Abstract
BACKGROUND:
There is a lack of evidence on description of burden and cases of childhood poisoning in developing countries. This study aimed to assess the characteristics of children with acute poisoning, and factors for time of presentation to health facility and nature of poisoning.
METHODS:
A cross-sectional study was conducted at three major pediatric referral hospitals in Addis Ababa, Ethiopia. Description of demographics of children with acute poisoning and factors associated with time to presentation and nature of poisoning were analyzed. Data were entered to Epi info 3.5.3 and analyzed with SPSS version 20.
RESULTS:
Over three years, we retrieved records of a total of 128 children admitted for acute poisoning. The mean age of victims was 5.46 (SD, standard deviation=4.48) years. The majority (29.7%) were poisoned by prescribed drugs. Most poisoning incidents (73.5%) were unintentional in nature. The median time to health facility visit was 15.5 hours. Age less than 2 years was related to earlier presentation to health facility (P=0.010, OR=0.28, 95%CI=0.10–0.74). Children with age more than 5 years was more likely to have intentional poisoning (χ2=25.06, P<0.0001). None of the victims was provided psychosocial evaluation and counseling.
CONCLUSION:
Most poisoning incidents are unintentional. Prescribed drugs are the commonest causes. Psychosocial counseling and care for the affected children is lacking. Family and community education should be given on prevention of poisoning. We recommend that caregivers take the required action in keeping prescribed drugs at home. Psychosocial support should be part of care and treatment of children with poisoning.
KEY WORDS: Poisoning, Children, Ethiopia
INTRODUCTION
Poisoning remains a major public health problem, particularly in children. Worldwide, every year, nearly one million children died from injuries.[1] For these deaths, poisoning is the fourth leading cause following road traffic accident, burns and drowning.[2] Children below the age of five years constitute about 15% of unintentional poisoning related deaths.[3] In fact, the true incidence of poisoning and the danger it causes is often times underreported.[4,5] Poisonings occur when substances are ingested, inhaled, injected or absorbed through the skin in quantities that are harmful to the body.[6]
Effective preventive and therapeutic approaches in childhood poisoning should be based on appropriate knowledge of general epidemiologic data to assist emergency department personnel on the proper management of poisoning cases.[7,8] In most settings of developing countries, childhood acute poisoning is poorly described. Short of knowledge of the scope of the problem and the importance of organizing a poisoning prevention and information center has been under emphasized in the Ethiopian context. This study aimed to assess the characteristics, clinical management and outcome of children with acute intoxication due to drugs and chemicals seeking medical care at the Pediatric Emergency Departments of Tikur Anbessa, Zewditu Memorial and Yakatit 12 hospitals.
METHODS
Setting
This study was conducted in the Pediatric Emergency Departments (PEDs) of Tikur Anbessa, Yekatit 12, and Zewditu Memorial hospitals. These three hospitals are the major hospitals with strong pediatric services and with established PEDs.
Included were children below the age of 14 years who were admitted to the hospitlas for poisoning over the past three years (2010–2013). Children beyond 14 years of age and with incomplete medical records were excluded.
Data collection procedures
A structured data retrieval form was prepared by the investigators; it was pretested on 5% of the total cases of poisoning. Required corrections and clarification were made based on the pretest. Interns were trained on the process of data collection and the contents of the data retrieval form. The collected information included gender, age, category of substance involved in poisoning, clinical presentation, place of poison exposure, route of exposure, history of poisoning, nature of poison exposure (accidental or intentional), treatment, outcome, period from poison exposure to arrival at hospital, and duration of observation or hospitalization. The nature of poison exposure was classified as intentional or accidental.
Statistical analysis
Data were put in Epi info 3.5.3 and analyzed with SPSS 20 for windows. Descriptive statistics was employed to produce tabulated percentages, mean, median and range of variables. Binary logistic regression was used to test the association between the time to presentation to health facilities and age, gender, associated morbidity and the location of poisoning. The Chi-square test and Fisher’s exact test were performed to test the association among categorical variables. A P value less than 0.05 was considered statistically significant.
