Abstract
The association between SES and health is well established; however, only a handful of studies have investigated the relationship between SES and daily cortisol parameters. Further, within this small literature, virtually no studies have looked at psychological factors that might mitigate this relationship. In this study, we tested whether life satisfaction—the overall subjective affective assessment of one’s own life—acts as a protective factor against cortisol dysregulation driven by low-SES. Among a large sample (N = 1,325) of individuals from the Midlife in the United States (MIDUS) survey, we found that low-SES individuals with high levels of life satisfaction had a cortisol circadian profile similar to those of high-SES individuals. In contrast, low-SES individuals reporting low life satisfaction experienced attenuated morning cortisol concentrations and a flatter (“less healthy”) diurnal cortisol slope. Although more studies are needed to investigate the constellation of psychological resources and processes through which life satisfaction exerts its effects, the current work shows that the general affective evaluation of one’s own life acts as a buffer against the detrimental effect of low-SES on health-related physiological processes.
Keywords: SES, Diurnal Cortisol, Life Satisfaction, Psychological Well-being
The impact of socioeconomic status (SES) on health has been scientifically investigated for decades, with low SES consistently identified as a reliable predictor of greater risk for poor health (Adler et al., 1994). A more recent challenge for researchers has been to identify the biological pathways through which chronic stress associated with low SES exerts its deleterious effect on health. The end product of the hypothalamic-pituitary adrenal (HPA) axis, cortisol, is widely viewed as one the main indicators of the individual cumulative physiological risk associated with chronic stress. Cortisol secretion follows a diurnal rhythm, with higher levels at awakening followed by an acute rise about 30 minutes later (i.e., Cortisol Awakening Response or CAR) and a progressive decline across the rest of the day (i.e., cortisol slope). Flattened cortisol circadian profiles have been showed to have negative implications for physical health (Kumari et al., 2010), including mortality (Kumari et al., 2011); therefore, it is not surprising that low-SES has been associated with flatter cortisol rhythms, with low cortisol levels at awakening and a less steep decline of cortisol throughout the day (Cohen et al., 2006; Gustafsson et al., 2010; Hajat et al., 2010; Dowd et al., 2011).
Life satisfaction, the overall subjective affective assessment of one’s own life (Pavot et al., 1991), has also been identified as a reliable predictor of good health and longevity; however, only few studies have looked at which physiological processes might be affected by this aspect of psychological well-being (Cacioppo et al., 2000). For example, no empirical study has tested whether low life satisfaction is associated with diurnal cortisol parameters predictive of undesirable health outcomes (e.g., flatter diurnal cortisol slope). Further, in various studies (Koivumaa-Honkanen et al., 2000; Siahpush et al., 2008), life satisfaction seems to predict positive health outcomes above and beyond SES, suggesting that SES and life satisfaction, albeit modestly correlated, might be two distinct pathways toward better health.
Within this framework, we hypothesized that life satisfaction may act as a protective factor against the detrimental effect of low-SES on physiological processes implicated on health. In other words, being satisfied with one’s life might buffer the physiological costs of low-SES. This novel hypothesis awaits empirical testing and is the central focus on the current study, wherein various parameters of diurnal cortisol were investigated.
Method
Data were drawn from the National Study of Daily Experiences (NSDE II; n = 2,022), a subsample of Midlife in the United States (MIDUS) II – the second wave of data collection for MIDUS I, a large panel survey of adults between the ages of 25 and 74. The NSDE II included four days of salivary cortisol collection and eight days of daily phone interviews. For the current study, inclusion criteria required that participants did not have missing values for the variables of interest during MIDUS II, and cortisol data collection for NSDE II. The sample consisted of 1,325 adults (54.6% female, 95.7% White/Caucasian; age, M = 56.6 years, SD = 11.7 years).
Measures
Socioeconomic status (SES)
Similarly to previous studies (Gruenewald et al., 2012), self-report data from various sources were used to derive an index of SES. Five indicators were used: education level (from 1 - no school/some grade school, to 12 - any type of doctorate), current financial situation (11 point Likert scale), difficulty in paying bills (1 - difficult, 2 - not very difficult, 3 - not at all difficult), participant wage on the last calendar year (from 1 - less than $0, to 42 - $200,000 or more), availability of money to meet basic needs (1 - not enough, 2 - just enough, 3 - more than enough). Scores on each of these scales, which all correlated among each other (average r = .305, range r = .092−.675, lowest p = .001), were standardized (i.e., z-scores) and a composite was computed, with high scores indicating higher SES.
