Abstract
Background
Disparities in trauma outcomes based on insurance and race are especially pronounced among young adults who have relatively high uninsured rates and incur a disproportionate share of trauma in the population. The 2010 dependent coverage provision (DCP) of the Affordable Care Act (ACA) allowed young adults to remain on their parent’s health insurance plans until age 26, leading to over 3 million young adults gaining insurance. We investigated the impact of the DCP on racial disparities in coverage expansion among trauma patients.
Study Design
Using the 2007–2012 National Trauma Databank, we compared changes in coverage among 529,844 19–25 year-olds to 484,974 controls aged 27–34 not affected by the DCP. Subgroup analyses were conducted by race and ethnicity and by census region.
Results
The pre-DCP uninsured rates among young adults were highest among black patients (48.1%) and Hispanic patients (44.3%), and significantly lower among Non-Hispanic white patients (28.9%). However, Non-Hispanic white young adults experienced a significantly greater absolute reduction in the uninsured rate (−4.9 percentage points) than black (−2.9, p=0.01) and Hispanic (−1.7, p<0.001) young adults. These absolute reductions correspond to a 17.0% relative reduction in the uninsured rate for white patients, 6.1% for black patients, and 3.7% for Hispanic patients. Racial disparities in the provision’s impact on coverage among trauma patients were largest in the South and West census regions (p<0.01).
Conclusions
While the DCP increased insurance coverage for young adult trauma patients of all races, both absolute and relative racial disparities in insurance coverage widened. The extent of these racial disparities also differed by geographic region. Though this policy produced overall progress towards greater coverage among young adults, its heterogeneous impact by race has important implications for future disparities research in trauma.
Keywords: trauma, race, disparities, insurance, health policy, ACA, NTDB
Introduction
Trauma continues to be the most common cause of death and physical disability among young adults in the United States (1). Trauma often requires complex acute care from providers across disciplines and extensive post-acute care rehabilitation and follow-up. Therefore, ensuring adequate access to high quality care through health insurance coverage is a priority for policymakers and trauma surgeons alike. Historically, young adults in the United States have had the highest uninsured rates of any age group, with 2010 estimates suggesting that 30% of young adults were uninsured (2). This age group also bears a disproportionate share of the trauma burden in the U.S. population (3). For racial and ethnic minorities, uninsured rates among young adults are even higher (4), and multiple studies have demonstrated that uninsured trauma patients receive less care and experience worse clinical outcomes (5–12)—though the underlying mechanisms remain unclear.
The 2010 Dependent Coverage Provision (DCP) was among the earliest enacted provisions of the Affordable Care Act (ACA), aiming to increase health insurance coverage rates in the U.S. The DCP specifically targeted young adults by allowing individuals to remain on their parents’ insurance plan until their 26th birthday. Early analyses of the DCP showed that as many as 3 million young adults gained coverage by the end of 2011 (13), with estimates of the decline in the uninsured rates ranging from 3 to 10 percentage points depending on the population analyzed (13–19). A 2012 study on young adult patients presenting to emergency departments showed an increase in the proportion of non-discretionary visits covered by private insurance after the DCP (18). A recent 2015 study showed that young adults treated at trauma centers experienced a 3.4 percentage point reduction in uninsured rates (20). However, the specific effect of this policy on existing racial disparities in insurance coverage among trauma patients has not been well characterized. Given the current surgical literature on existing racial disparities for trauma care (5,6,10,21–23), empirical data on whether the DCP reduced disparities would fill a critical gap in knowledge. Prior to enactment of federal insurance oversight by the ACA, insurance policies were regulated predominantly by the states, and as such pre-policy dependent coverage varied significantly across the country. Given the regional variations in population by race as well as variations in dependent coverage legislation, an analysis of changing patterns in racial disparities by geographic region is needed to better understand the potential impact of additional regional variation in implementing other key coverage expansion provisions of the ACA. The objective of the current study therefore, is to evaluate the impact of the DCP on racial disparities in coverage expansions, both nationally and regionally, among young adults with traumatic injury.