RESULTS
Over three years (between September 2010 and September 2013), we retrieved records of a total of 128 children from three major hospitals in Addis Ababa. The mean age of the victims was 65.5 months (SD=53.7 months; 95%CI=56.4–75.4. Females had 66 (51.6%) of the total incidents. Of the children, 68 (53.1%) were admitted to Yekatit 12 Hospital; 43 (33.6%) and 15 (11.7%) were admitted to Zewditu Memorial Hospital and Tikur Anbessa Hospital respectively. About 95 (74.2%) poisoning accidents happened at home; 8 (6.3%) and 25 (19.5%) occurred outside of home and were unrecorded respectively (Table 1).
Table 1.
Characteristics of children with poisoning who were admitted to three tertiary care hospitals in Addis Ababa, Ethiopia, February 2015
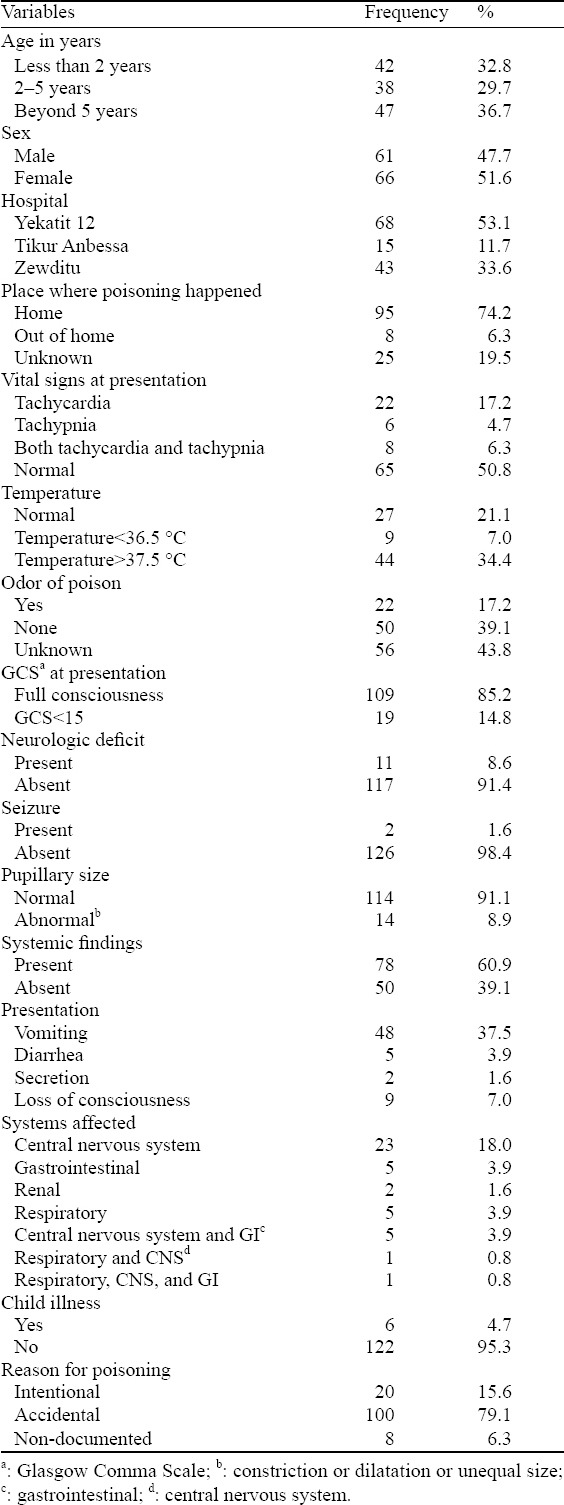
Sixty-five (50.8%) of the children had normal respiration and heart beat. Whereas, 22 (17.2%), 8 (6.3%), and 6 (4.7%) had tachycardia only, tachypnia only and both tachycardia and tachypnia, respectively. Fourty-four (34.4%) of the children had hypothermia at presentation; 27 (21.2%) and 9 (7.0%) had normal body temperature and fever, respectively. Odor of the poison was appreciated by professionals and/or caregivers for 22 (17.2%) of the children.
