Abstract
Background & Aims
Data on the incidence and natural history of diverticulitis are largely hospital-based and exclude the majority of diverticulitis patients, who are treated in an outpatient setting for uncomplicated diverticulitis. We assessed temporal trends in the epidemiology of diverticulitis in the general population.
Methods
Through the Rochester Epidemiology Project we reviewed the records of all individuals with a diagnosis of diverticulitis from 1980–2007 in Olmsted County, Minnesota.
Results
In 1980–1989 the incidence of diverticulitis was 115/100,000 person-years, which increased to 188/100,000 in 2000–2007 (P<.001). Incidence increased with age (P<.001); however, the temporal increase was greater in younger people (P<.001). Ten years after the index and second diverticulitis episodes, 22% and 55% had a recurrence, respectively. This recurrence rate was greater in younger people (hazard ratio [HR] per decade 0.63; 95% confidence interval [CI], 0.59–0.66) and women (HR 0.68; 95% CI, 0.58–0.80). Complications were seen in 12%; this rate did not change over time. Recurrent diverticulitis was associated with a decreased risk of complications (P<.001). Age was associated with increased risk of local (odds ratio [OR] 1.27 per decade; 95% CI, 1.04–1.57) and systemic (OR 1.83; 95% CI, 1.20–2.80) complications. Survival after diverticulitis was lower in older people (P<.001) and men (P<.001) and worsened over time (P<.001). The incidence of surgery for diverticulitis did not change from 1980–2007.
Conclusions
The incidence of diverticulitis has increased by 50% in 2000–2007 compared to 1990–1999, and more so in younger people. Complications are relatively uncommon. Recurrent diverticulitis is frequent but typically uncomplicated. Younger people with diverticulitis had less severe disease, more recurrence, and better survival.
Keywords: complication, diverticulitis, epidemiology, incidence, natural history, population-based, recurrence, surgery
BACKGROUND
Colonic diverticulosis is common, particularly in elderly persons (1, 2). While earlier studies suggested that up to 20% of people with diverticulosis develop diverticulitis (3), a more recent prospective study observed that the cumulative probability of developing diverticulitis was only 4% (4). Together with diverticular hemorrhage, diverticulitis is the most common gastrointestinal diagnosis in US hospitals (5). Between 1998 and 2005, hospital admissions and elective operations for diverticulitis increased by 26% and 29%, respectively, and by more than 70% each in patients younger than 45 years (6). These trends, also reported elsewhere (7–10), are of concern. Indeed, it has been estimated that approximately 16% of patients hospitalized for acute diverticulitis will undergo surgery for the same (11). However, as acknowledged in these studies (6) and a recent systematic review (11), they exclude most patients with uncomplicated disease, who are treated successfully with oral antibiotics in outpatient care (3). Except for one report from the United Kingdom (12), most studies on the epidemiology of diverticulitis are based on hospitalized patients. Hence, it is unclear, as posed previously (13), whether these temporal trends reflect true changes in the epidemiology of diverticulitis or simply temporal changes in practice patterns.
After resolution of acute diverticulitis, the natural history, or risk of recurrent diverticulitis and complications, guides the need for elective surgery (12). Recurrent diverticulitis occurs in 13% to 23% of people with uncomplicated and up to 40% of those with complicated diverticulitis (3). However, there are conflicting data on the risk of recurrent or complicated diverticulitis in younger vs older people (14, 15). Some, but not all, studies have reported more severe disease and a greater incidence of complications in young patients (16–19). A meta-analysis concluded that although the disease course is not different in younger patients, it tends to recur more often (15). Absent population-based data (12), several management guidelines are not strongly evidence-based, which limits the interpretation and conclusions (11). For example, the American Society of Colorectal Surgeons (ASCRS) recommends elective colectomy after recovery from an episode of complicated diverticulitis, and its stance against routine elective colonic resection after diverticulitis in younger people are supported by moderate- and low-quality evidence, respectively (3). In contrast, the American College of Gastroenterology and the World Gastroenterology Organization practice guidelines for diverticular disease suggest that elective surgery after one episode of uncomplicated diverticulitis may be “reasonably considered” in younger patients (20, 21). A better understanding of the epidemiology of diverticulitis in the population is necessary to guide its management appropriately and to plan future health care needs, particularly as the population ages. Therefore, we examined secular trends in the incidence and severity of diverticulitis among Olmsted County, Minnesota residents from January 1, 1980, to December 31, 2007, taking advantage of the population-based data resources of the Rochester Epidemiology Project (22).
METHODS
Setting
Medical care in Olmsted County is virtually self-contained within the community, thus allowing population-based epidemiologic research on the burden of diverse diseases. County residents obtain medical care almost exclusively from Mayo Clinic and Olmsted Medical Center. Both organizations are integrated health care systems with outpatient and inpatient facilities. Mayo Clinic and its affiliated hospital (Mayo Clinic Hospital — Rochester) have maintained medical records for more than 100 years that contain inpatient and outpatient data with indexed diagnoses (23). The medical records of the other providers who serve the local population are also indexed by the Rochester Epidemiology Project, providing a rich resource for documenting the epidemiology of several medical conditions (24). The population is relatively stable, particularly among older people.
Identification of Patients
Following approval by the Institutional Review Boards of Mayo Clinic and Olmsted Medical Center, the Rochester Epidemiology Project database was used to identify all Olmsted County residents who had a diagnosis of diverticulitis from January 1, 1980 through December 31, 2007. Patients who refused to authorize the use of their medical records for research were excluded from the study. As described previously for other conditions (25–27), diagnoses, local and systemic complications, and surgical procedures for diverticulitis were identified electronically using the Berkson coding system from January 1, 1980 through December 31, 1987, and the International Classification of Diseases, Ninth Revision, Clinical Modification codes from January 1, 1988 through December 31, 2007. Patients were monitored through 2007, death, or emigration from Olmsted County.
