Abstract
This study aimed to establish feasibility for myocardial speckle tracking (MST) and intra-observer reliability of both MST and tissue velocity imaging (TVI)-derived right ventricular (RV) strain (ϵ) and strain rate (SR) at rest and during upright incremental exercise. RV ϵ and SR were derived using both techniques in 19 healthy male participants. MST-derived ϵ and SR were feasible at rest (85% of segments tracked appropriately). Feasibility reduced significantly with progressive exercise intensity (3% of segments tracking appropriately at 90% maximum heart rate (HRmax)). Coefficient of variations (CoVs) of global ϵ values at rest was acceptable for both TVI and MST (7–12%), with low bias and narrow limits of agreement. Global SR data were less reliable for MST compared with TVI as demonstrated with CoV data (systolic SR=15 and 61%, early diastolic SR=16 and 17% and late diastolic SR=26 and 31% respectively). CoVs of global RV ϵ and SR obtained at 50% HRmax were acceptable using both techniques. As exercise intensity increased to 70 and 90% HRmax, reliability of ϵ and SR values reduced with larger variability in MST. We conclude that RV global and regional ϵ and SR data are feasible, comparable and reliable at rest and at 50% HRmax using both MST and TVI. Reliability was reduced during higher exercise intensities with only TVI acceptable for clinical and scientific use.
Keywords: right ventricle, exercise echocardiography, tissue Doppler and strain echocardiography, strain rate imaging
Introduction
Recent developments in novel echocardiographic techniques such as myocardial speckle tracking (MST) and tissue velocity imaging (TVI) have led to their application in the assessment of regional and global myocardial deformation (1, 2, 3). Both techniques have been validated for the assessment of the left ventricle (LV) in vitro (1, 4, 5) and in vivo (6, 7) and although some studies highlight agreement between techniques (8, 9) others have demonstrated contradictory values (10, 11, 12).
Right ventricular (RV) function is inherently difficult to assess, given its location, orientation and excess trabeculation (13). Both MST and TVI may overcome some of the limitations of standard echocardiography and hence have been applied to the assessment of RV systolic and diastolic function at rest (14, 15, 16) and during exercise (17). In view of this, the clinical application of both techniques at rest and during exercise may aid the diagnosis and serial management of conditions including pulmonary hypertension, RV infarction, arrhythmogenic RV cardiomyopathy (ARVC) and congenital heart disease.
In order to establish the usefulness of values obtained from MST- and TVI-derived ϵ and SR, feasibility, comparability (consistency between methods) and intra-observer reliability must be established. Attributing any differences between repeated measurements to a disease process, a clinical intervention or other changes in physiological state (e.g. exercise) must be done with careful consideration of the degree of measurement error or bias. A number of studies present reliability data as an aside to the primary focus, and although acceptable reliability is often established, the specific methodology is not transparent and minimal attention has been paid to study design (8, 11). Often, reliability data are obtained from the same acquisition which does not provide a true reflection of the clinical or research application, and ultimately establishes the reliability of the software only. To the best of our knowledge, there is only one study in the public domain that has assessed intra-observer reliability of RV ϵ and strain rate (SR) using a repeated acquisition within subject, within-day design. This was, however, limited to the resting values of global MST-derived RV ϵ and SR only (15). Furthermore, the American Society of Echocardiography guidelines (18) recommend to carry out all echocardiographic assessments with subjects in the left lateral decubitus position, but images obtained in alternate positions may be useful in clinical and research situations whereby loading, filling and blood flow are assessed. Of particular interest is the upright position, as in reality the physiological demands on the RV during exercise are often in this position. It is important to consider the effects of gravity on RV physiology, especially with respect to filling, and the impact of this on subsequent physiological function during exercise. Although these effects may be minimal, the assessment of RV function in the upright position may add value where a true functional assessment of the RV during exercise is required. The feasibility, comparability and reliability of MST and TVI in seated subjects at rest or during exercise are also unknown and it is therefore pertinent to investigate.
In view of these issues, the aims of this study are i) to establish the feasibility of MST-derived RV ϵ and SR at rest and during exercise at progressive intensities, ii) to compare the absolute values of global and regional RV ϵ and SR obtained from MST and TVI techniques at supine rest, upright rest and progressive intensity upright exercise, and iii) to establish the intra-observer reliability of global and regional RV ϵ and SR from both techniques at rest and during progressive exercise.
Methods
We aimed to provide the best case feasibility and reliability for MST and TVI by using young, healthy male subjects for all image acquisitions. Furthermore, the process of image optimisation was blinded (no reference to previous scans) within a repeated measures design to best reflect clinical and research practice.
Sample population
Nineteen participants (mean±s.d. age (range) of 21±2 (19–27) years) were recruited to take part in the study. All participants self-reported; being free of known cardiovascular disease, not taking any medication, no early family history of cardiovascular disease and not suffering from any other co-morbidities including diabetes, renal disease, respiratory disease or liver disease. Ethics approval was granted by the Liverpool John Moores Ethics Committee and all subjects provided written informed consent.
Study design
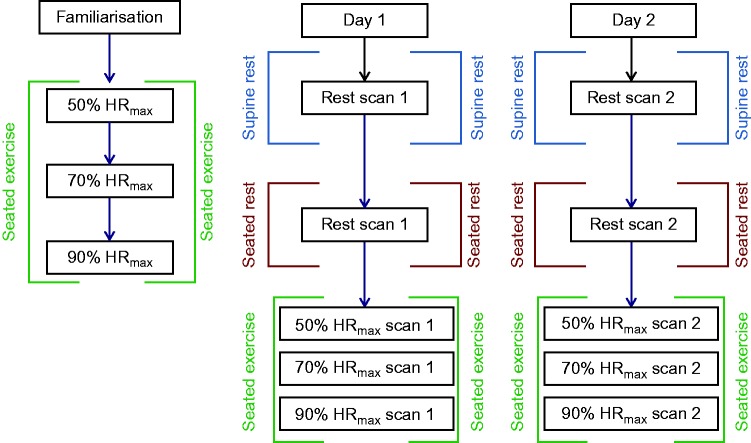
The study was undertaken using a repeated measures design (see Fig. 1). In brief, participants attended the laboratory on three separate occasions at the same time of day, having abstained from alcohol, exercise training and caffeine for a minimum of 24 h before exercise testing. On arrival at each session, standard anthropometric assessment of body mass and height was carried out before testing. The cycling exercise protocol was undertaken on the same cycle ergometer (Baum Electronics, Flörsheim am Main, Germany). Maximum heart rate (HRmax) for each participant was calculated according to the World Health Organisation (WHO) guideline equation: HRmax =220 (beats/min)−Age (years).
Figure 1.
Flow chart detailing methodological sequence for data acquisition.
Session 1
The initial testing session comprised a familiarisation trial on the cycle ergometer to obtain the specific workloads required to achieve and maintain 50, 70 and 90% HRmax at a steady-state. Furthermore, echocardiographic acoustic windows were assessed to ensure optimal image quality for MST whilst a 12-lead electrocardiogram (ECG) (Cardiopress, Spacelabs, Snoqualmie, WA, USA) was undertaken to assess for any underlying cardiovascular disease (19). Systolic and diastolic blood pressure was assessed via standard auscultation of the left brachial artery (Dinamap pro, GE Medical, Horten, Norway) during resting and exercising.