Methods
Analytic Sample
We performed a retrospective analysis of the NTDB from years 2007–2012. Our analytic data sample included 841,600 patients between the ages of 19 and 34 years old with known race during 2007–2009 and 2011–2012. Because the DCP began in September of 2010, we considered 2010 as a “washout year” and thus excluded all patient encounters during that year from the analysis. Inclusion of 2010 in sensitivity did not meaningfully alter the results. After applying age and year exclusion criteria, there were 40,123 patient encounters with missing race, but as this represented only 4.8% of our sample, they were excluded from our final analytic sample (Supplementary Appendix 1, online only).
Our treatment group consisted of young adults aged 19–25 (n=529,844), representing those eligible for the DCP. We defined our control group as 27–34 year olds (n=484,974) with similar demographics, insurance coverage rates, labor market trends, underlying medical problems, and injury characteristics (3,15,24).
Variables
Race was the main independent variable of interest, defined by a categorization system commonly used in other studies (5). Specifically, we defined the following mutually exclusive categories: Hispanic, white non-Hispanic, black non-Hispanic, or other non-Hispanic. Insurance status was as our key outcome variable. Insurance status was categorized into private coverage (including Blue Cross/Blue Shield, Private/Commercial Insurance, and workers’ compensation), public coverage (including Medicare, Medicaid, and other government), other (including no fault automobile and other), and uninsured (coded as “self pay” in the NTDB). For the main analysis, we focused on the change in proportion of uninsured patients within the study population.
Analysis
We first provided a descriptive analysis of pre-policy characteristics of our treatment and control groups (2007–2009) to compare patient demographics, including age, gender, and race, and injury characteristics including injury severity score (ISS, a measure of anatomic severity), revised trauma score (RTS, a measure of physiologic injury severity), blunt versus penetrating injury type, mechanism of injury, and the presence of a severe head injury or severe extremity injury. We also compared the groups on the following facility characteristics: level-1 or non-level-1 trauma center, teaching status, non-profit status, and safety-net status (safety-net hospitals defined as the top decile of facilities ranked by proportion of patients with no insurance or Medicaid) (7,25). All comparisons of treatment to control groups relied upon t-tests for continuous variables and chi-squared (χ2) tests for categorical variables.
Second, we employed a quasi-experimental difference-in-differences (DID) approach to compare changes in the uninsured rates in the treatment group before and after the DCP to the changes in our control group. This approach takes into account secular trends and assumes that these trends would have been similar for the two age groups in the absence of the DCP. It also accounts for time-invariant differences between the treatment and control group by adjusting for baseline differences in outcomes. To evaluate the effect of the DCP on young adults, we defined the pre-policy period as 2007–2009 and the post-policy period as 2011–2012.
We then performed three primary analyses. First we used a DID model to examine how the uninsured rate changed among 19–25 year old trauma patients before and after the DCP, as compared to 26–34 year olds, stratified by race. Second, we tested for between-race differences in the policy’s impact by adding to this model an interaction term between post-period, young adult, and race. Lastly, because pre-DCP policies regulating dependent insurance coverage varied by state, and because of the significant variation in racial make up of state populations, we performed a between-race DID analysis further stratified by geographic region (defined as Northeast, South, Midwest, and West).
This study was approved by the Institutional Review Board of Harvard Medical School. All analyses were completed using Stata version 13.0 (StataCorp). A two-sided p value of 0.05 was used to establish statistical significance.
Results
Table 1 shows descriptive statistics for the sample, comparing the 19–25 year olds and 27–34 year olds. Due to the large sample size, a number of differences in groups (injury type, mechanism, and severity among them) were statistically significant but did not appear to be clinically meaningful. The baseline uninsured rate for 19–25 year old trauma patients prior to the initiation of the DCP in our sample was 35.3%.
Table 1.
