Abstract
Background:
Obsessive-compulsive disorder (OCD) is a heterogeneous condition with a few major symptom dimensions. These symptom dimensions are thought to have unique clinical and neurobiological correlates. There seems to be a specific relation between OCD symptom dimensions and obsessive beliefs, but the findings are not consistent across studies. There is also a paucity of literature from culturally diverse settings. One of the reasons for the varied findings could be due to the method employed in measuring OCD symptoms.
Materials and Methods:
In this study, we examined the relation between symptom dimensions and obsessive beliefs using the Dimensional Yale-Brown Obsessive-Compulsive Scale and the Obsessive Beliefs Questionnaire respectively in 75 patients with Diagnostic and Statistical Manual of Mental Disorders-Fourth Edition OCD.
Results:
Perfectionism predicted both aggressive and symmetry dimensions whereas responsibility beliefs predicted sexual and religious dimensions.
Conclusions:
The findings suggest that certain obsessive beliefs predicted certain OCD symptom dimensions, but results are not entirely consistent with the published literature suggesting the possibility of cross-cultural variations. That the symptom dimensions have unique belief domains support the argument that symptom dimensions could be targeted to reduce the heterogeneity in etiological and treatment studies of OCD. Therapeutic interventions may have to aim at modifying unique belief domains underlying certain symptom dimensions rather than having generic cognitive-behavioral strategies.
Keywords: Obsessive beliefs, obsessive-compulsive disorder, symptom dimensions
INTRODUCTION
Obsessive-compulsive disorder (OCD) is a heterogeneous condition characterized by a wide range of symptoms that can be distilled down to a smaller number of unique symptom dimensions.[1] This heterogeneity can reduce our ability to understand not only its genetic and neurobiological basis but also in understanding the natural course and treatment response.[1] A meta-analysis of 21 studies involving over 5000 subjects showed there are four major symptom dimensions in OCD that include symmetry (symmetry obsessions, repeating, ordering, and counting compulsions), forbidden thoughts (aggression, sexual, religious, and somatic obsessions with checking compulsions), cleaning (contamination fears and washing and cleaning compulsions), and hoarding.[2] These four symptom dimensions explained a large proportion of the heterogeneity in the clinical symptoms of OCD. Emerging evidence suggest that the symptom dimensions of OCD have unique patterns of comorbidity,[3,4] heritability,[5,6,7] neuropsychological profile,[8,9] neuroanatomical correlates[10] and possibly a differential course,[11,12] and treatment response.[13,14]
There is also growing evidence that OCD symptom dimensions may have unique dysfunctional beliefs.[15,16,17] The Obsessive-Compulsive Cognitions Working Group developed an instrument to assess beliefs in OCD, the Obsessive Beliefs Questionnaire (OBQ).[18] Based on this instrument, several studies have examined the beliefs in relation to OCD symptom dimensions. Washing dimension is associated with overestimation of threat[15,16,19,20,21,22] and inflated responsibility;[15,16,20,21,22] forbidden thoughts with the over importance and need to control thoughts;[21,22,23,24,25,26] and symmetry with need for perfectionism and certainty.[17,22,24] However, findings are not consistent across studies. For example, checking is associated with exaggerated threat perception and inflated responsibility in nonclinical samples,[26,27] but with the need for perfectionism and certainty in OCD patients.[20,25] One study did not find any association between checking and any obsession beliefs.[21] Similarly, washing and forbidden thoughts have not always been associated with threat perception/inflated responsibility[25] and over importance/need to control thoughts,[20] respectively.
The reasons for discrepant findings could be related to the method employed to assess symptom dimensions. Most studies have employed instruments that measure only the presence or absence of individual symptoms and not the severity of the dimensions. The only exception is the study by Wheaton et al. which employed the Dimensional Obsessive-Compulsive Scale.[22] In this study, we examined the relationship between obsessive beliefs and symptom dimensions using the Dimensional Yale-Brown Obsessive-Compulsive scale (D-YBOCS).[28] This scale summarizes complex OCD phenotype into a few consistent and temporally stable symptom dimensions. The D-YBOCS assesses OCD symptoms within seven distinct dimensions that combine thematically related obsessions and compulsions. The instrument allows classifying the same type of ritual/compulsion under different symptom dimensions based on the functionality of the ritual rather than just the form of it.