Sessions 2 and 3
Sessions 2 and 3 followed an identical format 4 days apart. Following 10 min supine rest, brachial artery blood pressure was obtained and echocardiographic assessments were undertaken with the participant in the left lateral decubitus position. The participants were then transferred to a cycle ergometer, and blood pressure and echocardiography were repeated in a seated position at rest. The participants commenced exercise on the cycle ergometer at the workload required to achieve 50, 70 and 90% HRmax in a progressive order. After at least 1 min at a steady-state HR, at each exercise stage, echocardiography was undertaken for 2 min whilst heart rate was maintained.
Echocardiography
All images were acquired using a commercially available ultrasound system (Vivid Q, GE Medical) with a 1.5–4 MHz phased array transducer. All images were acquired by the same single sonographer. Whilst the sonographer was not blinded to the participant or test session, there was no access to, or assessment of, session 2 images before the completion of data collection in session 3 in an attempt to remove systematic bias. Images were recorded to a DVD in raw DICOM format and offline analysis was performed by the same sonographer using commercially available EchoPac software (Version 7, GE Medical). All parameters were presented as an average of three cardiac cycles.
2D myocardial speckle tracking
A standard 2D echocardiography was used to obtain a modified, lateral apical four chamber view for MST-derived ϵ imaging of the RV lateral wall (see Fig. 2) (20). For all MST images, 2D frame rates were acquired as high as possible but not above 90 frames per second (FPS). The images were optimised using gain, sector width and dynamic range, depth, frequency and sector angle with the focal point positioned at mid-RV cavity level. Offline analysis involved placing the region of interest around the RV lateral wall only from base to apex. Regional peak longitudinal ϵ and systolic (SRS), early diastolic (SRE) and late diastolic (SRA) SRs were obtained for RV basal, mid and apical wall segments. Global peak ϵ and SR were calculated as an average of the three RV myocardial segments. The MST software grades each segment depending on its ability to fit the tracking algorithm (21) and assigns it as acceptable or unacceptable. In addition to this, the sonographer independently assessed the 2D images to ensure appropriate tracking.
Figure 2.
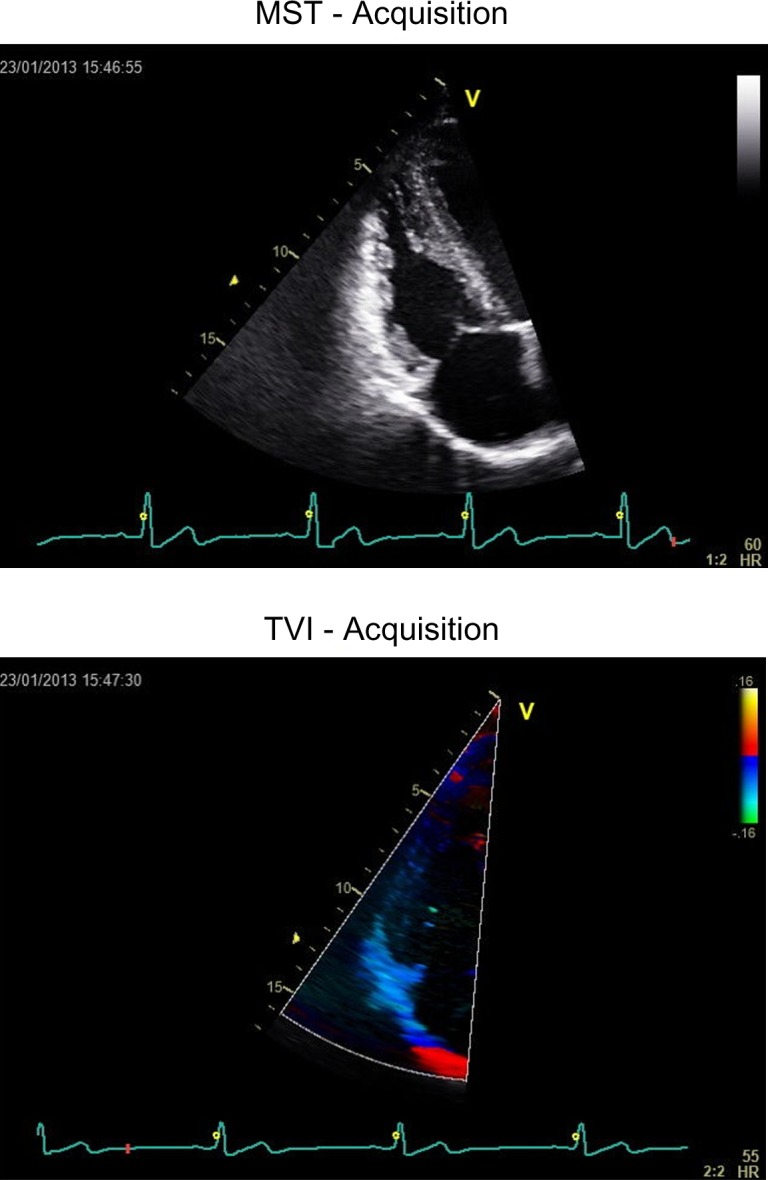
MST and TVI images demonstrating orientation for image acquisition.
Tissue velocity imaging
The apical four-chamber view was modified to ensure that the longitudinal movement of the RV lateral wall was aligned with the ultrasound beam and a colour tissue velocity region of interest (ROI) was superimposed. A narrow sector was utilised to obtain frame rates in excess of 200 FPS and gain, filter, pulse repetition frequency and depth were adjusted to optimise colour saturation and eliminate aliasing. All TVI acquisitions were analysed offline using the same software package and a large sample volume of 24 mm×4 mm was used to maximise the capture of either the basal, mid or apical segment, while ensuring similar segment size to that used during speckle-tracking analysis. The sample was anchored to the myocardium and adjusted throughout the cardiac cycle to ensure consistency of its anatomical position. Longitudinal ϵ, SRS, SRE and SRA were obtained for each segment and a global value was calculated as an average of all three segments.
Feasibility
For MST, both the software and an independent observer assessed the number of appropriately tracked segments at rest and during each exercise intensity, and this was converted to a percentage score.
Statistical analysis
All peak data are presented as mean±s.d. for each acquisition. To maximise comparison to past studies, we report a range of statistics related to the consistency of echocardiographic measures obtained in repeat scans. Intra-observer within-participant reliability was evaluated for both MST and TVI using repeated measures ANOVA (to assess systematic bias in the measurements) and coefficients of variation (CoV) to assess random error or noise (22). Bland-Altman's 95% limits of agreement (LoA) were also calculated as an indication of the typical error associated with these parameters. Statistical significance was set as P<0.05 for all statistical tests. In order to assess the agreement between MST and TVI methods, a paired t-test and Bland-Altman analysis of LoA were undertaken.
