Abstract
Hypertrophic cardiomyopathy (HCM) is a relatively common inherited cardiac condition with a prevalence of approximately one in 500. It results in otherwise unexplained hypertrophy of the myocardium and predisposes the patient to a variety of disease-related complications including sudden cardiac death. Echocardiography is of vital importance in the diagnosis, assessment and follow-up of patients with known or suspected HCM. The British Society of Echocardiography (BSE) has previously published a minimum dataset for transthoracic echocardiography, providing the core parameters necessary when performing a standard echocardiographic study. However, for patients with known or suspected HCM, additional views and measurements are necessary. These additional views allow more subtle abnormalities to be detected or may provide important information in order to identify patients with an adverse prognosis. The aim of this Guideline is to outline the additional images and measurements that should be obtained when performing a study on a patient with known or suspected HCM.
Keywords: hypertrophic cardiomyopathy, transthoracic echocardiography, 2D echocardiography, guidelines
Introduction
The British Society of Echocardiography (BSE) Education Committee has previously published a minimum dataset for a standard adult transthoracic echocardiogram (1). This Guideline specifically states that the minimum dataset is usually sufficient only when the echocardiographic study is entirely normal. The aim of the BSE Education Committee is to publish a series of appendices to cover specific pathologies supporting this minimum dataset.
