Abstract
Objective
To describe and compare characteristics and outcomes of patients who arrive by ambulance to the ED. We aimed to (i) compare patients with a delayed ambulance offload time (AOT) >30 min with those who were not delayed; and (ii) identify predictors of an ED length of stay (LOS) of >4 h for ambulance-arriving patients.
Methods
A retrospective, multi-site cohort study was undertaken in Australia using 12 months of linked health data (September 2007–2008). Outcomes of AOT delayed and non-delayed presentations were compared. Logistic regression analysis was undertaken to identify predictors of an ED LOS of >4 h.
Results
Of the 40 783 linked, analysable ambulance presentations, AOT delay of >30 min was experienced by 15%, and 63% had an ED LOS of >4 h. Patients with an AOT <30 min had better outcomes for: time to triage; ambulance time at hospital; time to see healthcare professional; proportion seen within recommended triage time frame; and ED LOS for both admitted and non-admitted patients. In-hospital mortality did not differ. Strong predictors of an ED LOS >4 h included: hospital admission, older age, triage category, and offload delay >30 min.
Conclusion
Patients arriving to the ED via ambulance and offloaded within 30 min experience better outcomes than those delayed. Given that offload delay is a modifiable predictor of an ED LOS of >4 h, targeted improvements in the ED arrival process for ambulance patients might be useful.
Keywords: ambulance, data linkage, emergency department, offload delay, outcome
Key findings.
Around 30% of ED presentations arrive via ambulance.
Offloading ambulance arriving patients within 30 minutes translates to better outcomes.
Linked health data provides an ability to more comprehensively understand the patient journey to inform patient and service delivery improvements.
Introduction
ED crowding and congestion are increasingly common issues facing acute healthcare systems internationally and have been associated with negative patient and staff outcomes.1 Associated with crowding, ambulance offload time (AOT) delay (i.e. extended time from ambulance arrival to ED to offload onto hospital stretcher, also called ambulance ramping) has emerged as an issue affecting care quality, patient safety and ability to respond to the surrounding community.2,3 Around 23% of the 7.1 million ED presentations made to Australian public hospitals in 2007–2008 were via ambulance.4 Research examining either patient or system outcomes associated with AOT delay is limited.
Key areas for hospital system improvements have been noted at the international, national and local level. Desired improvements focus on care quality in terms of safety, timeliness, patient-centredness, efficiency, effectiveness and equity.5–7 ‘Access’ is one component reflecting equity and effectiveness.8 Accessing emergency services and subsequent inpatient care (if required) in a timely fashion is important to safety and quality of care delivery. Following the implementation of 4 h targets set in the UK,7 similar ED ‘access’ targets were set for Australia by the Federal Government.9 An understanding of this target and other outcomes can inform the efficient use of ambulance and ED resources, as well as measuring and monitoring performance.
The aims of the present study were to examine whether, for patients who arrived to ED via ambulance: (i) differences in outcomes occurred for those who were AOT delayed by >30 min versus those not delayed; and (ii) which factors predicted ED length of stay (LOS) of >4 h.
Methods
Design and setting
A retrospective, cohort study was undertaken in three major public teaching hospitals located in Queensland, Australia, serving a population of approximately 800 000.10 All three EDs treated both adult and paediatric patients, and had a combined ED bed number of 122 and hospital bed number of 963. Hospitals A and C shared operational capability. The Queensland Ambulance Service (QAS) had 17 permanent stations and one rotary wing retrieval service located in the catchment area.
Patients
All patient presentations made to the three EDs over a 12 month period (3 September 2007–2 September 2008) were included. Deterministic data linkage between disparate data sources from ambulance, ED and hospital admission was undertaken. Figure 1 displays the sample inclusion process. A power calculation showed that the sample size was more than adequate to detect a difference in the outcome (ED LOS >4 h) and the chance of a type II error was negligible. Based on an alpha level of 0.05, model (Nagelkerke) R2 of 0.30 and 20 predictors for the outcome (ED LOS >4 h), our sample size provided a power of 99%.
Figure 1.
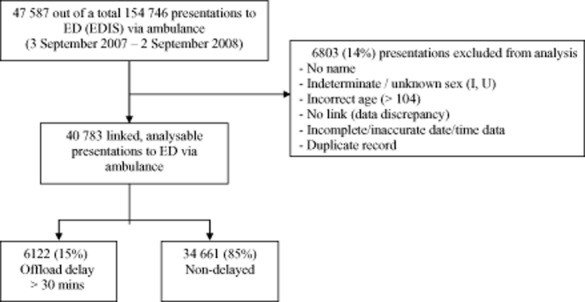
Sample inclusion flow diagram (data from three hospitals; 12 months).
Data collection
Table 1 presents the data used for the present study. Data were sourced from the Ambulance Service database, Emergency Department Information System (EDIS), and Hospital Based Corporate Information System (HBCIS).
Table 1.
