Abstract
Objective
Patients with suspected mesial temporal lobe (MTL) epilepsy typically undergo inpatient video–electroencephalography (EEG) monitoring with scalp and/or intracranial electrodes for 1 to 2 weeks to localize and lateralize the seizure focus or foci. Chronic ambulatory electrocorticography (ECoG) in patients with MTL epilepsy may provide additional information about seizure lateralization. This analysis describes data obtained from chronic ambulatory ECoG in patients with suspected bilateral MTL epilepsy in order to assess the time required to determine the seizure lateralization and whether this information could influence treatment decisions.
Methods
Ambulatory ECoG was reviewed in patients with suspected bilateral MTL epilepsy who were among a larger cohort with intractable epilepsy participating in a randomized controlled trial of responsive neurostimulation. Subjects were implanted with bilateral MTL leads and a cranially implanted neurostimulator programmed to detect abnormal interictal and ictal ECoG activity. ECoG data stored by the neurostimulator were reviewed to determine the lateralization of electrographic seizures and the interval of time until independent bilateral MTL electrographic seizures were recorded.
Results
Eighty-two subjects were implanted with bilateral MTL leads and followed for 4.7 years on average (median 4.9 years). Independent bilateral MTL electrographic seizures were recorded in 84%. The average time to record bilateral electrographic seizures in the ambulatory setting was 41.6 days (median 13 days, range 0–376 days). Sixteen percent had only unilateral electrographic seizures after an average of 4.6 years of recording.
Significance
About one third of the subjects implanted with bilateral MTL electrodes required >1 month of chronic ambulatory ECoG before the first contralateral MTL electrographic seizure was recorded. Some patients with suspected bilateral MTL seizures had only unilateral electrographic seizures. Chronic ambulatory ECoG in patients with suspected bilateral MTL seizures provides data in a naturalistic setting, may complement data from inpatient video-EEG monitoring, and can contribute to treatment decisions.
Keywords: EEG monitoring, Electrocorticography, Ambulatory EEG, Intracranial EEG, Responsive stimulation, Localization
Key Points
Ambulatory electrocorticograms were obtained in patients implanted with a responsive neurostimulator and bilateral mesial temporal intracranial electrodes.
In patients with bilateral seizures, the average time to record bilateral electrographic seizures in the ambulatory setting was 41.6 days (median 13, range 0–376).
Some patients suspected to have bilateral MTL seizures after standard diagnostic localization evaluations had only unilateral electrographic seizures.
Chronic ambulatory ECoG samples provide naturalistic data that complement inpatient monitoring, and may contribute information that affects treatment decisions.
Mesial temporal lobe (MTL) epilepsy is the most common surgically remediable form of epilepsy.1 Patients with MTL epilepsy being considered for resective surgery typically undergo inpatient video–electroencephalography (EEG) monitoring with scalp and sometimes intracranial electrodes to establish localization and lateralization of the seizure focus or foci. The duration of video-EEG monitoring varies but is usually <2 weeks. The literature suggests that for some patients, this period of monitoring may not be sufficient to establish whether the MTL seizure onsets are unilateral or bilateral, and, in patients with bilateral onset, to establish the relative distribution of left- and right-sided seizures.2–4
Electrocorticography (ECoG) samples were examined in patients with medically intractable partial seizures who were suspected to have bilateral MTL seizure onsets after standard localization testing, and were chronically implanted with bilateral MTL electrodes. The intent was to assess the time required to confidently determine the laterality of electrographic seizures in a naturalistic setting and to determine whether this information could influence treatment recommendations.
Methods
Ambulatory ECoG was analyzed retrospectively in subjects who were implanted with bilateral MTL electrodes while participating in a double-blind, randomized, sham-stimulation controlled investigational trial of the RNS System (NeuroPace, Inc., Mountain View, CA, U.S.A.) as an adjunctive treatment for adults with medically intractable partial-onset seizures from one or two foci.5 Subjects were 18 years of age or older with partial-onset seizures that were intractable to two or more antiepileptic medications and who had seizures arising from one or two foci, as identified by standard localization procedures at that center. After a 3-month baseline, subjects were implanted with the neurostimulator and leads. The neurostimulator was programmed in every subject to detect and store specific ECoG patterns identified by the physician, including electrographic seizures. One month after implantation, subjects were randomized 1:1 to receive responsive or sham stimulation for 4 months. After the completion of the fifth postimplantation month, all subjects entered an open-label period during which every subject received responsive stimulation. The open-label period was complete 2 years after implantation, after which subjects transitioned into a long-term treatment trial to provide an additional 7 years of prospective follow-up. The methodology, patient selection criteria, and results of the randomized controlled study and interim results of the ongoing long-term treatment study have been published previously.5–7
The RNS System provides responsive cortical stimulation via a cranially implanted programmable neurostimulator connected to recording and stimulating depth and/or subdural cortical strip leads that are surgically placed at the seizure focus. Each lead contains four electrode contacts, and up to two leads can be connected to the neurostimulator. The neurostimulator continuously senses ECoG activity through the electrodes and is programmed by the physician to detect specific patterns in the ECoG, such as patterns characteristic of the onset of an electrographic seizure, and to provide brief pulses of stimulation in response to the detected patterns. In usual clinical use, detection is optimized and then responsive stimulation is enabled.