- The intended benefits of such supplementary recommendations are to:
- Support cardiologists and echocardiographers to develop local protocols and quality control programs for adult transthoracic study.
- Promote quality by defining a set of descriptive terms and measurements, in conjunction with a systematic approach to performing and reporting a study in specific disease states.
- Facilitate the accurate comparison of serial echocardiograms performed in patients at the same or different sites.
This Guideline gives recommendations for the image and analysis dataset required in patients either being assessed for, or with a known diagnosis of hypertrophic cardiomyopathy (HCM). The views and measurements are supplementary to those outlined in the minimum dataset and are given assuming that a full study will be performed in all patients.
When the condition or acoustic windows of the patient prevent the acquisition of one or more components of the supplementary dataset, or when measurements result in misleading information (e.g. off-axis measurements), this should be stated.
This document is a guideline for echocardiography in HCM and will be updated in accordance with changes directed by publications or changes in practice (Table 1).
Table 1.
Additional views and measurements to be obtained in patients with known or suspected hypertrophic cardiomyopathy
| View (modality) | Measurement | Explanatory note | Image |
|---|---|---|---|
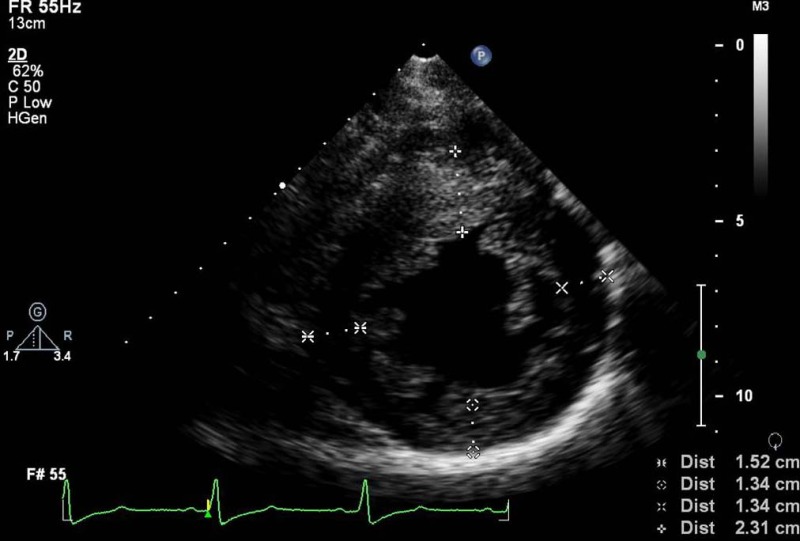
| PLAX (2D/MM) | IVSd | IVSd measure >3 cm is a key marker of increased risk (2)
Demonstrate if ASH is present Measure RV wall thickness if on axis |
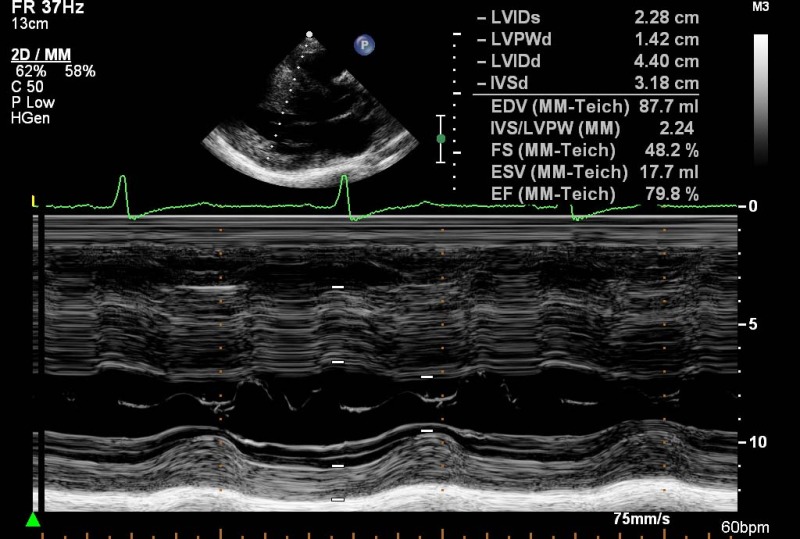
|
| PLAX (2D/MM) | LA size | Measure LA size (anterior–posterior diameter). LA diameter is one of the criteria used to estimate risk of sudden cardiac death (3) |
|
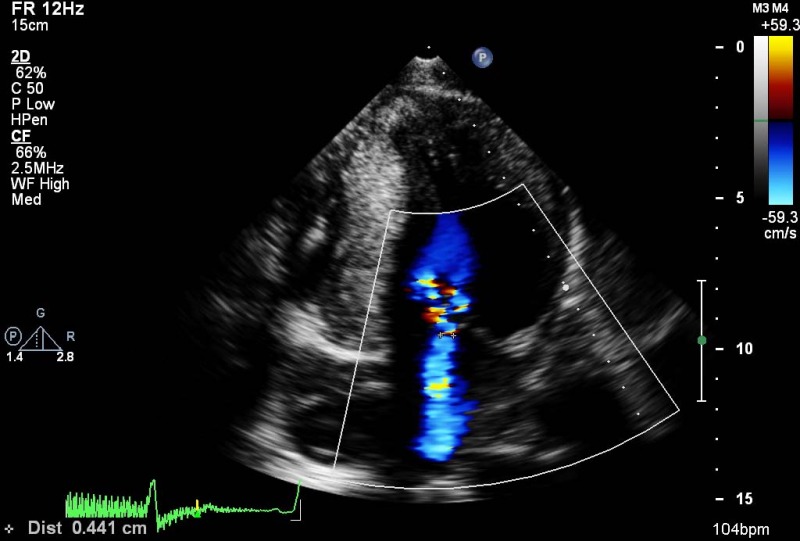
| PLAX (MM and CFM) | MV leaflet tips and AV leaflet tips | Demonstrate if SAM is present on M-Mode and for colour flow turbulence within the LVOT Demonstrate if early closure of the AV |
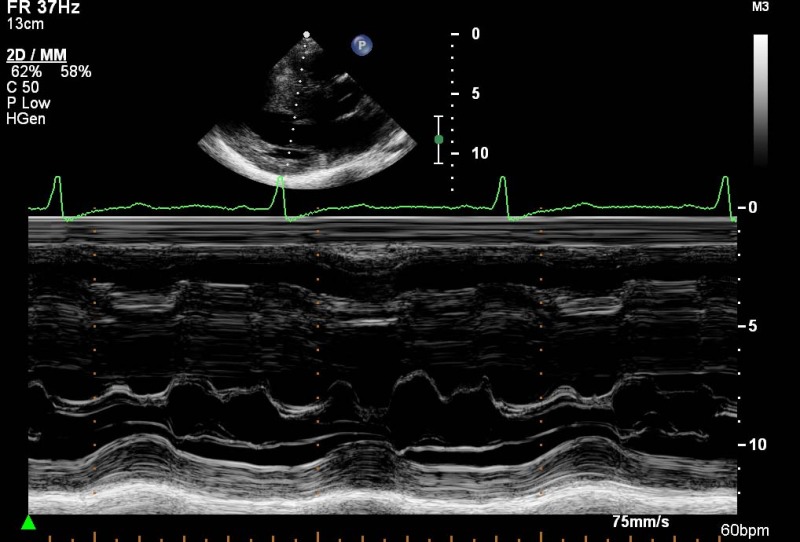
|
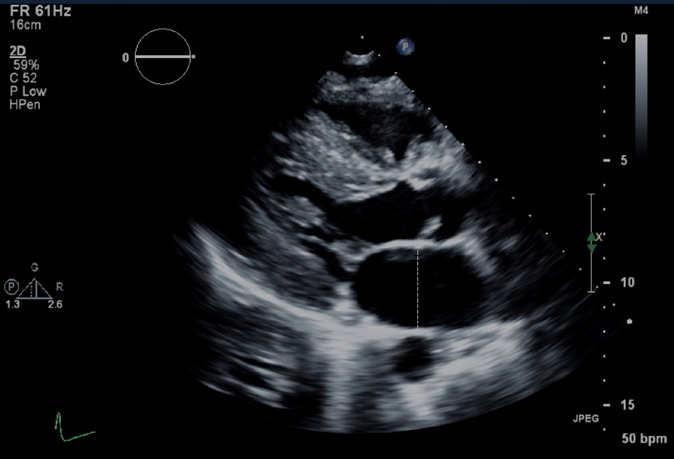
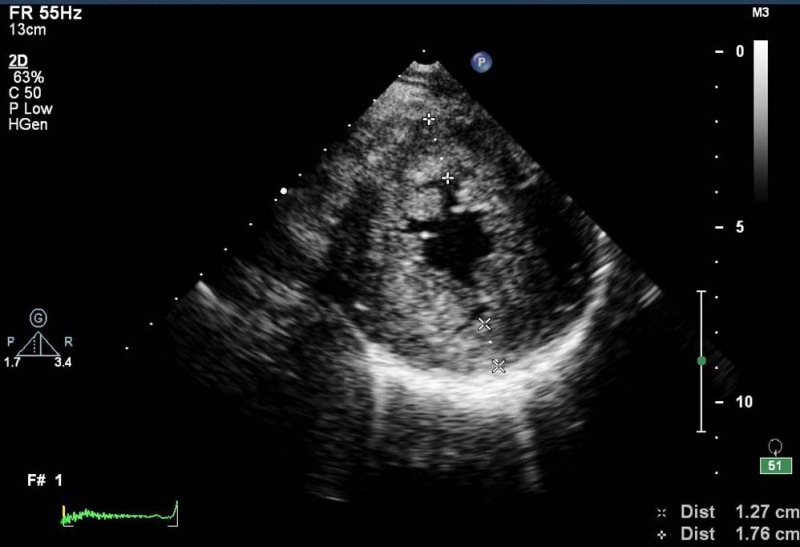
| PSAX MV (2D) | Frozen 2D image: obtain wall thickness measurements from level of the basal LV. Measure at four points, using clock face references (12, 3, 6, 9 o'clock) | To assess for asymmetric and symmetric segmental LV hypertrophy Segmental hypertrophy >1.5 cm (2) with normal or small LV internal cavity dimensions is strongly suggestive of HCM (in absence of other pathologies such as hypertension) |
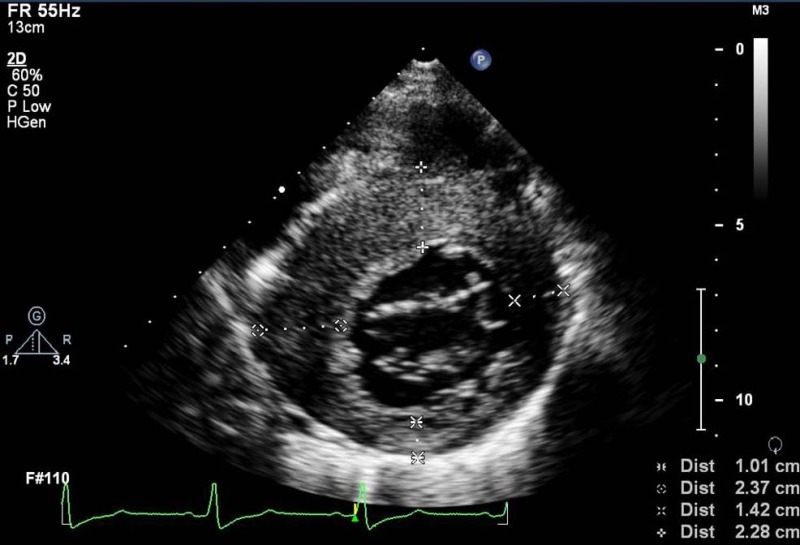
|
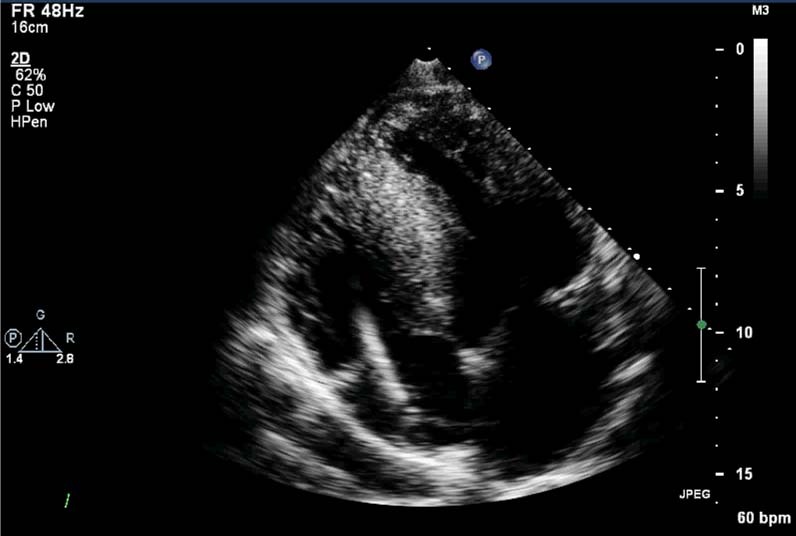
| PSAX PM (2D) | 2D frozen image at the mid-LV level. Measure at four points, using clock face references (12, 3, 6, 9 o'clock) | Avoid off-axis measurements, papillary muscle and trabeculations |
