each experimental animal, a maximum of 10 non-overlapping microscopic fields of the cortex, including at least a glomerulus, were captured at 100x with a Nikon DS-5Mc camera mounted on a Nikon Eclipse 80i microscope, before automated processing with ImageJ software. After elaboration of an appropriate plugin for batch measure, colour channel splitting, application of colour threshold and measurement of the percentage of moderately to strongly stained areas within the microscopic fields was consecutively and automatically performed for all images and all experimental groups.
Supplementary Material
ACKNOWLEDGEMENTS
The authors acknowledge the technical assistance of Jane Hamlett and Julie Haigh with iTRAQ and IHC analyses, respectively. The authors also thank Bob van de Water and Daniel Antoine for constructive feedback on the manuscript.
Support: This work was supported by the Medical Research Council as part of the Centre for Drug Safety Science [grant number G0700654], the Wellcome Trust [grant number 094128/Z/10/Z], the Novartis Research Foundation, and the Swiss National Centre of Competence in Research (NCCR) “Kidney.CH”, Switzerland. A.L. was supported by the International Fellowship Programme on Integrative Kidney Physiology and Pathophysiology of the European Community's Seventh Framework Programme (FP7/2007-2013) under grant agreement number 246539.
Footnotes
DISCLOSURE
All the authors declare no competing interests.
REFERENCES
- 1.Nash K, Hafeez A, Hou S. Hospital-acquired renal insufficiency. Am J Kidney Dis. 2002;39:930–936. doi: 10.1053/ajkd.2002.32766. [DOI] [PubMed] [Google Scholar]
- 2.Choudhury D, Ahmed Z. Drug-associated renal dysfunction and injury. Nat Clin Pract Nephrol. 2006;2:80–91. doi: 10.1038/ncpneph0076. [DOI] [PubMed] [Google Scholar]
- 3.Aleksunes LM, Goedken MJ, Rockwell CE, et al. Transcriptional regulation of renal cytoprotective genes by Nrf2 and its potential use as a therapeutic target to mitigate cisplatin-induced nephrotoxicity. J Pharmacol Exp Ther. 2010;335:2–12. doi: 10.1124/jpet.110.170084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Umemura T, Sai K, Takagi A, et al. Oxidative DNA damage, lipid peroxidation and nephrotoxicity induced in the rat kidney after ferric nitrilotriacetate administration. Cancer Lett. 1990;54:95–100. doi: 10.1016/0304-3835(90)90097-h. [DOI] [PubMed] [Google Scholar]
- 5.Jiang T, Huang ZP, Lin YF, et al. The Protective Role of Nrf2 in Streptozotocin-Induced Diabetic Nephropathy. Diabetes. 2010;59:850–860. doi: 10.2337/db09-1342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bryan HK, Olayanju A, Goldring CE, et al. The Nrf2 cell defence pathway: Keap1-dependent and -independent mechanisms of regulation. Biochem Pharmacol. 2013;85:705–717. doi: 10.1016/j.bcp.2012.11.016. [DOI] [PubMed] [Google Scholar]
- 7.Copple IM. The Keap1-Nrf2 cell defense pathway--a promising therapeutic target? Adv Pharmacol. 2012;63:43–79. doi: 10.1016/B978-0-12-398339-8.00002-1. [DOI] [PubMed] [Google Scholar]
- 8.Pergola PE, Krauth M, Huff JW, et al. Effect of bardoxolone methyl on kidney function in patients with T2D and Stage 3b-4 CKD. Am J Nephrol. 2011;33:469–476. doi: 10.1159/000327599. [DOI] [PubMed] [Google Scholar]