Each ECoG sample stored by the neurostimulator is typically 90 s (60 s before detection and 30 s after). If the neurostimulator’s 6-min storage capacity is filled, then the earliest sample may be overwritten by the newest. To free neurostimulator memory, patients use a handheld wireless wand at home to transfer data from the neurostimulator to a remote monitor, and then intermittently transmit the data securely through the internet to a secure centralized database for storage. The physician reviews these ECoG samples via a programmer in the office or remotely using a secure web browser.
ECoG recordings were reviewed by two independent reviewers. Electrographic seizures were defined as episodes of low-voltage fast activity or rhythmic sharp activity, distinct from background, evolving and lasting longer than 25 s. This definition of electrographic seizure was derived empirically, since this ensured that a clear onset and frequency evolution could be observed within the ECoG sample. In addition, the literature suggests that mesial temporal onset seizures with clinical symptoms will exceed this duration and that electrographic seizures that are clinically silent will be shorter.8,9
To determine seizure lateralization and the interval of time until independent bilateral MTL seizure onsets were recorded, ECoG data were reviewed from implant until at least one electrographic seizure was recorded from each side. For subjects in whom only unilateral seizures were recorded, all ECoG recordings were reviewed from implant to the data cut-off date (6/13/2013).
Results
Eighty-two of the 191 subjects who participated in the randomized controlled study were implanted with bilateral MTL electrodes (Fig. S1). The average follow-up for these subjects was 4.7 years (median 4.9 years; range 1.2 months to 7.1 years). During the first year after implantation, subjects transferred neurostimulator data to the remote monitor once per day on average (ranging from an average of 2.2 times a day to once every 3.7 days). This provided an average of 2.5 ECoG recordings per day (range 0.8–7.6) for physician review. An example of ECoG recordings obtained by the neurostimulator and viewed using the RNS System is provided in Figure1.
Figure 1.
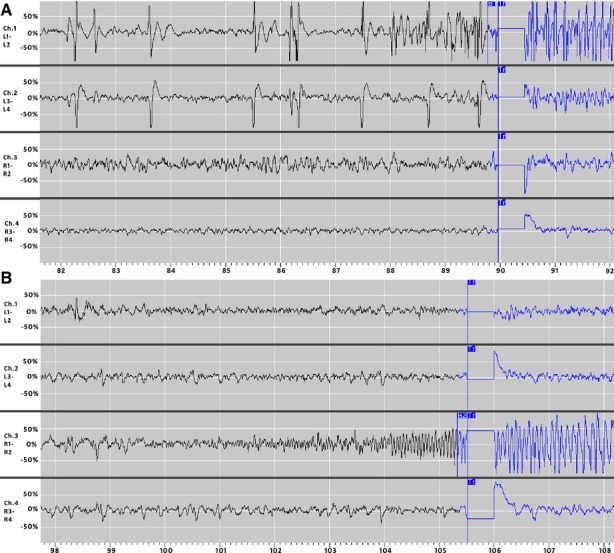
Examples of bilateral seizure onsets recorded in one subject. Panels A and B show left- and right- sided seizure onsets (respectively) recorded in the same subject. In Panel A, the onset in the left hippocampus begins with spiking followed by high amplitude fast activity on channel 1. The flag labeled “B1″ on the first channel at 89.8 s denotes detection of abnormal electrographic activity by the neurostimulator based on the programmed detection settings. The flags labeled “Tr” at 90 s indicate delivery of responsive stimulation. There is an artifact in the recording when responsive stimulation is delivered. In Panel B, the onset in the right hippocampus begins with rhythmic beta activity on channel 3. The flag labeled “B2” on the third channel at 105.3 s denotes detection of abnormal electrographic activity by the neurostimulator based on the programmed detection settings. The flags labeled “Tr” at 105.5 s indicate delivery of responsive stimulation.