|
| PSAX Apex (2D) | Apical-level measure at two points (12 and 6 o'clock) | Apical hypertrophy may be present if apical/basal lateral ratio is >1.5. Consideration should be given to use of LV opacification contrast |
|
| Modified PSAX (2D and PW/CW) | RV wall thickness and RVOT forward flow velocities | Modify both the RV inflow and outflow to assess for RVH and RVOT obstruction. RVH present if >0.5 cm |

|
| Modified A4C (2D) | RV wall thickness | If clear images can be obtained, measure RV wall thickness. Otherwise measurement from PLAX and subcostal views is preferred. RVH present if >0.5 cm |
|
| A4C and A2C (2D) | LA volume | Index LA volume to BSA (4) |
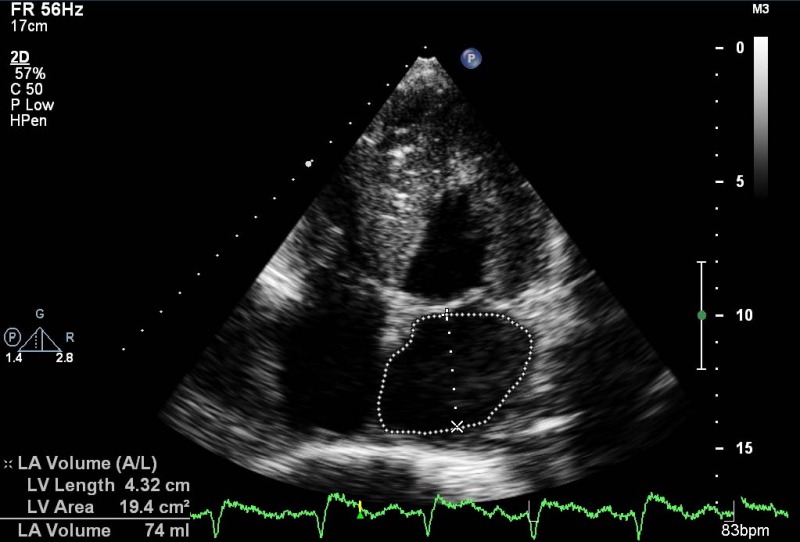
|
| A4C (CFM) | Aetiology and severity of mitral regurgitation | If SAM is present, MR may be eccentric and is usually mid/late systolic |
|
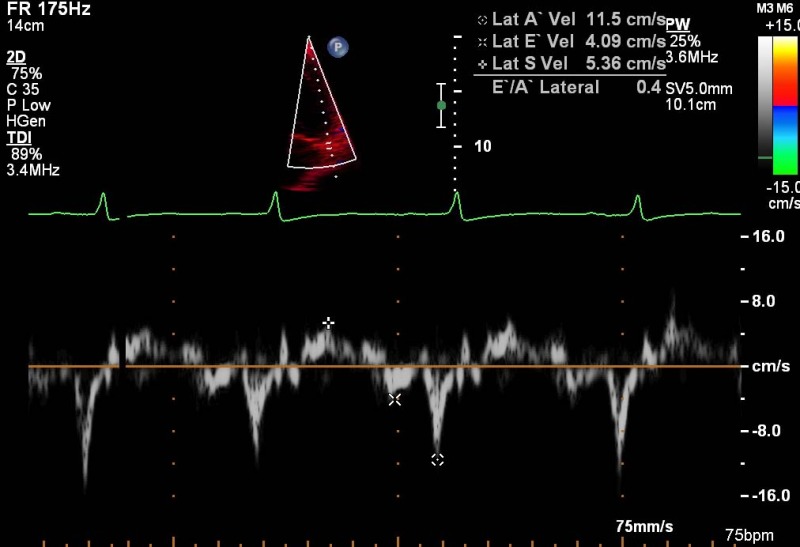
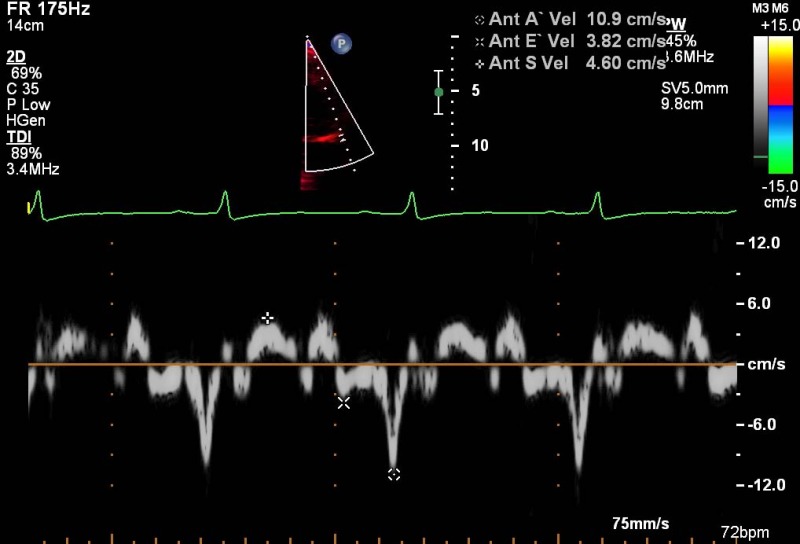
| A4C (PW TDI) | Systolic (s'), early (e') and atrial (a') relaxation velocities at anterolateral LV annulus | Reduction in s' or e' velocities below normal range for age and sex (5)
Assess for elevated LVEDp by measuring E/e'. Average septal and lateral velocities for e'. Abnormal if >10 (4) |
|
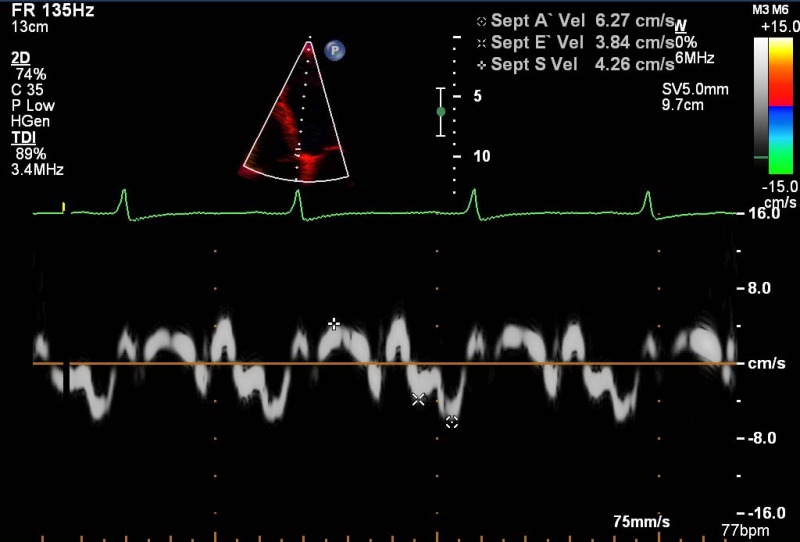
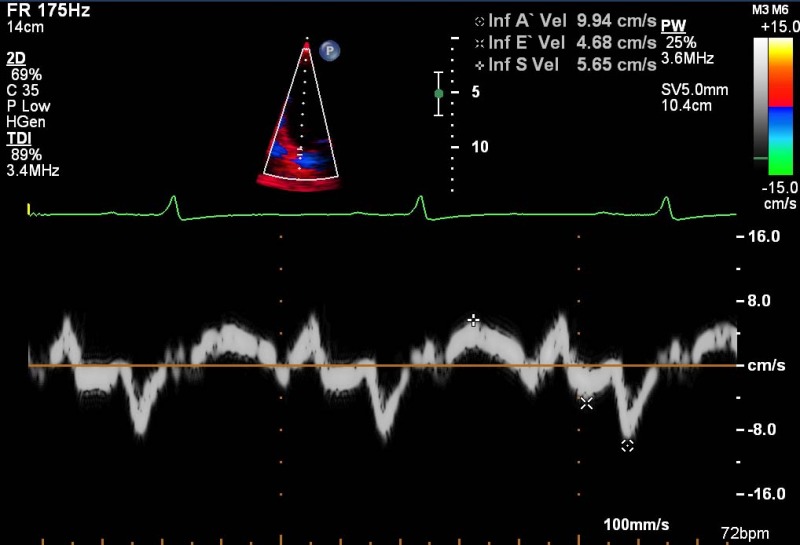
| A4C (PW TDI) | Systolic (s'), early (e') and atrial (a') relaxation velocities at inferoseptal LV annulus | Reduction in Sa or Ea velocities below normal range for age and sex (5)