Data collected from each health information source
| Data source | Data obtained |
|---|---|
| Ambulance data | |
| Unit Record Number (URN) | |
| Name | |
| Age | |
| Sex | |
| Post code pickup | |
| Suburb pickup | |
| Triage code allocated by Communications Centre | |
| Suburb location of base station | |
| Date and time of dispatch | |
| Date and time of arrival on scene | |
| Date and time of on-scene departure | |
| ED transported to | |
| Date and time of arrival to ED | |
| Date and time of ED triage | |
| Date and time off-stretcher | |
| Date and time case completed | |
| ED data | |
| Unit Record Number (URN) | |
| Name | |
| Age | |
| Sex | |
| Mode of arrival | |
| Australasian Triage Scale (ATS) category | |
| Presenting complaint category | |
| Date and time of arrival | |
| Date and time of triage | |
| Date and time seen by doctor | |
| Date and time of ED discharge | |
| Discharge disposition from ED | |
| International Classification of Diseases (ICD) 10 Code | |
| Hospital admission data | |
| Unit Record Number (URN) | |
| Name | |
| Date of birth | |
| Sex | |
| Post code | |
| Date and time of hospital admission | |
| Date and time of hospital discharge | |
| Discharge destination |
To link data from the three separate health information system databases, we used a deterministic linking approach developed in collaboration with the Commonwealth Scientific and Industrial Research Organisation (CSIRO). The accuracy of the linking strategy has been previously reported with sensitivity of between 95% and 99%, and specificity of between 75% and 99%.11 Appropriate Human Research Ethics approvals were obtained.
Statistical analysis
To describe patient characteristics, we used descriptive statistics, including median and interquartile range. Frequency and percentages were used for categorical variables. To identify differences between delayed and non-delayed groups, we used the Mann–Whitney U non-parametric test for continuous data and χ2 tests for categorical variables.
To identify independent predictors of ED LOS >4 h, univariate analysis was followed by multivariate logistic regression models (using the enter method). Predictors entered into the regression model included age, sex, triage category, time of presentation (in 8 h aliquots), day of week (as weekday/weekend), season, ambulance offload delay >30 min (Yes/No), ED International Classification of Diseases (ICD) 10 code, hospital admission (Yes/No) and hospital (A/B/C). We considered a two-sided P value of <0.05 to be statistically significant. Reference groups were based on previous research, cell size or the most logical comparison. SPSS version 18.0 (SPSS, Chicago, IL, USA) was used to analyse data.
Results
Characteristics of ambulance offload time delayed versus non-ambulance offload time delayed patient presentations
A total of 40 783 analysable patient presentations were made to the three EDs, via ambulance, during the 12 month study period. Of those 15% (n = 6122) were delayed by >30 min from arrival to ED offload. For each site, delayed and non-delayed ambulance presentations differed significantly for almost all demographic and ED characteristics (Table 2). Older people represented a higher proportion of the AOT delayed group, and the results for men and women were relatively balanced. The majority of presentations were in Australasian Triage Scale (ATS) category 3. AOT delays were most evident within this triage category. Although those presenting with ‘injury, poisoning and other consequences of external causes’ comprised the highest proportion of the ED illness groups, there was no specific illness group seen where AOT delays and non-delays differed. Most arrivals occurred during the evening shift (between 15.00 and 22.59 h), with AOT delays notably worse during this time period. Friday appeared to be the worst day for delays, and Saturday, the best. Winter months (not surprisingly) were worse for AOT delays (Table 2).
Table 2.
Comparisons of characteristics for AOT delayed and non-delayed patient presentations to three EDs
| Characteristic | Hospital A (n = 16 609) | Hospital B (n = 17 155) | Hospital C (n = 7019) | P value (non-delayed vs delayed) | |||||
|---|---|---|---|---|---|---|---|---|---|
| Non-delayed n = 15 189 (91.4%) | Delayed n = 1420 (8.6%) | Non-delayed n = 12 711 (74.1%) | Delayed n = 4444 (25.9%) | Non-delayed n = 6761 (96.5%) | Delayed n = 258 (3.7%) | Hospital | |||
| A | B | C | |||||||
| Median age (IQR) | 47 (25–71) | 56 (32–76) | 42 (22–64) | 52 (32–72) | 53 (31–75) | 60 (37–79) | <0.001 | <0.001 | 0.004 |
| Age group (years) | <0.001 | <0.001 | 0.005 | ||||||
| 0–15 | 1473 (9.7%) | 91 (6.4%) | 1811 (14.1%) | 264 (5.9%) | 503 (7.4%) | 13 (5.0%) | |||