Demographics for the 82 subjects implanted with bilateral MTL leads are presented in Table1. Based on preimplantation diagnostic localization procedures, which included video-EEG monitoring in all subjects, 71 of these 82 subjects were presumed to have bilateral seizures at the time of implantation of the RNS System. The remaining 11 subjects were presumed to have unilateral seizures; however, bilateral MTL leads were implanted because other diagnostic localization testing suggested contralateral MTL structural or functional abnormalities. These included bilateral hippocampal atrophy or mesial temporal sclerosis (three subjects), an intracarotid amobarbital (Wada) test indicating that the contralateral temporal lobe did not adequately support memory (five subjects), a prior contralateral temporal lobectomy (two subjects), or discordant EEG and positron emission tomography (PET) lateralization (one subject). No subject in this series had diagnostic localization testing that was entirely concordant for unilateral MTL epilepsy.
Table 1.
Demographic and clinical characteristics of subjects implanted with bilateral mesial temporal electrodes (N = 82)
| Female | 47.6% (39/82) |
|---|---|
| Age in yearsa (mean, SD, range) | 37.2 ± 10.9 (18–60) |
| Duration of epilepsy in yearsa (mean, SD, range) | 19.9 ± 13.2 (2–57) |
| Number of AEDs at enrollmenta (mean, SD, range) | 2.7 ± 1.1 (1–5) |
| Preimplantb seizure frequency per month (mean, SD, range) | 13.7 ± 17.4 (3.0–88.3) median = 7.0 |
| Prior intracranial monitoring | 42.7% (35/82) |
| Prior epilepsy surgery | 7.3% (6/82) |
| Prior VNS | 26.8% (22/82) |
| Hippocampal atrophy or mesial temporal sclerosis | 63.4% (52/82) |
| Unilateral | 34.6% (18/52) |
| Bilateral | 65.4% (34/52) |
| Preimplant electrographic seizuresb | |
| Bilateral | 86.6% (71/82) |
| Unilateral | 13.4% (11/82) |
| Left | 63.6% (7/11) |
| Right | 36.4% (4/11) |
At time of enrollment into the pivotal study.
Preimplant refers to evaluation prior to implantation of the RNS Neurostimulator and NeuroPace leads.
The most common lead implant strategy was to place depth leads along the long axis of the hippocampus. Ninety-six percent (79/82) of the subjects were implanted with a depth lead in each hippocampus, and 4% (3/82) were implanted with bilateral subtemporal cortical strip leads. Six of the 82 subjects had already undergone a temporal lobectomy, but leads were placed in residual MTL tissue. Examples of cortical strip lead and hippocampal depth lead implantations, as well as an example of a depth lead implantation in a subject with a prior temporal lobectomy are provided in Figure2.
Figure 2.
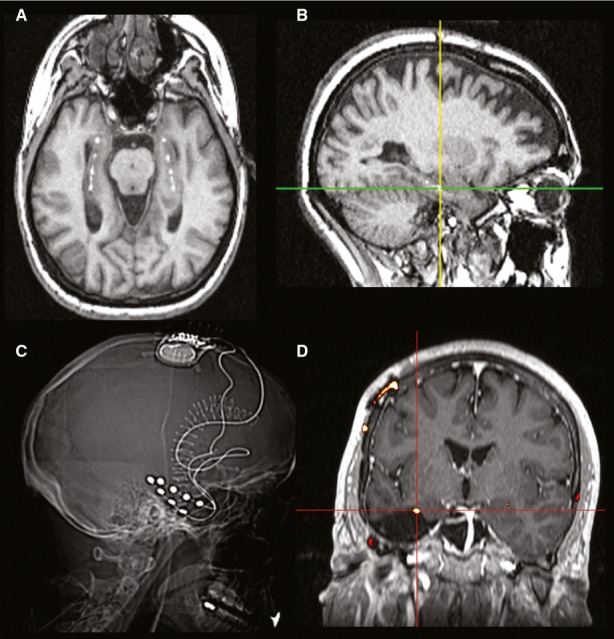
CT/MRI co-registered images of hippocampal lead implants. Panels A, B, and D show pre-implant MRI images co-registered with post-implant CT images. Panel A is an axial slice along the axis of the hippocampus showing the depth leads implanted bilaterally in the hippocampi. Panel B shows a sagittal image of the same implant, where the cross-hairs identify the second electrode of the depth lead implanted in the left hippocampus. Panel C shows a CT image of the neurostimulator (implanted in the parietal skull) connected to bilateral sub-temporal cortical strip leads. Panel D shows a coronal image of a depth lead implanted in the left hippocampus after a left temporal resection.
