Abstract
Background
Liver transplantation is performed at large transplant centers worldwide as a therapeutic intervention for patients with end-stage liver diseases.
Aim
To analyze the outcomes and incidence of liver transplantation performed at the University of São Paulo and to compare those with the State of São Paulo before and after adoption of the Model for End-Stage Liver Disease (MELD) score.
Method
Evaluation of the number of liver transplantations before and after adoption of the MELD score. Mean values and standard deviations were used to analyze normally distributed variables. The incidence results were compared with those of the State of São Paulo.
Results
There was a high prevalence of male patients, with a predominance of middle-aged. The main indication for liver transplantation was hepatitis C cirrhosis. The mean and median survival rates and overall survival over ten and five years were similar between the groups (p>0.05). The MELD score increased over the course of the study period for patients who underwent liver transplantation (p>0.05). There were an increased number of liver transplants after adoption of the MELD score at this institution and in the State of São Paulo (p<0.001).
Conclusion
The adoption of the MELD score led to increase the number of liver transplants performed in São Paulo.
Keywords: Transplantation, Disease, General surgery
Abstract
Racional
O transplante de fígado é realizado em grandes centros de transplante em todo o mundo como intervenção terapêutica para pacientes com doenças do fígado em fase terminal. Objetivo
Objetivo
Analisar os resultados e incidência de transplante de fígado realizado na Universidade de São Paulo e comparar com a do Estado de São Paulo antes e depois da adoção do Modelo para Doença Hepática Estágio Terminal (MELD).
Método
Avaliação do número de transplantes de fígado antes e depois da adoção do escore MELD. Os valores médios e desvios-padrão foram utilizados para analisar variáveis normalmente distribuídas. Os resultados de incidência foram comparados com os do Estado de São Paulo.
Resultados
Houve alta prevalência de homens, com predomínio na meia-idade. A principal indicação para o transplante de fígado foi cirrose por hepatite C. A média e as taxas de sobrevivência mediana e sobrevida global em dez e cinco anos, foram semelhantes entre os grupos (p>0,05). A pontuação MELD aumentou ao longo do período de estudo para os pacientes que se submeteram ao transplante de fígado (p>0,05). Houve aumento do número de transplantes de fígado após a adoção do escore MELD na Universidade de São Paulo e no Estado de São Paulo (p<0,001).
Conclusão
A adoção da pontuação MELD levou ao aumento do número de transplantes de fígado realizados em São Paulo.
INTRODUCTION
Liver disease accounts for a large number of fatalities worldwide and is one of the major causes of hospitalization. In advanced stages of liver disease, liver transplantation (LT) is the only effective intervention that can increase patient survival3,9.
The number of patients with renal dysfunction on the LT waiting list has increased since the adoption of the Model for End-Stage Liver Disease (MELD) score in 2002 for allocating liver allografts in the U.S.2,7,8.
This is particularly important when considering the potential demographic, ethnic and socioeconomic factors, the variable size of the LT waiting list, and the mean MELD score at the time of organ allocation. In addition, the different policies used to refer patients for combined transplantation procedures may alter the prognosis and long-term outcomes. In 2012, the average MELD score in patients transplanted in the department was 31.02.
The aim of this study was to evaluate the incidence and outcomes of LT performed at a single South American center before and after the adoption of the MELD score. Additionally, was compared the institutional results with those in a large neighboring area that includes the State of São Paulo.
METHODS
This study was approved by the Ethics Committee for Human Experimentation of the institution.
Clinical data from adult LT recipients performed between January 2002 and July 2012 at the Liver and Gastrointestinal Transplant Division, Department of Gastroenterology, School of Medicine, University of São Paulo, Brazil were reviewed retrospectively. After exclusion of patients who received split-liver transplantation, re-transplantation, or living donor LT, were studied 31 patients with combined liver and kidney transplantation (CLKT) and 592 patients with LT alone. Specifically, were analyzed variables that included gender, age, indication for transplantation, MELD score, incidence of LT alone and CLKT based upon MELD score and survival rate (overall survival) over the course of this 10 and 5-year study period.
Were collected data from the São Paulo Health Secretariat registry in the official government website (www.saude.gov.sp.br/transplante) where 3,961 unselected adult LT recipients were enrolled during the same study period in a large neighboring area (São Paulo State) that includes this and more than 15 other institutions.
The MELD score was utilized for the LT allocation system in Brazil since July 2006, replacing the previous chronological allocation system. Therefore, were compared the results from these two treatment groups: pre-MELD era from January 2002 to July 2006, and post-MELD era from July 2006 to July 2012.
Almost all surgical transplantation procedures were performed using a piggyback technique. University of Wisconsin and Custodiol were the preservation solutions most commonly employed. While the immunosuppressive regimen was customized to each patients, all patients received a steroid bolus during the anhepatic phase, steroid administration was tapered subsequently with complete cessation three to six months after transplantation; calcineurin inhibitor (tacrolimus or cyclosporine) was administered to all patients; mycophenolate mofetil was given to patients with CLKT or renal dysfunction.