Assess for elevated LVEDp by measuring E/e'. Average septal and lateral velocities for e'. Abnormal if >10 (4) |
|
| A5C and A3C (CFM) | Locate turbulent flow both within the LV cavity and the LVOT |
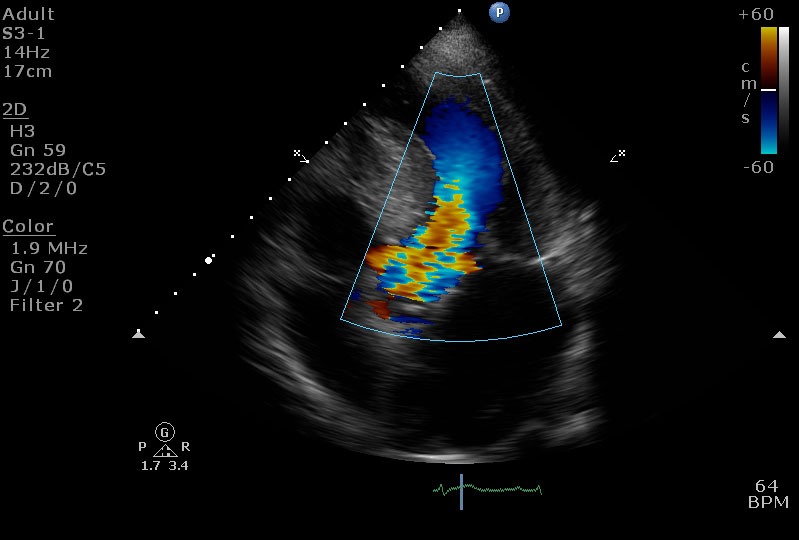
|
|
| A5C and A3C (PW/CW) | Quantify LVOT/LV intracavity dynamic flow gradient | Sample PW Doppler throughout the LV cavity, paying particular attention to areas with turbulent flow. HPRF/CW Doppler may be appropriate if aliasing occurs. Take care not to include MR jet in sample volume. A Valsalva manoeuvre should be performed in the sitting and semi-supine position (and then on standing if no gradient is produced) to assess dynamic LVOT gradients. The peak gradient (rest or Valsalva) should be recorded. In addition, exercise stress echocardiography should be considered in patients with LVOT gradients <50 mmHg at rest (with or without Valsalva) (3) |
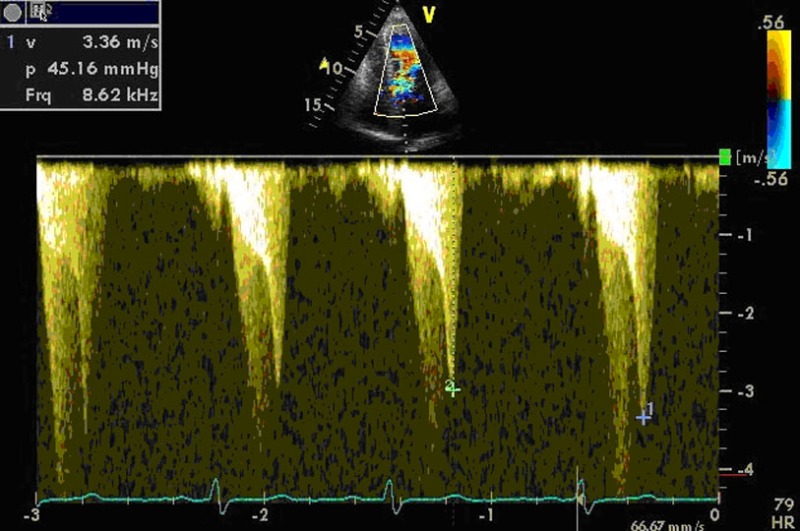
|
| A2C (PW TDI) | Systolic (s'), early (e') and atrial (a') relaxation velocities at inferior LV annulus | Reduction in s' or e' velocities below normal range for age and sex (5) |
|
| A2C (PW TDI) | Systolic (s'), early (e') and atrial (a') relaxation velocities at anterior LV annulus | Reduction in s' or e' velocities below normal range for age and sex (5) |
|
Abbreviations
| Views | |
| A2C | Apical two chamber |
| A4C | Apical four chamber |
| A5C | Apical five chamber |