| 16–64 | 8910 (58.7%) | 743 (52.3%) | 7769 (61.1%) | 2615 (58.8%) | 3742 (55.3%) | 124 (48.1%) | |||
| 65+ | 4806 (31.6%) | 586 (41.3%) | 3131 (24.6%) | 1565 (35.2%) | 2516 (37.2%) | 121 (46.9%) | |||
| Sex: male | 7882 (51.9%) | 701 (49.4%) | 6166 (48.5%) | 2058 (46.3%) | 3274 (48.4%) | 113 (43.8%) | 0.068 | 0.012 | 0.114 |
| Triage category | <0.001 | <0.001 | 0.053 | ||||||
| 1 | 464 (3.1%) | 10 (0.7%) | 272 (2.1%) | 13 (0.3%) | 59 (0.9%) | 1 (0.4%) | |||
| 2 | 3759 (24.7%) | 280 (19.7%) | 1744 (13.7%) | 445 (10.0%) | 1465 (21.7%) | 55 (21.3%) | |||
| 3 | 811 (53.4%) | 929 (65.4%) | 6835 (53.8%) | 3215 (72.3%) | 3777 (55.9%) | 164 (63.6%) | |||
| 4 | 2731 (18.0%) | 190 (13.4%) | 3643 (28.7%) | 740 (16.7%) | 1418 (21.0%) | 36 (14.0%) | |||
| 5 | 125 (0.8%) | 11 (0.8%) | 217 (1.7%) | 31 (0.7%) | 42 (0.6%) | 2 (0.8%) | |||
| ED ICD 10† | <0.001 | <0.001 | 0.983 | ||||||
| Injury, poisoning and certain other consequences of external causes (S00–T98) | 4058 (27.4%) | 365 (26.0%) | 2925 (24.2%) | 980 (23.2%) | 1622 (24.0%) | 58 (22.5%) | |||
| Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified (R00–R99) | 2478 (16.7%) | 273 (19.4%) | 2051 (17.0%) | 831 (19.7%) | 1317 (19.5%) | 54 (20.9%) | |||
| Diseases of the circulatory system (I00–I99) | 1461 (9.9%) | 112 (8.0%) | 1281 (10.6%) | 494 (11.7%) | 649 (9.6%) | 24 (9.3%) | |||
| Factors influencing health status and contact with health services (Z00–Z99) | 1459 (9.8%) | 110 (7.8%) | 1255 (10.4%) | 276 (6.5%) | 380 (5.6%) | 16 (6.2%) | |||
| Diseases of the respiratory system (J00–J99) | 1145 (7.7%) | 92 (6.5%) | 1090 (9.0%) | 347 (8.2%) | 574 (8.5%) | 22 (8.5%) | |||
| Mental and behavioural disorders (F00–F99) | 788 (5.3%) | 88 (6.3%) | 595 (4.9%) | 175 (4.1%) | 439 (6.5%) | 19 (7.4%) | |||
| All other | 3443 (23.2%) | 365 (26.0%) | 2875 (23.8%) | 1119 (26.5%) | 1776 (26.3%) | 65 (25.2%) | |||
| Shift of presentation | <0.001 | <0.001 | <0.001 | ||||||
| Morning (07.00–14.59 h) | 5750 (37.9%) | 587 (41.3%) | 4915 (38.7%) | 1914 (43.1%) | 2818 (41.7%) | 98 (38.0%) | |||
| Evening (15.00–22.59 h) | 5692 (37.5%) | 712 (50.1%) | 4689 (36.9%) | 2048 (46.1%) | 2649 (39.2%) | 137 (53.1%) | |||
| Night (23.00–06.59 h) | 3747 (24.7%) | 121 (8.5%) | 3107 (24.4%) | 482 (10.8%) | 1294 (19.1%) | 23 (8.9%) | |||
| Day of week | <0.001 | <0.001 | <0.001 | ||||||
| Monday | 2114 (13.9%) | 218 (15.4%) | 1707 (13.4%) | 784 (17.6%) | 1032 (15.3%) | 69 (26.7%) | |||
| Tuesday | 1964 (12.9%) | 227 (16.0%) | 1857 (14.6%) | 581 (13.1%) | 960 (14.2%) | 31 (12.0%) | |||
| Wednesday | 2008 (13.2%) | 183 (12.9%) | 1745 (13.7%) | 586 (13.2%) | 941 (13.9%) | 35 (13.6%) | |||
| Thursday | 2128 (14.0%) | 195 (13.7%) | 1727 (13.6%) | 730 (16.4%) | 959 (14.2%) | 29 (11.2%) | |||
| Friday | 2194 (14.4%) | 228 (16.0%) | 1772 (13.9%) | 745 (16.8%) | 954 (14.1%) | 41 (15.9%) | |||
| Saturday | 2351 (15.5%) | 190 (13.4%) | 2001 (15.7%) | 494 (11.1%) | 938 (13.9%) | 23 (8.9%) | |||
| Sunday | 2430 (16.0%) | 179 (12.6%) | 1908 (15.0%) | 524 (11.8%) | 977 (14.5%) | 30 (11.6%) | |||
| Weekday/Weekend | <0.001 | <0.001 | 0.006 | ||||||
| Weekday | 10 408 (68.5%) | 1051 (74.0%) | 8802 (69.2%) | 3426 (77.1%) | 4846 (71.7%) | 205 (79.5%) | |||
| Weekend | 4781 (31.5%) | 369 (26.0%) | 3909 (30.8%) | 1018 (22.9%) | 1915 (28.3%) | 53 (20.5%) | |||
| Season | <0.001 | <0.001 | <0.001 | ||||||
| Summer | 3757 (24.7%) | 376 (26.5%) | 3613 (28.6%) | 1040 (23.4%) | 1570 (23.2%) | 40 (15.5%) | |||
| Autumn | 3696 (24.3%) | 356 (25.1%) | 2955 (23.2%) | 1072 (24.1%) | 1769 (26.2%) | 72 (27.9%) | |||
| Winter | 3800 (25.0%) | 415 (29.2%) | 2693 (21.2%) | 1269 (28.6%) | 2031 (30.0%) | 122 (47.3%) | |||
| Spring | 3936 (25.9%) | 273 (19.2%) | 3432 (27.0%) | 1063 (23.9%) | 1391 (20.6%) | 24 (9.3%) | |||
Delayed refers to >30 min. †Based on 16 237 (Hospital A); 16 294 (Hospital B); 7015 (Hospital C) cases where diagnosis data were entered. AOT, ambulance offload time; ICD 10, international statistical classification of disease and related health problems (10th revision); IQR, interquartile range.
Outcomes of ambulance offload time delayed versus non-ambulance offload time delayed patient presentations
Outcomes for AOT delayed versus non-delayed patients are presented in Table 3. Most outcomes differed statistically between delayed and non-delayed patient presentations across each site. Overall, patients offloaded within 30 min had better outcomes, including time to triage, ambulance time at ED (turnaround time), time to see a healthcare professional, being seen within ATS time frame, ED LOS for admitted and non-admitted patients, processed in the ED within 4 h, and admission requirement. No statistically significant differences for in-hospital mortality were identified between delayed and non-delayed presentations at any of the three sites.
Table 3.