Results
Feasibility of MST and TVI
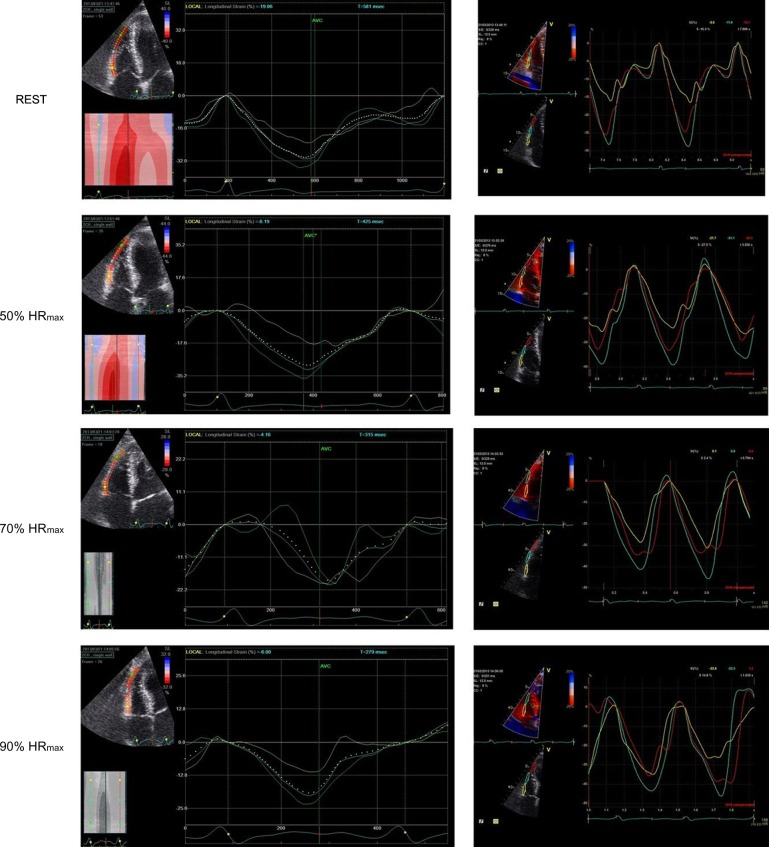
Fifty-seven segments were available for analysis at each time point. For MST-derived ϵ and SR, the successful completion of analysis on these segments as determined by the software and an experienced operator at supine rest was 86 and 89% and 85 and 80% at seated rest respectively. During incremental exercise, the absolute number of successfully ‘trackable’ segments reduced significantly with increasing heart rates for the assessment undertaken by both software and operator. Successful tracking percentages for the experienced operator were 59, 21 and 3% for 50, 70 and 90% HRmax respectively. Due to the anchoring nature of TVI-derived ϵ and SR, the quantification of feasibility is not possible; however unlike MST-derived indices, when assessed subjectively all segments adequately followed myocardial movement at all exercise intensities. An example of the variation in ϵ at each % HRmax as determined by both MST and TVI is presented in Fig. 3.
Figure 3.
Exemplar results for a single participant demonstrating MST and TVI derived ϵ curves at rest and incremental exercise intensities.
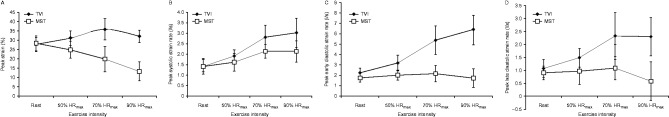
Comparability of global peak values
At rest, data derived from MST and TVI were similar (P>0.05) with the exception of SRE (P=0.003, see Fig. 4). During exercise, data derived from the two techniques were significantly different with TVI resulting in higher peak values than MST for all variables (P<0.03, see Fig. 4). Interestingly, peak values of ϵ and SR decreased at higher intensities when assessed with MST, conversely TVI-derived ϵ and SR data demonstrated a physiological response with increased deformation at higher heart rates.
Figure 4.
Comparison of absolute values derived from both techniques for global RV ϵ (A), SRS (B), SRE (C) and SRA (D).
Reliability
All reliability data are presented in Tables 1 and 2. No systematic bias was shown for MST and TVI-derived RV global or regional ϵ or SR at rest and during incremental exercise (P>0.05).
Table 1.
Intra-observer reliability and absolute mean±s.d. values for RV ϵ and SR at rest in two body positions
| TVI scan 1 | TVI scan 2 | CoV | LoA | MST scan 1 | MST scan 2 | CoV | LoA | |
|---|---|---|---|---|---|---|---|---|
| REST supine ϵ | ||||||||
| Global (%) | −28±4 | −27±2 | 7 | −0.4 (−5.3 to 4.6) | −28.36±3.95 | −28.86±2.40 | 12 | 0.5 (−7.3 to 8.3) |
| Basal (%) | −27±6 | −25±7 | 17 | −2.4 (−14.2 to 9.4) | −29.75±5.58 | −30.56±6.76 | 18 | 0.9 (−13.2 to 14.9) |
| Mid (%) | −30±6 | −32±5 | 12 | 1.9 (−7.8 to 11.6) | −30.21±6.45 | −29.00±5.22 | 12 | −0.3 (−10.1 to 9.5) |
| Apical (%) | −26±8 | −25±9 | 17 | −0.7 (−11.5 to 10.1) | −27.28±8.43 | −26.97±8.63 | 85 | −0.3 (−24.5 to 23.85) |
| REST seated ϵ | ||||||||
| Global (%) | −27±4 | −26±4 | 8 | −0.4 (−6.4 to 5.6) | −26.56±3.67 | −25.78±4.24 | 12 | −0.8 (−15.6 to 14) |
| Basal (%) | −28±8 | −31±5 | 17 | −1.5 (−13.3 to 10.2) | −28.31±8.28 | −30.53±5.08 | 43 | 2.2 (−13.7 to 18.1) |
| Mid (%) | −29±3 | −29±5 | 15 | 1.0 (−9.9 to 11.9) | −29.30±3.41 | −28.70±5.41 | 13 | −0.6 (−9.7 to 8.5) |
| Apex (%) | −23±7 | −19±10 | 14 | −0.6 (−9.8 to 8.5) | −23.32±7.36 | −19.3±10.02 | 46 | −4.0 (−21.6 to 13.5) |
| REST supine SRS | ||||||||
| Global (l/s) | −1.49±0.30 | −1.53±0.31 | 15 | 0.0 (−0.5 to 0.6) | −1.45±0.41 | −1.54±0.21 | 61 | 0.1 (−0.7 to 0.8) |
| Basal (l/s) | −1.38±0.47 | −1.29±0.43 | 29 | −0.1 (−1.1 to 0.9) | −2.00±0.6 | −2.01±0.57 | 29 | 0.0 (−1.4 to 1.5) |
| Mid (l/s) | −1.59±0.32 | −1.79±0.45 | 22 | 0.3 (−0.7 to 1.2) | −1.71±0.43 | −1.66±0.4 | 27 | −0.1 (−1.2 to 1.1) |
| Apical (l/s) | −1.56±0.52 | −1.61±0.37 | 24 | 0.0 (−0.8 to 0.9) | −1.64±0.43 | −1.74±0.44 | 34 | 0.1 (−1 to 1.2) |
| REST seated SRS | ||||||||
| Global (l/s) | −1.53±0.43 | −1.59±0.54 | 11 | 0.1 (−0.5 to 0.6) | −1.53±0.27 | −1.42±0.32 | 32 | −0.1 (−0.9 to 0.7) |
| Basal (l/s) | −1.40±0.66 | −1.54±0.69 | 24 | 0.1 (−0.6 to 0.9) | −2.39±0.7 | −2.37±0.58 | 25 | 0.0 (−1.5 to 1.4) |
| Mid (l/s) | −1.76±0.53 | −1.75±0.50 | 11 | 0.0 (−0.5 to 0.5) | −1.87±0.25 | −1.86±0.41 | 17 | 0.0 (−0.8 to 0.8) |
| Apical (l/s) | −1.45±0.31 | −1.48±0.56 | 29 | 0.0 (−0.9 to 0.9) | −1.59±0.28 | −1.5±0.73 | 49 | −0.1 (−1.5 to 1.3) |
| REST supine SRE | ||||||||
| Global (l/s) | 2.23±0.48 | 2.18±0.37 | 16 | 0.0 (−0.8 to 0.9) | 1.75±0.4 | 1.76±0.24 | 17 | 0.0 (−0.7 to 0.7) |