The first analysis considered all 82 subjects. Thirteen (16%) of the 82 subjects had only unilateral electrographic seizures after an average of 4.6 years of ambulatory ECoG recording (Table2). Sixty-nine (84%) of 82 ultimately had bilateral MTL electrographic seizures with an average time to record the first contralateral electrographic seizure of 41.6 days (median 13 days; range 0–376 days). The first contralateral electrographic seizure was recorded within the first postimplantation month in 68% (47/69), which was before randomization and therefore before any subject was treated with responsive stimulation. Thirty-two percent (22/69) of the subjects had the first contralateral electrographic seizure after the fourth week, which was when one half of the subjects were randomized to receive responsive stimulation. In these 22 subjects, there was no difference between those randomized to receive responsive stimulation (N = 11) and those in the group who did not receive responsive stimulation (sham stimulation group, N = 11) in the time to record the first contralateral seizure (p = 0.51, two-sample t-test). Figure3 illustrates the length of time before independent bilateral MTL electrographic seizures were recorded.
Table 2.
Lateralization of electrographic seizures by inpatient EEG and by chronic ambulatory electrocorticography (ECoG) N = 82
| Electrographic seizure onsets by inpatient EEG monitoring | Electrographic seizure onset by chronic ambulatory ECoG | |
|---|---|---|
| Bilateral (n = 69) | Unilateral (n = 13) | |
| Bilateral (n = 71) | 75.6% (n = 62) | 11.0% (n = 9) |
| Unilateral (n = 11) | 8.5% (n = 7) | 4.9% (n = 4) |
Figure 3.
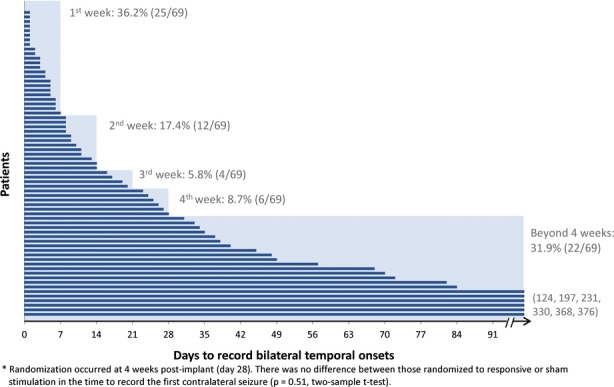
Time to record bilateral temporal onsets.
The next analysis considered the 71 subjects who were presumed to have independent bilateral seizure onsets based on preimplantation diagnostic localization procedures. Nine of these 71 subjects had only unilateral electrographic seizures by chronic ambulatory ECoG after an average follow-up of 5.0 years (median 4.8 years; range 2.9–6.5 years). Bilateral electrographic MTL seizures were recorded by ambulatory ECoG in 62 (87%) of the 71 subjects. The first contralateral seizure was obtained during the first week of ambulatory ECoG in 38.7% (24/62), during the second week in 17.7% (11/62), during the third week in 6.5% (4/62), during the fourth week in 9.7% (6/62), and after the fourth week in 27.4% (17/62).
Eleven of the 82 subjects were thought to most likely have unilateral seizures based on the preimplantation diagnostic localization, although all of these subjects had localization testing that suggested that there were contralateral MTL abnormalities. Two of these subjects had already had a temporal lobectomy, and inpatient seizure onsets were ipsilateral to the side of resection. With chronic ambulatory ECoG, 7 (64%) of these 11 subjects had independent bilateral electrographic MTL seizures, with an average time of 72.4 days (median 35 days; range 7–330 days) to record the first contralateral electrographic seizure. Four of the 11 subjects had only unilateral seizures recorded by chronic ambulatory ECoG, with an average duration of 3.9 years (median 4.1 years; range 0.4–7.0 years) of recording.
Lateralization results by ambulatory ECoG were assessed in subjects according to whether they had undergone a temporal lobe resection. Six of the 82 subjects had already had a temporal lobectomy. Lateralization by preimplantation diagnostic localization testing and chronic bilateral ECoG recording was concordant in two of these patients (bilateral onsets). Two of the six were presumed to have unilateral seizures prior to implantation but had bilateral electrographic seizures recorded during chronic ambulatory ECoG, and two subjects were presumed to have bilateral seizures prior to implantation but had only unilateral seizures recorded with chronic ambulatory ECoG (contralateral to the resection in both subjects). The average duration of time to the first contralateral seizure in the four post lobectomy subjects with bilateral onsets was 100 days (median 34.5 days; range 1–330 days).
Seventy-six of the 82 subjects had not had a temporal lobectomy and 65 of these 76 subjects had bilateral electrographic seizures recorded by ambulatory ECoG. The duration of time before a contralateral seizure was recorded was on average 38 days (median 11 days; range 0–376 days).
Demographic and clinical characteristics were compared between those subjects who ultimately had bilateral independent MTL electrographic seizures and those whose seizures remained strictly unilateral. There was no difference between the two groups in duration of epilepsy, seizure frequency, number of AEDs, frequency of mesial temporal sclerosis (MTS) or hippocampal atrophy, or history of treatment with epilepsy surgery or with vagus nerve stimulation (VNS) (Table S1).