Patient and Injury Characteristics, 2007–2009
| Ages 19 to 25 y | Ages 27 to 34 y | p Values | |
|---|---|---|---|
| Total encounters, n | 187,584 | 166,970 | |
| Mean age, y | 21.8 | 29.7 | <0.001 |
| Male, % | 76 | 76 | 0.20 |
| Race/Ethnicity, % | <0.001 | ||
| White | 54.6 | 54.5 | |
| Black | 21.1 | 20.6 | |
| Hispanic | 17.5 | 18.2 | |
| Other | 6.8 | 6.7 | |
| Insurance type, % | <0.001 | ||
| Private | 31.3 | 32.4 | |
| Public | 18.2 | 18.7 | |
| Other | 15.2 | 14.0 | |
| Uninsured | 35.3 | 35.3 | |
| Intent, % | <0.001 | ||
| Unintentional | 72.0 | 74.0 | |
| Self-Harm | 2.1 | 2.4 | |
| Assault | 26.0 | 24.0 | |
| Mechanism, % | <0.001 | ||
| Fall | 10.1 | 13.8 | |
| Gun shot wound | 12.2 | 9.6 | |
| Motor vehicle collision | 41.0 | 36.2 | |
| Motorcycle | 6.1 | 7.0 | |
| Other | 6.8 | 8.6 | |
| Pedestrian/bicyclist | 5.2 | 5.4 | |
| Stab | 8.8 | 9.1 | |
| Struck | 9.7 | 10.4 | |
| Critical Injury, ISS ≥ 25, % | 34.6 | 32.2 | <0.001 |
| Traumatic brain injury, % | 20.0 | 18.1 | <0.001 |
| Severe extremity injury, % | 12.7 | 12.0 | <0.001 |
| Level 1 trauma center, % | 64.0 | 65.0 | <0.001 |
| Safety net hospital, % | 11.0 | 11.3 | 0.01 |
| Non-profit hospital, % | 94.0 | 94.0 | 0.21 |
| University teaching hospital, % | 56.0 | 57.0 | <0.001 |
Next, we compared the annual uninsured rates for 19–25 year olds relative to 27–34 year olds, stratified by race (Figure 1). White patients had lower pre-policy uninsured rates and greater coverage gains than did black and Hispanic patients. Table 2 shows that after controlling for age, year, and gender, the absolute decrease in the uninsured rate for 19–25 year old trauma patients after DCP implementation was 4.9 percentage points for white patients, 2.9 percentage points for black patients, and 1.7 percentage points for Hispanic patients (p<0.001 for all groups). These absolute values correspond with a 17.0% relative reduction in the uninsured rate for white patients, a 6.1% relative reduction for black patients, and a 3.7% relative reduction for Hispanic patients. The between-race DID model demonstrated that the variation in reduction of uninsured rates varied significantly by race (Table 2).
Figure 1.
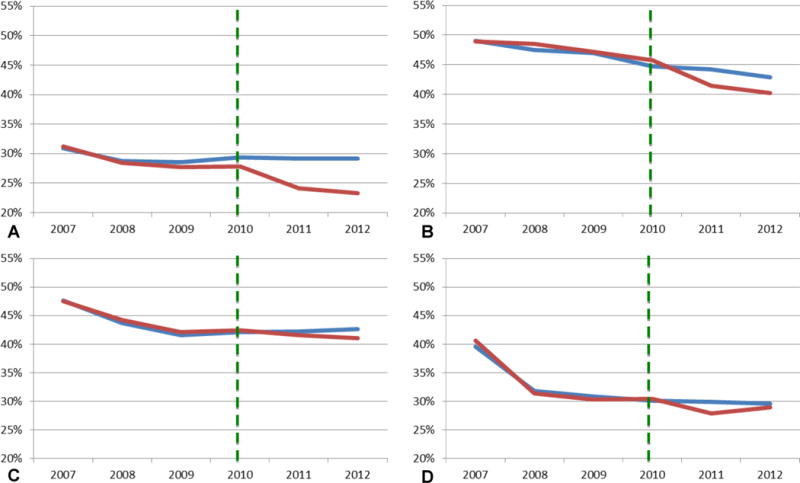
Racial variation in the change in uninsured rate after the ACA’s Dependent Coverage Provision. (A) White, non-Hispanic; (B) Black, non-Hispanic; (C) Hispanic; (D) other race. Red line, policy-eligible 19- to 25-year-olds vs blue line, policy-ineligible 26- to 34-year-olds. Green dashed line, the Affordable Care Act’s Dependent Coverage Provision (ACA-DCP) took effect in 2010. (Authors analysis of data from the National Trauma Data Bank, 2007–2012 [n = 801,477].)