To verify the accuracy of the diagnoses obtained from the electronic database, physicians reviewed the medical records of a random sample of 100 patients with index diverticulitis (G.P.); all patients with complicated diverticulitis (O.E.); diverticulitis diagnosed on 2 or more occasions (G.P.); and all surgeries for diverticulitis (R.P. and G.P.). All 100 index patients satisfied ASCRS clinical criteria for sigmoid diverticulitis (3), i.e., acute-onset abdominal pain and left lower quadrant tenderness on examination; however, surgery disclosed acute appendicitis in 1 patient. In addition, 73 patients had at least 1 additional characteristic, including leukocytosis (n=45), evidence of diverticulitis at computed tomography (CT) (n=44), and/or fever (n=20). Among patients with recurrent diverticulitis, resolution of inflammation was documented by clinical features after the prior episode.
Computed Tomography for Diverticulitis
Increased use of abdominal CT may affect temporal trends in the incidence of acute diverticulitis (28). Hence, an experienced radiologist (J.G.F.) reviewed the abdominal CT scans of all 897 Olmsted County residents in whom the procedure was indicated for evaluation of diverticulitis at Mayo Clinic from January 1, 1997 (which is when the institutional electronic database of radiologic examinations commenced) through December 31, 2007. The CT criteria for diverticulitis were thickening of the colonic wall (≥4 mm) with signs of inflammation of pericolonic fat (i.e., hypervascularization or pericolic edema) with or without abscess formation or contained/free perforation (29), as well as the exclusion of other processes causing these imaging findings by the GI radiologist.
Statistical Analysis
The incidence of index diverticulitis was estimated by considering the entire population of Olmsted County to be at risk; the denominator (i.e., age - and sex-specific person-years) was derived from decennial census data with linear interpolation between census years (30). Because the Olmsted County population is similar to the white population of this country, the incidence rates were directly age- and sex-adjusted to the United States white population in 2000 (31). Estimates of standard errors and 95% confidence intervals (CI) assumed that the incidence episodes followed a Poisson distribution (30). Temporal trends in the incidence rates were analyzed for 3 calendar periods (1980–1989, 1990–1999, and 2000–2007). A Poisson regression model assessed the association of age, sex, and calendar period with the observed incidence rates. A linear regression model was used to assess the number of patients who had a CT scan for suspected diverticulitis, using an arc sin square root transformation of the observed proportions. The Cochran-Armitage trend test was used to assess temporal trends in the utilization of CT of the abdomen and pelvis to diagnose diverticulitis. The Kaplan-Meier method was used to estimate the cumulative risk (1 minus survival free) of any complication, risk of each type of complication, risk of recurrent diverticulitis, and overall survival. The 95% CI was estimated using the log transform method (with modified lower limit). Cox proportional hazards regression was used to assess the association of time to complication, time to recurrence, and time to surgery with age, sex, and calendar period. Development of a complication and development of a recurrence were treated as time-dependent covariates, and their associations with time to recurrence and time to complication, respectively, were assessed.
RESULTS
During the 27-year study period, 1980–2007, 3,222 people had an initial (index) diagnosis of diverticulitis; 56% were women; and the mean age was 62±16 years.
Temporal Trends in the Incidence of Diverticulitis
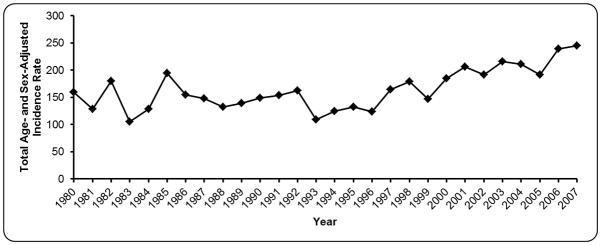
The incidence (per 100,000 person-years) was 115 in 1980–1989, increased by 7% to 123 in 1990–1999 (P<.001), and increased thereafter by 53% to 188 in 2000–2007 (P<.001). Similar trends were observed in men and women (P=.10). The age- and sex-adjusted (to the US white population in the year 2000) incidence rates also increased after the year 2000, reaching a peak of 245 patients per 100,000 in 2007 (Figure 1).
Figure 1.
Age- and Sex-Adjusted Annual Incidence of Diverticulitis in Olmsted County, Minnesota, 1980–2007.
Temporal Trends in the Relation Between Index Diverticulitis, Age, and Sex
The age-specific incidence of diverticulitis (per 100,000 person-years) increased with age (P<.001) from 10 in the second decade of life to 535 in the ninth decade (Table 1 and Figure 2). While the incidence increased with age in all 3 calendar periods, the increase over time was greatest among people younger than 50 years (P<.001 for age by calendar period interaction) as shown in Figure 2. The age-specific incidence rates increased by 85% and 132% in people aged 30–39 years and 40–49 years, respectively, from 1980–1989 to 2000–2007.
Table 1.
Age- and Sex-Specific Incidence of Diverticulitis per 100,000 Person-years Among Residents of Olmsted County, Minnesota in 3 Time Periods Between 1980–2007
| Characteristic | 1980–1989 | 1990–1999 | 2000–2007 | 1980–2007 | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age-group, yr | Female | Male | Overalla | Female | Male | Overalla | Female | Male | Overalla | Female | Male | Overalla |
| 18–29 | 5 | 12 | 8 | 7 | 5 | 6 | 13 | 23 | 18 | 8 | 13 | 10 |
| 30–39 | 22 | 41 | 31 | 28 | 41 | 34 | 39 | 77 | 58 | 29 | 53 | 41 |
| 40–49 | 66 | 68 | 67 | 81 | 102 | 91 | 131 | 182 | 156 | 97 | 124 | 110 |
| 50–59 | 195 | 174 | 185 | 184 | 173 | 178 | 262 | 281 | 271 | 216 | 212 | 214 |
| 60–69 | 281 | 294 | 287 | 344 | 285 | 316 | 491 | 341 | 419 | 374 | 307 | 343 |
| 70–79 | 437 | 401 | 423 | 431 | 331 | 390 | 560 | 502 | 534 | 476 | 413 | 450 |
| 80–89 | 641 | 411 | 574 | 454 | 435 | 448 | 617 | 544 | 592 | 564 | 470 | 535 |
| 90–99 | 467 | 1269 | 617 | 480 | 326 | 450 | 445 | 829 | 526 | 464 | 748 | 521 |
| Subtotal | 124 | 104 | 115 | 134 | 110 | 123 | 194 | 182 | 188 | 151 | 133 | 142 |
| Age-adjustedb rate (95% CI) | 148 (134–162) | 145 (128–161) | 149 (137–162) | 137 (124–150) | 208 (194–223) | 210 (194–227) | 170 (162–177) | 166 (157–175) | ||||
| Age- and sex-adjustedc rate (95% CI) | 147 (136–157) | 144 (135–153) | 209 (198–220) | 168 (162–174) | ||||||||
Sex-adjusted to Olmsted County population in corresponding decade.