Statistical analyses were performed using the SPSS 20.0 software package. Overall patient survival analyses were conducted using the Kaplan-Meier method (Log Rank; Mantel-Cox). Mean and median values and standard deviations were used to examine normally distributed variables. Student's t-test for unpaired data was used for comparisons. The chi-square test was used for comparing the frequencies of the liver transplantation modalities. P-values less than 0.05 were considered statistically significant.
RESULTS
Clinical profile
In this study, were analyzed all LT performed at the center over the course of ten years. A high prevalence of male referred to both modalities of transplantation was observed. The mean age of patients was also similar in both treatment groups, with a predominance of middle-aged males.
In patients who underwent CLKT, the average MELD score was 26.2, and the scores ranged from 16 to 37. For the CLKT, the warm and total liver ischemia time ranged, respectively, from 35 to 90 minutes (mean ± SD 48.29 ±11.89) and from 4.5 to 13.7 hours (7.76±2.30). The main indication for CLKT transplantation was hepatitis C cirrhosis (25.8%), followed by alcoholic cirrhosis (22.5%), hepatitis B cirrhosis (16.1%), cryptogenic cirrhosis (12.9%), and autoimmune hepatitis (9.7%). Combined HBV and HCV cirrhosis occurred in one case (3.22%), and other causes such as primary sclerosing cholangitis and Caroli disease occurred in three cases (9.7%).
Patient survival rates
Mean and median survival rates and overall survival over the ten and five years of the study are shown in Table 1. The overall survival rates of patients in the CLKT and LT alone groups were approximately 68% and 75%, respectively. Survival in the short and long term was similar for the two types of transplantation, although was observed a decrease in the long-term survival of the CLKT group (Table 1). There were no significant differences in survival between the transplantation modalities.
TABLE 1.
Mean and median survival time (ten years) for combined liver and kidney transplantation and liver transplantation alone and one and five year survival rate
| p* | ||||
|---|---|---|---|---|
| Mean | 67.8±10.1 | 75.0 ± 2.2 | 74.7 ± 2.2 | NS |
| Median | 60.0±28.7 | 84.0 ±6.6 | 84.0 ± 6.5 | NS |
| One year survival | 85% | 85% | 85% | - |
| Five years survival | 50% | 65% | 60% | - |
CLKT =combined liver and kidney transplantation; LTA; ± =mean and standard error; p =0.620 (NS)
Pre-MELD and post-MELD era
In the post-MELD era group, all patients transplanted in São Paulo State had a mean MELD score of 28.5, with a median of 29 and a mode of 24. Regarding the LT only procedures performed at this institution, the MELD´s mean, median and mode values were 30.5, 29 and 29, respectively.
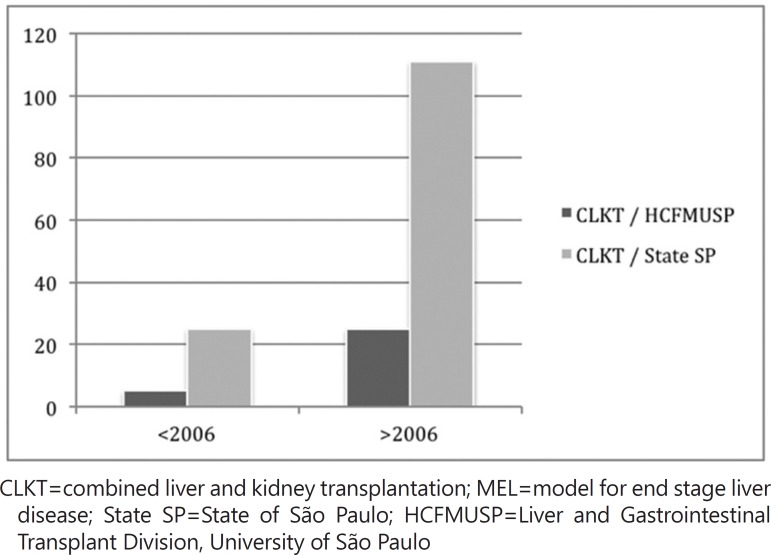
CLKT was performed more frequently during the post-MELD era, as demonstrated in Table 2 and Figure 1. The rate of CKLT rose globally from 2.1% to 4% in the post-MELD era, this increase was highly statistically significant (p<0.0001).
TABLE 2.
Comparison of all transplants performed in State of São Paulo from MELD era
| p value | |||||
|---|---|---|---|---|---|
| HCFMUSP | 158 (96.3) | 6 (3.7) | 479 (95) | 25 (5) | 0.46 |
| SP state | 989 (98.1) | 19 (1.9) | 2201 (96.3) | 85 (3.7) | <0.001 |
| Total | 1147 (97.9) | 25 (2.1) | 2680 (96) | 109 (4) | <0.001 |
CLKT=combined liver and kidney transplantation; LTA=liver transplantation alone; ±=mean and standard error number and percentage; MELD era: model for end-stage liver disease (after 2006)
FIGURE 1.