Table 2.
Changes in Uninsured Rate by Race for Young Adult Trauma Patients Ages 19 to 25 years vs 26 to 34 years, Before and After the Affordable Care Act’s Dependent Coverage Provision
| Ages 19 to 25 y | Ages 26 to 34 y | Difference in change between age groups, %* | Relative change in uninsured population, % | p Value for between-group difference† | |||
|---|---|---|---|---|---|---|---|
| Uninsured Before ACA-DCP, % | Uninsured After ACA-DCP, % | Uninsured Before ACA-DCP, % | Uninsured After ACA-DCP, % | ||||
| Non-Hispanic white† | 28.9 | 23.7 | 29.2 | 29.2 | −4.9 | −17.0 | Ref |
| Non-Hispanic black† | 48.1 | 40.8 | 47.7 | 43.5 | −2.9 | −6.1 | 0.008 |
| Hispanic† | 44.3 | 41.3 | 43.9 | 42.4 | −1.7 | −3.7 | <0.001 |
Adjusted for age, year, and facility effects.
p Value for within race change is all p<0.01.
ACA, Affordable Care Act; DCP, dependent coverage provision; CI, confidence interval.
(Authors analysis of data from the National Trauma Data Bank, 2007–2012 [n = 801,477].)
Table 3 demonstrates that the pre-policy uninsured rates, the percentage-point decline in uninsured rates by race, and the variation in this decline between races all differed by geographic region. Regionally stratified uninsured rates by race ranged from 17.4–36.8% for white patients, 34.5–52.4% for black patients, and 33.5%–55.7% for Hispanic patients. White patients experienced the greatest reductions in uninsured rates in the South and the West (−5.3% and −5.1%, respectively, p<0.001 for both). Black patients experienced the greatest reductions in uninsured rates in the Midwest and the Northeast (−3.8% and −4.6% respectively, p<0.05 for both). Hispanic patients experienced a significant −5.2% decline in the Midwest (p<0.05), while all other regions showed changes that did not significantly differ from baseline (p>0.05). Notably, the most significant disparities in racial coverage change occurred in the South and West. In the Midwest and Northeast, racial disparities in coverage change were not statistically significant, with the exception of Hispanic patients in the Northeast experiencing no coverage change as compared to the −3.2% decrease in the uninsured rate experienced by white patients (p=0.042).
Table 3.
Regional Variation of Racial Disparities in Coverage Expansion after the Affordable Care Act’s Dependent Coverage Provision
| Uninsured rate for 19- to 25-year-olds, Pre-ACA DCP, %* | Adjusted change in uninsured rate, %† | p Value for subgroup change | p Value for between group change | |
|---|---|---|---|---|
| South | ||||
| White‡ | 36.8 | −5.3 | <0.001§ | Ref |
| Black‖ | 52.4 | −2.0 | 0.054 | 0.005¶ |
| Hispanic‖ | 55.7 | −1.8 | 0.075 | 0.009¶ |
| Other | 50.0 | −0.6 | 0.800 | 0.063 |
| West | ||||
| White‡ | 23.8 | −5.1 | <0.001§ | Ref |
| Black‖ | 34.5 | −2.3 | 0.131 | 0.155 |
| Hispanic‖ | 36.5 | −1.5 | 0.084 | 0.002¶ |
| Other | 30.3 | −2.6 | 0.04* | 0.086 |
| Midwest | ||||
| White‡ | 27.6 | −4.9 | <0.001§ | Ref |
| Black# | 50.9 | −3.8 | 0.012* | 0.600 |
| Hispanic# | 43.4 | −5.2 | 0.016* | 0.999 |
| Other | 29.4 | 1.0 | 0.648 | 0.004¶ |
| Northeast | ||||
| White‡ | 17.4 | −3.2 | <0.001§ | Ref |
| Black# | 37.3 | −4.6 | 0.005¶ | 0.416 |
| Hispanic‖ | 33.5 | 1.1 | 0.592 | 0.042* |
| Other | 29.9 | −0.7 | 0.787 | 0.213 |
Pre-ACA DCP: 2007 to 2009.