| Basal (l/s) | 2.23±0.69 | 2.41±0.71 | 27 | −0.2 (−1.5 to 1.1) | 3.04±1.03 | 2.59±0.79 | 40 | 0.5 (−2 to 2.9) |
| Mid (l/s) | 2.24±0.68 | 2.32±0.46 | 21 | −0.1 (−1.3 to 1.1) | 1.78±0.57 | 1.87±0.45 | 20 | −0.1 (−1 to 0.8) |
| Apical (l/s) | 2.21±0.98 | 1.81±0.58 | 34 | 0.4 (−1.4 to 2.2) | 1.90±0.73 | 1.79±0.66 | 90 | 0.1 (−2.1 to 2.3) |
| REST seated SRE | ||||||||
| Global (l/s) | 2.11±0.55 | 2.29±0.57 | 16 | −0.2 (−1.1 to 0.7) | 1.77±0.35 | 1.67±0.34 | 20 | 0.1 (−0.8 to 1.0) |
| Basal (l/s) | 2.30±0.85 | 2.53±0.83 | 27 | −0.2 (−1.7 to 1.3) | 2.85±0.93 | 2.78±0.76 | 26 | 0.1 (−1.8 to 1.9) |
| Mid (l/s) | 2.17±0.63 | 2.28±0.71 | 23 | −0.1 (−1.5 to 1.3) | 2.04±0.49 | 1.93±0.52 | 33 | 0.1 (−1.5 to 1.7) |
| Apical (l/s) | 1.84±0.60 | 2.07±0.62 | 35 | −0.2 (−1.8 to 1.4) | 1.68±0.72 | 1.44±0.72 | 81 | 0.2 (−1.7 to 2.1) |
| REST supine SRA | ||||||||
| Global (l/s) | 1.07±0.34 | 1.08±0.34 | 26 | 0.0 (−0.8 to 0.7) | 0.90±0.26 | 0.93±0.21 | 31 | 0.0 (−0.7 to 0.6) |
| Basal (l/s) | 1.01±0.39 | 0.98±0.46 | 36 | 0.1 (−0.8 to 0.9) | 1.14±0.47 | 1.18±0.31 | 37 | 0.0 (−1.1 to 1.1) |
| Mid (l/s) | 1.27±0.56 | 1.31±0.62 | 45 | 0.0 (−1.2 to 1.1) | 1.26±0.38 | 1.13±0.38 | 26 | 0.1 (−0.7 to 1) |
| Apical (l/s) | 0.91±0.44 | 0.97±0.61 | 66 | 0.1 (−1.5 to 1.3) | 1.06±0.57 | 1.03±0.42 | 189 | 0.0 (−1.3 to 1.4) |
| REST seated SRA | ||||||||
| Global (l/s) | 0.94±0.28 | 1.06±0.33 | 21 | −0.1 (−0.6 to 0.4) | 0.86±0.26 | 0.81±0.29 | 33 | 0.1 (−0.5 to 0.6) |
| Basal (l/s) | 0.92±0.51 | 1.19±0.55 | 31 | −0.3 (−1.1 to 0.6) | 1.39±0.62 | 1.31±0.43 | 46 | 0.1 (−1.2 to 1.4) |
| Mid (l/s) | 1.08±0.37 | 1.15±0.49 | 34 | −0.1 (−0.9 to 0.8) | 1.07±0.29 | 0.97±0.43 | 39 | 0.1 (−0.6 to 0.8) |
| Apical (l/s) | 0.81±0.41 | 0.83±0.33 | 54 | 0.0 (−1 to 0.9) | 0.82±0.38 | 0.77±0.44 | 58 | 0.1 (−0.6 to 0.7) |
Table 2.
Intra-observer reliability and absolute mean±s.d. values for RV ϵ and SR during incremental exercise
| TVI scan 1 | TVI scan 2 | CoV | LoA | MST scan 1 | MST scan 2 | CoV | LoA | |
|---|---|---|---|---|---|---|---|---|
| 50% ϵ | ||||||||
| Global (%) | −31±5 | −32±4 | 7 | 0.4 (−5.3 to 6.1) | −25±5 | −26±4 | 14 | 0.9 (6.9 to 8.8) |
| Basal (%) | −34±8 | −35±8 | 16 | 0.9 (−14.7 to 16.5) | −28±8 | −29±8 | 38 | 1.0 (−22.9 to 25.1) |
| Mid (%) | −34±5 | −34±7 | 12 | −0.3 (−10.8 to 10.2) | −26±5 | −27±7 | 23 | 0.6 (−9.6 to 10.7) |
| Apical (%) | −27±8 | −27±10 | 17 | 0.3 (−13 to 13.5) | −22±8 | −22±10 | 89 | −0.3 (−19.7 to 19.2) |
| 70% ϵ | ||||||||
| Global (%) | −36±7 | −35±7 | 11 | −1.3 (−12.1 to 9.5) | −20±7 | −19±7 | 73 | −0.8 (−15.6 to 14.0) |
| Basal (%) | −37±8 | −37±10 | 23 | 0.4 (−22 to 22.7) | −27±8 | −26±10 | 33 | −0.9 (−20.6 to 18.7) |
| Mid (%) | −38±7 | −36±7 | 23 | −2.6 (−24.2 to 18.9) | −21±7 | −20±7 | 63 | −0.9 (−17.6 to 15.8) |
| Apical (%) | −32±10 | −31±7 | 22 | −1.5 (−18.6 to 15.6) | −15±10 | −13±7 | 175 | −2.5 (−23.0 to 18.2) |
| 90% ϵ | ||||||||
| Global (%) | −32±5 | −33±5 | 8 | 0.7 (−6.7 to 8) | −13±5 | −13±5 | 67 | −0.9 (−12.8 to 11.1) |
| Basal (%) | −35±7 | −37±6 | 32 | 1.9 (−23.7 to 27.5) | −19±7 | −18±6 | 59 | −1.5 (−21.7 to 18.7) |
| Mid (%) | −33±7 | −34±8 | 20 | 1.0 (−17 to 19) | −14±7 | −15±8 | 46 | 1.1 (−17.0 to 19.3) |
| Apical (%) | −28±7 | −27±7 | 25 | −0.9 (−17.6 to 15.8) | −13±7 | −10±7 | 104 | −2.4 (−22.8 to 18.1) |
| 50% SRS | ||||||||
| Global (l/s) | −1.96±0.32 | −2.15±0.61 | 16 | 0.2 (−0.8 to 1.2) | −1.66±0.43 | −1.81±0.28 | 33 | 0.2 (−0.7 to 1.1) |
| Basal (l/s) | −2.04±0.59 | −2.33±1.21 | 30 | 0.3 (−1.8 to 2.4) | −2.93±0.95 | −2.96±0.95 | 37 | 0.0 (−2.3 to 2.4) |
| Mid (l/s) | −2.04±0.34 | −2.27±0.47 | 16 | 0.2 (−0.7 to 1.2) | −2.03±0.58 | −2.16±0.52 | 44 | 0.1 (−1.2 to 1.4) |
| Apical (l/s) | −1.79±0.45 | −1.85±0.49 | 19 | 0.1 (−0.8 to 0.9) | −1.72±0.6 | −1.92±0.57 | 40 | 0.2 (−1.0 to 1.4) |
| 70% SRS | ||||||||
| Global (l/s) | −2.87±0.59 | −2.90±0.49 | 16 | 0.0 (−1.1 to 1.2) | −2.19±0.34 | −2.08±0.46 | 22 | −0.1 (−1.2 to 0.9) |
| Basal (l/s) | −3.10±1.09 | −2.94±1.07 | 25 | −0.2 (−2.1 to 1.8) | −3.46±0.8 | −3.65±0.99 | 35 | 0.2 (−2.8 to 3.2) |
| Mid (l/s) | −3.06±0.54 | −2.98±0.60 | 15 | −0.1 (−1.3 to 1.1) | −2.50±0.4 | −2.62±0.61 | 19 | 0.1 (−1.1 to 1.3) |
| Apical (l/s) | −2.49±0.89 | −2.80±0.88 | 31 | 0.3 (−1.3 to 1.9) | −2.51±0.85 | −2.59±0.8 | 40 | 0.1 (−2.3 to 2.4) |
| 90% SRS | ||||||||