Comparison of outcomes for AOT delayed and non-delayed patient presentations to three EDs
| Outcome | Hospital A | Hospital B | Hospital C | P value (non-delayed vs delayed) | |||||
|---|---|---|---|---|---|---|---|---|---|
| Non-delayed n = 15 189 (91.4%) | Delayed n = 1420 (8.6%) | Non-delayed n = 12 711 (74.1%) | Delayed n = 4444 (25.9%) | Non-delayed n = 6761 (96.5%) | Delayed n = 258 (3.7%) | Hospital | |||
| A | B | C | |||||||
| Median (IQR) time to triage (min)† | 4 (2–8) | 11 (5–21) | 2 (1–4) | 3 (2–6) | 4 (2–7) | 11 (5–22) | <0.001 | <0.001 | <0.001 |
| Median (IQR) offload time (min)† | 10 (6–15) | 41 (35–52) | 11 (7–18) | 58 (41–88) | 10 (7–15) | 39 (35–48) | <0.001 | <0.001 | <0.001 |
| Median (IQR) time at ED (min)† | 23 (14–33) | 48 (39–62) | 34 (23–48) | 73 (55–104) | 20 (12–29) | 47 (39–58) | <0.001 | <0.001 | <0.001 |
| Median (IQR) time to see healthcare professional (min)† | 37 (12–102) | 65 (27–132) | 48 (18–106) | 71 (32–130) | 26 (12–61) | 45 (21–85) | <0.001 | <0.001 | <0.01 |
| Median (IQR) ED length of stay (total) (min)† | 333 (200–543) | 373 (243–628) | 265 (158–444) | 357 (223–606) | 308 (190–515) | 386 (227–696) | <0.001 | <0.001 | <0.001 |
| Median (IQR) ED length of stay (admitted) (min)† | 456 (303–687) | 515 (357–811) | 423 (274–643) | 523 (350–803) | 446 (306–700) | 497 (347–959) | <0.001 | <0.001 | 0.003 |
| Median (IQR) ED length of stay (not admitted) (min)† | 236 (148–373) | 273 (186–391) | 213 (130–336) | 283 (184–440) | 215 (143–334) | 270 (161–403) | <0.001 | <0.001 | 0.002 |
| Seen within ATS, n (%) | 5754 (39.9%) | 315 (22.7%) | 4758 (39.4%) | 1034 (23.9%) | 3474 (51.4%) | 86 (33.3%) | <0.001 | <0.001 | <0.001 |
| Admitted/Transferred/Discharged <4 h, n (%) | 5081 (33.5%) | 349 (24.6%) | 5696 (44.8%) | 1267 (28.5%) | 2479 (36.7%) | 68 (26.4%) | <0.001 | <0.001 | 0.001 |
| Admitted, n (%)† | 7417 (48.8%) | 724 (51.0%) | 4121 (32.4%) | 1651 (37.2%) | 3196 (47.3%) | 136 (52.7%) | 0.120 | <0.001 | 0.086 |
| Access blocked, n (%)‡ | 3449 (46.5%) | 398 (55.0%) | 1724 (41.8%) | 936 (56.7%) | 1437 (45.0%) | 71 (52.2%) | <0.001 | <0.001 | 0.096 |
| Median (IQR) hospital length of stay (days)‡ | 2 (1–6) | 3 (1–7) | 2 (1–6) | 3 (1–6) | 2 (1–4) | 1.5 (1–4) | 0.05 | <0.001 | 0.59 |
| In-hospital mortality, all admissions, n (%)‡ | 266 (3.6%) | 21 (2.9%) | 144 (3.5%) | 56 (3.4%) | 76 (2.4%) | 6 (4.4%) | 0.340 | 0.848 | 0.134 |
Admitted: based on ED patient presentations (n = 16 609; 17 155; 7019).
Access blocked and in-hosp mortality: based on all presentations requiring hospital admission (n = 8141; 5772; 3332); Hospital LOS: based on ED presentations requiring hospital admission (n = 8141; 5772; 3332). Delayed refers to >30 min. Numbers included in analysis: For Hospitals A, B and C, respectively, QAS Time at ED: based on patient presentations (n = 16 597; 17 128; 7018); time to see Dr: based on patient presentations (n = 15 819; 16 409; 7012); ED LOS (total): based on patient presentations (n = 16 609; 17154; 7019); ED LOS (not admitted): based on patient presentations (n = 8468; 11 382; 3687); ED LOS (admitted): based on ED patient presentations (n = 8141; 5772; 3332); seen within ATS: based on ED patient presentations (n = 15 821; 16 413; 7012). AOT, ambulance offload time; ATS, Australasian Triage Scale; ICD 10, International Statistical Classification of Disease and Related Health Problems (10th revision); IQR, interquartile range; LOS, length of stay.
Predictors of emergency department length of stay >4 h for presentations via ambulance
Logistic regression analysis was undertaken to identify independent predictors of an ED LOS of >4 h. The proportion of patient presentations arriving by ambulance that had an ED LOS of >4 h within each potential predictor entered into the univariate regression model is presented in Table 4. Table 4 also displays the crude odds ratio (OR), 95% confidence interval (CI) and P value of each predictor. All univariate predictors were entered into the multivariate logistic regression model that identified 13 independent predictors of higher odds of an ED LOS >4 h. These were: admission requirement (OR 5.49), age (16–64 years, OR 2.39; 65+ years, OR 4.20), triage category (category 2, OR 1.60; category 3, OR 2.33; category 4, OR 1.91), AOT delay >30 min (OR 1.65), season (winter, OR 1.31; autumn, OR 1.27), larger hospital (Hospital A, OR 1.45; Hospital B, OR 1.08), weekday presentation (OR 1.06) and female gender (OR 1.05).
Table 4.