On the basis of existing literature, we hypothesized that the harm/aggression and sexual/religious dimensions would be associated with “over importance” and “need to control” thoughts, the contamination dimension with “exaggerated threat perception” and “inflated responsibility” and symmetry with the need for “perfectionism and certainty.”
MATERIALS AND METHODS
Participants
The sample of the present study consisted of 75 English speaking patients with Diagnostic and Statistical Manual of Mental Disorders-Fourth Edition diagnosis of primary OCD.[29] Patients with OCD were selected from the OCD Clinic, the Behavior Medicine Unit, and the inpatient services of the National Institute of Mental Health and Neurosciences, Bengaluru from April 2010 to January 2011. Among the 98 suitable patients, 23 could not be recruited (10 did not come for the appointment, 8 patients did not meet the severity criterion, 3 patients could not comprehend English, and 2 had comorbid bipolar disorder). All patients had a total score of ≥16 on the Yale-Brown Obsessive-Compulsive Severity Scale (Y-BOCS).[30] The Ethics Committee of the Institute approved the study and all the patients provided written informed consent to participate in the study.
Assessments
The MINI International Neuropsychiatric Interview was administered to confirm the diagnosis of OCD and other comorbid disorders.[31] Illness severity was assessed using the Y-BOCS. Symptom dimensions were measured using the D-YBOCS.[28] These assessments were performed by the first author who was trained in administering the instruments by the senior author (YCJR). The senior author/consultants of the OCD clinic confirmed the diagnosis of OCD after independent clinical examination and review of the information obtained. Subsequently, the patients completed the OBQ-87.[18]
In the D-YBOCS, obsessions and compulsions are divided into seven different symptom dimensions: Contamination/cleaning, symmetry/ordering/arranging/counting, sexual/religious, aggression, somatic, hoarding/collecting, and miscellaneous obsessions and compulsions. Severity for each dimension is measured on three ordinal scales with six anchor points that focus on symptom frequency (0-5), the amount of distress they cause (0-5) and the degree to which they interfere with functioning (0-5) during the previous week. Global symptom severity is estimated using the above three ordinal scales (0-15). The overall impairment due to symptoms is assessed on a scale of “none” (0 points) to “severe” (15 points). The total global score is obtained by combining the sum of the global symptom severity scores for frequency, distress and interference (0-15) and the overall impairment score (0-15), yielding a maximum total global severity score of 30. A study by Rosario-Campos et al. showed high correlations between the self-report and expert rating of severity, suggesting that either version could be used alone.[28] In our study, we have used the clinician-administered version of the instrument.
The OBQ-87[18] is an 87 items self-administered questionnaire entailing six belief domains:
-
(1)
Tolerance for uncertainty,
-
(2)
Threat estimation,
-
(3)
Control of thoughts,
-
(4)
Importance of thoughts,
-
(5)
Responsibility, and
-
(6)
Perfectionism. Each item is rated on a seven-point scale.
Statistical analysis
We performed linear regression analyses (backward) to identify the predictors of the individual D-YBOCS symptom dimensions. Six individual belief dimensions of OBQ were entered into regression analyses. Comorbid anxiety (social phobia, generalized anxiety disorder, social phobia, and panic disorder) and depressive disorders (major depression and dysthymia) were also entered into the regression analyses to eliminate the confounding effect of these comorbid disorders. We employed a conservative P ≤ 0.01 in view of a series of regression analyses.
RESULTS
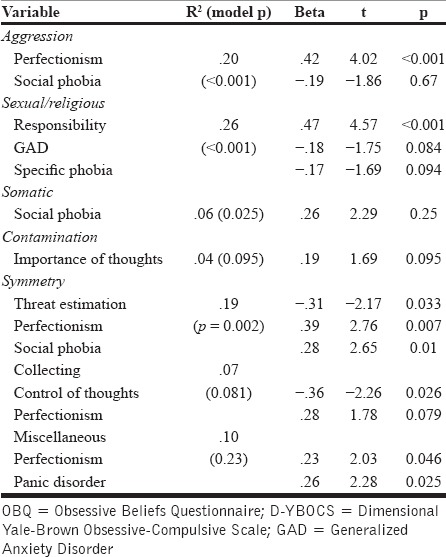
Demographic and clinical characteristics are shown in Table 1. As can be seen in Table 2, perfectionism predicted aggression dimension and responsibility predicted the sexual/religious dimension. Similarly, perfectionism, threat estimation and social phobia predicted symmetry dimension. The OBQ failed to predict other symptom dimensions.
