Abstract
Background and Aims:
Inhalation anesthesia with sevoflurane may be enhanced by several drugs or techniques. The aim of the present study was to investigate the effect of nitrous oxide (N2O) pretreatment on the speed of anesthesia induction with sevoflurane.
Material and Methods:
Eighty patients scheduled for hysteroscopy under general anesthesia were randomly assigned to inhale for 10 min before induction 50% N2O in oxygen or air via a facemask. Anesthesia was induced with 7-8% sevoflurane in oxygen via a facemask. Bispectral index (BIS), end-tidal carbon dioxide (EtCO2) tidal volume, respiratory rate, oxygen saturation (SpO2), and heart rate were recorded every minute during the 10 min pretreatment periods and every 30 s during the first 300 s of induction with sevoflurane. During induction of anesthesia inspired and end-tidal sevoflurane concentrations were also recorded.
Results:
During the 10 min of inspired 50% N2O or air BIS, EtCO2, tidal volume, respiratory rate and heart rate values did not differ between the two groups except for the SpO2, which was higher in the N2O group (P < 0.001). During induction of anesthesia the N2O group exhibited lower BIS values (P = 0.001), being significant at 60-150 s (P < 0.001, P < 0.001, P = 0.002, P = 0.014) as well as at 270 s (P = 0.004). EtCO2 and tidal volume were consistently lower in the N2O group (P = 0.001, P = 0.041 respectively) and respiratory rate was higher (P = 0.007).
Conclusion:
Our results show that pretreatment of the patients with 50% N2O for 10 min enhances the speed of induction with sevoflurane as assessed by the BIS monitoring.
Keywords: Bispectral index, inhalation induction, nitrous oxide, sevoflurane
Introduction
Sevoflurane has a low blood/gas partition coefficient and does not irritate the airways. These properties render sevoflurane suitable for inhalation induction of anesthesia. Inhalation induction should provide rapid loss of consciousness to ensure patient's comfort and satisfaction and to avoid adverse effects such as excitations, breath holding, coughing and/or laryngospasm. Several adjuvants and techniques have been proposed to ensure a rapid induction of anesthesia with sevoflurane, such as intravenous (IV) midazolam,[1] clonidine,[2] fentanyl,[3] breathing different gas flows,[4] or ventilation with larger tidal volumes.[5]
The effect of nitrous oxide (N2O) when added to the inhalation of sevoflurane in oxygen has been controversial.[2,6,7,8] N2O added to oxygen was reported to make shorter the induction time with sevoflurane, an effect similar to that produced by clonidine.[2] These results are not consistent with the results obtained from other studies, which conclude that the addition of N2O to the sevoflurane/oxygen mixture is not advantageous regarding the speed of induction of anesthesia.[6,7,8] In contrast, results from previous studies point out that the addition of N2O to the sevoflurane/oxygen mixture may be associated with more, though minor, excitatory phenomena.[7]
Our hypothesis was that the speed of inhalation induction with sevoflurane may benefit from the pretreatment with N2O, and subsequent volume contraction[9] before sevoflurane administration. The aim of the present study was to investigate the effect of pretreatment with 50% N2O in oxygen on the speed of inhalation induction of anesthesia with sevoflurane in women undergoing minor gynecological procedures.
Material and Methods
The study was approved by the Institutional Review Board (N-79/04-04-06). Eighty patients American Society of Anesthesiology physical status I or II scheduled for hysteroscopy under general anesthesia, who accepted an inhalation induction with no premedication, gave their written informed consent to participate in the study protocol. The study was conducted between October 2006 and March 2009. Patients with body weight exceeding the ideal body weight by 25%, with central nervous system disease, respiratory disease, hyper-or hypothyroidism, intake of sedatives, hypnotics, and antidepressants were excluded from the study before randomization. Difficult airway was not an exclusion criterion.