Predictors of ED LOS >4 h for patient presentations via ambulance
| Predictor | Total patient presentations (n) | ED LOS >4 h (%) | Crude odds ratio (95% CI) | P value | Adjusted odds ratio (95% CI) | P value |
|---|---|---|---|---|---|---|
| Age group (years) | ||||||
| 0–15 | 4155 | 37.1 | 1.0† | 1.0† | ||
| 16–64 | 23 903 | 59.1 | 2.45 (2.29–2.62) | <0.001 | 2.39 (2.21–2.58) | <0.001 |
| 65+ | 12 725 | 80.0 | 6.78 (6.28–7.32) | <0.001 | 4.20 (3.85–4.59) | <0.001 |
| Gender | ||||||
| Female | 20 589 | 64.3 | 1.08 (1.04–1.13) | <0.001 | 1.05 (1.00–1.10) | 0.039 |
| Male | 20 194 | 62.4 | 1.0† | 1.0† | ||
| Triage category | ||||||
| 1 | 819 | 55.8 | 2.63 (2.06–3.35) | <0.001 | 0.64 (0.48–0.86) | 0.003 |
| 2 | 7748 | 69.9 | 4.84 (3.93–5.95) | <0.001 | 1.60 (1.25–2.05) | <0.001 |
| 3 | 23 030 | 66.7 | 4.16 (3.39–5.11) | <0.001 | 2.33 (1.84–2.97) | <0.001 |
| 4 | 8758 | 51.1 | 2.17 (1.76–2.67) | <0.001 | 1.91 (1.50–2.43) | <0.001 |
| 5 | 428 | 32.5 | 1.0† | 1.0† | ||
| ED ICD 10 Code‡ | ||||||
| Injury, poisoning and certain other consequences of external causes (S00–T98) | 10 008 | 53.1 | 0.54 (0.52–0.57) | <0.001 | 0.58 (0.54–0.62) | <0.001 |
| Symptoms, signs and abnormal clinical and laboratory findings, not elsewhere classified (R00–R99) | 7004 | 71.9 | 1.56 (1.47–1.65) | <0.001 | 1.05 (0.97–1.13) | 0.23 |
| Diseases of the circulatory system (I00–I99) | 4021 | 75.4 | 1.84 (1.70–1.98) | <0.001 | 0.58 (0.53–0.65) | <0.001 |
| Factors influencing health status and contact with health services (Z00–Z99) | 3496 | 31.4 | 0.23 (0.21–0.24) | <0.001 | 0.26 (0.24–0.29) | <0.001 |
| Diseases of the respiratory system (J00–J99) | 3270 | 71.5 | 1.46 (1.35–1.58) | <0.001 | 0.85 (0.77–0.94) | <0.001 |
| Mental and behavioural disorders (F00–F99) | 2104 | 68.3 | 1.23 (1.12–1.35) | <0.001 | 0.95 (0.85–1.06) | 0.35 |
| All other | 9643 | 72.7 | 1.70 (1.62–1.79) | <0.001 | 1.0† | NS |
| Shift of presentation | ||||||
| Early (07.00–14.59 h) | 16 082 | 65.9 | 1.05 (0.99–1.11) | 0.075 | 0.76 (0.71–0.81) | <0.001 |
| Evening (15.00–22.59 h) | 15 927 | 60.0 | 0.82 (0.77–0.86) | <0.001 | 0.66 (0.62–0.71) | <0.001 |
| Night (23.00–06.59 h) | 8774 | 64.8 | 1.0† | |||
| Weekday/Weekend | ||||||
| Weekday | 28 738 | 64.4 | 1.15 (1.10–1.21) | <0.001 | 1.06 (1.01–1.12) | 0.022 |
| Weekend | 12 045 | 61.0 | 1.0† | 1.0† | ||
| Season‡ | ||||||
| Summer | 10 414 | 60.3 | 0.84 (0.80–0.88) | <0.001 | 0.96 (0.90–1.03) | 0.241 |
| Autumn | 9920 | 65.5 | 1.13 (1.08–1.19) | <0.001 | 1.27 (1.19–1.36) | <0.001 |
| Winter | 10 330 | 67.3 | 1.26 (1.20–1.32) | <0.001 | 1.31 (1.22–1.40) | <0.001 |
| Spring | 10 119 | 60.4 | 0.85 (0.81–0.89) | <0.001 | 1.0† | NS |
| Offload delay | ||||||
| ≤30 min | 34 661 | 61.8 | 1.0† | 1.0† | ||
| >30 min | 6122 | 72.5 | 1.63 (1.54–1.73) | <0.001 | 1.65 (1.54–1.78) | <0.001 |
| Admission requirement | ||||||
| Not admitted | 23 538 | 47.5 | 1.0† | 1.0† | ||
| Admitted | 17 245 | 85.0 | 6.28 (5.98–6.59) | <0.001 | 5.49 (5.18–5.81) | <0.001 |
| Hospital‡ | ||||||
| A | 16 609 | 67.3 | 1.34 (1.28–1.39) | <0.001 | 1.45 (1.35–1.55) | <0.001 |
| B | 17 155 | 59.4 | 0.75 (0.72–0.78) | <0.001 | 1.08 (1.01–1.16) | 0.027 |
| C | 7019 | 63.7 | 1.02 (0.97–1.07) | 0.51 | 1.0† | NS |
Reference group. ‡Reference group was all other groups within the predictor variable (e.g. reference group for summer was all other seasons). Multiple regression model parameters using Enter method: (n = 39 546, 20 predictors); Cox and Snell R2: 0.22; Nagelkerke R2: 0.30; Hosmer and Lemeshow Test: x2 = 30.32, d.f. = 8, P < 0.001. ICD 10, International Statistical Classification of Disease and Related Health Problems (10th revision); LOS, length of stay; NS, not significant.