Age-adjusted to United States white population in 2000.
Age- and sex-adjusted to United States white population in 2000.
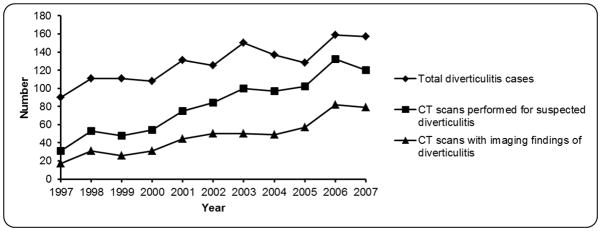
Figure 2.
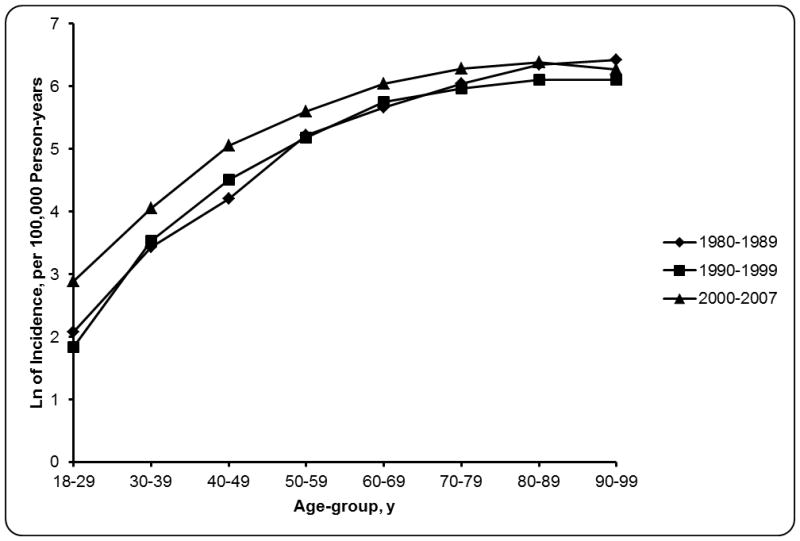
Relation Between Age and Incidence of Diverticulitis in Olmsted County, Minnesota, 1980–1989 and 2000–2007. The separation between the curves was greater for the 2000–2007 period and the earlier epochs in younger people, which reflects a more prominent increase in incidence over time. Ln indicates the natural logarithm of incidence rate of diverticulitis per 100,000 person-years.
Temporal Trends in the CT Diagnosis of Diverticulitis
Among the 3,222 patients, the number of abdominal CT scans to assess for diverticulitis increased by 287%, from 31 in 1997 (P<.001) to 120 in 2007 (Figure 3). Of these scans, the number of abdominal CT scans that revealed features of diverticulitis was 17 and 79 in 1997 and 2007, respectively. The proportion of scans that demonstrated diverticulitis did not change significantly (P=.22) between 1997, i.e., 17/31 (55%) and 2007, i.e., 79/120 (66%). However, because more patients had a CT scan for suspected diverticulitis, the proportion of patients who had CT findings of diverticulitis increased (P<.001) from 19% in 1997 to 50% in 2007.
Figure 3.
Temporal Trends in Radiologic Diagnosis of Diverticulitis, 1997–2007. The proportion of patients in whom computed tomography (CT)-documented diverticulitis increased significantly over time.
Recurrent Diverticulitis
Over the 27-year study period, 635 patients had 1 episode of recurrent diverticulitis, 280 patients had 2 episodes, and 127 patients had 3. After the index diagnosis of diverticulitis, the cumulative incidence of the first recurrent diverticulitis was 8% at 1 year, 17% at 5 years, and 22% at 10 years (Figure 4). After the second episode of diverticulitis, the cumulative incidence of yet another episode was 19% at 1 year, 44% at 5 years, and 55% at 10 years. After the third episode, the cumulative incidence was 24% at 1 year and 40% at 3 years. The risk of the first recurrent episode was univariately associated with age (P<.001) and time period (P<.001) but not with sex. In the multivariable model, age, sex, and time period were independent predictors of the time to first recurrence. The risk of the first recurrent episode was greater in younger people and women and greater between the 1990–1999 and 2000–2007 periods (vs 1980–1989) (Table 2).
Figure 4.
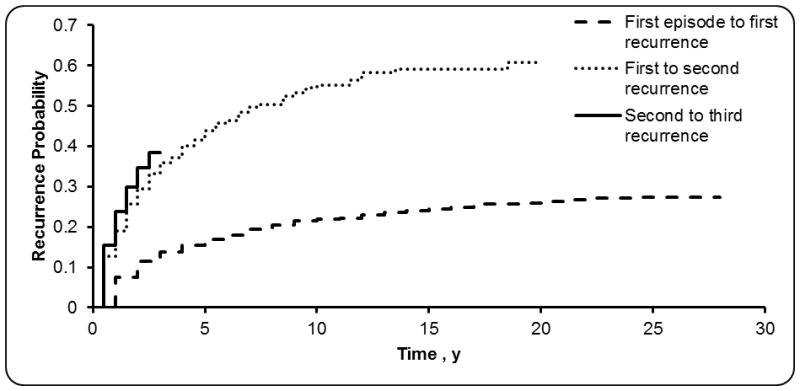
Kaplan-Meier Estimates of Cumulative Risk of Recurrent Diverticulitis.