Life satisfaction
Life satisfaction was assed using a four-item scale in which participants were asked to report on a scale from 0 to 10 the quality of their overall life, work, health, and family1 (α = .65). For example, people were asked: “On a scale of 0 to 10, where 0 means the worst and 10 means the best, how would you rate your life these days?”. Higher scores in the scale reflect higher levels of life satisfaction (Prenda and Lachman, 2001).
Salivary cortisol
Salivary cortisol was collected using Salivettes (Sarstedt, Rommelsdorft, Germany). On average, saliva collection during NSDE II occurred 20.54 months (SD = 13.57) after the MIDUS II questionnaire assessment. On days 2–5 of the 8-day NSDE study period, participants self-collected saliva samples at four time points each day; immediately upon waking, 30 minutes later to assess cortisol awakening response (CAR), before lunch, and at bedtime. Cortisol concentrations were quantified with a commercially available luminescence immunoassay (IBL, Hamburg, Germany) with intra-assay and interassay coefficients of variability less than 5%. Saliva collection compliance was assessed using nightly telephone interviews and paper-and-pencil logs included in the collection kits. Cortisol values were log-transformed to correct for positive skew in the cortisol distribution (Adam and Kumari, 2009). In order to make sure that all transformed scores were positive, a constant of 1 was added before the transformation.
Potential Covariates
Several standard covariates in diurnal cortisol studies (Adam and Kumari, 2009) were included in the analyses. Specifically, covariates included age, gender (male = 0, female = 1), race/ethnicity (0 = white, 1 = nonwhite), smoker (0 = non smoker, 1 = smoker), average hours of sleep and average wake time across the days of salivary cortisol sampling. In secondary analyses, we also controlled for average daily negative affect (14 items rated on 5-point Likert scale, α = .89; see for example, Almeida et al., 2001) and average daily positive affect (13 items rated on 5-point Likert scale, α = .96; see for example, Almeida et al., 2001) as a stringent test the robustness of effects of life satisfaction on cortisol parameters.
Data Analysis
Hierarchical Linear Modeling (HLM) was used for data analyses. HLM allows for the simultaneous estimation of multiple cortisol parameters (cortisol at wakeup, CAR, and slope) and the prediction of individual differences in diurnal cortisol profiles. Following prior diurnal cortisol research (Adam and Kumari, 2009), Time Since Waking, Time Since Waking-squared, and CAR (dummy coded 0 or 1) were modeled at Level-1 to provide estimates of each participant’s diurnal cortisol rhythm. At Level-2 (person-level), we first tested the effect of SES while controlling for life satisfaction, and then we included the SES X life satisfaction interaction term. In addition, to control for potential confounding effects, the covariates described above were included at Level-2. In line with prior studies (e.g., Adam et al., 2006), cortisol intercept, slope (effect of time), and CAR were all allowed to vary randomly at Level-2 (i.e., treated as random effects), while Time Since Waking-squared was treated as a fixed effect with no Level-2 predictors. Continuous person-level variables were all standardized. All significance tests were 2-tailed with robust standard errors.
Results
SES and life satisfaction were only mildly correlated (r = .289, p < .001) and, both were associated with a steeper diurnal slope, such that high-SES people (β28 = −.003, p = .024) and people reporting higher levels of life satisfaction (β27 = −.002, p = .017) experienced a steeper cortisol decline throughout the day. SES was also positively associated with morning cortisol (β08 = .032, p = .025), such that individuals with higher SES had higher levels of cortisol at awakening. The same effect was not found for life satisfaction (β07 = .011 p = .383). Neither SES (β18 = −.006, p = .537) nor life satisfaction (β17 = .019, p = .080) predicted CAR.
Next, we added the SES × life satisfaction interaction term and found that life satisfaction moderated the relation between SES and cortisol slope (β19 = .002 p = .029). In particular, the slope across the day associated with low levels of SES disappeared in those individuals who reported high levels of life satisfaction, but remained for those individuals who reported low levels of life satisfaction. Although a similar trend was found for morning cortisol, it failed to reach statistical significance (β07 = −.023 p = .077).