Discussion
Our study was set within the context of increasing demand for ambulance services and increasing ED presentations, before the introduction of the National Emergency Access Target (NEAT), but during the time where access block was increasing. This pre-NEAT data are useful as it presents a comprehensive picture regarding the flow of patients who arrive by ambulance through the ED. Historically, because of the issues with disparate databases, the complexities around actual offload delays and subsequent flow on effects have been incompletely understood. Thus, the value in the present study is to provide the best understanding available, leading to an increased ability to decipher and present the evidence of what clinicians know and also to inform the need for targeted quality improvement. Working in a health system that mandates and monitors key priority indicators can be challenging, but offers opportunities to identify areas/hospitals where specific improvement strategies can be implemented. As an example, recent recommendations from the Queensland Department of Health indicate that 90% of patients should have an AOT delay of less than 30 min.12 Our findings indicate that specific service improvement opportunities should be offered/invested in Hospital B (74% offloaded <30 min) in order to meet the 90% target.
Characteristics and outcomes of ambulance offload time delayed patients
The ability to link patient-level records across and within systems enabled an understanding of access issues and the patient journey that encompasses the ambulance, ED and hospital admission episodes of care. Age was one of the most important factors of AOT delay. Those aged 65+ reflected a higher proportion in the AOT delayed group compared with the non-delayed for each site.
A small proportion of patient presentations via ambulance were seen within the recommended ATS time frame. This was notably better for the AOT non-delayed group (non-delayed: 42%, AOT delayed: 24%, P < 0.001). The inability to meet these time frames is concerning, given that accessibility (that includes waiting times for ED care) is one of the health system performance indicators of the National Health Performance Framework.13
Waiting time (from arrival to treatment) is one of three distinct phases of a patient’s journey through the ED.14 The other two are time to triage (from arrival) and ED LOS, both for non-admitted and admitted patients.14 Regarding time to triage, our findings indicate that time to triage for all ambulance patients (median 3 min) was within those identified by Sibbritt et al.14 and was longer for the delayed AOT group. Regarding LOS, our findings indicate that the EDs performed well for patients who were not admitted because the ED LOS was, on average, 51 min shorter than the national average of 281 min.13 However, for admitted patients, ED LOS was far longer (by 212 min) than the average of 244 min.13 This was evident at each site and the AOT delayed group had longer ED LOS compared with the non-delayed group. This long ED LOS for admitted patients is reflected in the associated levels of access block (46.5%) where more than 8 h had elapsed to access an inpatient bed. This is suggestive of access issues external to the ED, such as limited inpatient bed capacity. Other Australian research reporting access block in the early 2000s were much lower at around 5–10%, depending on the state of hospital occupancy; the higher the occupancy, the higher the access block.15
Predictors of long emergency department length of stay (>4 h) for patients arriving via ambulance
Four hour targets for EDs to see, treat, admit or discharge patients were introduced in 2004 in the UK and in 2012 in Australia (NEAT).9 Although these targets are set with good intentions (i.e. to improve timeliness of care), literature from a variety of countries indicates that achieving a 4 h target is not always possible,16 is largely hospital dependent,16 and requires organisational ownership17 and cautious forethought before implementation.16 The UK experience7 led to concerns how these targets were achieved. There was an apparent ‘last minute syndrome’ where spikes in activity during the last 20 min of the 4 h were evident and were suggested to result in target-led rather than needs-led care.18 Interviews with leadership staff from nine hospitals in England also indicated that a lack of organisational ownership contributes to negative effects on staff, incomplete process improvement and risks to patients.17 A review of the literature indicated that ‘There is no clear evidence that the target to ED completion of 98% of patients in 4 h in itself has had any effect on the quality of care in ED in the UK’ (p. 395).16 In our study (undertaken before the establishment of the 4 h target), only 37% of patients arriving to the ED by ambulance were admitted, transferred or discharged within 4 h. With a 4 h or 6 h mandate now in place across several countries, recommendations12 and changes have been made to service delivery in order to meet these targets. With the aim to achieve a 90% NEAT, learning from the experiences of others17 is warranted and measuring other quality indicators should also be considered.19
Knowing what predictors are associated with a long ED LOS can help identify which patients are less likely to meet the NEAT target. Hospital admission was the strongest predictor of an ED LOS >4 h for patients arriving to the ED by ambulance, with odds five times that of patients not admitted. Older age and offload times exceeding 30 min were also strong predictors of an ED LOS >4 h, with all having an OR greater than 1.5. This is consistent with other research from the USA20 and France.21
Admission to hospital and subsequent time to make this decision could be considered a possible modifiable component, and given it had the largest OR (five times that of those with ED LOS <4 h), it warrants further exploration. Two main factors might influence this predictor. First, the process of hospital admission might have resulted in a longer ED LOS for admitted patients. That is, the time taken to refer, review, admit and transfer patients in need of admission might take more time than the discharge of patients from ED. Efforts to shorten one or more of these time periods would require concerted efforts to involve inpatient teams and could reduce ED LOS. Second, the use of hospital avoidance models and pathways for patients who would normally be admitted might have an effect on ED LOS. Examples of where these have been shown to be effective in preventing/reducing admission requirement include: antibiotic use in a ‘hospital at home’ or outpatient approach,22 hospital in the nursing home,23 palliative care24 and early pregnancy assessment clinics.25 Imperative to these models appear to be a careful patient selection and dedicated person/team approach. The integration of ambulance service providers within these teams, as appropriate, warrants consideration.