Patients were randomly allocated to the air (FiO2 = 0.21) or N2O (N2O/O2:50/50, FiO2 = 0.5) group. Randomization was done by means of odd and even numbers retrieved from a computer-generated table (http://www.randomizer.org) corresponding to the N2O and to the air group respectively. The pretreatment gas was administered via N2O-oxygen flow meters or an air flow meter connected to the wall pipelines, all covered by drapes so the investigators were blinded to the gas administered. Group allocation to intervention was done by an independent anesthesiologist not participating in the study who arranged the gases before induction (air or N2O/O2), covered the flow meters with drapes and recorded the group each patient was assigned.
Induction of anesthesia
In the operating room a peripheral vein was catheterized and a Ringer's solution infusion was started. Monitoring consisted of pulse oximetry, electrocardiogram, heart rate, noninvasive arterial pressure, end-tidal carbon dioxide (EtCO2), inspired and end-tidal sevoflurane concentrations, tidal volume and respiratory rate (S/5™ Anesthesia Monnitor, Datex-Ohmeda Division, Datex-Ohmeda, Helsinki, Finland) and bispectral index (BIS xp A-2000™ Monitor, System Rev 3.21, ASPECT Medical Systems, Leiden, The Netherlands).
According to the group allocation, in the preinduction period patients were fully awake, breathing spontaneously either 50% N2O in oxygen (FiO2 = 0.5) or air (FiO2 = 0.21) for 10 min via a Mapleson C breathing system and a tightly fitting face mask. The face mask was hold by the attending anesthesiologist. In the meantime, the anesthetic circuit was primed with 8% sevoflurane: An oxygen flow 6 L/min was allowed to pass through the circle anesthetic system with the sevoflurane vaporizer dial being set at 8% for 5 min. An endotracheal tube was attached to the end of the anesthetic system with the distal end tightly surrounded by a plastic bag.[9] After the completion of the 10 min administration of the N2O/oxygen or air, the face mask was connected to the sevoflurane primed anesthetic circuit and all patients were allowed to breathe spontaneously sevoflurane in oxygen with the sevoflurane vaporizer set at 8% and an oxygen flow rate 6 L/min. After a 5 min period of sevoflurane inhalation, the study protocol and data collection were completed. A short acting opioid was given IV and a supraglottic airway device was inserted for the ventilation of patients during surgery.
Measurements
During the 10 min preinduction period, BIS, respiratory rate, tidal volume, EtCO2, heart rate and oxygen saturation (SpO2) were recorded every minute. The same parameters were recorded every 30 s during the first 5 min induction period with the patient breathing sevoflurane in oxygen. During the induction period inspired and end-tidal sevoflurane concentrations were also recorded every 30 s. Arterial blood pressure was recorded only before starting the pretreatment with the gas and after completion of measurements to avoid stimulus during cuff inflation affecting BIS measurements.
We hypothesized that the speed of inhalation induction with sevoflurane will be enhanced by N2O pretreatment, and possible subsequent volume contraction occurring before sevoflurane administration. BIS was the primary outcome measure, the rest variables being secondary outcome measures. At each time point, three consecutive BIS values were read and the median one was selected.
Data analysis
Initial sample size estimation showed that approximately 40 patients are needed in each group to detect a clinically relevant reduction of BIS after induction of anesthesia by 30% with a power of 0.80 and level of significance of 5%.
To assess differences in patients’ characteristics between the two groups, two independent samples t-tests for normally distributed responses and Mann-Whitney tests for nonnormally distributed responses were carried out. Overall group differences in all variables were assessed by using repeated measures ANOVA. A paired samples t-test or a Mann-Whitney test was used to assess differences at each time point wherever appropriate. All analyses were performed using the Statistical Package for Social Sciences (SPSS) software, version 11.0 (SPSS Inc., Chicago, IL, USA).