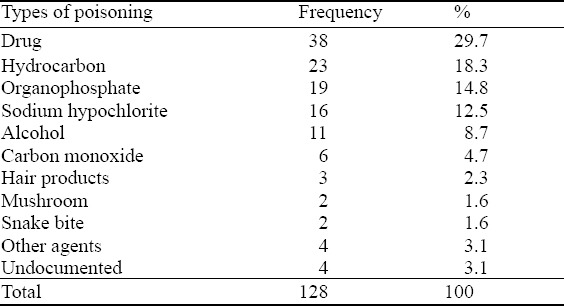
Thirty-eight (29.7%) of the children were poisoned by prescribed drugs for themselves and other family members (Table 2). Seven family members were on medication while the children were poisoned. Five children had a family history of poisoning and all of them had drug as cause of poisoning.
Table 2.
Type of poison of 128 acutely poisoned children from September 2010 to September 2013, February 2015
Atropine was given as an antidote for 8 (6.3%) children with organophosphate poisoning and oxygen was given for all children with carbon monoxide poisoning. Diphenhydramine was used in carbamezipine poisoning. Gastric lavage using a nasogastric tube was done for 23 (18%) children. In children who suffered from detergent poisoning, 8 (53.3%) received antacids. Serum levels were not checked for any of the poisoning types.
The median time to hospital visit from the time of poisoning was 15.5 hours; it ranged from one hour to one month. Home remedies were given to 24 (18.7%) of the children. Twenty-two (83.3%) children were given milk, and at last 2 (1.6%) of them induced vomiting: one had a vomiting with milk, and the other had a vomiting with milk and water at home. Six children required intensive care unit treatment. All the included children survived after treatment. The mean duration of hospitalization for the children was 17.7 days (SD=21.9).
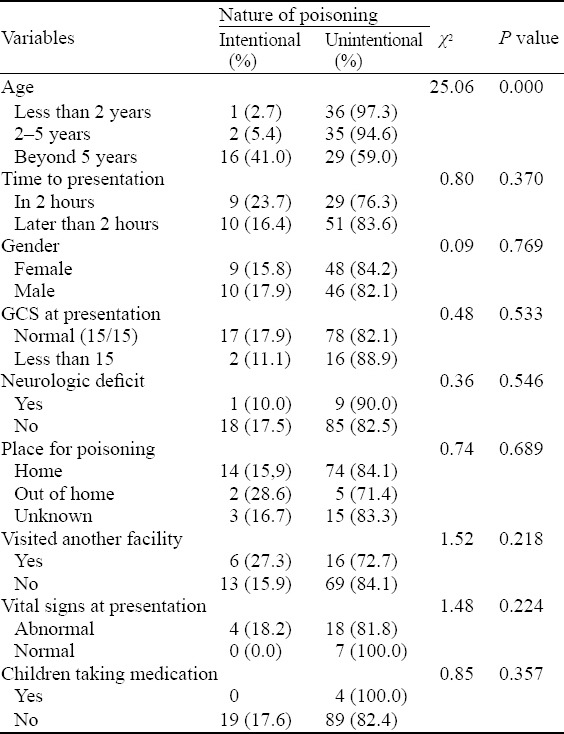
Unintentional poisoning occurred in 100 (77.5%) of the children, whereas intentional poisoning was seen in 20 (15.5%). The common causes of intentional poisoning were as follows: drugs (n=6), organophosphate (n=3) and sodium hypochlorite (n=2); undocumented (n=8). Children aged more than 5 years were more likely to have intentional poisoning (χ2=25.06, P<0.0001) (Table 3). There was no history of poisoning in all the children.
Table 3.
Association of variables with nature of poisoning among acutely poisoned children, February 2015
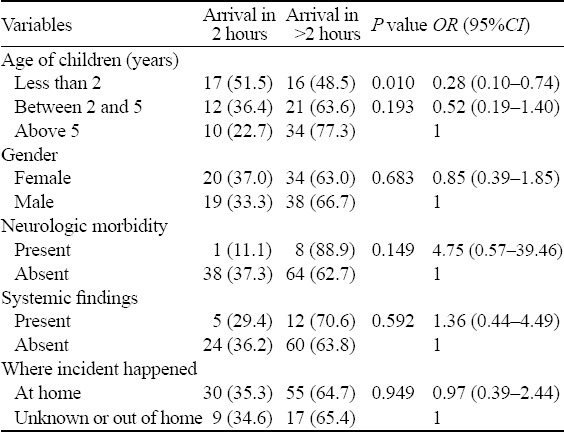
Further analysis of the factors for delayed presentation found that young age was related to an earlier presentation as compared to children older than 2 years (P=0.010, OR=0.28, 95%CI=0.10–0.74) (Table 4).