Table 2.
Multivariable Analysis of the Risk of Recurrent and Complicated Diverticulitis Among Olmsted County, Minnesota, Residents, 1980–2007
| Variable | First Episode of Recurrent Diverticulitis, HR (95% CI) | Diverticulitis Complication Type, Compared With Abscess Alone, OR (95% CI) | |
|---|---|---|---|
| Obstruction, Fistula, Stricture, or Peritonitis | Bacteremia or Septicemia | ||
| Age (per 10 yr) | 0.63 (0.59–0.66) | 1.27 (1.04–1.57) | 1.83 (1.20–2.80) |
| Male sex | 0.69 (0.58, 0.80) | 1.69 (1.07–2.66) | 1.18 (0.48–2.93) |
| 1990–1999a | 2.17 (1.74, 2.69) | 0.92 (0.53–1.60) | 0.52 (0.18–1.47) |
| 2000–2007a | 5.12 (4.11, 6.37) | 0.70 (0.41–1.20) | 0.49 (0.18–1.38) |
Abbreviations: HR, hazard ratio; OR, odds ratio.
Reference calendar period is 1980–1989.
Among 641 patients who received a CT scan for the diagnosis of their index episode between 1997 and 2007, 433 patients (68%) had CT features of diverticulitis. The risk of recurrence was higher in patients with compared to without (P<.001) CT features of diverticulitis (hazard ratio [HR] 1.74; 95% CI, 1.12–2.71); see Supplementary Figure 1a. The cumulative incidence of the first recurrent episode five years after the index episode was 86% in patients with CT-confirmed diverticulitis, compared to 56% of diverticulitis patients diagnosed without CT confirmation.
Complications of Diverticulitis
Of the 3,222 patients, 386 (12%) had 1 or more complications of diverticulitis. The incidence of complications (14% in 1980–1989, 12.7% in 1990–1999, and 10.3% in 2000–2007) did not change significantly over time (P=.44). Complications included pericolonic abscess (267 patients, 69%), peritonitis (103 patients, 27%), obstruction (59 patients, 15%), and fistula (53 patients, 14%). Septicemia (23 patients, 6%), bacteremia (10 patients, 3%), and stricture (9 patients, 2%) were uncommon. Among patients with complications, 275 (71%) had only 1 complication, 84 (22%) had 2, and 27 (7%) had 3 or more. Among 111 patients with more than one complication, 66 patients had multiple simultaneous complications (i.e., within 30 days of each other) while 55 had complications that were temporally separated from each other. The total of 66 and 55 (i.e., 121) is greater than 110 because 10 patients had both simultaneous and separate complications.
Patients with complicated diverticulitis had a mean age of 62.4±16 years, and 54% were women. Sixty-three percent were age 60 years or older, 31% 40 to 59 years and 7% were younger than 40 years. Survival free of the initial complication was not univariately associated with age, sex, or calendar period. However, among patients with complications, age (P<.001), but not sex or calendar period, was univariately associated with the type of complication. In the multivariable analysis, compared with the reference group (i.e., patients with an abscess alone), age was associated with an increased risk of local (odds ratio [OR] 1.27 per decade; 95% CI, 1.04–1.57) and systemic (OR 1.83; 95% CI, 1.20–2.80) complications (Table 2). In addition, men had an increased risk of local complications (OR 1.69; 95% CI, 1.07–2.66) relative to women with an abscess. The association between calendar period and type of complication was not significant (P=.17). The risk of a future complication related to diverticulitis was not different in patients with compared to without CT features of diverticulitis at the index episode (P=.15) (Supplementary Figure 1b).
Surgery for Diverticulitis
Surgery for diverticulitis was performed in 454 patients, of whom 250 had complicated diverticulitis; 125 of them had emergency surgery, all for complicated diverticulitis. Because surgery for diverticulitis may have been performed several years after the index diagnosis, temporal trends in surgery for diverticulitis were evaluated by analyzing the number of patients that had surgery for diverticulitis expressed as a proportion of all index cases that year. This proportion did not change significantly over time (Supplementary Figure 2). In the multivariable analysis, the time to the first operation for diverticulitis was not related to age (P=.13), sex (P=.56) and year (P=.53).
Relation Between Recurrent Diverticulitis and Complications
Of 386 patients with a complication, 286 had no preceding episodes of diverticulitis (Supplementary Figure 3). Complications were more often related to the index episode than to recurrent diverticulitis (McNemar test, P<.001).
Compared with uncomplicated index diverticulitis, the risk of recurrent diverticulitis was not different in patients who were treated without surgery for a complication of diverticulitis that occurred either during or subsequent to the index episode but before recurrent diverticulitis (HR 0.90; 95% CI, 0.62–1.30) but was significantly lower in complicated cases who underwent surgery (HR 0.20; 95% CI, 0.09–0.46) as shown in Figure 5A. Excluding patients who had a complication related to the index episode, the time to first complication was longer, and the risk of a complication was lower (HR 0.53; 95% CI, 0.37–0.76), in patients who had recurrent diverticulitis (Figure 5B). Among 37 patients who had a recurrence after a complication, none of them had a subsequent complication.
Figure 5.