- 9.de Zeeuw D, Akizawa T, Audhya P, et al. Bardoxolone methyl in type 2 diabetes and stage 4 chronic kidney disease. N Engl J Med. 2013;369:2492–2503. doi: 10.1056/NEJMoa1306033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chin MP, Reisman SA, Bakris GL, et al. Mechanisms contributing to adverse cardiovascular events in patients with type 2 diabetes mellitus and stage 4 chronic kidney disease treated with bardoxolone methyl. Am J Nephrol. 2014;39:499–508. doi: 10.1159/000362906. [DOI] [PubMed] [Google Scholar]
- 11.Kitteringham NR, Abdullah A, Walsh J, et al. Proteomic analysis of Nrf2 deficient transgenic mice reveals cellular defence and lipid metabolism as primary Nrf2-dependent pathways in the liver. J Proteomics. 2010;73:1612–1631. doi: 10.1016/j.jprot.2010.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Enomoto A, Itoh K, Nagayoshi E, et al. High sensitivity of Nrf2 knockout mice to acetaminophen hepatotoxicity associated with decreased expression of ARE-regulated drug metabolizing enzymes and antioxidant genes. Toxicol Sci. 2001;59:169–177. doi: 10.1093/toxsci/59.1.169. [DOI] [PubMed] [Google Scholar]
- 13.Liu J, Wu KC, Lu YF, et al. Nrf2 protection against liver injury produced by various hepatotoxicants. Oxid Med Cell Longev. 2013;2013:305861. doi: 10.1155/2013/305861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Walsh J, Jenkins RE, Wong M, et al. Identification and quantification of the basal and inducible Nrf2-dependent proteomes in mouse liver: Biochemical, pharmacological and toxicological implications. J Proteomics. 2014 doi: 10.1016/j.jprot.2014.05.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shelton LM, Park BK, Copple IM. Role of Nrf2 in protection against acute kidney injury. Kidney Int. 2013;84:1090–1095. doi: 10.1038/ki.2013.248. [DOI] [PubMed] [Google Scholar]
- 16.Leonard MO, Kieran NE, Howell K, et al. Reoxygenation-specific activation of the antioxidant transcription factor Nrf2 mediates cytoprotective gene expression in ischemia-reperfusion injury. FASEB J. 2006;20:2624–2626. doi: 10.1096/fj.06-5097fje. [DOI] [PubMed] [Google Scholar]
- 17.Liu M, Grigoryev DN, Crow MT, et al. Transcription factor Nrf2 is protective during ischemic and nephrotoxic acute kidney injury in mice. Kidney Int. 2009;76:277–285. doi: 10.1038/ki.2009.157. [DOI] [PubMed] [Google Scholar]
- 18.Yoon HY, Kang NI, Lee HK, et al. Sulforaphane protects kidneys against ischemia-reperfusion injury through induction of the Nrf2-dependent phase 2 enzyme. Biochem Pharmacol. 2008;75:2214–2223. doi: 10.1016/j.bcp.2008.02.029. [DOI] [PubMed] [Google Scholar]
- 19.Wu QQ, Wang Y, Senitko M, et al. Bardoxolone methyl (BARD) ameliorates ischemic AKI and increases expression of protective genes Nrf2, PPARgamma, and HO-1. Am J Physiol Renal Physiol. 2011;300:F1180–1192. doi: 10.1152/ajprenal.00353.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Elangovan S, Hsieh TC. Control of cellular redox status and upregulation of quinone reductase NQO1 via Nrf2 activation by alpha-lipoic acid in human leukemia HL-60 cells. Int J Oncol. 2008;33:833–838. [PubMed] [Google Scholar]
- 21.Malhotra D, Portales-Casamar E, Singh A, et al. Global mapping of binding sites for Nrf2 identifies novel targets in cell survival response through ChIP-Seq profiling and network analysis. Nucleic Acids Res. 2010;38:5718–5734. doi: 10.1093/nar/gkq212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ruiz S, Pergola PE, Zager RA, et al. Targeting the transcription factor Nrf2 to ameliorate oxidative stress and inflammation in chronic kidney disease. Kidney Int. 2013;83:1029–1041. doi: 10.1038/ki.2012.439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Choi BH, Kang KS, Kwak MK. Effect of redox modulating NRF2 activators on chronic kidney disease. Molecules. 2014;19:12727–12759. doi: 10.3390/molecules190812727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jeong HS, Ryoo IG, Kwak MK. Regulation of the expression of renal drug transporters in KEAP1-knockdown human tubular cells. Toxicol In Vitro. 2015;29:884–892. doi: 10.1016/j.tiv.2015.03.013. [DOI] [PubMed] [Google Scholar]