The other modifiable predictor of an ED LOS >4 h was AOT delay. It should be noted that this AOT delay likely reflects a broader systems issue that warrants review. In the interim, targeted improvements in the ED arrival process for ambulance patients might be useful. The use of ‘offload nurses’ within EDs has been reported in Canada since 2008.26 Funded by the ambulance service, the offload nurse role can operate up to 24/7, 365 days per year,26 and receive up to five ambulance patients at a time to enable paramedics to respond back to the surrounding community. The effectiveness of these ‘offload nurse’ roles will require formal evaluation.
The non-modifiable predictors of long ED LOS for patients presenting via ambulance can be used to inform clinicians of ‘high risk groups’ for which a targeted intervention might be useful, particularly patients over 65 years (80% in our study had an ED LOS of >4 h). Specific recommendations for the management of older persons in the ED are available from a number of organisations (such as the Australian and New Zealand Society of Geriatric Medicine, ANZSGM,27 and the American Geriatrics Society).28 Although recommendations on the care of elderly patients in the ED have been developed, the uptake and application of these within EDs are currently unclear.
Limitations
Various terms (e.g. ‘ambulance offload delay’, ‘drop off delay’, ‘ambulance ramping’ and ‘handover delay’), definitions and time frames (>15 min,2 <30 min, 30–60 min and >60 min29) are used in the literature to describe waiting times to offload ambulance patients into the ED. Consistency is required, given the potential implication on patient safety outcomes30 and to enable local, national and international comparisons. The definition and time frame (>30 min) used in our study was based on clinical relevance and has been used in other recent Australian reports and research.12,29
This was a retrospective analysis of prospectively collected data. As such, there might have been inaccuracies within the data provided; however, this issue is not unique to our study.29 Fourteen per cent of ambulance arrivals were unable to be analysed, and so interpretation of our results should consider this. Because of the nature of missing data (e.g. age, date and time), comparison for analysable factors for missing data cases versus cases with available data was unable to be performed. Because of the large volume of data analysed, statistical significance might not necessarily relate to clinical significance. However, sample size was not the only factor determining significance, as not all outcomes were significant.
Conclusion
The aim of the present study was to describe and compare outcomes for patients who arrive to the ED via ambulance and experienced delays. The present study confirms that transport by ambulance to hospital does not guarantee timely access to medical care while there is AOT delay and blocked access to hospital inpatient beds. Along with older age, triage category (ATS 2, 3, 4) and offload times exceeding 30 min are easily identifiable predictors of an ED LOS of >4 h. The whole patient journey needs to be included in future planning and in the design of health services. Strategic innovation needs careful analysis to ensure that the intervention does not shift the problem onto another part of the system.
Acknowledgments
We acknowledge and thank the staff from the hospital and ambulance service decision support services for extracting data for the researchers.
We received funding from the Queensland Emergency Medicine Research Foundation, Gold Coast Hospital Foundation and Queensland Ambulance Service to undertake the present study.
Competing interests
Several authors were employees at the institution where this study was undertaken. The authors alone are responsible for the content and writing of the paper. GK is a section editor for Emergency Medicine Australasia.
References
- Sun BC, Hsia RY, Weiss RE, et al. Effect of emergency department crowding on outcomes of admitted patients. Ann. Emerg. Med. 2013;61:605–11.e6. doi: 10.1016/j.annemergmed.2012.10.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hitchcock M, Crilly J, Gillespie B, Chaboyer W, Tippett V, Lind J. The effect of ambulance ramping on emergency department length of stay and in-patient mortality. Aust. Emerg. Nurs. J. 2010;13:17–24. [Google Scholar]
- Cooney DR, Millin MG, Carter A, Lawner BJ, Nable JV, Wallus HJ. Ambulance diversion and emergency department offload delay: resource document for the National Association of EMS Physicians Position Statement. Prehosp. Emer. Care. 2011;15:555–561. doi: 10.3109/10903127.2011.608871. [DOI] [PubMed] [Google Scholar]
- Australian Institute of Health and Welfare (AIHW) Australian Hospital Statistics 2007–2008 Health Service Series no. 33. Cat. No. HSE 71. Canberra: AIHW; 2009. [Google Scholar]
- Institute of Medicine. Future of Emergency Care – Hospital-Based Emergency Care: At the Breaking Point. Washington, DC: National Academy Press; 2006. [Google Scholar]
- Australian Commission on Safety and Quality in Health Care (ACSQHC) 2010. Australian Safety and Quality Framework for Health Care. [Cited 26 Apr 2015.] Available from URL: http://www.safetyandquality.gov.au/wp-content/uploads/2012/04/Australian-SandQ-Framework1.pdf. [DOI] [PubMed]
- Letham K, Gray A. The four hour target in the NHS emergency departments: a critical comment. Emergencias. 2012;24:69–72. [Google Scholar]
- National Health. 2012. Performance Authority. National Health Reform: Performance and accountability framework. [Cited 26 Apr 2015.] Available from URL: http://www.nhpa.gov.au/internet/nhpa/publishing.nsf/Content/PAF.
- Council of Australian Governments. 2011. The National Health Reform Agreement - National Partnership Agreement on Improving Public Hospital Services. [Cited 27 Apr 2015.] Available from URL: http://www.federalfinancialrelations.gov.au/content/npa/health_reform/national-workforce-reform/national_partnership.pdf.