Table 1.
Demographic and clinical characteristics of the sample (n = 75)
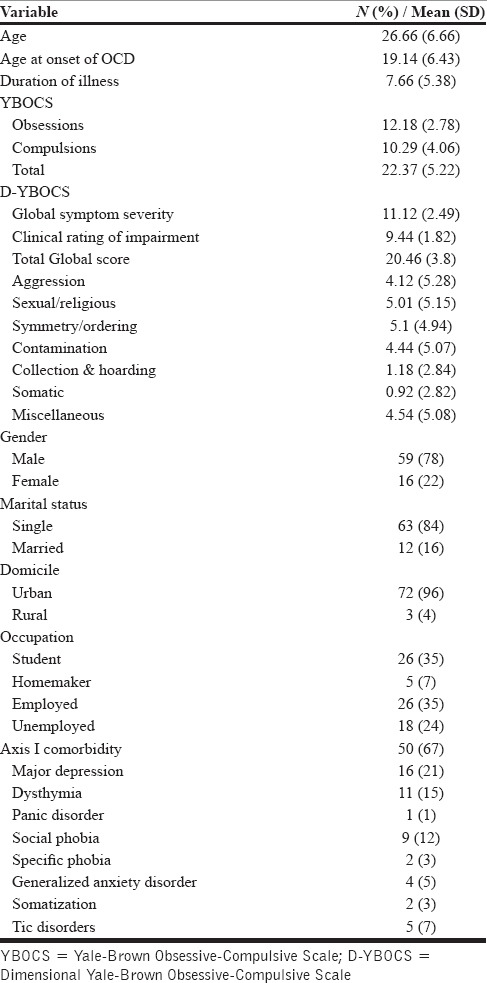
Table 2.
Regression analyses showing OBQ belief domains predicting D-YBOCS symptom dimensions
DISCUSSION
The present study aimed to examine the relation between dysfunctional beliefs and OCD symptom dimensions. Perfectionism predicted both aggressive and symmetry dimensions whereas responsibility beliefs predicted sexual and religious dimensions.
Study findings lend support to the notion that symptom dimensions may have unique dysfunctional beliefs. However, our findings do not fully support the hypothesis generated by us based on the results of previous studies. We had hypothesized that the harm/aggression and the sexual/religious dimensions would be associated with the over importance and need to control thoughts; the contamination dimension with the exaggerated threat perception and inflated responsibility; and the symmetry with the need for perfectionism and certainty.
Exaggerated threat perception[15,16,19,20,21,22] and inflated responsibility[15,16,20,21,22] is typically though not always associated with contamination fears and washing/cleaning dimension.[25] Curiously, in this study, contamination dimension was not predicted by any dysfunctional belief. On the other hand, inflated responsibility predicted sexual/religious dimension, a finding not consistent with the findings of previous studies, which found an association with over importance and need to control thoughts.[21,22,23,24,25,26] Need for perfectionism predicted both symmetry and aggressive dimensions. Association between aggressive dimension and perfectionism is somewhat consistent with studies involving OCD patients with checking which is commonly the result of aggression and harm related obsessions,[20,25] but not with nonclinical samples.[26,27]
The reasons for discrepant findings could be culturally determined. It is possible that the association between certain dysfunctional beliefs and symptom dimensions are influenced by cultural factors. For example, typical symptoms of contamination dimension are often the fear of contracting or spreading illness which may understandably lead to exaggerated threat perception and an inflated sense of responsibility. Though systematic data is not available pertaining to types of contamination obsessions that are common in the Indian population, in our clinical experience, fear of contracting and even so spreading illness to others is rather less common. Our patients often report contamination with dust, sticky substances and other such environmental agents rather than infective agents causing perhaps more of disgust than feeling responsible for contracting or spreading illness.
Aggression/harm related obsessions (and checking) have been associated with exaggerated threat perception and an inflated sense of responsibility.[22] In our study, aggressive dimension was associated with perfectionism again raising the possibility of cultural influences because in Indian samples checking is not typically associated with harm related obsessions, but with pathological doubts.[12,32] Sexual and religious obsessions have been associated with importance and need to control thoughts,[22] but in this study, they were associated with an inflated sense of responsibility. People who suffer from sexual and blasphemy related obsessions are often concerned that they may act out on their urges/thoughts; therefore an inflated sense of responsibility to prevent awful consequences is understandable.