Change in uninsured rate among policy-eligible 19- to 25-year-olds after the policy took effect, as compared to pre-/post-policy change in uninsured rate among policy-ineligible 26- to 34-year-olds. Adjusted for: age, sex, year.
p<0.001 for within-race change in uninsured rate.
p < 0.05
p < 0.001.
p>0.05 for within-race change in uninsured rate.
p < 0.01.
p <0.05 for within-race change in uninsured rate.
p < 0.05.
ACA, Affordable Care Act; DCP, dependent coverage provision.
(Authors analysis of data from the National Trauma Data Bank, 2007–2012 [n = 801,477].)
Discussion
The ACA’s 2010 dependent coverage provision led to significant coverage gains for young adult trauma patients among all races. However, this study shows that the degree of decline in uninsured rates due to the DCP varied significantly by race, with white patients experiencing a relative 17% reduction in uninsured status, while black and Hispanic patients experienced relative reductions of 6.1 and 3.7%, respectively. These insurance coverage changes by race also varied by geographic region, with the greatest disparities occurring in the South and West. These findings suggest that for young adult patients presenting with traumatic injury, the DCP produced meaningful increases in coverage, but these gains were most concentrated among white young adults.
This study is the first to our knowledge to identify significant disparities in coverage gains between white, black, and Hispanic patients (Figure 1). An earlier study on the impact of the DCP on trauma patients showed that minorities, those with severe injuries, and those presenting to safety net hospitals saw the smallest coverage gains (20); however this study did not examine disparities between specific racial or ethnic groups, nor variation across census regions. Other studies examining the effect of the DCP on the general young adult population have shown no population-level differences in the relative degree of coverage expansion between races (4,14,15,26). In one study, a sub-group analysis by income found that non-Hispanic white patients were more likely to receive coverage than Hispanic patients among patients below 133% of the federal poverty line (4). It may be that our findings are driven in part by young adult trauma patients captured by the NTDB representing an oversampling of lower-income men more prone to high-risk activities and less likely to have parents with prior insurance coverage, as compared to prior population survey databases.
When viewing the DCP as an isolated policy, these findings suggest that for young adult trauma patients, racial disparities in uninsured rates widened. White patients had the lowest pre-policy uninsured rates and saw the greatest declines after the coverage expansion. Conversely, black and Hispanic patients had both higher pre-policy uninsured rates and experienced much smaller declines after the DCP. As the DCP is based on the presence of parental private insurance coverage, these findings are not unexpected in light of known racial disparities in labor market trends and employer-sponsored insurance coverage (27).
However, the DCP was not designed as the sole policy lever in the ACA that could reduce disparities in insurance coverage for young adults. The ACA includes an array of provisions aimed at reducing the number of uninsured individuals in the United States. Two complementary coverage expansion provisions of the ACA that are most relevant to this study and its population includes the creation of health insurance exchanges to provide coverage options for individuals who do not have employer-sponsored coverage and Medicaid expansion to increase coverage among low-income individuals. As initially designed, this multi-faceted insurance coverage expansion policy approach was meant to focus on three populations with high pre-ACA uninsured rates; namely young adults, those without employer based coverage, and low-income individuals who did not meet traditionally Medicaid eligibility (28). This study’s findings suggest that the DCP increased coverage rates among trauma patients of all races, and yet simultaneously widened pre-existing racial disparities in both relative and absolute terms. These findings provide important information for policymakers and trauma providers to better understand the changing dynamics of health care coverage among young adult trauma victims. This is especially important given the clear state-level variation in implementing state-level health insurance exchanges and Medicaid expansions in 2014.