| Global (l/s) | −3.09±0.70 | −3.04±0.51 | 13 | −0.1 (−1.1 to 1) | −2.18±0.52 | −1.98±0.48 | 28 | −0.2 (−1.4 to 1.0) |
| Basal (l/s) | −3.53±1.08 | −3.41±0.65 | 25 | −0.1 (−2.3 to 2) | −4.15±1.35 | −3.89±0.65 | 33 | −0.3 (−3.4 to 2.9) |
| Mid (l/s) | −3.01±1.08 | −3.48±0.90 | 32 | 0.5 (−1.9 to 2.8) | −2.82±0.6 | −2.66±0.74 | 28 | −0.2 (−2.0 to 1.6) |
| Apical (l/s) | −2.74±1.34 | −2.31±0.81 | 49 | −0.4 (−3 to 2.2) | −3.01±1.34 | −2.53±0.86 | 34 | −0.5 (−2.8 to 1.8) |
| 50% SRE | ||||||||
| Global (l/s) | 3.23±0.71 | 3.43±0.64 | 13 | −0.2 (−1.3 to 0.9) | 2.01±0.45 | 1.95±0.31 | 19 | 0.1 (−0.9 to 1.0) |
| Basal (l/s) | 3.70±1.29 | 4.23±1.56 | 26 | −0.5 (−2.6 to 1.6) | 3.19±1.10 | 2.87±0.93 | 58 | 0.3 (−2.9 to 3.6) |
| Mid (l/s) | 3.16±1.20 | 3.05±0.80 | 25 | 0.1 (−2.2 to 2.5) | 2.37±0.68 | 2.26±0.5 | 28 | 0.1 (−1.5 to 1.7) |
| Apical (l/s) | 2.82±0.90 | 3.00±0.92 | 31 | −0.2 (−2.3 to 1.9) | 2.03±0.7 | 2.26±0.5 | 54 | 0.0 (−2.0 to 1.9) |
| 70% SRE | ||||||||
| Global (l/s) | 5.38±1.58 | 5.23±1.20 | 19 | 0.2 (−2.4 to 2.7) | 2.17±0.79 | 2.06±0.6 | 71 | 0.1 (−1.5 to 1.8) |
| Basal (l/s) | 5.03±2.27 | 6.03±1.87 | 35 | −1.0 (−5.3 to 3.3) | 3.73±1.63 | 3.83±0.99 | 30 | −0.1 (−3.2 to 3.0) |
| Mid (l/s) | 5.90±2.44 | 5.21±1.64 | 29 | 0.7 (−3.4 to 4.8) | 2.58±0.92 | 2.65±0.49 | 51 | −0.1 (−1.8 to 1.7) |
| Apical (l/s) | 5.23±1.93 | 4.45±1.65 | 29 | 0.8 (−2.3 to 3.9) | 2.07±1.17 | 2.05±1.02 | 80 | 0.0 (−3.0 to 3.0) |
| 90% SRE | ||||||||
| Global (l/s) | 6.36±1.43 | 5.97±1.49 | 23 | 0.4 (−2.7 to 3.5) | 1.73±0.87 | 2.04±0.88 | 89 | −0.3 (−2.9 to 2.3) |
| Basal (l/s) | 6.42±2.53 | 7.01±1.59 | 29 | −0.6 (−5.1 to 4) | 3.02±1.35 | 3.93±0.65 | 211 | −0.9 (−5.0 to 3.2) |
| Mid (l/s) | 6.97±1.99 | 6.71±2.03 | 29 | 0.3 (−4.5 to 5) | 2.12±1.15 | 2.60±1.25 | 73 | −0.5 (−3.5 to 2.5) |
| Apical (l/s) | 5.56±1.93 | 4.57±1.89 | 54 | 1.0 (−4.5 to 6.5) | 2.18±1.43 | 1.95±1.22 | 271 | 0.2 (−3.4 to 3.9) |
| 50% SRA | ||||||||
| Global (l/s) | 1.48±0.36 | 1.47±0.40 | 14 | 0.0 (−0.5 to 0.5) | 0.96±0.51 | 1.05±0.44 | 78 | −0.1 (−1.1 to 0.9) |
| Basal (l/s) | 1.95±0.84 | 1.92±1.02 | 42 | 0.0 (−1.5 to 1.5) | 1.49±0.73 | 1.77±0.86 | 71 | −0.3 (−2.1 to 1.6) |
| Mid (l/s) | 1.51±0.73 | 1.36±0.60 | 42 | 0.2 (−1.2 to 1.5) | 1.16±0.61 | 1.33±0.44 | 24 | −0.2 (−1.2 to 0.9) |
| Apical (l/s) | 0.98±0.36 | 1.12±0.38 | 46 | −0.1 (−1.1 to 0.9) | 1.19±0.65 | 1.08±0.68 | 70 | 0.1 (−1.1 to 1.3) |
| 70% SRA | ||||||||
| Global (l/s) | 2.32±0.90 | 2.47±0.85 | 19 | −0.2 (−1.1 to 0.8) | 1.08±0.44 | 0.80±0.48 | 88 | 0.3 (−0.9 to 1.4) |
| Basal (l/s) | 2.66±1.59 | 2.53±1.30 | 58 | 0.1 (−2.2 to 2.5) | 2.55±0.92 | 2.08±1.3 | 83 | 0.5 (−2.4 to 3.4) |
| Mid (l/s) | 2.32±1.15 | 2.75±1.12 | 23 | −0.4 (−1.9 to 1.1) | 1.34±0.56 | 1.08±0.7 | 98 | 0.3 (−1.1 to 1.6) |
| Apical (l/s) | 1.77±1.04 | 1.88±0.99 | 46 | −0.1 (−2.1 to 1.8) | 1.34±0.93 | 0.93±0.7 | 125 | 0.4 (−1.9 to 2.7) |
| 90% SRA | ||||||||
| Global (l/s) | 2.29±0.74 | 2.40±0.82 | 18 | −0.1 (−1.2 to 1) | 0.58±0.75 | 0.69±0.67 | 89 | −0.1 (−2.1 to 1.8) |
| Basal (l/s) | 2.34±1.17 | 2.82±1.50 | 42 | −0.5 (−2.9 to 1.9) | 1.48±0.65 | 1.30±1.15 | 272 | 0.2 (−3.6 to 4.0) |
| Mid (l/s) | 2.30±0.91 | 2.31±1.11 | 52 | −0.0 (−2.7 to 2.6) | 0.71±0.84 | 1.07±0.99 | 158 | −0.4 (−2.8 to 2.1) |
| Apical (l/s) | 2.23±1.47 | 2.07±1.01 | 60 | 0.2 (−2.4 to 2.7) | 1.23±1.13 | 1.09±1.29 | 307 | 0.2 (−3.3 to 3.6) |
Rest
CoVs of global ϵ values were acceptable for both MST and TVI, ranging from 7 to 12%, with narrow LoA. Regional data demonstrated less favourable reliability data although values obtained from TVI were superior to MST. Data of the mid-wall segment were presented with the lowest between test variation for both techniques, whereas the poorest reliability was observed in the MST assessment of the apical wall segment. Global SR data were more consistent between tests, particularly for TVI when compared with MST as demonstrated with CoV data (SRS=15 and 61%, SRE=16 and 17% and SRA=26 and 31% respectively). That aside a narrow LoA bias was observed for both techniques, particularly of SRS and SRE. Regional SR data demonstrated greater intra-observer variability than global data, with more favourable data derived using TVI. There were no systematic differences in global or regional measures of reliability when the data were acquired in a seated position compared with supine position at rest.