- 25.Ozkok A, Edelstein CL. Pathophysiology of cisplatin-induced acute kidney injury. Biomed Res Int. 2014;2014:967826. doi: 10.1155/2014/967826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Reisman SA, Chertow GM, Hebbar S, et al. Bardoxolone methyl decreases megalin and activates nrf2 in the kidney. J Am Soc Nephrol. 2012;23:1663–1673. doi: 10.1681/ASN.2012050457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Xu B, Yoshida Y, Zhang Y, et al. Two-dimensional electrophoretic profiling of normal human kidney: differential protein expression in glomerulus, cortex and medulla. J Electrophoresis. 2005;49:5–13. [Google Scholar]
- 28.Oh GS, Kim HJ, Choi JH, et al. Pharmacological activation of NQO1 increases NAD levels and attenuates cisplatin-mediated acute kidney injury in mice. Kidney Int. 2013 doi: 10.1038/ki.2013.330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gang GT, Kim YH, Noh JR, et al. Protective role of NAD(P)H:quinone oxidoreductase 1 (NQO1) in cisplatin-induced nephrotoxicity. Toxicol Lett. 2013;221:165–175. doi: 10.1016/j.toxlet.2013.06.239. [DOI] [PubMed] [Google Scholar]
- 30.Wu KC, Cui JY, Klaassen CD. Beneficial Role of Nrf2 in Regulating NADPH Generation and Consumption. Toxicological Sciences. 2011;123:590–600. doi: 10.1093/toxsci/kfr183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tanaka Y, Aleksunes LM, Goedken MJ, et al. Coordinated induction of Nrf2 target genes protects against iron nitrilotriacetate (FeNTA)-induced nephrotoxicity. Toxicol Appl Pharmacol. 2008;231:364–373. doi: 10.1016/j.taap.2008.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Wu J, Liu X, Fan J, et al. Bardoxolone methyl (BARD) ameliorates aristolochic acid (AA)-induced acute kidney injury through Nrf2 pathway. Toxicology. 2014;318:22–31. doi: 10.1016/j.tox.2014.01.008. [DOI] [PubMed] [Google Scholar]
- 33.Yates MS, Tauchi M, Katsuoka F, et al. Pharmacodynamic characterization of chemopreventive triterpenoids as exceptionally potent inducers of Nrf2-regulated genes. Mol Cancer Ther. 2007;6:154–162. doi: 10.1158/1535-7163.MCT-06-0516. [DOI] [PubMed] [Google Scholar]
- 34.Nowik M, Lecca MR, Velic A, et al. Genome-wide gene expression profiling reveals renal genes regulated during metabolic acidosis. Physiol Genomics. 2008;32:322–334. doi: 10.1152/physiolgenomics.00160.2007. [DOI] [PubMed] [Google Scholar]
- 35.Busque SM, Stange G, Wagner CA. Dysregulation of the glutamine transporter Slc38a3 (SNAT3) and ammoniagenic enzymes in obese, glucose-intolerant mice. Cell Physiol Biochem. 2014;34:575–589. doi: 10.1159/000363024. [DOI] [PubMed] [Google Scholar]
- 36.Levey AS, Eckardt KU, Tsukamoto Y, et al. Definition and classification of chronic kidney disease: a position statement from Kidney Disease: Improving Global Outcomes (KDIGO) Kidney Int. 2005;67:2089–2100. doi: 10.1111/j.1523-1755.2005.00365.x. [DOI] [PubMed] [Google Scholar]
- 37.Small DM, Coombes JS, Bennett N, et al. Oxidative stress, anti-oxidant therapies and chronic kidney disease. Nephrology (Carlton) 2012;17:311–321. doi: 10.1111/j.1440-1797.2012.01572.x. [DOI] [PubMed] [Google Scholar]