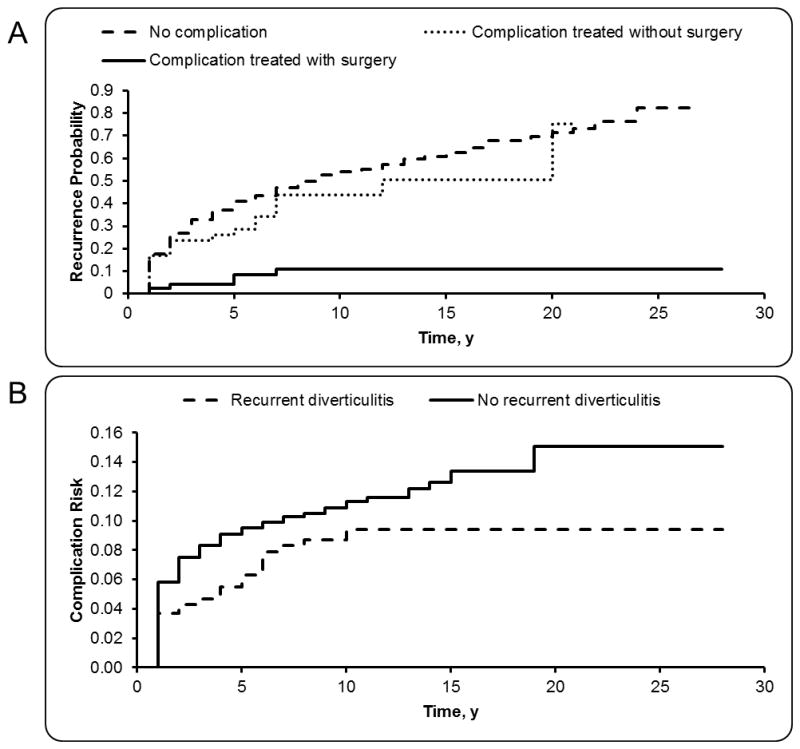
Risks of Recurrence and Complication in Diverticulitis. A) Risk of recurrent diverticulitis after complicated diverticulitis. B) Risk of complicated diverticulitis after recurrent diverticulitis.
Survival after Diverticulitis
Of 3,222 patients, 1,720 had zero follow-up. Survival after diverticulitis was not significantly different from the expected survival for a similar (i.e., Minnesota white) population (P=.78). However, among people with diverticulitis, the risk of death was greater in older people (HR per decade 2.12; 95% CI, 2.00–2.25), greater in men than women (HR 1.57; 95% CI, 1.37–1.80), and greater in the more recent calendar periods. Thus, compared with the 1980–1989 period, the HRs adjusted for age and sex were 1.34 (95% CI, 1.15–1.56) in 1990–1999 and 1.87 (95% CI, 1.50–2.33) in 2000–2007. To obviate the confounding effect of differences in the duration of follow up amongst epochs, 5-year survival was also estimated. The differences in observed survival after the diagnosis of diverticulitis across calendar periods were relatively small, and the estimated 5-year survival rates were 0.71, 0.69, and 0.65 for patients diagnosed in 1980–1989, 1990–1999, and 2000–2007, respectively.
Compared to patients without complicated diverticulitis, patients with complicated diverticulitis had a greater risk of death (HR 1.36; 95% CI, 1.14–1.62) as shown in Supplementary Figure 4. The estimated 5-year survival rates were 0.65 and 0.68 in patients with and without complications, respectively.
DISCUSSION
Systematic searches of the MEDLINE and PubMed databases using the key words “diverticulitis” and “population or community” and the key words “diverticulitis” and “United States” suggest that this is the first comprehensive population-based study on diverticulitis in this country. Such data provide a more accurate perspective on temporal trends in the incidence and natural history (complications, recurrence rate, and surgery) of acute diverticulitis in the population (outpatients and inpatients combined) than do hospital series, which are distorted by referral of the most severely-affected patients.
The incidence of diverticulitis was stable between the 1980–1989 and 1990–1997 periods but increased by 53% during the 2000–2007 period, which exceeds the 26% increase in hospitalization for diverticulitis seen in the United States between 1998 and 2005 (6). In contrast to earlier studies, the utilization of surgery for diverticulitis did not change over time (6). The proportion of patients with CT findings of diverticulitis increased from 19% in 2000 to 50% in 2007, suggesting that increased use of CT may partly, but not entirely, explain the increased incidence of diverticulitis. Similarly, the National Hospital Ambulatory Medical Care Survey observed that the use of CT to investigate unexplained abdominal pain in the emergency department increased after the year 2001 (32). Consistent with consensus guidelines and clinical practice, diverticulitis was diagnosed by clinical criteria alone. While CT is very sensitive and specific for diagnosing diverticulitis, it has been suggested that CT may not be as diagnostic in early or mild diverticulitis. Also, temporal trends in the utilization of CT would confound the estimated incidence of CT-confirmed diverticulitis. Of interest, the proportion, among a subset of 100 patients, who had leukocytosis (45%) and fever (20%) was similar to the corresponding proportions among patients with clinical features and CT findings of uncomplicated diverticulitis (33). Nonetheless the estimated incidence of disease in this study is probably an upper limit estimate that is likely higher than the incidence of CT-confirmed diverticulitis.
While the incidence of diverticulitis was, as observed previously, greatest among elderly persons (6, 34), the temporal increase was more pronounced in younger people, by 125%, 85%, and 132% in people aged 18–29, 30–39, and 40–49 years, respectively. Whether these findings are related to underlying differences in the pathogenesis of diverticulosis in younger people is unknown. The prevalence of low dietary fiber intake and obesity, both putative risk factors for diverticulitis (35, 36) has increased in young adults and children over the last decade (37–39). This may perhaps contribute to the increased incidence of diverticulitis in the younger age groups over time. However, younger persons with diverticulitis had a lower risk of local and systemic complications. Therefore, our observations suggest that the previously-observed, disproportionately-greater temporal increase in hospitalization for diverticulitis in younger people (13) is more likely explained by an increased incidence of diverticulitis than by more severe disease.
The incidence of recurrent diverticulitis was 17% at 5 years after the index episode, which is comparable to the estimated risk of 13% to 23% previously reported in the literature (3). This risk was greater in younger people, in women, and in patients with CT-confirmed diverticulitis. After the second and third episodes, the risk of recurrent diverticulitis was higher: 44% at 5 years and 40% at 3 years, respectively. However, the precise clinical features in index and recurrent cases were not compared.