An analysis was performed to assess whether abnormalities on magnetic resonance imaging (MRI) were likely to predict whether electrographic seizure onsets recorded by chronic ambulatory ECoG would be unilateral or bilateral, and whether MRI findings predicted the time until bilateral electrographic seizures were recorded. Those with bilateral MTS and/or atrophy were more likely to have independent bilateral MTL electrographic seizures, whereas those with unilateral MTS or atrophy were more likely to have unilateral electrographic seizures (p = 0.03, Fisher’s exact test; Table S2). MRI findings of MTS and/or atrophy did not predict whether the first contralateral seizure was recorded within the first 2 weeks (n = 37) or after the first 2 weeks (n = 32; p = 0.34, Fisher’s exact test), although there was a trend for subjects with earlier bilateral seizures to have bilateral MTS and/or atrophy (54.1% vs. 31.3%, p = 0.09, Fisher’s exact test).
Another variable that could predict whether the lateralization obtained by chronic ambulatory ECoG differed from the preimplantation lateralization was whether the subject had previously undergone inpatient video-EEG monitoring with intracranial electrodes. Thirty-five subjects had undergone inpatient intracranial monitoring prior to implantation of the RNS System; 34 were thought to have bilateral seizures, and one to have unilateral seizures. The determination regarding lateralization of MTL seizures changed in three subjects after chronic ambulatory ECoG (8.6%). These three subjects were presumed to have bilateral onsets but had only unilateral MTL electrographic seizures during chronic ambulatory ECoG (Table S3). The first bilateral electrographic seizure In the 31 subjects with bilateral onsets occurred within 1 week in 35.5% (11/31), during the second week in 19.4% (6/31), during the third week in 6.5% (2/31), during the fourth week in 9.7% (3/31), and after 2 weeks in 29.0% (9/31).
Forty-seven subjects had not undergone intracranial monitoring prior to implantation of the RNS System; 37 were considered to have bilateral MTL onsets and 10 were considered unilateral. The conclusion about lateralization changed in 13 of these subjects after chronic ambulatory ECoG (27.7%). Six subjects originally categorized as bilateral had only unilateral electrographic seizures, and seven originally categorized as unilateral had bilateral electrographic seizures (Table S4). In the 38 subjects with bilateral electrographic seizures during chronic ambulatory ECoG, the first contralateral seizure was obtained within 1 week in 36.8% (14/38), during the second week in 15.8% (6/38), during the third week in 5.3% (2/38), during the fourth week in 7.9% (3/38), and after 4 weeks in 34.2% (13/38).
To assess whether the frequency of ECoG recordings influenced the time to record the first contralateral seizure, an analysis was conducted of the four subjects whose baseline seizure rate was higher than their average ECoG storage rate since seizure recordings in these subjects could potentially be overwritten and not available for review. All of these subjects had independent bilateral seizures recorded within the first 20 days after implantation, indicating that the overall results are unlikely to reflect less-frequent sampling in those with longer latencies to the first contralateral seizure.
The additional data obtained from chronic ambulatory ECoG led to a temporal lobe resection in three patients who were not previously thought to be surgery candidates. Each was believed to have bilateral MTL onsets based on inpatient monitoring and other diagnostic localization testing. One subject had only unilateral MTL electrographic seizures after 4.4 years of chronic ambulatory ECoG. This subject had a unilateral temporal lobectomy and continued to have seizures after the initial resective procedure, but then became seizure free after a second procedure 21 months later. Another subject had only unilateral MTL electrographic seizures recorded for 1 year before the first contralateral MTL electrographic seizure was recorded. This subject had a unilateral temporal lobectomy 2 years after the implant and continued to be seizure free 3 years postresection. The third subject had bilateral MTL electrographic seizures recorded within the first month after implantation but based on the distribution of seizures was felt to be a candidate for a palliative nondominant temporal lobectomy. This surgery was performed 1 year after implantation and achieved a 63% reduction in seizure frequency. In each of these cases, the neurostimulator and at least one lead were left in place to sense and record the ECoG and to provide responsive stimulation in the remaining hippocampus.
Discussion
Patients with MTL epilepsy who are being considered for an epilepsy resective surgery undergo inpatient video-EEG monitoring with scalp and/or intracranial electrodes as well as neuroimaging and functional tests to establish localization and lateralization of the seizure focus or foci. The considerable hospital resources required for scalp and intracranial video-EEG monitoring and the risk for infection with prolonged intracranial monitoring usually limit the duration of monitoring to 1 to 2 weeks. The literature suggests that for some patients with MTL onsets, this period of monitoring may not be sufficient to definitively establish whether the seizure onset is unilateral or bilateral, and, in patients with bilateral onsets, to establish the relative distribution of seizures across left and right.2–4 In addition, seizures recorded after electrode implantation7 or with acute medication withdrawal10–12 may not be clinically or electrographically typical for that patient.