| A3C | Apical three chamber or apical long axis |
| PLAX | Parasternal long axis |
| PSAX | Parasternal short axis |
| SC | Subcostal |
| SSN | Suprasternal |
| Modality | |
| CFM | Colour flow Doppler |
| CW | Continuous-wave Doppler |
| PW | Pulse wave Doppler |
| TDI | Tissue Doppler imaging |
| Measurement and explanatory text | |
| a' | Lateral and/or septal late annular relaxation velocity |
| Ao | Aorta |
| ASH | Asymmetrical septal hypertrophy |
| AV | Aortic valve |
| BSA | Body surface area |
| DT | Deceleration time |
| e' | Lateral and/or septal early annular relaxation velocity |
| HCM | Hypertrophic cardiomyopathy |
| HPRF | High pulse repetition frequency |
| IVC | Inferior vena cava |
| IVSd | Interventricular septal width in diastole |
| LA | Left atrium |
| LLPV | Left lower pulmonary vein |
| LPA | Left pulmonary artery |
| LUPV | Left upper pulmonary vein |
| LV | Left ventricle |
| LVEDp | Left ventricular end-diastolic pressure |
| LVIDd/s | Left ventricular internal dimension in diastole and systole |
| LVOT | Left ventricular outflow tract |
| LVPWd | Left ventricular posterior wall width in diastole |
| MAPSE | Mitral annular plane systolic excursion |
| MR | Mitral regurgitation |
| MV | Mitral valve |
| PA | Pulmonary artery |
| PAP | Pulmonary artery pressure |
| PHT | Pressure half-time |
| PR | Pulmonary regurgitation |
| PS | Pulmonary stenosis |
| PV | Pulmonary valve |
| RA | Right atrium |
| RLPV | Right lower pulmonary vein |
| RUPV | Right upper pulmonary vein |