Only 12% of patients had a complication of diverticulitis, which is less than the estimated prevalence of 20% in a systematic review and likely because our study was based on a community population rather than more selected populations as in other studies (19). Of complications, 60% were related to the index episodes. Similar to a study from the United Kingdom (12), recurrent diverticulitis was not associated with an increased risk of complications. The proportion of patients with complications treated with emergency (125 of 386 patients [32%]) and elective (125 of 386 patients [32%]) surgery was similar to a previous meta-analysis (40). Compared with uncomplicated index diverticulitis, the risk of recurrence was lower in complicated patients treated operatively, but did not differ significantly compared to complicated patients treated nonoperatively. These findings support retrospective studies that suggest that expectant nonoperative management is safe in complicated diverticulitis (41–43), and they raise questions about the recommendation to “typically” consider elective colectomy after an episode of complicated diverticulitis (3). Although data were not sufficient to evaluate outcomes by complication type in the present study, surgery is generally necessary for symptomatic relief in patients with fistula or stricture (3).
Survival was not significantly different among the diverticulitis patients compared with the white population of Minnesota generally. Among patients with diverticulitis, survival was shorter in men, older people, and persons who received the diagnosis in 2000–2007 than in the previous time periods. Survival was lower among patients with compared to without complications of diverticulitis (12). The causes of death and the prevalence of other comorbid conditions were not studied.
Using the Rochester Epidemiology Project, we could identify diverticulitis in all patients in Olmsted County regardless of whether they were treated as outpatients or inpatients. Although we verified the accuracy of electronic coding for identifying diverticulitis, its complications, and surgery, the clinical diagnosis of diverticulitis may have been inaccurate in some patients (28). The relationship between obesity and the course of diverticulitis was not assessed (35, 44). The incidence of irritable bowel syndrome after diverticulitis was not assessed.(45, 46) Moreover, outmigration rates for this population are low, but it is conceivable that some patients with diverticulitis had a complication at a medical center outside Olmsted County that was not reflected in community medical records. Such errors should not vary over time.
In conclusion, the incidence of diverticulitis has increased in 2000–2007 compared to 1990–1999, particularly among younger people. Of patients with diverticulitis, only 12% had complications. Recurrent diverticulitis was common and more so in younger people. However, younger people also had less severe diverticulitis and longer survival thereafter. The risk of complications was lower in recurrent diverticulitis. Among patients with complicated diverticulitis treated conservatively, the risk of recurrence was not greater than in uncomplicated diverticulitis. Taken together, these observations counter the recommendation that elective surgery is a “reasonable option” after a single episode of diverticulitis in young patients (20, 21). Rather, they provide additional evidence, which currently is “low,” to support the recommendation that “routine elective resection based on young age (<50 years) is no longer recommended” for acute diverticulitis (3).
Supplementary Material
Risks of Recurrence and Complications With versus Without CT Confirmation of Diverticulitis. A) Risk of recurrent diverticulitis after CT-confirmed diverticulitis. B) Risk of complicated diverticulitis after CT-confirmed diverticulitis.
Temporal trends in surgery for diverticulitis. Operations for diverticulitis, expressed as a proportion of all index cases that year, did not change over time.
Timing of Occurrence of Complications of Diverticulitis. Most complications occurred with the first (index) episode of diverticulitis.
Lower Survival after Complicated than Uncomplicated Diverticulitis
What is current knowledge?
Our understanding of the incidence and natural history of diverticulitis is almost entirely based on hospitalized patients – hence ignores the vast majority of patients with uncomplicated diverticulitis who are treated as outpatients
The rates of hospital admissions and elective surgeries for diverticulitis have been increasing, particularly among younger people.
The risk of recurrent diverticulitis is higher after complicated than uncomplicated diverticulitis.
There are conflicting data on the risk of recurrent or complicated diverticulitis in younger, compared to older people
What is new here?
This is the first comprehensive, population-based study of diverticulitis in the United States
The incidence of diverticulitis has increased by 50% since 2000 and more so in younger people.
Recurrent diverticulitis did not increase the risk of subsequent complications and complications did not increase the risk of recurrent diverticulitis
Younger people with diverticulitis had less severe disease, greater recurrence, and better survival.
How might it impact on clinical practice in the foreseeable future?
These findings question the recommendation to “typically” consider elective colectomy after an episode of complicated diverticulitis
Provide evidences to support the recommendation against routine elective resection in younger patients
Supports the need to individualize elective surgery after recurrent diverticulitis
Acknowledgments
Grant Support: This study was made possible using the resources of the Rochester Epidemiology Project, which is supported by the National Institute on Aging of the National Institutes of Health under Award Number R01AG034676. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.” Dr. Bharucha was supported in part by grant R01 DK78924 from the National Institutes of Health, US Department of Health and Human Services.
Abbreviations
- ASCRS
American Society of Colon and Rectal Surgeons
- CI
confidence intervals
- CT
computed tomography
- HR
hazard ratio
- OR
odds ratio
- SD
standard deviation
Footnotes
Author contributions: Study concept and design: Bharucha, Melton, and Zinsmeister.
Acquisition of data: Bharucha, Parthasarathy, Fletcher, Ditah, Ewelukwa, Pendlimari.
Analysis and Interpretation of data: Bharucha, Parthasarathy, Zinsmeister.
Drafting of the manuscript: Bharucha, Parthasarathy.
Critical revision of the manuscript for important intellectual content: All authors
Statistical expertise: Zinsmeister.
Obtained funding and study supervision: Bharucha.