The ability to monitor intracranial EEG on an ambulatory basis offers the opportunity to record that patient’s typical seizures in a naturalistic setting over an extended period and without reducing antiepileptic medications. In the patients in this series who were demonstrated by chronic ambulatory ECoG to have independent bilateral MTL electrographic seizure onsets, the average time to document the first contralateral seizure was >5 weeks, with a range of days to many months. Ambulatory ECoG was clinically useful: the electrographic seizure lateralization changed from the preimplantation lateralization in nearly 20% of subjects, and some subjects were identified as candidates for temporal lobectomy.
In some instances, chronic ambulatory ECoG provided lateralization data that contradicted lateralization made by preimplantation diagnostic localization procedures. Seven of 11 patients were presumed to have unilateral seizures but ultimately had bilateral electrocorticographic seizures recorded by chronic ambulatory ECoG. Nine of 71 subjects who were presumed to have bilateral seizures had only unilateral electrographic seizures after years of ambulatory ECoG. Three subjects were identified as candidates for resective surgery based on the chronic ambulatory ECoG recordings.
Data from chronic ambulatory ECoG may complement but cannot substitute for inpatient monitoring with scalp and/or intracranial electrodes. First, the ambulatory ECoG data does not indicate whether a clinical seizure has occurred. Second, spatial sampling is limited to a few electrodes rather than the extensive electrode arrays possible in the inpatient setting. The chronically implanted electrodes are placed near the seizure onset in order to detect the electrographic seizure, which requires that standard inpatient scalp and/or intracranial monitoring be performed to plan lead electrode locations. In addition, the ECoG storage capacity of the neurostimulator is limited and, unlike inpatient monitoring, not all electrographic seizures are necessarily stored. If all ECoG samples are not stored, it may take longer to establish that there are bilateral electrographic seizures. However, there was no evidence to suggest that the latency to the first contralateral seizure was related to the rate at which subjects transferred ECoG data for storage.
A potential confound in this data set is that detection settings were modified during the trial as necessary to improve the detection specificity, and this could have impacted the ability to record electrographic seizures, as different detection settings will influence what type of ECoG activity is stored by the neurostimulator. However, detection settings were initially programmed to be highly sensitive to the types of ECoG patterns characteristic of electrographic seizures and were subsequently adjusted to be more sensitive to that patient’s specific ictal-onset patterns. Thus, it is unlikely that ECoG recordings containing electrographic seizures would not be detected and stored.
Although there was no standard protocol for evaluating and localizing seizure foci, the physicians participating in this study were highly experienced in procedures to localize seizure foci and were able to select the type of lead and lead location. Depth leads were most commonly used and were usually placed along the length of the hippocampus. Cortical strip leads were less commonly used. It is possible that one implant strategy could be better able to capture seizures than another, but there is not sufficient data from this series to determine the relative merits.
It is unlikely that responsive stimulation therapy or changes in antiepileptic medications affected the determination of laterality. Responsive stimulation was not enabled in any of the subjects in the first month after implant, which is when the majority (68%) of the bilateral onsets were captured. After the first month, there was no difference in the time to detection of the first contralateral electrographic seizure between those randomized to receive responsive stimulation and those who were not. Similarly, antiepileptic medications were held constant during the first 5 months after implant (per the study protocol), during which 93% of the bilateral onsets were captured.
Patients with medically intractable epilepsy of mesial temporal onset who are candidates for potentially curative mesial temporal lobe resection can be reliably identified with inpatient video-EEG monitoring and MRI, supplemented as needed with tests of MTL function such as PET and neuropsychological and intracarotid testing.