Incremental exercise
CoVs and LoAs of global RV ϵ obtained from seated exercise at 50% HRmax were acceptable for both techniques. Global SR was less reliable using the MST technique. Regional data were more variable for both techniques compared with global measures (see Table 2). As exercise intensity increased to 70 and 90% HRmax, reliability of ϵ data decreased. Intra-observer reliability during exercise for both global ϵ and SR was only considered acceptable when derived from TVI. LoA widened proportional to exercise intensity, more so for MST than TVI (given in Table 2).
Discussion
The key findings from this study are the following: i) MST is feasible, producing physiological RV global and regional data when at rest in both supine and seated positions and during sub-maximal cycling exercise at 50% HRmax. At higher heart rates, MST is less feasible and does not provide physiological values of RV ϵ and SR. ii) TVI-derived RV ϵ provides similar values at rest; however, during exercise, TVI produced consistently higher values than MST. iii) Intra-observer reliability of global RV ϵ using both techniques at rest is good; however, regional data is more disparate with the apical segment providing the poorest reliability. Only TVI provided data with adequate reliability for global and regional measures for use during cycling exercise at higher heart rates.
Feasibility
The assessment of RV function using a conventional echocardiography is challenging and the introduction of myocardial ϵ imaging has provided potential to study RV mechanics at rest and during exercise (17, 23) and it is pertinent to establish feasibility during these conditions. The feasibility of MST-derived global and regional RV ϵ and SR at rest in this study is in line with values previously reported for the LV (9) (88%) and the RV (16) (93%) and therefore confirms its potential application. During exercise, the feasibility for MST ranged from 3 to 51% when compared with previously reported values of 18 to 38% (17). The inferior tracking seen in this study may be a consequence of operator exclusion as the specific methodology of computer vs operator tracking analysis has not been clearly described in previous work.
Comparability of global peak values
At rest, Teske et al. (16) assessed regional RV ϵ and SR values in patients with RV cardiomyopathy, endurance athletes and control subjects using TVI and MST, and reported similar values between techniques with a small bias towards greater values using TVI. Absolute values were significantly different between the three participant groups. La Gerche et al. (17) have previously compared RV global and regional ϵ derived using MST and TVI during exercise. They reported increased RV global ϵ with progressive exercise intensity when derived using TVI but a reduction in RV global ϵ when derived using MST as seen in this study. In view of our findings and their corroboration with La Gerche et al. (17), the in-exercise assessment of RV ϵ should be constrained to TVI methodology only. The absolute values derived using MST in-exercise presented herein are indicative of pathology, which is extremely unlikely given the current cohort. A number of possible explanations for this can be proposed. MST techniques are limited to a frame rate of ∼90 FPS due to the inability of the tracking algorithm to detect sufficient change in the myocardium speckle pattern as well as increased noise at high frame rates (24). This will have the effect of under sampling (a temporal resolution of ∼11 ms) with the potential of missing the true peak when changes in RV function are small in amplitude and fast acting (14). The higher frame rate for TVI (>200 FPS) appears to derive an absolute value in fitting with the known physiological response to exercise of increased RV ϵ and SR (17). It is also apparent that at higher exercise intensity, image quality deteriorates due to upper body movement and increased respiratory activity. MST is highly dependent on image quality and out-of-plane motion (21), more so than TVI-derived ϵ (2) and may, in part, explain the findings from this study. Furthermore, repeated image acquisitions especially during exercise are challenging to standardise for the RV due to the complex location, geometry, excess trabeculation and lack of anatomical markers.
Reliability
The data of this study is in agreement with Oxborough et al. (15) who reported similar intra-observer reliability data for MST-derived RV global ϵ at rest in a young male cohort (CoV 7%). A difference of 6% with respect to MST-derived global RV ϵ has been previously reported between elite athletes and controls (23) and a reduction of 8% in RV ϵ has been reported following percutaneous closure of an atrial-septal defect (25) and therefore observed changes in this magnitude should be interpreted with caution.
In-exercise echocardiography poses a number of challenges; however, upright exercise provides the ideal setting to establish a physiological understanding of the hearts capacity and reserve. A number of studies have utilised MST (9, 26, 27, 28, 29) and TVI (30, 31, 32, 33) during exercise to assess LV function. The application of MST and TVI to the RV during exercise has been limited. MST has been applied to determine the RV functional response between patients with ARVC and control post-stress testing, with values of ϵ increasing by 5 and 19% for ARVC and controls respectively (34). In view of our findings of poor reproducibility at higher rates, data of this nature require larger sample sizes and careful interpretation.
The intra-observer reliability of TVI and MST techniques in La Gerche's study decreased as exercise intensity increased, and RV global ϵ showed a bias towards TVI during exercise with LoA increasing to ∼−20 to 20% compared with ∼−10 to 10% in this study. Regional deformation was not assessed by La Gerche et al. (17) during exercise and further work is needed to determine if regional RV deformation derived during exercise is feasible given the poor intra-observer reliability for both techniques in this study.
Practical considerations
At rest, global ϵ and SR measures derived using either MST or TVI are feasible and comparable (with the exception of SRE SR). Repeat research and clinical assessments should consider utilising one methodology throughout to minimise variability. Not blinding the operator to the original images may help to standardise repeat RV image acquisitions using the previous images as a reference point. This may reduce the variability that is inherent to the techniques and may allude to routine clinical use. At present, care must be taken in attributing small changes within the boundaries of the measurement error reported in this study to any factor other than methodological variance. Given the data in this study, TVI is more appropriate for heart rates above 106 beats/min (as determined by average heart rate at 50% HRmax plus two s.d.). In-exercise assessment of RV function at higher heart rates is possible using TVI and could be applied for the diagnosis and monitoring conditions such as ARVC, pulmonary embolism and hypertension, and RV infarction as measurement error is comparable with changes seen in clinical assessments (14). TVI is more time consuming and fastidious compared with MST, and for clinical assessments, MST may provide a useful, reliable and time-efficient technique in patients whom HRmax is unlikely to be in excess of 50% HRmax during exercise testing. Global parameters as an average of the three myocardial segments provide superior reliability when compared with regional data for both techniques and should be considered for research and clinical practice.