Both SES and life satisfaction correlated negatively with negative affect (r = −.169, p < .001 and r = −.300, p < .001, respectively) and positively with positive affect (r = .145, p < .001 and r = .364, p < .001, respectively). Thus, the same analyses when run including positive and negative affect as covariates (Model 1 and Model 2). In agreement with the initial analyses, life satisfaction moderated the relation between SES and cortisol slope (β211 = .002 p = .041). Further, life satisfaction moderated the relation between SES and morning cortisol (β011 = −.025 p = .047), such as that the initial positive covariation between SES and cortisol at wakeup was only present for those people reporting low levels of life satisfaction and disappeared for those people reporting high levels of life satisfaction. Panel A of Figure 1 depicts the diurnal cortisol slopes of high SES individuals at high (1 SD above the mean) and low (1 SD below the mean) self-reported life satisfaction, while the diurnal cortisol slopes of low SES individuals at high and low self-reported life satisfaction are depicted in Panel B of Figure 1.
Figure 1.
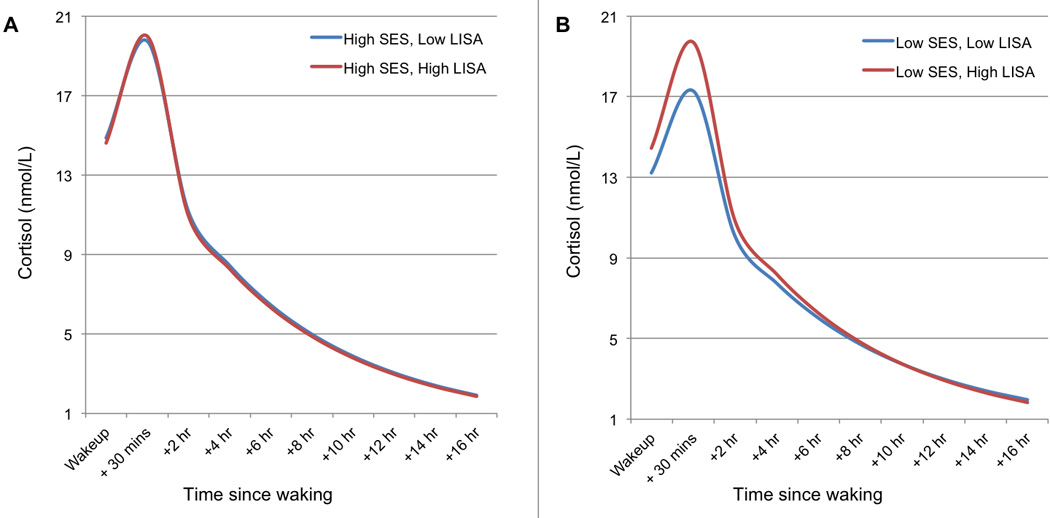
Effects of SES and self-reported life satisfaction (LISA) on diurnal cortisol levels. Cortisol level (nmol/L) is graphed as a function of time since waking for (A) high SES participants who reported high and low levels of LISA (i.e., levels 1 SD above and below the mean) and (B) low SES participants who reported high and low levels of LISA (i.e., 1 SD above and below the mean). When LISA was high, SES was not associated with cortisol slope steepness.
Discussion
Confirming previous findings, we found that high-SES individuals had higher cortisol at awakening (Dowd et al., 2011) and a steeper cortisol slope (Hajat et al., 2010). A similar cortisol decline throughout the day was also found among people reporting high levels of life satisfaction compared to their low life satisfaction counterparts. The most novel finding of the current report, however, was that life satisfaction acted as a protective factor against alterations of the HPA axis observed in low-SES individuals. Specifically, we found that low-SES individuals with high levels of life satisfaction had a cortisol circadian profile similar to those of high-SES individuals. On the other hand, individuals with lower SES and reporting low life satisfaction experienced lower morning cortisol concentrations – likely a rebound of an overactive HPA axis during the waking hours necessary to offset the physiological costs of high cortisol (Miller et al., 2007) - and a flatter diurnal cortisol slope. Neither SES nor life satisfaction nor their interaction impacted CAR.