- Australian Bureau of Statistics. 2010. National Regional Profile 2006–2010 [Cited 26 Apr 2015.] Available from URL: http://stat.abs.gov.au/itt/r.jsp?databyregion#/
- Crilly J, O’Dwyer J, O’Dwyer M, et al. Linking ambulance, emergency department and hospital admissions data: understanding the emergency journey. Med. J. Aust. 2011;194:S34–37. doi: 10.5694/j.1326-5377.2011.tb02941.x. [DOI] [PubMed] [Google Scholar]
- Queensland Government. 2012. Metropolitan Emergency Department Access Initiative: A report on ambulance ramping in metropolitan hospitals. Queensland Government. [Cited 26 Apr 2015.] Available at URL: http://www.health.qld.gov.au/publications/medai-report/final_medai_report.pdf.
- Australian Institute of Health and Welfare. Australian Hospital Statistics 2008–2009 Health series no. 17. Cat. No. HSE 84. Canberra: AIHW; 2010. [Google Scholar]
- Sibbritt D, Isbister GK, Walker R. Emergency department performance indicators that encompass the patient journey. Qual. Manag. Health Care. 2006;15:27–38. doi: 10.1097/00019514-200601000-00004. [DOI] [PubMed] [Google Scholar]
- Sprivulis PC, Da Silva JA, Jacobs IG, Frazer AR, Jelinek GA. The association between hospital overcrowding and mortality among patients admitted via Western Australian emergency departments. MJA. 2006;184:208–212. doi: 10.5694/j.1326-5377.2006.tb00416.x. [DOI] [PubMed] [Google Scholar]
- Jones P, Schimanski K. The four hour target to reduce emergency department waiting time: a systematic review of clinical outcomes. Emerg. Med. Australas. 2010;22:391–398. doi: 10.1111/j.1742-6723.2010.01330.x. [DOI] [PubMed] [Google Scholar]
- Weber EJ, Mason S, Carter A, et al. Emptying the corridors of shame: organisational lessons learnt from England’s 4 h emergency throughput target. Ann. Emerg. Med. 2011;57:79–88. doi: 10.1016/j.annemergmed.2010.08.013. [DOI] [PubMed] [Google Scholar]
- Mason S, Nicholl J, Locker T. Four hour emergency target: targets still lead care in emergency departments. B.M.J. 2010;341:c3579. doi: 10.1136/bmj.c3579. [DOI] [PubMed] [Google Scholar]
- Keijzers G. NEAT in need of a sweet spot. Emerg. Med. Australas. 2014;26:217–218. doi: 10.1111/1742-6723.12242. [DOI] [PubMed] [Google Scholar]
- Wiler JL, Handel DA, Ginde AA, et al. Predictors of patient length of stay in 9 emergency departments. Am. J. Emerg. Med. 2012;30:1860–1864. doi: 10.1016/j.ajem.2012.03.028. [DOI] [PubMed] [Google Scholar]
- Casalino E, Wargon M, Peroziello A, et al. Predictive factors for longer length of stay in an emergency department: a prospective multicentre study evaluating the impact of age, patient’s clinical acuity and complexity, and care pathways. Emerg. Med. J. 2014;31:361–368. doi: 10.1136/emermed-2012-202155. [DOI] [PubMed] [Google Scholar]
- Gooday C, Hallam C, Sieber C, et al. An antibiotic formulary for a tertiary care foot clinic: admission avoidance using intramuscular antibiotics for borderline foot infections in people with diabetes. Diabet. Med. 2013;30:581–589. doi: 10.1111/dme.12074. [DOI] [PubMed] [Google Scholar]
- Crilly J, Chaboyer W, Wallis M, Thalib L, Polit D. An outcomes evaluation of an Australian Hospital in the Nursing Home admission avoidance programme. J. Clin. Nurs. 2011;20:1178–1187. doi: 10.1111/j.1365-2702.2010.03371.x. [DOI] [PubMed] [Google Scholar]
- Rosenberg M, Rosenberg L. Integrated model of palliative care in the emergency department. West. J. Emerg. Med. 2013;14:633–636. doi: 10.5811/westjem.2013.5.14674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wendt K, Crilly J, Beatson N. An evaluation of early pregnancy outcomes in one Australian Emergency Department: Part 2. Aust. Emerg. Nurs. J. 2012;15:77–85. [Google Scholar]
- Community Services Department. 2013. Hamilton Paramedic Service. Dedicated Offload Nurses to Receive Ambulance Patients in Hospital Emergency Departments. [Cited 26 Apr 2015.] Available from URL: https://www.hamilton.ca/NR/rdonlyres/51175727-E619-43FF-8B1F-9BD65DB60863/0/Mar25_5_3__CS13014__Dedicated_Offload_Nurses_t.pdf.
- 2008. Australian and New Zealand Society of Geriatric Medicine. Position Statement No. 14. The management of older patients in the emergency department. [Cited 26 Apr 2015.] Available from URL: http://www.anzsgm.org/ManagementofOlderPatientsintheEmergencyDepartment.pdf.pdf.
- The American Geriatrics Society. 2014. Press Release. How to care for older adults in the Emergency Department: medical groups issue comprehensive guidelines. [Cited 26 Apr 2015]. Available from URL: http://geriatricscareonline.org/ProductAbstract/geriatric-emergency-department-guidelines/CL013.
- Cone DC, Middleton PM, Marashi Pour S. Analysis and impact of delays in ambulance to emergency department handovers. Emerg. Med. Australas. 2012;24:525–533. doi: 10.1111/j.1742-6723.2012.01589.x. [DOI] [PubMed] [Google Scholar]
- Cooney DR, Wojcik S, Seth N, Vasisko C, Stimson K. Evaluation of ambulance offload delay at university hospital emergency department. Int. J. Emerg. Med. 2013;6:15. doi: 10.1186/1865-1380-6-15. [DOI] [PMC free article] [PubMed] [Google Scholar]