Table 4.
Predictors of delay in presentation to health facilities from time of poisoning, February 2015
Regarding the provision of post exposure counseling for childdren with poisoning, we found no records suggesting that none of them was provided with such services. Nor the children had psychosocial evaluation by a child psychiatrist and a follow-up after the incident.
DISCUSSION
The results of the current study showed that childhood poisoning is not an uncommon problem in this setting. Most children were poisoned with prescribed drugs for themselves or family and most poisoning incidents were unintentional. The majority of the children were poisoned at home. Young age was associated with earlier presentation to healthcare settings after the incident of poisoning. In the present study, the small number of retrieved patient records was possibly due to poor health seeking behaviors and referral systems that led to a small number of patients managed at large hospitals and/or poor record keeping at the hospitals.
In the current study, most of the children were female unlike the studies in Nigeria and Taiwan province, where more males than females were reported.[9,10] This difference might be explained by the differences in study design and socio-cultural values. The finding of more poisoning episodes in children under five years old was similarly reported in Nigeria and Taiwan province, China.[9,10] Other epidemiological studies of pediatric poisoning have demonstrated that the most common risk factors for poison exposure are young age and female gender, which are in agreement with our findings.[11–17]
Poisoning incidents can be categorized into intentional or unintentional types based on how they happened, but most of childhood poisonings are accidental in nature. In the current study, most episodes were unintentional similar to those reported by Paudyal et al[18] (unintentional poisoning 98.4%) and by authors from Taiwan province (77.7%).[10] Identifying children with intentional poisoning is crucial as this could be an indication of a serious psychosocial behavior or possibility of child abuse. Prescription drugs are the commonest causes of poisoning in our study unlike kerosene being the most common agent in other studies.[11,18]
In the current study, the mean duration of hospital stay is greater than that reported from central Nepal.[18] This difference could be explained by the differences in the timely arrival to health facilities after the poisoning incident and the severity of the cases.
Similar to the findings of the current study, other researchers have reported that proper education on the prevention of future poison exposure was lacking for patients who visit emergency departments.[19] We did not find records indicating that the children received any post exposure counseling and that there was no follow-up description. Though there is limited evidence suggesting that nasogastric lavage is an effective treatment for patients with poisoning, a significant number of patients who received such treatment should be evaluated.
The main limitation of the current study is its retrospective design and hence it has incomplete data. While this study is crucial in indicating the gaps for improvement and information on poisoning in Ethiopia, it is difficult to know the real prevalence of poisoning and the associated factors.
In conclusion, poisoning is not an uncommon health problem and it is usually unintentional. Prescribed drugs are the commonest cause of poisoning. Young age is associated with an earlier presentation to a health setting. Psychosocial counseling and care is lacking in the treatment of children with poisoning.
We recommend that caregivers should be responsible for keeping prescribed drugs at home. Community education on prevention of poisoning and early referral and care is necessary. Psychosocial support should be part of the treatment of such children. We also suggest that prospective studies be conducted to identify the prevalence and associated factors.
ACKNOWLEDGMENT
The authors would like to appreciate the support from the Ethiopian Pediatric Society and also to thank Dr Sabrina Butters for his comments on the study proposal.
Footnotes
Funding: None.
Ethical approval: The study was approved by the Ethics Committee of the University.
Conflicts of interest: Thhere are no competing interest and personal relationships with other people or organizations that could influence the study.
Contributors: Tilahun B proposed the study and wrote the first draft. All authors read and approved the final manuscript.