Results
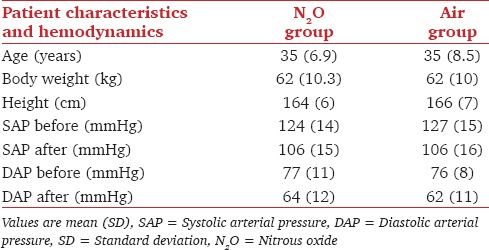
The N2O and the air groups did not differ in age, body weight, and height. Similarly, they did not differ in systolic and diastolic arterial pressure before or after the end of measurements [Table 1].
Table 1.
Patient characteristics, SAP and DAP blood pressures before and after the measurements
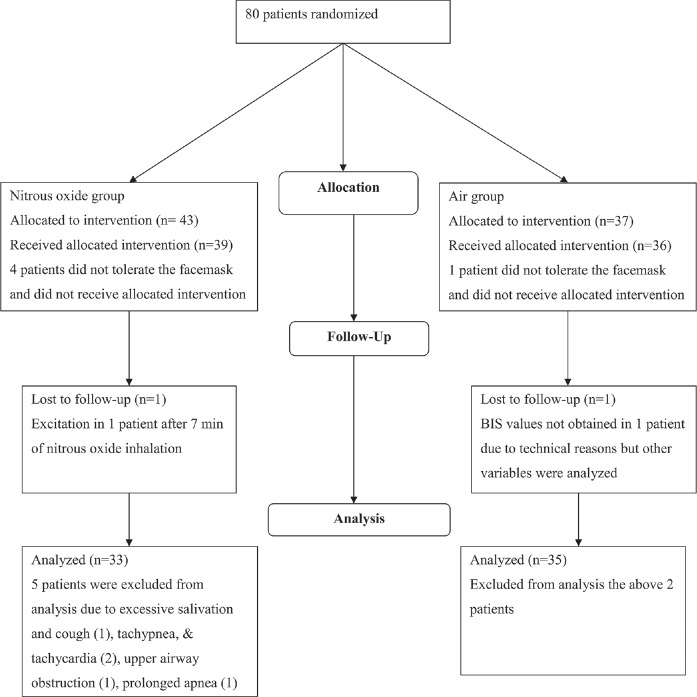
Of the 80 patients recruited for the study, 43 patients were assigned to the N2O and 37 to the air group. Four patients in the N2O group and one patient in the air group did not accept the facemask from the very beginning and no data were collected from these patients. One patient in the N2O group presented excitatory movements and removed the mask after N2O inhalation for 7 min and no further data were collected. In another patient in the air group BIS values were not at any time point obtained due to technical reasons, but all the other variables were recorded and analyzed [Figure 1].
Figure 1.
The flow diagram of the study
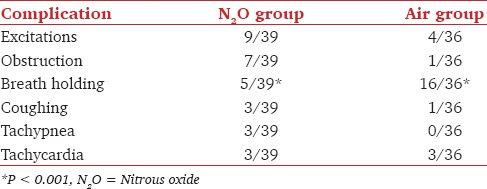
During sevoflurane inhalation in the N2O group the study was interrupted in one patient at 120 s due to persisting cough and salivation, in one patient at 180 s due to tachypnea, tachycardia and upper airway obstruction, in one patient at 210 s due to tachypnea and tachycardia, in one patient at 240 s due to upper airway obstruction, and in one patient at 270 s due to prolonged apnea. The overall incidence of complications in each group is shown in Table 2.
Table 2.
The incidence of complications during pretreatment with N2O or air followed by sevoflurane induction in the N2O and air groups
During the 10 min period of breathing 50% N2O in oxygen or air, the BIS, EtCO2, tidal volume, respiratory rate and heart rate did not differ between the group given N2O and that given air, nor was there a trend to a difference. SpO2 was slightly but significantly greater in patients given N2O, consistent with the higher inspired oxygen concentration of oxygen breathed.