Limitations
This study utilised a ‘best case’ reliability model using a homogenous group of young, fit, healthy male subjects and thus application of the intra-observer reliability data derived in this study to clinical populations should be done with caution. It is vital to expand on this method with different populations where image quality may be a defining factor in the techniques available to assess RV function. It would also be appropriate to assess inter-observer reliability of this method with the current population. It is also important to note that MST software is designed and recommended for use on the LV only and therefore the validity of this technique when applied to the RV remains unknown. Furthermore, the use of a large sample size for deriving TVI ϵ and SR allowed the direct comparison with the segments provided by the automated speckle analysis software and whilst this also reduces overall noise there is a trade-off with reduced axial resolution. In view of this, there is a potential for artefact-induced errors in absolute values; however, as our findings were comparative with other published data and a physiological response was observed during exercise, it is unlikely that this limitation had any impact on our results. Although previous studies assessing RV function immediately following exercise have transferred subjects to the left lateral decubitus position in accordance with ASE guidelines, the subsequent heart rate in healthy trained individuals may rapidly decrease in recovery creating an additional practical challenge. To assess RV function at a specific heart rate, the use of a supine cyclergometer could perhaps overcome the limitations of upright exercise scanning and may add value to an in-exercise echocardiographic assessment.
Conclusion
Global MST and TVI-derived ϵ and SR are feasible, comparable and reproducible at rest in supine and seated positions and up to 50% HRmax (cut-off 106 beats/min). At higher heart rates MST-derived RV ϵ and SR do not provide physiological values, and are less reproducible than TVI-derived values. Global parameters as an average of the three myocardial segments provide superior reliability when compared with regional data.
Acknowledgements
The authors thank all of our participants for volunteering their time for the study.
Declaration of interest
The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of the research reported.
Funding
This research did not receive any specific grant from any funding agency in the public, commercial or not-for-profit sector.
References
- 1. Langeland S D'hooge J Claessens T Claus P Verdonck P Suetens P Sutherland GR Bijnens B RF-based two-dimensional cardiac strain estimation: a validation study in a tissue-mimicking phantom IEEE Transactions on Ultrasonics, Ferroelectrics, and Frequency Control 51 2004. 1537–1546. 10.1109/TUFFC.2004.1367495 [DOI] [PubMed] [Google Scholar]
- 2. Sutherland GR Di Salvo G Claus P D'hooge J Bijnens B Strain and strain rate imaging: a new clinical approach to quantifying regional myocardial function Journal of the American Society of Echocardiography 17 2004. 788–802. 10.1016/j.echo.2004.03.027 [DOI] [PubMed] [Google Scholar]
- 3. Støylen A Heimdal A Bjørnstad K Wiseth R Vik-Mo H Torp H Angelsen B Skjaerpe T Strain rate imaging by ultrasonography in the diagnosis of coronary artery disease Journal of the American Society of Echocardiography 13 2000. 1053–1064. 10.1067/mje.2000.106573 [DOI] [PubMed] [Google Scholar]
- 4. Heimdal A Stoylen A Torp H Skjaerpe T Real-time strain rate imaging of the left ventricle by ultrasound Journal of the American Society of Echocardiography 11 1998. 1013–1019. 10.1016/S0894-7317(98)70151-8 [DOI] [PubMed] [Google Scholar]
- 5. Behlohlavek M Bartelson VB Zobitz ME Real-time strain rate imaging: validation of peak compression and expansion rates by tissue-mimicking phantom Echocardiography 18 2001. 565–571. 10.1046/j.1540-8175.2001.00565.x [DOI] [PubMed] [Google Scholar]
- 6. Korinek J Wang J Sengupta PP Miyazaki C Kjaergaard J McMahon E Abraham TP Belohlavek M Two-dimensional strain – a Doppler-independent ultrasound method for quantitative of regional deformation: validation in vitro and in vivo Journal of the American Society of Echocardiography 18 2005. 1247–1253. 10.1016/j.echo.2005.03.024 [DOI] [PubMed] [Google Scholar]
- 7. Urheim S Edvardsen T Torp H Angelsen B Smiseth OA Myocardial strain by Doppler echocardiography. Validation of a new method to quantify regional myocardial function Circulation 102 2000. 1158–1164. 10.1161/01.CIR.102.10.1158 [DOI] [PubMed] [Google Scholar]
- 8. Cho GY Chan J Leano R Strudwick M Marwick TH Comparison of two-dimensional speckle and tissue velocity based strain and validation with harmonic phase magnetic resonance imaging American Journal of Cardiology 97 2006. 1661–1666. 10.1016/j.amjcard.2005.12.063 [DOI] [PubMed] [Google Scholar]
- 9. Hanekom L Cho GY Leano R Jeffriess L Marwick TH Comparison of two-dimensional speckle and tissue Doppler strain measurement during dobutamine stress echocardiography: an angiographic correlation European Heart Journal 28 2007. 1765–1772. 10.1093/eurheartj/ehm188 [DOI] [PubMed] [Google Scholar]
- 10. Marwick TH Consistency of myocardial deformation imaging between vendors European Journal of Echocardiography 11 2010. 414–416. 10.1093/ejechocard/jeq006 [DOI] [PubMed] [Google Scholar]
- 11. Shave R George K Whyte G Middleton N Hart E Artis N Oxborough D A comparison of Doppler, tissue Doppler imaging, and strain rate imaging in the assessment of postexercise left ventricular function Applied Physiology, Nutrition, and Metabolism 34 2009. 33–39. 10.1139/H08-127 [DOI] [PubMed] [Google Scholar]
- 12. Oxborough D Batterham AM Shave R Artis N Birch KM Whyte G Ainslie PN George KP Interpretation of two-dimensional and tissue Doppler-derived strain (epsilon) and strain rate data: is there a need to normalize for individual variability in left ventricular morphology? European Journal of Echocardiography 10 2009. 677–682. 10.1093/ejechocard/jep037 [DOI] [PubMed] [Google Scholar]
- 13. Ho SY Nihoyannopoulos P Anatomy, echocardiography, and normal right ventricular dimensions Heart 92 2006. I2–I13. 10.1136/hrt.2005.077875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Jategaonkar SR Scholtz W Butz T Bogunovic N Faber L Horstkotte D Two-dimensional strain and strain rate imaging of the right ventricle in adult patients before and after percutaneous closure of atrial septal defects European Journal of Echocardiography 10 2009. 499–502. 10.1093/ejechocard/jen315 [DOI] [PubMed] [Google Scholar]
- 15. Oxborough D George K Birch K Intraobserver reliability of two-dimensional ultrasound derived strain imaging in the assessment of the left ventricle, right ventricle, and left atrium of healthy human hearts Echocardiography 29 2012. 793–802. 10.1111/j.1540-8175.2012.01698.x [DOI] [PubMed] [Google Scholar]