| RV | Right ventricle |
| RVH | Right ventricular hypertrophy |
| RVIDd | Right ventricular cavity diameter in diastole |
| RWMA | Regional wall motion abnormality |
| RVOT | Right ventricular outflow tract |
| RVOTd | Right ventricular outflow tract dimension |
| s' | Lateral and/or septal systolic annular velocity |
| SAM | Systolic anterior motion |
| STJ | Sinotubular junction |
| SVol | Stroke volume |
| TAPSE | Tricuspid annular plane systolic excursion |
| TR | Tricuspid regurgitation |
| TV | Tricuspid valve |
| Vmax | Maximum velocity |
| VSD | Ventricular septal defect |
| VTI | Velocity time integral |
Footnotes
(N Smith is the lead author)
(R Steeds is the Guidelines Chair)
Declaration of interest
This manuscript was prepared by the British Society of Echocardiography Education Committee. The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of this guideline.
Funding
This guideline did not receive any specific grant from any funding agency in the public, commercial or not-for-profit sector.
References
- 1. Wharton G Steeds R Allen J Phillips H Jones R Kanagala P Lloyd G Masani N Mathew T Oxborough D et al. A minimum dataset for a standard adult transthoracic echocardiogram: a guideline protocol from the British Society of Echocardiography Echo Research and Practice 2 2015. G9–G24. 