During sevoflurane induction BIS values were lower in the N2O group [Table 3 and Figure 2]. At the time points 60, 90, 120 and 150 s, the BIS values in the N2O versus air group were: 77 ± 19.0 versus 92 ± 8.6 (P < 0.001), 44 ± 19.8 versus 73 ± 21.4 (P < 0.001), 36 ± 12.4 versus 55 ± 24.7 (P = 0.002) and 32 ± 11.0 versus 45 ± 20.8 (P = 0.014), respectively. EtCO2 and tidal volume values were lower and respiratory rate higher in the N2O group when compared to the air group. SpO2, heart rate, inspired and end-tidal sevoflurane concentration did not differ significantly between the two groups during the first 300 s of sevoflurane inhalation [Table 3].
Table 3.
BIS, EtCO2, VT, RR, SpO2, HR and FI and FE sevoflurane concentrations in the N2O- and air-breathing groups during induction of anesthesia with sevoflurane
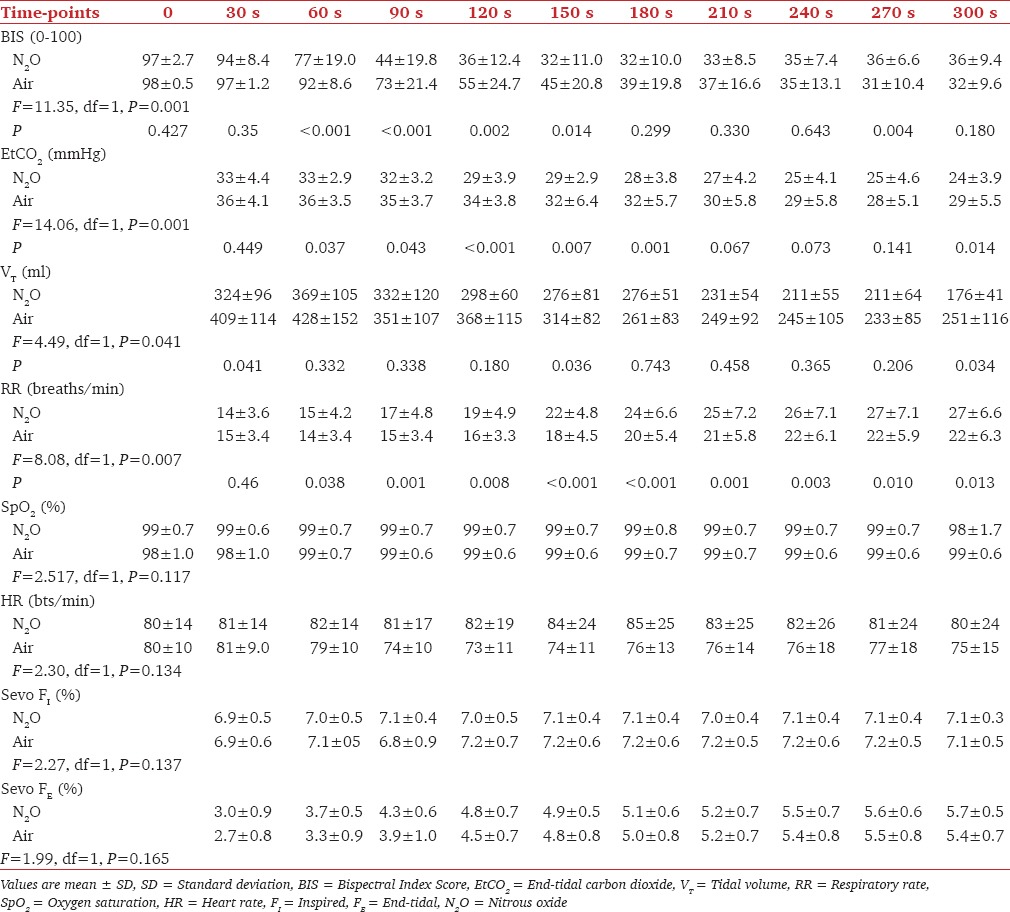
Figure 2.