Patients for whom there is consistent localization to one temporal lobe in aggregate and for whom there are not concerns for significant memory or language deficits after resection, have a high probability of becoming seizure free after a temporal lobectomy. One-year and 2-year seizure remission can be achieved in at least 65% of patients with unilateral mesial temporal lobe seizure onsets after a temporal lobectomy.13 However, seizure remission is not achieved or sustained in all patients. Patients who have experienced two seizure-free years after temporal lobectomy have a relapse rate, on average, of 3.25% each year,14 with 60% of patients having at least one recurrence in the first 10 years.15 Lack of a sustained seizure remission could be caused by residual epileptogenic cortex, including a contralateral mesial temporal seizure focus. This hypothesis is supported by the risk factors that predict persistent seizures after a unilateral anterior temporal lobectomy, which include bilateral temporal lobe epileptiform abnormalities, structural or functional imaging that show either no abnormalities or bilateral or contralateral abnormalities, and neuropsychological testing and/or intracarotid amobarbital (Wada) testing indicating contralateral memory abnormalities.14 These findings could indicate that the patient has independent bilateral MTL onsets.16,17 This may be a common clinical scenario; postmortem neuropathologic studies describe bilateral mesial temporal sclerosis (MTS) in up to 80% of patients with MTL epilepsy.18–20
Demographics and clinical characteristics such as duration and frequency of seizures and treatment history did not differentiate subjects for whom chronic ambulatory ECoG monitoring provided information that contradicted lateralization using inpatient EEG monitoring from patients with consistent lateralization. The only exception appeared to be related to whether the subject had undergone inpatient intracranial monitoring. Lateralization changed after chronic ambulatory ECoG in 8.6% of those subjects who had been evaluated with inpatient intracranial monitoring (all presumed to be bilateral with inpatient monitoring but determined to be unilateral in the ambulatory setting) and in 27.6% of those patients who did not have inpatient intracranial monitoring (lateralization changing equally between bilateral and unilateral). The time to record the first MTL electrographic seizure during chronic ambulatory ECoG monitoring was not different; about 30% required >4 weeks before the first contralateral electrographic seizure was recorded.
Patients such as the subjects in this analysis who display bilateral independent MTL seizures during inpatient monitoring with scalp and/or EEG monitoring and those who have unilateral seizure onsets with other localization findings that are discordant and/or suggestive of memory or language deficits after surgery may not be good candidates for a resective surgery. This series suggests that chronic ambulatory ECoG may provide additional information to help define treatment options.
Disclosure of Conflicts of Interest
Author Emily Mirro certifies that she has equity ownership/stock options with NeuroPace and is an employee of NeuroPace. Author Felice T. Sun certifies that she has equity ownership/stock options with NeuroPace and is a contractor for NeuroPace. Author Martha J. Morrell certifies that she has equity ownership/stock options with NeuroPace and is an employee of NeuroPace. Author Robert Gross certifies that he serves as a consultant to NeuroPace and receives compensation for these services. NeuroPace develops products related to the research described in this paper. The terms of this arrangement have been reviewed and approved by Emory University in accordance with its conflict of interest policies. The remaining authors have no conflicts of interest that are relevant to this research activity. We confirm that we have read the Journal’s position on issues involved in ethical publication and affirm that this report is consistent with those guidelines.
Biography
 Epileptologist Dr. King-Stephens is director of clinical neurophysiology at Sutter Pacific’s Epilepsy Program.
Epileptologist Dr. King-Stephens is director of clinical neurophysiology at Sutter Pacific’s Epilepsy Program.
Supporting Information
Figure S1. Flow chart of subjects implanted with leads bilaterally in the MTL.
Table S1. Demographic and clinical characteristics by lateralization categorization (N=82).
Table S2. Temporal lobe MRI findings and lateralization of mesial temporal electrographic seizures by ambulatory ECoG
Table S3. Lateralization of electrographic seizures by inpatient intracranial EEG and by chronic ambulatory ECoG (N = 35).
Table S4. Lateralization of electrographic seizures by inpatient extracranial EEG and by chronic ambulatory ECoG (N=47).