- 38.Kim HJ, Sato T, Rodriguez-Iturbe B, et al. Role of intrarenal angiotensin system activation, oxidative stress, inflammation, and impaired nuclear factor-erythroid-2-related factor 2 activity in the progression of focal glomerulosclerosis. J Pharmacol Exp Ther. 2011;337:583–590. doi: 10.1124/jpet.110.175828. [DOI] [PubMed] [Google Scholar]
- 39.Kim HJ, Vaziri ND. Contribution of impaired Nrf2-Keap1 pathway to oxidative stress and inflammation in chronic renal failure. Am J Physiol Renal Physiol. 2010;298:F662–671. doi: 10.1152/ajprenal.00421.2009. [DOI] [PubMed] [Google Scholar]
- 40.Aminzadeh MA, Nicholas SB, Norris KC, et al. Role of impaired Nrf2 activation in the pathogenesis of oxidative stress and inflammation in chronic tubulo-interstitial nephropathy. Nephrol Dial Transplant. 2013;28:2038–2045. doi: 10.1093/ndt/gft022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ding Y, Stidham RD, Bumeister R, et al. The synthetic triterpenoid, RTA 405, increases the glomerular filtration rate and reduces angiotensin II-induced contraction of glomerular mesangial cells. Kidney Int. 2013;83:845–854. doi: 10.1038/ki.2012.393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Vaziri ND, Liu S, Farzaneh SH, et al. Dose-dependent deleterious and salutary actions of Nrf2 inducer, dh404, in chronic kidney disease. Free Radic Biol Med. 2015 doi: 10.1016/j.freeradbiomed.2015.04.022. [DOI] [PubMed] [Google Scholar]
- 43.Miyazaki Y, Shimizu A, Pastan I, et al. Keap1 inhibition attenuates glomerulosclerosis. Nephrol Dial Transplant. 2014;29:783–791. doi: 10.1093/ndt/gfu002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Itoh K, Chiba T, Takahashi S, et al. An Nrf2 small Maf heterodimer mediates the induction of phase II detoxifying enzyme genes through antioxidant response elements. Biochem Biophys Res Commun. 1997;236:313–322. doi: 10.1006/bbrc.1997.6943. [DOI] [PubMed] [Google Scholar]
- 45.McMahon M, Itoh K, Yamamoto M, et al. The Cap’n’Collar basic leucine zipper transcription factor Nrf2 (NF-E2 p45-related factor 2) controls both constitutive and inducible expression of intestinal detoxification and glutathione biosynthetic enzymes. Cancer Res. 2001;61:3299–3307. [PubMed] [Google Scholar]
- 46.Irizarry RA, Hobbs B, Collin F, et al. Exploration, normalization, and summaries of high density oligonucleotide array probe level data. Biostatistics. 2003;4:249–264. doi: 10.1093/biostatistics/4.2.249. [DOI] [PubMed] [Google Scholar]
- 47.Eisenhart C. The assumptions underlying the analysis of variance. Biometrics. 1947;3:1–21. [PubMed] [Google Scholar]
- 48.Benjamini Y, Hochberg Y. Controlling the False Discovery Rate: A Practical and Powerful Approach to. Multiple Testing. Journal of Royal Statistical Society, Series B. 1995;57:289–300. [Google Scholar]
- 49.R-Development-Core-Team . R: A language and environment for statistical computing. R Foundation for Statistical Computing; 2005. [Google Scholar]
- 50.van Helden J. Regulatory sequence analysis tools. Nucleic Acids Res. 2003;31:3593–3596. doi: 10.1093/nar/gkg567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hayes JD, McMahon M, Chowdhry S, et al. Cancer chemoprevention mechanisms mediated through the Keap1-Nrf2 pathway. Antioxid Redox Signal. 2010;13:1713–1748. doi: 10.1089/ars.2010.3221. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.