Although wealth contributes to life satisfaction, these two aspects of well-being only partially overlap, as shown by the modest correlation in our sample. This is particularly true in wealthier societies wherein non-material needs such as sense of belonging and self-actualization come to the foreground (Diener and Diener, 2009). Given this scenario, the individual evaluation of one’s life positivity in areas other than finance appear to mitigate the negative consequences associated with low SES. This hypothesis is partially supported by those studies that showed how life satisfaction predicts health outcomes and reduced mortality above and beyond SES (Koivumaa-Honkanen et al., 2000; Siahpush et al., 2008). For example, Siahpush and colleagues (2008) found higher levels of life satisfaction were longitudinally associated with better self-reported ratings of physical health as well as less incidence of disabilities and health conditions. Koivumaa-Honkanen et al. (2000), instead, found that low levels of life satisfaction were positively associated with increased risk of mortality. Our findings provide the first empirical evidence that diurnal cortisol may be a physiological pathway through which life satisfaction imparts its protective health effects. Flatter diurnal cortisol rhythms have been found to predict incidence of metabolic and cardiovascular conditions (Kumari et al., 2010) as well as increased mortality (Kumari et al., 2011). The importance of the present finding is in showing that dysregulation in the HPA axis, which is associated with low-SES, may be able to be reversed if life satisfaction in other areas of life is promoted.
Notably, life satisfaction is not simply the mere resultant of objective life conditions, but rather the affective and cognitive assessment of one’s quality of life based on that person’s life standards/expectations (Pavot et al., 1991). Therefore, life satisfaction can be improved not only by ameliorating external life circumstances, but also interventions such as mindfulness training (Mackenzie et al., 2006), expressive writing (Wing et al., 2006), and psychotherapy aimed to improve beliefs guiding individual evaluations about one’s life. We hope that our finding will open a new line of investigation aiming at understanding the more proximal mechanisms through which life satisfaction act as a protective factor against the physiological cost associated with financial hardship.
Table 1.
HLM Models of Diurnal Cortisol Parameters
| Fixed effect (independent variable) | Model 1 |
Model 2 |
||||
|---|---|---|---|---|---|---|
| Estimate | SE | P | Estimate | SE | P | |
| Morning cortisol, π0 | ||||||
| Average Morning Cortisol (Intercept), β00 | 2.726 | 0.021 | <.001 | 2.735 | 0.021 | <.001 |
| Female, β01 | −0.111 | 0.025 | <.001 | −0.114 | 0.025 | <.001 |
| Ethnicity, β02 | −0.091 | 0.056 | 0.105 | −0.090 | 0.056 | 0.111 |
| Age, β03 | 0.036 | 0.013 | 0.006 | 0.035 | 0.013 | 0.007 |
| Average Waketime, β04 | −0.029 | 0.017 | 0.093 | −0.028 | 0.017 | 0.106 |
| Average Sleep time, β05 | 0.060 | 0.015 | <.001 | 0.061 | 0.015 | 0.000 |
| Smoker, β06 | −0.033 | 0.036 | 0.361 | −0.031 | 0.036 | 0.385 |
| Daily Positive Affect, β07 | −0.020 | 0.016 | 0.212 | −0.021 | 0.016 | 0.198 |
| Daily Negative Affect, β08 | 0.010 | 0.016 | 0.542 | 0.013 | 0.016 | 0.407 |
| Life Satisfaction, β09 | 0.020 | 0.012 | 0.107 | 0.016 | 0.012 | 0.181 |
| SES, β010 | 0.034 | 0.014 | 0.018 | 0.030 | 0.014 | 0.032 |
| SES X Life Satisfaction, β011 | -- | -- | -- | −0.025 | 0.013 | 0.047 |
| Cortisol Awakening Response, π1 | ||||||
| Average CAR, β10 | 0.342 | 0.015 | <.001 | 0.344 | 0.015 | <.001 |
| Female, β11 | 0.098 | 0.020 | <.001 | 0.097 | 0.020 | <.001 |
| Ethnicity, β12 | 0.033 | 0.046 | 0.473 | 0.033 | 0.046 | 0.469 |