Disclosures: None of the authors have any conflicts of interest that are relevant to the manuscript
References
- 1.Shaheen NJ, Hansen RA, Morgan DR, et al. The burden of gastrointestinal and liver diseases, 2006. Am J Gastroenterol. 2006;101:2128–38. doi: 10.1111/j.1572-0241.2006.00723.x. [DOI] [PubMed] [Google Scholar]
- 2.Everhart JE, Ruhl CE. Burden of digestive diseases in the United States part II: lower gastrointestinal diseases. Gastroenterology. 2009;136:741–54. doi: 10.1053/j.gastro.2009.01.015. [DOI] [PubMed] [Google Scholar]
- 3.Feingold D, Steele SR, Lee S, et al. Practice parameters for the treatment of sigmoid diverticulitis. Dis Colon Rectum. 2014;57:284–94. doi: 10.1097/DCR.0000000000000075. [DOI] [PubMed] [Google Scholar]
- 4.Shahedi K, Fuller G, Bolus R, et al. Long-term risk of acute diverticulitis among patients with incidental diverticulosis found during colonoscopy. Clin Gastroenterol Hepatol. 2013;11:1609–13. doi: 10.1016/j.cgh.2013.06.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Peery AF, Dellon ES, Lund J, et al. Burden of gastrointestinal disease in the United States: 2012 update. Gastroenterology. 2012;143:1179–87. e1–3. doi: 10.1053/j.gastro.2012.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Etzioni DA, Mack TM, Beart RW, Jr, et al. Diverticulitis in the United States: 1998–2005: changing patterns of disease and treatment. Ann Surg. 2009;249:210–7. doi: 10.1097/SLA.0b013e3181952888. [DOI] [PubMed] [Google Scholar]
- 7.Makela J, Kiviniemi H, Laitinen S. Prevalence of perforated sigmoid diverticulitis is increasing. Dis Colon Rectum. 2002;45:955–61. doi: 10.1007/s10350-004-6335-5. [DOI] [PubMed] [Google Scholar]
- 8.Kang JY, Hoare J, Tinto A, et al. Diverticular disease of the colon--on the rise: a study of hospital admissions in England between 1989/1990 and 1999/2000. Aliment Pharmacol Ther. 2003;17:1189–95. doi: 10.1046/j.1365-2036.2003.01551.x. [DOI] [PubMed] [Google Scholar]
- 9.Warner E, Crighton EJ, Moineddin R, et al. Fourteen-year study of hospital admissions for diverticular disease in Ontario. Can J Gastroenterol. 2007;21:97–9. doi: 10.1155/2007/943460. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jamal Talabani A, Lydersen S, Endreseth BH, et al. Major increase in admission- and incidence rates of acute colonic diverticulitis. Int J Colorectal Dis. 2014;29:937–45. doi: 10.1007/s00384-014-1888-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Morris AM, Regenbogen SE, Hardiman KM, et al. Sigmoid diverticulitis: a systematic review. JAMA. 2014;311:287–97. doi: 10.1001/jama.2013.282025. [DOI] [PubMed] [Google Scholar]
- 12.Humes DJ, West J. Role of acute diverticulitis in the development of complicated colonic diverticular disease and 1-year mortality after diagnosis in the UK: population-based cohort study. Gut. 2012;61:95–100. doi: 10.1136/gut.2011.238808. [DOI] [PubMed] [Google Scholar]
- 13.Etzioni DA, Cannom RR, Ault GT, et al. Diverticulitis in California from 1995 to 2006: increased rates of treatment for younger patients. Am Surg. 2009;75:981–5. [PubMed] [Google Scholar]
- 14.Konvolinka CW. Acute diverticulitis under age forty. Am J Surg. 1994;167:562–5. doi: 10.1016/0002-9610(94)90098-1. [DOI] [PubMed] [Google Scholar]
- 15.Katz LH, Guy DD, Lahat A, et al. Diverticulitis in the young is not more aggressive than in the elderly, but it tends to recur more often: systematic review and meta-analysis. J Gastroenterol Hepatol. 2013;28:1274–81. doi: 10.1111/jgh.12274. [DOI] [PubMed] [Google Scholar]
- 16.Ambrosetti P, Robert JH, Witzig JA, et al. Acute left colonic diverticulitis in young patients. J Am Coll Surg. 1994;179:156–60. [PubMed] [Google Scholar]
- 17.Minardi AJ, Jr, Johnson LW, Sehon JK, et al. Diverticulitis in the young patient. Am Surg. 2001;67:458–61. [PubMed] [Google Scholar]
- 18.Schweitzer J, Casillas RA, Collins JC. Acute diverticulitis in the young adult is not “virulent. Am Surg. 2002;68:1044–7. [PubMed] [Google Scholar]
- 19.Kaiser AM, Jiang JK, Lake JP, et al. The management of complicated diverticulitis and the role of computed tomography. Am J Gastroenterol. 2005;100:910–7. doi: 10.1111/j.1572-0241.2005.41154.x. [DOI] [PubMed] [Google Scholar]
- 20.Stollman NH, Raskin JB. Diagnosis and management of diverticular disease of the colon in adults. Ad Hoc Practice Parameters Committee of the American College of Gastroenterology. Am J Gastroenterol. 1999;94:3110–21. doi: 10.1111/j.1572-0241.1999.01501.x. [DOI] [PubMed] [Google Scholar]
- 21.Murphy T, Hunt RH, Fried M, et al. World Gastroenterology Organisation Practice Guidelines: Diverticular Disease. 2007 Available from: http://www.worldgastroenterology.org/assets/downloads/en/pdf/guidelines/07_diverticular_disease.pdf.