The new health insurance exchanges could potentially aid the remaining uninsured minority population of young adult trauma patients who did not benefit from the DCP through targeted efforts to reach the young adult population most vulnerable for accidental traumatic injury, namely minorities. If successful, the insurance exchanges may help curtail some of the post-DCP widening of the racial disparities among young adult trauma patients while also attaining broader coverage goals to reduce the number of the uninsured. It is less clear, however, how the state-based Medicaid expansions will affect this persistent insurance coverage racial disparity among young adults. Given the accidental and unpredictable nature of traumatic injury and the relatively lower-wages for the young-adult population, Medicaid expansion could potentially be of significant benefit to young adults most at-risk for traumatic injury. However, given the 2012 Supreme Court ruling that allowed states to opt out of Medicaid expansion, many of these benefits will go unrealized. In fact, only 29 out of 50 states plus the District of Columbia plan to or have already implemented Medicaid expansion (29), and the regions with the most states opting out of Medicaid expansion are the regions where we found the greatest racial disparities in coverage change after the DCP. Taken together, it is unclear the degree to which these two policies will be able to curtail the unintended consequences of the DCP on widening racial disparities in insurance coverage for trauma patients.
Our study has a number of limitations. First, while the NTDB is the largest national trauma database, it is a convenience sample as opposed to being drawn from a nationally representative sample. It does contain, however, data from approximately 95% of all Level 1 trauma centers, as defined by the American College of Surgeons (ACS). Though it purposefully over-represents the most severely injured patients, the NTDB has been used throughout the clinical literature to understand racial and insurance coverage disparities in trauma care (11,30–32). Second, the NTDB is a visit-level database; thus, it does not follow individual patients over time and is potentially subject to double counting. Third, because this study relies upon a visit-level analysis with a sample limited to those individuals with a trauma event, our estimates are not analogous to previous population-based estimates of coverage changes due to the DCP. Finally, the NTDB does not provide information on patient income, a key covariate in the analysis of racial disparities. However, our analysis does not seek to explain the independent effect of one’s race on their likelihood of gaining coverage from the DCP. Rather, we seek to describe the actual, real-world effects of the policy—intentional or unintentional—on racial disparities around the country.
In conclusion, our findings show that the DCP led to a substantial decrease in uninsured rates for young adult trauma patients of all races; however, benefits of the DCP were concentrated among white patients. Worsening racial disparities in insurance coverage were most evident in the South and the West—the regions with the fewest states intending to expand Medicaid in accordance with the ACA (29). Future work will be needed to evaluate the full impact of further insurance coverage expansion, with continued implementation of the ACA, on racial disparities and clinical outcomes among the injured.
Supplementary Material
Acknowledgments
Support: Drs Sommers serves part-time and Tsai currently serves full-time as advisors in the Office of the Assistant Secretary for Planning and Evaluation, at the U.S. Department of Health and Human Services (HHS). This paper does not represent the views of HHS. Dr Sommers also receives grants from AHRQ, the National Institute for Healthcare Management, and the Commonwealth Fund. Dr Song was supported by a National Research Service Award from the National Institute on Aging (F30-AG039175).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosure Information: Nothing to disclose.
Disclaimer: Data for this study are from the Committee on Trauma, American College of Surgeons. NTDB Version 7.2 Chicago, IL, 2009. The content reproduced from the NTDB remains the full and exclusive copyrighted property of the American College of Surgeons. The American College of Surgeons is not responsible for any claims arising from works based on the original data, text, tables, or figures.
Presented at the Eastern Association for the Surgery of Trauma Annual Meeting, Lake Buena Vista, FL, January 2015.
References
- 1.Ten Leading Causes of Death by Age Group. United States – 2010 National Vital Statistics System. National Center for Health Statistics, CDC; Available at: http://www.cdc.gov/injury/wisqars/pdf/10LCID_All_Deaths_By_Age_Group_2010-a.pdf. Accessed February 24, 2015. [PubMed] [Google Scholar]
- 2.DeNavas-Walt C, Proctor BD, Smith JC. Income, poverty, and health insurance coverage in the United States: 2009. US Census Bureau; 2010. Available at: http://www.census.gov/prod/2010pubs/p60-238.pdf. Accessed February 24, 2015. [Google Scholar]
- 3.National Trauma Data Bank, Annual Report. 2012 Available at: http://www.facs.org/trauma/ntdb/pdf/ntdb-annual-report-2012.pdf. Accessed February 24, 2015.