| Age, β13 | 0.027 | 0.010 | 0.011 | 0.026 | 0.010 | 0.011 |
| Average Waketime, β14 | −0.006 | 0.011 | 0.564 | −0.006 | 0.011 | 0.576 |
| Average Sleep time, β15 | −0.013 | 0.011 | 0.227 | −0.013 | 0.011 | 0.228 |
| Smoker, β16 | 0.083 | 0.029 | 0.004 | 0.083 | 0.029 | 0.004 |
| Daily Positive Affect, β17 | 0.004 | 0.013 | 0.759 | 0.004 | 0.013 | 0.765 |
| Daily Negative Affect, β18 | 0.008 | 0.014 | 0.568 | 0.008 | 0.014 | 0.539 |
| Life Satisfaction, β19 | 0.020 | 0.011 | 0.080 | 0.019 | 0.011 | 0.097 |
| SES, β110 | 0.007 | 0.010 | 0.517 | 0.006 | 0.010 | 0.556 |
| SES X Life Satisfaction, β111 | -- | -- | -- | −0.004 | 0.008 | 0.602 |
| Time Since Waking, π2 | ||||||
| Average Linear Slope, β20 | −0.135 | 0.004 | <.001 | −0.136 | 0.004 | <.001 |
| Female, β21 | 0.002 | 0.002 | 0.4 | 0.002 | 0.002 | 0.354 |
| Ethnicity, β22 | 0.021 | 0.006 | <.001 | 0.021 | 0.006 | <.001 |
| Age, β23 | 0.006 | 0.001 | <.001 | 0.006 | 0.001 | <.001 |
| Average Waketime, β24 | −0.001 | 0.001 | 0.668 | −0.001 | 0.001 | 0.642 |
| Average Sleep time, β25 | −0.007 | 0.001 | <.001 | −0.007 | 0.001 | <.001 |
| Smoker, β26 | 0.016 | 0.003 | <.001 | 0.016 | 0.003 | <.001 |
| Daily Positive Affect, β27 | 0.001 | 0.001 | 0.301 | 0.001 | 0.001 | 0.286 |
| Daily Negative Affect, β28 | 0.002 | 0.001 | 0.073 | 0.002 | 0.001 | 0.099 |
| Life Satisfaction, β29 | −0.002 | 0.001 | 0.029 | −0.002 | 0.001 | 0.043 |
| SES, β210 | −0.002 | 0.001 | 0.03 | −0.002 | 0.001 | 0.052 |
| SES X Life Satisfaction, β211 | -- | -- | -- | 0.002 | 0.001 | 0.041 |
| Time Since Waking2, π3 | ||||||
| Average Curvature, β30 | 0.002 | 0.0002 | <.001 | 0.002 | 0.0002 | <.001 |
Note. Intercepts indicate average cortisol values at wakeup; average slopes of time since waking indicate change in cortisol per 1-hour change in time; average slopes of time since waking2 indicate change in cortisol per 1-hour change in time2. CAR = Cortisol Awakening Response.
Highlights.
Among 1,325 adults, low socioeconomic status and low life satisfaction independently predicted a flatter diurnal cortisol slope.
Low socioeconomic status predicted low morning cortisol.
Life satisfaction buffered the effect of socioeconomic status of cortisol slope.
Effects remained significant after controlling for both demographics and psychological factors.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
The family satisfaction item was created by averaging scores for relationship with spouse/partner and relationship with children as indicated in the original study (Prenda and Lachman, 2001).
References
- Adam EK, Hawkley LC, Kudielka BM, Cacioppo JT. Day-to-day dynamics of experience–cortisol associations in a population-based sample of older adults. Proceedings of the National Academy of Sciences. 2006;103:17058–17063. doi: 10.1073/pnas.0605053103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adam EK, Kumari M. Assessing salivary cortisol in large-scale, epidemiological research. Psychoneuroendocrinology. 2009;34:1423–1436. doi: 10.1016/j.psyneuen.2009.06.011. [DOI] [PubMed] [Google Scholar]
- Adler NE, Boyce T, Chesney MA, Cohen S, Folkman S, Kahn RL, Syme SL. Socioeconomic status and health: the challenge of the gradient. Am. Psychol. 1994;49:15–24. doi: 10.1037//0003-066x.49.1.15. [DOI] [PubMed] [Google Scholar]
- Almeida DM, Wethington E, McDonald DA. Daily variation in paternal engagement and negative mood: Implications for emotionally supportive and conflictual interactions. Journal of Marriage and Family. 2001;63:417–429. [Google Scholar]
- Cacioppo JT, Burleson MH, Poehlmann KM, Malarkey WB, Kiecolt-Glaser JK, Berntson GG, Uchino BN, Glaser R. Autonomic and neuroendocrine responses to mild psychological stressors: effects of chronic stress on older women. Ann. Behav. Med. 2000;22:140–148. doi: 10.1007/BF02895778. [DOI] [PubMed] [Google Scholar]