References
- Engel J, Jr, Wiebe S, French J, et al. Practice parameter: temporal lobe and localized neocortical resections for epilepsy: report of the Quality Standards Subcommittee of the American Academy of Neurology, in association with the American Epilepsy Society and the American Association of Neurological Surgeons. Neurology. 2003;60:538–547. doi: 10.1212/01.wnl.0000055086.35806.2d. [DOI] [PubMed] [Google Scholar]
- Sum JM, Morrell MJ. Predictive value of the first ictal recording in determining localization of the epileptogenic region by scalp/sphenoidal EEG. Epilepsia. 1995;36:1033–1040. doi: 10.1111/j.1528-1157.1995.tb00963.x. [DOI] [PubMed] [Google Scholar]
- Noe KH, Drazkowski JF. Safety of long-term video-electroencephalo-graphic monitoring for evaluation of epilepsy. Mayo Clin Proc. 2009;84:495–500. doi: 10.4065/84.6.495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smart O, Rolston JD, Epstein CM, et al. Hippocampal seizure-onset laterality can change over long timescales: a same-patient observation over 500 days. Epilepsy Behav Case Rep. 2014;1:56–61. doi: 10.1016/j.ebcr.2013.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morrell MJ. Responsive cortical stimulation for the treatment of medically intractable partial epilepsy. Neurology. 2011;77:1295–1304. doi: 10.1212/WNL.0b013e3182302056. [DOI] [PubMed] [Google Scholar]
- Heck CN, King-Stephens D, Massey AD, et al. Two year seizure reduction in adults with medically intractable partial onset epilepsy treated with responsive neurostimulation: final results of the RNS® System Pivotal trial. Epilepsia. 2014;55:432–441. doi: 10.1111/epi.12534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bergey GK, Morrell MJ, Mizrahi EM, et al. Long-term treatment with responsive brain stimulation in adults with refractory partial seizures. Neurology. 2015;84:810–817. doi: 10.1212/WNL.0000000000001280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Afra P, Jouny CC, Bergey GK. Duration of complex partial seizures: an intracranial EEG study. Epilepsia. 2008;49:677–684. doi: 10.1111/j.1528-1167.2007.01420.x. [DOI] [PubMed] [Google Scholar]
- Sperling MR, O’Connor MJ. Auras and subclinical seizures: characteristics and prognostic significance. Ann Neurol. 1990;28:320–328. doi: 10.1002/ana.410280304. [DOI] [PubMed] [Google Scholar]
- Engel J, Jr, Crandall PH. Falsely localizing ictal onsets with depth EEG telemetry during anticonvulsant withdrawal. Epilepsia. 1983;24:344–355. doi: 10.1111/j.1528-1157.1983.tb04898.x. [DOI] [PubMed] [Google Scholar]
- Marciani MG, Gotman J, Andermann F, et al. Patterns of seizure activation after withdrawal of antiepileptic medication. Neurology. 1985;35:1537–1543. doi: 10.1212/wnl.35.11.1537. [DOI] [PubMed] [Google Scholar]
- Marks DA, Katz A, Scheyer R, et al. Clinical and electrographic effects of acute anticonvulsant withdrawal in epileptic patients. Neurology. 1991;41:508–512. doi: 10.1212/wnl.41.4.508. [DOI] [PubMed] [Google Scholar]
- Wiebe S, Blume WT, Girvin JP, et al. A randomized, controlled trial of surgery for temporal-lobe epilepsy. N Engl J Med. 2001;345:311–318. doi: 10.1056/NEJM200108023450501. [DOI] [PubMed] [Google Scholar]
- McIntosh AM, Kalnins RM, Mitchell LA, et al. Temporal lobectomy: long-term seizure outcome, late recurrence and risks for seizure recurrence. Brain. 2004;127:2018–2030. doi: 10.1093/brain/awh221. [DOI] [PubMed] [Google Scholar]
- Sperling MR, Nei M, Zangaladze A, et al. Prognosis after late relapse following epilepsy surgery. Epilepsy Res. 2008;78:77–81. doi: 10.1016/j.eplepsyres.2007.10.011. [DOI] [PubMed] [Google Scholar]
- Salanova V, Markand O, Worth R. Temporal lobe epilepsy: analysis of failures and the role of reoperation. Acta Neurol Scand. 2005;111:126–133. doi: 10.1111/j.1600-0404.2005.00371.x. [DOI] [PubMed] [Google Scholar]
- Hennessy MJ, Elwes RD, Binnie CD, et al. Failed surgery for epilepsy. A study of persistence and recurrence of seizures following temporal resection. Brain. 2000;123(Pt 12):2445–2466. doi: 10.1093/brain/123.12.2445. [DOI] [PubMed] [Google Scholar]
- Falconer MA, Taylor DC. Surgical treatment of drug-resistant epilepsy due to mesial temporal sclerosis. Etiology and significance. Arch Neurol. 1968;19:353–361. doi: 10.1001/archneur.1968.00480040019001. [DOI] [PubMed] [Google Scholar]
- Meencke HJ, Veith G, Lund S. Bilateral hippocampal sclerosis and secondary epileptogenesis. Epilepsy Res Suppl. 1996;12:335–342. [PubMed] [Google Scholar]
- Margerison JH, Corsellis JA. Epilepsy and the temporal lobes. A clinical, electroencephalographic and neuropathological study of the brain in epilepsy, with particular reference to the temporal lobes. Brain. 1966;89:499–530. doi: 10.1093/brain/89.3.499. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Figure S1. Flow chart of subjects implanted with leads bilaterally in the MTL.
Table S1. Demographic and clinical characteristics by lateralization categorization (N=82).
Table S2. Temporal lobe MRI findings and lateralization of mesial temporal electrographic seizures by ambulatory ECoG
Table S3. Lateralization of electrographic seizures by inpatient intracranial EEG and by chronic ambulatory ECoG (N = 35).
Table S4. Lateralization of electrographic seizures by inpatient extracranial EEG and by chronic ambulatory ECoG (N=47).