- 22.Melton LJ., 3rd History of the Rochester Epidemiology Project. Mayo Clin Proc. 1996;71:266–74. doi: 10.4065/71.3.266. [DOI] [PubMed] [Google Scholar]
- 23.Rocca WA, Yawn BP, St Sauver JL, et al. History of the Rochester Epidemiology Project: half a century of medical records linkage in a US population. Mayo Clin Proc. 2012;87:1202–13. doi: 10.1016/j.mayocp.2012.08.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.St Sauver JL, Grossardt BR, Yawn BP, et al. Data resource profile: the Rochester Epidemiology Project (REP) medical records-linkage system. Int J Epidemiol. 2012;41:1614–24. doi: 10.1093/ije/dys195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McNamara DR, Tleyjeh IM, Berbari EF, et al. Incidence of lower-extremity cellulitis: a population-based study in Olmsted county, Minnesota. Mayo Clin Proc. 2007;82:817–21. doi: 10.4065/82.7.817. [DOI] [PubMed] [Google Scholar]
- 26.Ptaszynski AE, Hooten WM, Huntoon MA. The incidence of spontaneous epidural abscess in Olmsted County from 1990 through 2000: a rare cause of spinal pain. Pain Med. 2007;8:338–43. doi: 10.1111/j.1526-4637.2006.00173.x. [DOI] [PubMed] [Google Scholar]
- 27.Uslan DZ, Crane SJ, Steckelberg JM, et al. Age- and sex-associated trends in bloodstream infection: a population-based study in Olmsted County, Minnesota. Arch Intern Med. 2007;167:834–9. doi: 10.1001/archinte.167.8.834. [DOI] [PubMed] [Google Scholar]
- 28.Andeweg CS, Knobben L, Hendriks JC, et al. How to diagnose acute left-sided colonic diverticulitis: proposal for a clinical scoring system. Ann Surg. 2011;253:940–6. doi: 10.1097/SLA.0b013e3182113614. [DOI] [PubMed] [Google Scholar]
- 29.Ambrosetti P, Jenny A, Becker C, et al. Acute left colonic diverticulitis--compared performance of computed tomography and water-soluble contrast enema: prospective evaluation of 420 patients. Dis Colon Rectum. 2000;43:1363–7. doi: 10.1007/BF02236631. [DOI] [PubMed] [Google Scholar]
- 30.Bergstralh EJ, Offord KP, Chu CP, et al. Calculating Incidence, Prevalence, And Mortality Rates For Olmsted County, Minnesota: An Update. Rochester: Mayo Clinic; 1992. [Google Scholar]
- 31.Blandon RE, Bharucha AE, Melton LJ, 3rd, et al. Incidence of pelvic floor repair after hysterectomy: A population-based cohort study. Am J Obstet Gynecol. 2007;197:664, e1–7. doi: 10.1016/j.ajog.2007.08.064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pines JM. Trends in the rates of radiography use and important diagnoses in emergency department patients with abdominal pain. Med Care. 2009;47:782–6. doi: 10.1097/MLR.0b013e31819748e9. [DOI] [PubMed] [Google Scholar]
- 33.Longstreth GF, Iyer RL, Chu LH, et al. Acute diverticulitis: demographic, clinical and laboratory features associated with computed tomography findings in 741 patients. Aliment Pharmacol Ther. 2012;36:886–94. doi: 10.1111/apt.12047. [DOI] [PubMed] [Google Scholar]
- 34.Masoomi H, Buchberg BS, Magno C, et al. Trends in diverticulitis management in the United States from 2002 to 2007. Arch Surg. 2011;146:400–6. doi: 10.1001/archsurg.2010.276. [DOI] [PubMed] [Google Scholar]
- 35.Strate LL, Liu YL, Aldoori WH, et al. Obesity increases the risks of diverticulitis and diverticular bleeding. Gastroenterology. 2009;136:115–122. e1. doi: 10.1053/j.gastro.2008.09.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Crowe FL, Balkwill A, Cairns BJ, et al. Source of dietary fibre and diverticular disease incidence: a prospective study of UK women. Gut. 2014;63:1450–6. doi: 10.1136/gutjnl-2013-304644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Saldanha LG. Fiber in the diet of US children: results of national surveys. Pediatrics. 1995;96:994–7. [PubMed] [Google Scholar]
- 38.Singh GK, Kogan MD, van Dyck PC. A multilevel analysis of state and regional disparities in childhood and adolescent obesity in the United States. J Community Health. 2008;33:90–102. doi: 10.1007/s10900-007-9071-7. [DOI] [PubMed] [Google Scholar]
- 39.King DE, Mainous AG, 3rd, Carnemolla M, et al. Adherence to healthy lifestyle habits in US adults, 1988–2006. Am J Med. 2009;122:528–34. doi: 10.1016/j.amjmed.2008.11.013. [DOI] [PubMed] [Google Scholar]
- 40.Lamb MN, Kaiser AM. Elective resection versus observation after nonoperative management of complicated diverticulitis with abscess: a systematic review and meta-analysis. Dis Colon Rectum. 2014;57:1430–40. doi: 10.1097/DCR.0000000000000230. [DOI] [PubMed] [Google Scholar]
- 41.Broderick-Villa G, Burchette RJ, Collins JC, et al. Hospitalization for acute diverticulitis does not mandate routine elective colectomy. Arch Surg. 2005;140:576–81. doi: 10.1001/archsurg.140.6.576. discussion 581–3. [DOI] [PubMed] [Google Scholar]
- 42.Nelson RS, Ewing BM, Wengert TJ, et al. Clinical outcomes of complicated diverticulitis managed nonoperatively. Am J Surg. 2008;196:969–72. doi: 10.1016/j.amjsurg.2008.07.035. discussion 973–4. [DOI] [PubMed] [Google Scholar]
- 43.Gaertner WB, Willis DJ, Madoff RD, et al. Percutaneous drainage of colonic diverticular abscess: is colon resection necessary? Dis Colon Rectum. 2013;56:622–6. doi: 10.1097/DCR.0b013e31828545e3. [DOI] [PubMed] [Google Scholar]
- 44.Bose KP, Khorshidi I, Southern WN, et al. The impact of ethnicity and obesity on the course of colonic diverticulitis. J Clin Gastroenterol. 2013;47:160–4. doi: 10.1097/MCG.0b013e318259e71c. [DOI] [PubMed] [Google Scholar]
- 45.Jung HK, Choung RS, Locke GR, 3rd, et al. Diarrhea-predominant irritable bowel syndrome is associated with diverticular disease: a population-based study. Am J Gastroenterol. 2010;105:652–61. doi: 10.1038/ajg.2009.621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Cohen E, Fuller G, Bolus R, et al. Increased risk for irritable bowel syndrome after acute diverticulitis. Clin Gastroenterol Hepatol. 2013;11:1614–9. doi: 10.1016/j.cgh.2013.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Risks of Recurrence and Complications With versus Without CT Confirmation of Diverticulitis. A) Risk of recurrent diverticulitis after CT-confirmed diverticulitis. B) Risk of complicated diverticulitis after CT-confirmed diverticulitis.
Temporal trends in surgery for diverticulitis. Operations for diverticulitis, expressed as a proportion of all index cases that year, did not change over time.
Timing of Occurrence of Complications of Diverticulitis. Most complications occurred with the first (index) episode of diverticulitis.
Lower Survival after Complicated than Uncomplicated Diverticulitis