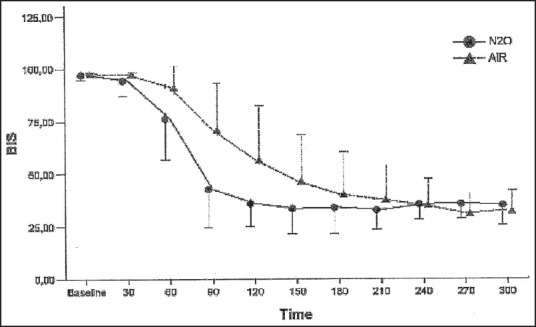
Bispectral index values (mean ± standard deviation) during inhalation with sevoflurane in the nitrous oxide and air groups
Discussion
The results of the present study suggest that pretreatment with N2O in 50% oxygen for 10 min before inhalation induction with sevoflurane enhances induction as assessed by decreased BIS values. These results are not consistent with other studies when N2O was administered concomitantly with sevoflurane for inhalation induction. Nevertheless, these studies were based on clinical criteria, which are subjective and therefore more difficult to be quantified.
O'shea et al. found that the addition of 50% N2O to the sevoflurane/oxygen mixture had no effect on the speed of induction and was associated with more excitatory effects. The investigators defined induction time as the time needed for the raised arm to fall to the horizontal level.[7]
Also, according to Siau and Liu, 66% N2O added to oxygen did not decrease the induction time with 8% sevoflurane when compared to the induction time of 8% sevoflurane in oxygen alone. Adverse events during induction were similar in the two groups. The induction time was defined as the time to cessation of finger tapping. These investigators administered higher concentrations of N2O than those administered in the present study but did not prime the circle breathing circuit with sevoflurane.[8]
In a previous study, we have shown that pretreatment with 100% oxygen enhances the inhalation induction with ≥7% sevoflurane as assessed by BIS monitoring.[10]
Replacing nitrogen in the lungs with a more soluble gas like oxygen, results in lung collapse, decreased functional residual capacity and increased alveolar concentration of the inhaled anesthetic, that is, sevoflurane.[11,12] In contrast to oxygen, in the present study the N2O was discontinued during induction. It is worthy to note that during induction, the end-tidal (FE) sevoflurane concentration (though no statistically significant) was higher during the first 120 s. The higher FE is consistent with increased ventilation in the N2O group, as indicated by the higher respiratory rates and the lower CO2 values. Increased ventilation favors the uptake of the volatile anesthetic.
In the present study, oxygen is also expected to enhance the sevoflurane uptake and to diminish the difference between the N2O and air groups as it is more soluble than nitrogen and part of the lungs will collapse to some extent (absorption atelectasis).[12] Similarly, N2O-being 32 times more soluble than nitrogen - is rapidly up taken by the blood, resulting in lung contraction and increased alveolar concentration of sevoflurane. However, eventually alveolar collapsing will be associated with pulmonary shunt which will delay sevoflurane uptake.[13] The time points at which BIS values differ significantly in the present study are between 60 and 150 s.
The inspired and expired sevoflurane concentrations did not differ between the N2O and the air groups during the 300 s period of induction, though the end-tidal/inspired concentration (F E/FI) ratio for sevoflurane was consistently higher by 2-7% in the N2O group. Sevoflurane due to its low blood gas partition coefficient might not benefit from the second gas effect phenomenon. However Taheri and Eger have nicely demonstrated the second gas effect for desflurane, an agent even less blood soluble.[14] Hendrickx et al. demonstrated a higher ratio of alveolar/inspired (F A/FI) sevoflurane concentration when N2O was added to the inspired mixture.[15] Peyton et al. reported a two to three times more powerful second gas effect of N2O on arterial versus the end-expired sevoflurane pressures and attributed this effect to ventilation perfusion inhomogeneity by general anesthesia.[16] In both studies, sevoflurane measurements were performed after IV induction of anesthesia and during mechanical ventilation.[15,16] Our data were collected with the patients breathing spontaneously and receiving solely sevoflurane without other anesthetics or adjuvants.