That our findings are somewhat different compared to those of previously published studies, point toward potential cross-cultural variations, but other factors may have also played a role. The OBQ measures a set of dysfunctional beliefs which are well supported by empirical research, but it may not be an exhaustive measure of all the cognitive phenomena involved in OCD.[22] We did not examine other constructs such as disgust sensitivity,[33] “not just right” experiences[34] and contamination specific cognitions.[35]
Our findings have clinical and research implications. From a clinical perspective, it is possible to develop specific treatment strategies to deal with unique core beliefs underlying the individual symptom dimensions rather than having generic cognitive-behavioral strategies. For example, in dealing with symmetry and exactness, focus of treatment may have to be on cognitions related to perfectionism. However, it is yet to be established that targeting specific beliefs system would lead to improved outcomes. From a theoretical perspective, that the symptom dimensions have unique belief domains support the argument that symptom dimensions could be targeted to reduce the heterogeneity in etiological and treatment studies of OCD.[1,10,13]
Certain limitations of the study have to be considered in interpreting the findings. The sample was drawn from a tertiary care psychiatric hospital with specialized services for OCD. Moreover, sample size is small and included mainly English speaking patients. Therefore, generalizability may be limited. Cross-sectional design of the study precludes drawing inferences on causality. Though the tools used for the present study have been widely used in clinical and research setting, psychometric properties in an Indian population are yet to be established. A study on a much larger representative sample with measurement of belief domains in Indian languages is warranted. Finally, it is also interesting to examine if the belief domains can serve as cognitive endophenotypes just as neuropsychological and neuroanatomical correlates.
CONCLUSION
Study findings demonstrate that symptom dimensions may have unique underlying dysfunctional beliefs. However, our findings differed from published literature in that no belief predicted contamination dimension and “over importance” and “need to control thoughts” failed to predict harm/aggression and sexual/religious dimensions. Our findings point toward potential cross-cultural variations that need to be systematically studied in larger samples with the inclusion of additional constructs such as disgust sensitivity, “not just right” experiences and contamination specific cognitions.
ACKNOWLEDGMENT
The study was done as part of the M Phil (clinical psychology) dissertation of the first author; the study was non-funded.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Mataix-Cols D, Rosario-Campos MC, Leckman JF. A multidimensional model of obsessive-compulsive disorder. Am J Psychiatry. 2005;162:228–38. doi: 10.1176/appi.ajp.162.2.228. [DOI] [PubMed] [Google Scholar]
- 2.Bloch MH, Landeros-Weisenberger A, Rosario MC, Pittenger C, Leckman JF. Meta-analysis of the symptom structure of obsessive-compulsive disorder. Am J Psychiatry. 2008;165:1532–42. doi: 10.1176/appi.ajp.2008.08020320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hasler G, LaSalle-Ricci VH, Ronquillo JG, Crawley SA, Cochran LW, Kazuba D, et al. Obsessive-compulsive disorder symptom dimensions show specific relationships to psychiatric comorbidity. Psychiatry Res. 2005;135:121–32. doi: 10.1016/j.psychres.2005.03.003. [DOI] [PubMed] [Google Scholar]
- 4.Prabhu L, Cherian AV, Viswanath B, Kandavel T, Bada Math S, Janardhan Reddy YC. Symptom dimensions in OCD and their association with clinical characteristics and comorbid disorders. J Obsessive Compuls Relat Disord. 2012;2:14–21. [Google Scholar]