- Cohen S, Doyle WJ, Baum A. Socioeconomic status is associated with stress hormones. Psychosom. Med. 2006;68:414–420. doi: 10.1097/01.psy.0000221236.37158.b9. [DOI] [PubMed] [Google Scholar]
- Diener E, Diener M. Culture and well-being. Springer; 2009. Cross-cultural correlates of life satisfaction and self-esteem; pp. 71–91. [DOI] [PubMed] [Google Scholar]
- Dowd JB, Ranjit N, Do DP, Young EA, House JS, Kaplan GA. Education and levels of salivary cortisol over the day in US adults. nn. Behav. Med. 2011;41:13–20. doi: 10.1007/s12160-010-9224-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruenewald TL, Karlamangla AS, Hu P, Stein-Merkin S, Crandall C, Koretz B, Seeman TE. History of socioeconomic disadvantage and allostatic load in later life. Soc. Sci. Med. 2012;74:75–83. doi: 10.1016/j.socscimed.2011.09.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gustafsson PE, Janlert U, Theorell T, Hammarström A. Life-course socioeconomic trajectories and diurnal cortisol regulation in adulthood. Psychoneuroendocrinology. 2010;35:613–623. doi: 10.1016/j.psyneuen.2009.09.019. [DOI] [PubMed] [Google Scholar]
- Hajat A, Diez-Roux A, Franklin TG, Seeman T, Shrager S, Ranjit N, Castro C, Watson K, Sanchez B, Kirschbaum C. Socioeconomic and race/ethnic differences in daily salivary cortisol profiles: the multi-ethnic study of atherosclerosis. Psychoneuroendocrinology. 2010;35:932–943. doi: 10.1016/j.psyneuen.2009.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koivumaa-Honkanen H, Honkanen R, Viinamäki H, Heikkilä K, Kaprio J, Koskenvuo M. Self-reported life satisfaction and 20-year mortality in healthy Finnish adults. Am. J. Epidemiol. 2000;152:983–991. doi: 10.1093/aje/152.10.983. [DOI] [PubMed] [Google Scholar]
- Kumari M, Chandola T, Brunner E, Kivimaki M. A nonlinear relationship of generalized and central obesity with diurnal cortisol secretion in the Whitehall II study. The Journal of Clinical Endocrinology & Metabolism. 2010;95:4415–4423. doi: 10.1210/jc.2009-2105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumari M, Shipley M, Stafford M, Kivimaki M. Association of diurnal patterns in salivary cortisol with all-cause and cardiovascular mortality: findings from the Whitehall II study. The Journal of Clinical Endocrinology & Metabolism. 2011;96:1478–1485. doi: 10.1210/jc.2010-2137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mackenzie CS, Poulin PA, Seidman-Carlson R. A brief mindfulness-based stress reduction intervention for nurses and nurse aides. Appl. Nurs. Res. 2006;19:105–109. doi: 10.1016/j.apnr.2005.08.002. [DOI] [PubMed] [Google Scholar]
- Miller GE, Chen E, Zhou ES. If it goes up, must it come down? Chronic stress and the hypothalamic-pituitary-adrenocortical axis in humans. Psychol. Bull. 2007;133:25–45. doi: 10.1037/0033-2909.133.1.25. [DOI] [PubMed] [Google Scholar]
- Pavot W, Diener E, Colvin CR, Sandvik E. Further validation of the Satisfaction with Life Scale: Evidence for the cross-method convergence of well-being measures. J. Person. Assess. 1991;57:149–161. doi: 10.1207/s15327752jpa5701_17. [DOI] [PubMed] [Google Scholar]
- Prenda KM, Lachman ME. Planning for the future: a life management strategy for increasing control and life satisfaction in adulthood. Psychol. Aging. 2001;16:206. [PubMed] [Google Scholar]
- Siahpush M, Spittal M, Singh GK. Happiness and life satisfaction prospectively predict self-rated health, physical health, and the presence of limiting, long-term health conditions. Am. J. Health Promot. 2008;23:18–26. doi: 10.4278/ajhp.061023137. [DOI] [PubMed] [Google Scholar]
- Wing JF, Schutte NS, Byrne B. The effect of positive writing on emotional intelligence and life satisfaction. J. Clin. Psychol. 2006;62:1291–1302. doi: 10.1002/jclp.20292. [DOI] [PubMed] [Google Scholar]