Pretreatment with N2O may not ensure an overall faster inhalation induction, but highlights the failure of previous studies to demonstrate enhancement of sevoflurane induction by concomitant N2O administration. Nonetheless, shorter periods of exposure may also enhance the sevoflurane induction. Previous studies failed to show a more rapid induction of anesthesia with sevoflurane for various reasons. As sevoflurane is an agent with low solubility, it may not benefit the very first minutes of induction by the concomitant administration of N2O. The additive synergism of the N2O and sevoflurane might also enhance the inhalation induction. However, such a synergism should also enhance the induction times in other studies. So we remain with our hypothesis that this difference between the N2O and air groups may be attributed to the pretreatment rather than the co-administration of N2O during sevoflurane induction of anesthesia.[13] A very early increased concentration effect due to volume reduction and before the “shunt” effect, as N2O is taken up by the pulmonary capillaries or increased ventilation, as shown by the lower EtCO2, in the N2O group may have influenced the speed of the sevoflurane uptake.
In clinical practice, fast inhalational induction may be beneficial for both patients and hospitals; it may shorten the second stage of anesthesia, thus reducing the risk of agitation/adverse respiratory events, and increase patient's satisfaction, while-depending on the time saved - it may also decrease the overall operating room time and facilitate fast turnover.[17,18]
Our measurements are limited by the sensitivity of the device we used to measure sevoflurane and N2O, thus the infrared analyzer, as the gold standard to measure concentrations of inhaled anesthetics is the gas chromatography or the mass spectrometry. Other limitations of the study are the number of dropouts, which may have an impact on the study power and the relatively long period of N2O pretreatment which weakens the clinical implementation of our results and shorter pretreatment periods like 2 or 3 min may be clinically applicable.
Conclusion
Under the present study design, breathing of 50% N2O in oxygen before induction with sevoflurane enhances the speed of induction in the very early period as assessed by the BIS monitor.
Acknowledgements
The authors thank Mrs. Aikaterini Dimitriou for helping in statistical analysis of the data.
Footnotes
Source of Support: Nil
Conflicts of Interest: None declared.
References
- 1.Nishiyama T, Matsukawa T, Yokoyama T, Hanaoka K. Rapid inhalation induction with 7% sevoflurane combined with intravenous midazolam. J Clin Anesth. 2002;14:290–5. doi: 10.1016/s0952-8180(02)00361-6. [DOI] [PubMed] [Google Scholar]
- 2.Watanabe T, Inagaki Y, Ishibe Y. Clonidine premedication effects on inhaled induction with sevoflurane in adults: A prospective, double-blind, randomized study. Acta Anaesthesiol Scand. 2006;50:180–7. doi: 10.1111/j.1399-6576.2006.00910.x. [DOI] [PubMed] [Google Scholar]
- 3.Katoh T, Nakajima Y, Moriwaki G, Kobayashi S, Suzuki A, Iwamoto T, et al. Sevoflurane requirements for tracheal intubation with and without fentanyl. Br J Anaesth. 1999;82:561–5. doi: 10.1093/bja/82.4.561. [DOI] [PubMed] [Google Scholar]