- 5.Leckman JF, Pauls DL, Zhang H, Rosario-Campos MC, Katsovich L, Kidd KK, et al. Obsessive-compulsive symptom dimensions in affected sibling pairs diagnosed with Gilles de la Tourette syndrome. Am J Med Genet B Neuropsychiatr Genet. 2003;116B:60–8. doi: 10.1002/ajmg.b.10001. [DOI] [PubMed] [Google Scholar]
- 6.Hasler G, Kazuba D, Murphy DL. Factor analysis of obsessive-compulsive disorder YBOCS-SC symptoms and association with 5-HTTLPR SERT polymorphism. Am J Med Genet B Neuropsychiatr Genet. 2006;141B:403–8. doi: 10.1002/ajmg.b.30309. [DOI] [PubMed] [Google Scholar]
- 7.Katerberg H, Delucchi KL, Stewart SE, Lochner C, Denys DA, Stack DE, et al. Symptom dimensions in OCD: Item-level factor analysis and heritability estimates. Behav Genet. 2010;40:505–17. doi: 10.1007/s10519-010-9339-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hashimoto N, Nakaaki S, Omori IM, Fujioi J, Noguchi Y, Murata Y, et al. Distinct neuropsychological profiles of three major symptom dimensions in obsessive-compulsive disorder. Psychiatry Res. 2011;187:166–73. doi: 10.1016/j.psychres.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 9.Lawrence NS, Wooderson S, Mataix-Cols D, David R, Speckens A, Phillips ML. Decision making and set shifting impairments are associated with distinct symptom dimensions in obsessive-compulsive disorder. Neuropsychology. 2006;20:409–19. doi: 10.1037/0894-4105.20.4.409. [DOI] [PubMed] [Google Scholar]
- 10.Mataix-Cols D, Wooderson S, Lawrence N, Brammer MJ, Speckens A, Phillips ML. Distinct neural correlates of washing, checking, and hoarding symptom dimensions in obsessive-compulsive disorder. Arch Gen Psychiatry. 2004;61:564–76. doi: 10.1001/archpsyc.61.6.564. [DOI] [PubMed] [Google Scholar]
- 11.Eisen JL, Sibrava NJ, Boisseau CL, Mancebo MC, Stout RL, Pinto A, et al. Five-year course of obsessive-compulsive disorder: Predictors of remission and relapse. J Clin Psychiatry. 2013;74:233–9. doi: 10.4088/JCP.12m07657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cherian AV, Math SB, Kandavel T, Reddy YC. A 5-year prospective follow-up study of patients with obsessive-compulsive disorder treated with serotonin reuptake inhibitors. J Affect Disord. 2014;152-154:387–94. doi: 10.1016/j.jad.2013.09.042. [DOI] [PubMed] [Google Scholar]
- 13.Mataix-Cols D, Rauch SL, Manzo PA, Jenike MA, Baer L. Use of factor-analyzed symptom dimensions to predict outcome with serotonin reuptake inhibitors and placebo in the treatment of obsessive-compulsive disorder. Am J Psychiatry. 1999;156:1409–16. doi: 10.1176/ajp.156.9.1409. [DOI] [PubMed] [Google Scholar]
- 14.Mataix-Cols D, Rauch SL, Baer L, Eisen JL, Shera DM, Goodman WK, et al. Symptom stability in adult obsessive-compulsive disorder: Data from a naturalistic two-year follow-up study. Am J Psychiatry. 2002;159:263–8. doi: 10.1176/appi.ajp.159.2.263. [DOI] [PubMed] [Google Scholar]
- 15.Rachman S. A cognitive theory of compulsive checking. Behav Res Ther. 2002;40:625–39. doi: 10.1016/s0005-7967(01)00028-6. [DOI] [PubMed] [Google Scholar]
- 16.Rachman S. Fear of contamination. Behav Res Ther. 2004;42:1227–55. doi: 10.1016/j.brat.2003.10.009. [DOI] [PubMed] [Google Scholar]
- 17.Summerfeldt LJ. Ordering, incompleteness and arranging. In: Abramowitz JS, McKay D, Taylor S, editors. Clinical Handbook of Obsessive-Compulsive and Related Problems. Baltimore: Johns Hopkins University Press; 2008. pp. 44–60. [Google Scholar]
- 18.Obsessive Compulsive Cognitions Working Group. Development and initial validation of the obsessive beliefs questionnaire and the interpretation of intrusions inventory: Part I. Behav Res Ther. 2001;39:987–1006. doi: 10.1016/s0005-7967(00)00085-1. [DOI] [PubMed] [Google Scholar]