- 4.Shane DM, Ayyagari P. Will health care reform reduce disparities in insurance coverage?: evidence from the dependent coverage mandate. Medical Care. 2014;52(6):528–34. doi: 10.1097/MLR.0000000000000134. [DOI] [PubMed] [Google Scholar]
- 5.Haider AH, Chang DC, Efron DT, et al. Race and insurance status as risk factors for trauma mortality. Arch Surg. 2008;143(10):945–9. doi: 10.1001/archsurg.143.10.945. [DOI] [PubMed] [Google Scholar]
- 6.Haider AH, Ong’uti S, Efron DT, et al. Association between hospitals caring for a disproportionately high percentage of minority trauma patients and increased mortality: a nationwide analysis of 434 hospitals. Arch Surg. 2012;147(1):63–70. doi: 10.1001/archsurg.2011.254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bell TM, Zarzaur BL. Insurance status is a predictor of failure to rescue in trauma patients at both safety net and non-safety net hospitals. J Trauma Acute Care Surg. 2013;75(4):728–33. doi: 10.1097/TA.0b013e3182a53aaa. [DOI] [PubMed] [Google Scholar]
- 8.Haas JS, Goldman L. Acutely injured patients with trauma in Massachusetts: differences in care and mortality, by insurance status. Am J Public Health. 1994;84(10):1605–8. doi: 10.2105/ajph.84.10.1605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Doyle JJ., Jr Health insurance, treatment and outcomes: using auto accidents as health shocks. Review of Economics and Statistics. 2005;87(2):256–70. [Google Scholar]
- 10.Salim A, Ottochian M, DuBose J, et al. Does insurance status matter at a public, level I trauma center? J Trauma. 2010;68(1):211–6. doi: 10.1097/TA.0b013e3181a0e659. [DOI] [PubMed] [Google Scholar]
- 11.Haider AH, Weygandt PL, Bentley JM, et al. Disparities in trauma care and outcomes in the United States. J Trauma Acute Care Surg. 2013;74(5):1195–205. doi: 10.1097/TA.0b013e31828c331d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rosen H, Saleh F, Lipsitz S, et al. Downwardly mobile: the accidental cost of being uninsured. Arch Surg. 2009;144(11):1006–11. doi: 10.1001/archsurg.2009.195. [DOI] [PubMed] [Google Scholar]
- 13.Sommers BD, Kronick R. The Affordable Care Act and insurance coverage for young adults. JAMA. 2012;307(9):913–4. doi: 10.1001/jama.307.9.913. [DOI] [PubMed] [Google Scholar]
- 14.Barbaresco S, Courtemanche CJ, Qi Y. Impacts of the Affordable Care Act dependent coverage provision on health-related outcomes of young adults. Cambridge (MA): National Bureau of Economic Research; 2014. May, (NBER Working Paper No. 20148). [DOI] [PubMed] [Google Scholar]
- 15.Sommers BD, Buchmueller T, Decker SL, et al. The Affordable Care Act has led to significant gains in health insurance and access to care for young adults. Health Affairs. 2013;32(1):165–74. doi: 10.1377/hlthaff.2012.0552. [DOI] [PubMed] [Google Scholar]
- 16.Sommers BD. Number of young adults gaining insurance due to the Affordable Care Act now tops 3 million. Department of Health and Human Services. ASPE Issue Brief. 2012 Jun 19; [Google Scholar]
- 17.Antwi YA, Moriya AS, Simon K. Access to health insurance and the use of inpatient medical care: evidence from the Affordable Care Act young adult mandate. doi: 10.1016/j.jhealeco.2014.11.007. Available at: Available at: business.illinois.edu/nmiller/mhec/Antwi.pdf. Accessed: February 24, 2015. [DOI] [PubMed]
- 18.Mulcahy A, Harris K, Finegold K, et al. Insurance coverage of emergency care for young adults under health reform. N Engl J Med. 2013;368(22):2105–12. doi: 10.1056/NEJMsa1212779. [DOI] [PubMed] [Google Scholar]