10.1530/ERP-14-0079 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Maron BJ McKenna WJ Danielson GK Kappenberger LJ Kuhn HJ Seidman CE Shah PM Spencer WH III Spirito P Ten Cate FJ et al. American College of Cardiology/European Society of Cardiology clinical expert consensus document on hypertrophic cardiomyopathy. A report of the American College of Cardiology Foundation Task Force on Clinical Expert Consensus Documents and the European Society of Cardiology Committee for Practice Guidelines Journal of the American College of Cardiology 42 2003. 1687–1713. 10.1016/S0735-1097(03)00941-0 [DOI] [PubMed] [Google Scholar]
- 3. Elliott PM Anastasakis A Borger MA Borggrefe M Cecchi F Charron P Hagege AA Lafont A Limongelli G Mahrholdt H et al. ESC Guidelines on diagnosis and management of hypertrophic cardiomyopathy: the Task Force for the Diagnosis and Management of Hypertrophic Cardiomyopathy of the European Society of Cardiology (ESC) European Heart Journal 35 2014. 2733–2779. 10.1093/eurheartj/ehu199 [DOI] [PubMed] [Google Scholar]
- 4.Masani N, Wharton G, Allen J, Chambers J, Graham J, Jones R, Rana B 2011 British Society of Echocardiography Guidelines for Chamber Quantification; http://www.bsecho.org/media/40506/chamber-final-2011_2_.pdf
- 5. Nagueh SF Appleton CP Gillebert TC Marino PN Oh JK Smiseth OA Waggoner AD Flachskampf FA Pellikka PA Evangelista A Recommendations for the evaluation of left ventricular diastolic function by echocardiography Journal of the American Society of Echocardiography 22 2009. 107–133. 10.1016/j.echo.2008.11.023 [DOI] [PubMed] [Google Scholar]



 This work is licensed under a
This work is licensed under a