- 19.Jones MK, Menzies RG. The cognitive mediation of obsessive-compulsive hand washing. Behav Res Ther. 1997;35:843–50. doi: 10.1016/s0005-7967(97)00035-1. [DOI] [PubMed] [Google Scholar]
- 20.Obsessive Compulsive Cognitions Working Group. Psychometric validation of the obsessive belief questionnaire and interpretation of intrusions inventory - Part 2: Factor analyses and testing of a brief version. Behav Res Ther. 2005;43:1527–42. doi: 10.1016/j.brat.2004.07.010. [DOI] [PubMed] [Google Scholar]
- 21.Tolin DF, Brady RE, Hannan S. Obsessional beliefs and symptoms of obsessive-compulsive disorder in a clinical sample. J Psychopathol Behav Assess. 2008;30:31–42. [Google Scholar]
- 22.Wheaton MG, Abramowitz JS, Berman NC, Riemann BC, Hale LR. The relationship between obsessive beliefs and symptom dimensions in obsessive-compulsive disorder. Behav Res Ther. 2010;48:949–54. doi: 10.1016/j.brat.2010.05.027. [DOI] [PubMed] [Google Scholar]
- 23.Rachman S. A cognitive theory of obsessions. Behav Res Ther. 1997;35:793–802. doi: 10.1016/s0005-7967(97)00040-5. [DOI] [PubMed] [Google Scholar]
- 24.Purdon C. Unacceptable obsessional thoughts and covert rituals. In: Abramowitz JS, McKay D, Taylor S, editors. Clinical Handbook of Obsessive-Compulsive and Related Problems. Baltimore: Johns Hopkins University Press; 2008. pp. 61–75. [Google Scholar]
- 25.Julien D, O’Connor KP, Aardema F, Todorov C. The specificity of belief domains in obsessive-compulsive symptom subtypes. Pers Individ Dif. 2006;41:1205–16. [Google Scholar]
- 26.Tolin DF, Woods CM, Abramowitz JS. Relationship between obsessive beliefs and obsessive-compulsive symptoms. Cognit Ther Res. 2003;27:657–69. [Google Scholar]
- 27.Myers SG, Fisher PL, Wells A. Belief domains of the Obsessive Beliefs Questionnaire-44 (OBQ-44) and their specific relationship with obsessive-compulsive symptoms. J Anxiety Disord. 2008;22:475–84. doi: 10.1016/j.janxdis.2007.03.012. [DOI] [PubMed] [Google Scholar]
- 28.Rosario-Campos MC, Miguel EC, Quatrano S, Chacon P, Ferrao Y, Findley D, et al. The dimensional Yale-brown obsessive-compulsive scale (DY-BOCS): An instrument for assessing obsessive-compulsive symptom dimensions. Mol Psychiatry. 2006;11:495–504. doi: 10.1038/sj.mp.4001798. [DOI] [PubMed] [Google Scholar]
- 29.Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: Americal Psychiatric Association; 2000. American Psychiatric Association. [Google Scholar]
- 30.Goodman WK, Price LH, Rasmussen SA, Mazure C, Fleischmann RL, Hill CL, et al. The Yale-brown obsessive compulsive scale. I. Development, use, and reliability. Arch Gen Psychiatry. 1989;46:1006–11. doi: 10.1001/archpsyc.1989.01810110048007. [DOI] [PubMed] [Google Scholar]
- 31.Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59(Suppl 20):22–33. [PubMed] [Google Scholar]
- 32.Cherian AV, Narayanaswamy JC, Srinivasaraju R, Viswanath B, Math SB, Kandavel T, et al. Does insight have specific correlation with symptom dimensions in OCD? J Affect Disord. 2012;138:352–9. doi: 10.1016/j.jad.2012.01.017. [DOI] [PubMed] [Google Scholar]
- 33.Olatunji BO, Sawchuk CN, Lohr JM, de Jong PJ. Disgust domains in the prediction of contamination fear. Behav Res Ther. 2004;42:93–104. doi: 10.1016/s0005-7967(03)00102-5. [DOI] [PubMed] [Google Scholar]
- 34.Coles ME, Frost RO, Heimberg RG, Rhéaume J. “Not just right experiences”: Perfectionism, obsessive-compulsive features and general psychopathology. Behav Res Ther. 2003;41:681–700. doi: 10.1016/s0005-7967(02)00044-x. [DOI] [PubMed] [Google Scholar]
- 35.Cisler JM, Brady RE, Olatunji BO, Lohr JM. Disgust and obsessive beliefs in contamination-related OCD. Cognit Ther Res. 2010;34:439–48. doi: 10.1007/s10608-009-9253-y. [DOI] [PMC free article] [PubMed] [Google Scholar]