- 19.Antwi YA, Moriya AS, Simon K. National Bureau of Economic Research. 2012. Jun, Effects of federal policy to insure young adults: evidence from the 2010 Affordable Care Act dependent coverage mandate. (NBER Working Paper No. 18200). [Google Scholar]
- 20.Scott JW, Sommers BD, Tsai TC, et al. Dependent coverage provision led to uneven insurance gains and unchanged mortality rates in young adult trauma patients. Health Affairs. 2015;34(1):125–133. doi: 10.1377/hlthaff.2014.0880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Selassie AW, Pickelsimer EE, Frazier L, Jr, Ferguson PL. The effect of insurance status, race, and gender on ED disposition of persons with traumatic brain injury. Am J Emerg Med. 2004;22(6):465–73. doi: 10.1016/j.ajem.2004.07.024. [DOI] [PubMed] [Google Scholar]
- 22.Shafi S, la Plata de CM, Diaz-Arrastia R, et al. Ethnic disparities exist in trauma care. J Trauma Injury Infection Crit Care. 2007;63(5):1138–42. doi: 10.1097/TA.0b013e3181568cd4. [DOI] [PubMed] [Google Scholar]
- 23.Downing SR, Oyetunji TA, Greene WR, et al. The impact of insurance status on actuarial survival in hospitalized trauma patients: when do they die? J Trauma. 2011;70(1):130–4. doi: 10.1097/TA.0b013e3182032b34. discussion 134–5. [DOI] [PubMed] [Google Scholar]
- 24.Cantor JC, Monheit AC, Delia D, Lloyd K. Early impact of the Affordable Care Act on health insurance coverage of young adults. Health Serv Res. 2012;47(5):1773–90. doi: 10.1111/j.1475-6773.2012.01458.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vettukattil AS, Haider AH, Haut ER, et al. Do trauma safety-net hospitals deliver truly safe trauma care? A multilevel analysis of the National Trauma Data Bank. J Trauma Injury Infection Crit Care. 2011;70(4):978–84. doi: 10.1097/TA.0b013e31820b5d0c. [DOI] [PubMed] [Google Scholar]
- 26.O’Hara B, Brault MW. The disparate impact of the ACA-Dependent expansion across population subgroups. Health Serv Res. 2013;48(5):1581–92. doi: 10.1111/1475-6773.12067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lillie-Blanton M, Hoffman C. The role of health insurance coverage in reducing racial/ethnic disparities in health care. Health Aff. 2005;24(2):398–408. doi: 10.1377/hlthaff.24.2.398. [DOI] [PubMed] [Google Scholar]
- 28.Sommers BD, Graves JA, Swartz K, Rosenbaum S. Medicaid and marketplace eligibility changes will occur often in all states; policy options can ease impact. Health Affairs. 2014;33(4):700–7. doi: 10.1377/hlthaff.2013.1023. [DOI] [PubMed] [Google Scholar]
- 29.Status of State Action on the Medicaid Expansion Decision. Kaiser Family Foundation; Available at: http://kff.org/health-reform/state-indicator/state-activity-around-expanding-medicaid-under-the-affordable-care-act/. Accessed February 24, 2015. [Google Scholar]
- 30.National Trauma Data Bank, Annual Report. 2013 Available at: http://www.facs.org/trauma/ntdb/pdf/ntdb-annual-report-2013.pdf. Accessed February 24, 2015.
- 31.Bolorunduro OB, Haider AH, Oyetunji TA, et al. Disparities in trauma care: are fewer diagnostic tests conducted for uninsured patients with pelvic fracture? AJS. 2013;205(4):365–70. doi: 10.1016/j.amjsurg.2012.10.026. [DOI] [PubMed] [Google Scholar]
- 32.Englum BR, Villegas C, Bolorunduro O, et al. Racial, Ethnic, and Insurance Status Disparities in Use of Posthospitalization Care after Trauma. J Am Coll Surg. 2011;213(6):699–708. doi: 10.1016/j.jamcollsurg.2011.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