- 4.Knaggs CL, Drummond GB. Randomized comparison of three methods of induction of anaesthesia with sevoflurane. Br J Anaesth. 2005;95:178–82. doi: 10.1093/bja/aei149. [DOI] [PubMed] [Google Scholar]
- 5.Enekvist B, Bodelsson M, Sturesson LW, Johansson A. Larger tidal volume increases sevoflurane uptake in blood: A randomized clinical study. Acta Anaesthesiol Scand. 2010;54:1111–6. doi: 10.1111/j.1399-6576.2010.02291.x. [DOI] [PubMed] [Google Scholar]
- 6.Yurino M, Kimura H. Comparison of induction time and characteristics between sevoflurane and sevoflurane/nitrous oxide. Acta Anaesthesiol Scand. 1995;39:356–8. doi: 10.1111/j.1399-6576.1995.tb04077.x. [DOI] [PubMed] [Google Scholar]
- 7.O’shea H, Moultrie S, Drummond GB. Influence of nitrous oxide on induction of anaesthesia with sevoflurane. Br J Anaesth. 2001;87:286–8. doi: 10.1093/bja/87.2.286. [DOI] [PubMed] [Google Scholar]
- 8.Siau C, Liu EH. Nitrous oxide does not improve sevoflurane induction of anesthesia in adults. J Clin Anesth. 2002;14:218–22. doi: 10.1016/s0952-8180(02)00349-5. [DOI] [PubMed] [Google Scholar]
- 9.Korman B, Mapleson WW. Concentration and second gas effects: Can the accepted explanation be improved? Br J Anaesth. 1997;78:618–25. doi: 10.1093/bja/78.5.618. [DOI] [PubMed] [Google Scholar]
- 10.Fassoulaki A, Petropoulos G, Kottis G, Sarantopoulos C. Pre-oxygenation enhances induction with sevoflurane as assessed using bispectral index monitoring. Acta Anaesthesiol Scand. 2006;50:475–80. doi: 10.1111/j.1399-6576.2006.00981.x. [DOI] [PubMed] [Google Scholar]
- 11.Hedenstierna G. Gas exchange pathophysiology during anesthesia. Anesthesiol Clin N Am. 1998;16:113–27. [Google Scholar]
- 12.Rothen HU, Sporre B, Engberg G, Wegenius G, Reber A, Hedenstierna G. Atelectasis and pulmonary shunting during induction of general anaesthesia - Can they be avoided? Acta Anaesthesiol Scand. 1996;40:524–9. doi: 10.1111/j.1399-6576.1996.tb04483.x. [DOI] [PubMed] [Google Scholar]
- 13.Eger EI, 2nd, Severinghaus JW. Effect of uneven pulmonary distribution of blood and gas on induction with inhalation anesthetics. Anesthesiology. 1964;25:620–6. doi: 10.1097/00000542-196409000-00007. [DOI] [PubMed] [Google Scholar]
- 14.Taheri S, Eger EI., 2nd A demonstration of the concentration and second gas effects in humans anesthetized with nitrous oxide and desflurane. Anesth Analg. 1999;89:774–80. doi: 10.1097/00000539-199909000-00047. [DOI] [PubMed] [Google Scholar]
- 15.Hendrickx JF, Carette R, Lemmens HJ, De Wolf AM. Large volume N2O uptake alone does not explain the second gas effect of N2O on sevoflurane during constant inspired ventilation. Br J Anaesth. 2006;96:391–5. doi: 10.1093/bja/ael008. [DOI] [PubMed] [Google Scholar]
- 16.Peyton PJ, Horriat M, Robinson GJ, Pierce R, Thompson BR. Magnitude of the second gas effect on arterial sevoflurane partial pressure. Anesthesiology. 2008;108:381–7. doi: 10.1097/ALN.0b013e318164caf3. [DOI] [PubMed] [Google Scholar]
- 17.Hall JE, Ebert TJ, Harmer M. Induction characteristics with 3% and 8% sevoflurane in adults: An evaluation of the second stage of anaesthesia and its haemodynamic consequences. Anaesthesia. 2000;55:545–50. doi: 10.1046/j.1365-2044.2000.01476.x. [DOI] [PubMed] [Google Scholar]
- 18.Joshi GP. Inhalational techniques in ambulatory anesthesia. Anesthesiol Clin North America. 2003;21:263–72. doi: 10.1016/s0889-8537(02)00074-3. [DOI] [PubMed] [Google Scholar]