Number of transplants performed in the State of São Paulo and the Liver and Gastrointestinal Transplant Division, University of São Paulo, before and after 2006 (adoption of MELD score), 2002 to 2012
DISCUSSION
In this study, were examined the outcomes of liver transplantations performed at a large center in Brazil and compared with the results obtained in the State of São Paulo. Were assessed the outcomes of LT performed at a large center in Brazil and compared the patient survival rates of the combined liver and kidney transplantation and liver transplantation alone. These results showed no differences in the overall survival rates of these transplantation modalities.
The overall one and 5-year survival rates of patients who underwent liver transplantation (either combined or single procedure) were 85% and 60%, respectively. The short-term survival results were similar for both modalities, but was observed prolonged long-term survival in the LT alone group. The similar survival rate in both groups is interesting, considering the predictive morbidity factors found in patients who underwent CLKT.
The MELD scores of patients who underwent transplantation before 2006 was lower than those referred for an intervention after 2006. This was expected, and as a result of the higher degree of severity of patients transplanted after 2006, their prognosis was poorer. This finding is consistent with that reported in other countries 8,7,9,10,4,1.
In Brazil, the absolute number of observed LT is relatively large, approximately 1,500 per year. However, the number of donations per million of population is approximately ten, less than in the U.S. and Europe 2,7. In this study, the mismatch between supply and demand resulted in the MELD score to rise, and increased the number of transplants after the adoption of the MELD score.
CONCLUSION
The adoption of the MELD score increased the number of liver transplants performed in São Paulo.
Footnotes
Conflicts of interest: none
Financial source: none
REFERENCES
- 1.Aguilera V, Ferrer I, Berenguer M, Rivera J, Rubín Á, Moya Á, et al. Comparison of results of combined liver-kidney transplantation vs: isolated liver transplantation. Ann Hepatol. 2013;12(2):274–281. [PubMed] [Google Scholar]
- 2.Bloom RD, Bleicher M. Simultaneous liver-kidney transplantation in the MELD era. Adv Chronic Kidney Dis. 2009;16(4):268–277. doi: 10.1053/j.ackd.2009.05.005. [DOI] [PubMed] [Google Scholar]
- 3.Charlton MR, Wall WJ, Ojo AO, Gines P, Textor S, Shihab FS, et al. Report of the first international liver transplantation society expert panel consensus conference on renal insufficiency in liver transplantation. Liver transplantation : official publication of the American Association for the Study of Liver Diseases and the International Liver Transplantation Society. 2009;15(11):S1–S34. doi: 10.1002/lt.21877. [DOI] [PubMed] [Google Scholar]
- 4.Kiberd B, Skedgel C, Alwayn I, Peltekian K. Simultaneous liver kidney transplantation: a medical decision analysis. Transplantation. 2011;91(1):121–127. doi: 10.1097/tp.0b013e3181fcc943. [DOI] [PubMed] [Google Scholar]
- 5.Ma Y, Wang GD, He XS, Li Q, Li JL, Zhu XF, et al. Simultaneous liver and kidney transplantation: analysis of a single-center experience. Chinese medical journal. 2010;123(10):1259–1263. [PubMed] [Google Scholar]
- 6.Nacif LS, Andraus W, Haddad LB, Pinheiro RS, D'Albuquerque LAC. MELD Era Increases the Number of Combined Liver and Kidney Transplantations. Liver. 2013;2:124–124. doi: 10.4172/2167-0889.1000124. [DOI] [Google Scholar]
- 7.Nadim MK, Sung RS, Davis CL, Andreoni KA, Biggins SW, Danovitch GM, et al. Simultaneous liver-kidney transplantation summit: current state and future directions. Am J Transplant. 2012;12(11):2901–2908. doi: 10.1111/j.1600-6143.2012.04190.x. [DOI] [PubMed] [Google Scholar]
- 8.Schmitt TM, Kumer SC, Al-Osaimi A, Shah N, Argo CK, Berg C, et al. Combined liver-kidney and liver transplantation in patients with renal failure outcomes in the MELD era. Transpl Int. 2009;22(9):876–883. doi: 10.1111/j.1432-2277.2009.00887.x. [DOI] [PubMed] [Google Scholar]
- 9.Weber ML, Ibrahim HN, Lake JR. Renal dysfunction in liver transplant recipients: evaluation of the critical issues. Liver Transpl. 2012;18(11):1290–1301. doi: 10.1002/lt.23522. [DOI] [PubMed] [Google Scholar]
- 10.Zhu XF, He XS, Chen GH, Chen LZ, Wang CX, Huang JF. Combined liver and kidney transplantation in Guangzhou, China. Hepatobiliary Pancreat Dis Int. 2007;6(6):585–589. [PubMed] [Google Scholar]