- 16. Teske AJ De Boeck BW Olimulder M Prakken NH Doevendans PA Cramer MJ Echocardiographic assessment of regional right ventricular function: a head-to-head comparison between 2-dimensional and tissue Doppler-derived strain analysis Journal of the American Society of Echocardiography 21 2008. 275–283. 10.1016/j.echo.2007.08.027 [DOI] [PubMed] [Google Scholar]
- 17. La Gerche A Burns AT D'Hooge J Macisaac AI Heidbüchel H Prior DL Exercise strain rate imaging demonstrates normal right ventricular contractile reserve and clarifies ambiguous resting measures in endurance athletes Journal of the American Society of Echocardiography 25 2012. 253–U139. 10.1016/j.echo.2011.11.023 [DOI] [PubMed] [Google Scholar]
- 18. Lang RM Bierig M Devereux RB Flachskampf FA Foster E Pellikka PA Picard MH Roman MJ Seward J Shanewise JS et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography's guidelines and standards committee and the chamber quantification writing group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology Journal of the American Society of Echocardiography 18 2005. 1440–1463. 10.1016/j.echo.2005.10.005 [DOI] [PubMed] [Google Scholar]
- 19. Corrado D Pelliccia A Heidbuchel H Sharma S Link M Basso C Biffi A Buja G Delise P Gussac I et al. Recommendations for interpretation of 12-lead electrocardiogram in the athlete European Heart Journal 31 2010. 243–259. 10.1093/eurheartj/ehp473 [DOI] [PubMed] [Google Scholar]
- 20. Rudski LG Lai WW Afilalo J Hua L Handschumacher MD Chandrasekaran K Solomon SD Louie EK Schiller NB Guidelines for the echocardiographic assessment of the right heart in adults: a report from the American Society of Echocardiography endorsed by the European Association of Echocardiography, a registered branch of the European Society of Cardiology, and the Canadian Society of Echocardiography Journal of the American Society of Echocardiography 23 2010. 685–713. 10.1016/j.echo.2010.05.010 [DOI] [PubMed] [Google Scholar]
- 21. Mor-Avi V Lang RM Badano LP Belohlavek M Cardim NM Derumeaux G Galderisi M Marwick T Nagueh SF Sengupta PP et al. Current and evolving echocardiographic techniques for the quantitative evaluation of cardiac mechanics: ASE/EAE consensus statement on methodology and indications endorsed by the Japanese Society of Echocardiography Journal of the American Society of Echocardiography 24 2011. 277–313. 10.1016/j.echo.2011.01.015 [DOI] [PubMed] [Google Scholar]
- 22. Vianna-Pinton R Moreno CA Baxter CM Lee KS Tsang TS Appleton CP Two-dimensional speckle-tracking echocardiography of the left atrium: feasibility and regional contraction and relaxation differences in normal subjects Journal of the American Society of Echocardiography 22 2009. 299–305. 10.1016/j.echo.2008.12.017 [DOI] [PubMed] [Google Scholar]
- 23. Teske AJ Prakken NH De Boeck BW Velthuis BK Martens EP Doevendans PA Cramer MJ Echocardiographic tissue deformation imaging of right ventricular systolic function in endurance athletes European Heart Journal 30 2009. 969–977. 10.1093/eurheartj/ehp040 [DOI] [PubMed] [Google Scholar]
- 24. Geyer H Caracciolo G Abe H Wilansky S Carerj S Gentile F Nesser HJ Khandheria B Narula J Sengupta PP Assessment of myocardial mechanics using speckle tracking echocardiography: fundamentals and clinical applications Journal of the American Society of Echocardiography 23 2010. 351–369. 10.1016/j.echo.2010.02.015 [DOI] [PubMed] [Google Scholar]
- 25. D'Andrea A Caso P Bossone E Scarafile R Riegler L Di Salvo G Gravino R Cocchia R Castaldo F Salerno G et al. Right ventricular myocardial involvement in either physiological or pathological left ventricular hypertrophy: an ultrasound speckle-tracking two-dimensional strain analysis European Journal of Echocardiography 11 2010. 492–500. 10.1093/ejechocard/jeq007 [DOI] [PubMed] [Google Scholar]
- 26. Esch BT Scott JM Warburton DE Thompson R Taylor D Cheng Baron J Paterson I Haykowsky MJ Left ventricular torsion and untwisting during exercise in heart transplant recipients Journal of Physiology 587 2009. 2375–2386. 10.1113/jphysiol.2009.170100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Doucende G Schuster I Rupp T Startun A Dauzat M Obert P Nottin S Kinetics of left ventricular strains and torsion during incremental exercise in healthy subjects: the key role of torsional mechanics for systolic–diastolic coupling Circulation. Cardiovascular Imaging 3 2010. 586–594. 10.1161/CIRCIMAGING.110.943522 [DOI] [PubMed] [Google Scholar]
- 28. Stöhr EJ González-Alonso J Pearson J Low DA Ali L Barker H Shave R Effects of graded heat stress on global left ventricular function and twist mechanics at rest and during exercise in healthy humans Experimental Physiology 96 2011. 114–124. 10.1113/expphysiol.2010.055137 [DOI] [PubMed] [Google Scholar]
- 29. Soullier C Obert P Doucende G Nottin S Cade S Perez-Martin A Messner-Pellenc P Schuster I Exercise response in hypertrophic cardiomyopathy: blunted left ventricular deformational and twisting reserve with altered systolic–diastolic coupling Circulation. Cardiovascular Imaging 5 2012. 324–332. 10.1161/CIRCIMAGING.111.968859 [DOI] [PubMed] [Google Scholar]
- 30. Pierre-Justin G Lancellotti P Pierard LA What indices quantify regional myocardial function during supine bicycle in healthy subject: natural strain and strain rate? International Journal of Cardiology 102 2005. 21–31. 10.1016/j.ijcard.2004.03.086 [DOI] [PubMed] [Google Scholar]
- 31. Goebel B Arnold R Koletzki E Ulmer HE Eichhorn J Borggrefe M Figulla HR Poerner TC Exercise tissue Doppler echocardiography with strain rate imaging in healthy young individuals: feasibility, normal values and reproducibility International Journal of Cardiovascular Imaging 23 2007. 149–155. 10.1007/s10554-006-9130-7 [DOI] [PubMed] [Google Scholar]
- 32. Goodman JM Busato GM Frey E Sasson Z Left ventricular contractile function is preserved during prolonged exercise in middle-aged men Journal of Applied Physiology 106 2009. 494–499. 10.1152/japplphysiol.90506.2008 [DOI] [PubMed] [Google Scholar]
- 33. Tan YT Wenzelburger F Lee E Heatlie G Leyva F Patel K Frenneaux M Sanderson JE The pathophysiology of heart failure with normal ejection fraction: exercise echocardiography reveals complex abnormalities of both systolic and diastolic ventricular function involving torsion, untwist, and longitudinal motion Journal of the American College of Cardiology 54 2009. 36–46. 10.1016/j.jacc.2009.03.037 [DOI] [PubMed] [Google Scholar]
- 34. Teske AJ Cox MG De Boeck BW Doevendans PA Hauer RN Cramer MJ Echocardiographic tissue deformation imaging quantifies abnormal regional right ventricular function in arrhythmogenic right ventricular dysplasia/cardiomyopathy Journal of the American Society of Echocardiography 22 2009. 920–927. 10.1016/j.echo.2009.05.014 [DOI] [PubMed] [Google Scholar]



 This work is licensed under a
This work is licensed under a