REFERENCES
- 1.Bronstein AC, Spyker DA, Cantilena LR, Jr, Green JL, Rumack BH, Heard SE, et al. 2007 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS):25th Annual Report. Clin Toxicol (Phila) 2008;46:927–1057. doi: 10.1080/15563650802559632. [DOI] [PubMed] [Google Scholar]
- 2.Hyder AA, Wali S, Fishman S, Schenk E. The burden of unintentional injuries among the under-five population in South Asia. Acta Paediatrica. 2008;97:267–275. doi: 10.1111/j.1651-2227.2008.00670.x. [DOI] [PubMed] [Google Scholar]
- 3.Peden MK, Sharma G. The Injury Chart Book: A graphical overview of the global burden of injuries. Geneva: World Health Organization; 2002. [Google Scholar]
- 4.Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJL. Measuring the Global Burden of Disease and Risk Factors 1990–2001. In: Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJL, editors. Global Burden of Disease and Risk Factors. Chapter 1. Washington (DC): World Bank; 2006. [Google Scholar]
- 5.Eddleston M. Patterns and problems of deliberate self poisoning in the developing world. QJM. 2000;93:715–731. doi: 10.1093/qjmed/93.11.715. [DOI] [PubMed] [Google Scholar]
- 6.Murray CJ, Lopez AD, editors. The global burden of disease: A comprehensive assessment of mortality and disability from diseases, injuries, and risk factors in 1990 and projected to 2020. Harvard School of Public Health (on behalf of the World Health Organization and The World Bank) 1996:120–122. [Google Scholar]
- 7.Desalew M, Aklilu A, Amanuel A, Addisu M, Ethiopia T. Pattern of acute adult poisoning at Tikur Anbessa specialized teaching hospital, A retrospective study, Ethiopia. Hum Exp Toxicol. 2011;30:523–527. doi: 10.1177/0960327110377520. [DOI] [PubMed] [Google Scholar]
- 8.Abula T, Wondmikun Y. The pattern of acute poisoning in a teaching hospital, north-west Ethiopia. Ethiop Med J. 2006;44:183–189. [PubMed] [Google Scholar]
- 9.Lin YR, Liu TH, Liu TA, Chang YJ, Chou CC, Wu HP. Pharmaceutical poisoning exposure and outcome analysis in children admitted to the pediatric emergency department. Pediatr Neonatol. 2011;52:11–17. doi: 10.1016/j.pedneo.2010.12.003. [DOI] [PubMed] [Google Scholar]
- 10.Yang CC, Wu JF, Ong HC, Kuo YP, Deng JF, Ger J. Children poisoning in Taiwan. Indian J Pediatr. 1997;64:469–483. doi: 10.1007/BF02737751. [DOI] [PubMed] [Google Scholar]
- 11.Lamireau T, Lanas B, Kennedy A, Fayon M, Penouil F, Favarell-Garrigues JC, et al. Epidemiology of poisoning in children: a 7-year survey in a paediatric emergency care unit. Eur J Emerg Med. 2002;9:9–14. doi: 10.1097/00063110-200203000-00004. [DOI] [PubMed] [Google Scholar]
- 12.Andiran N, Sarikayalar F. Pattern of acute poisonings in childhood in Ankara: what has changed in twenty years?Turk J Pediatr. 2004;46:147–152. [PubMed] [Google Scholar]
- 13.Demorest RA, Posner JC, Osterhoudt KC, Henretig FM. Poisoning prevention education during emergency department visits for childhood poisoning. Pediatr Emerg Care. 2004;20:281–284. doi: 10.1097/01.pec.0000125654.20443.33. [DOI] [PubMed] [Google Scholar]
- 14.Hincal F, Hincal AA, Müftü Y, Sarikayalar F, Ozer Y, Cevik N, et al. Epidemiological aspects of childhood poisonings in Ankara: a 10-year survey. Hum Toxicol. 1987;6:147–152. doi: 10.1177/096032718700600207. [DOI] [PubMed] [Google Scholar]
- 15.Mintegi S, Fernández A, Alustiza J, Canduela V, Mongil I, Caubet I, et al. Emergency visits for childhood poisoning: a 2-year prospective multicenter survey in Spain. Pediatr Emerg Care. 2006;22:334–338. doi: 10.1097/01.pec.0000215651.50008.1b. [DOI] [PubMed] [Google Scholar]
- 16.Oguche S, Bukbuk DN, Watila IM. Pattern of hospital admissions of children with poisoning in the Sudano-Sahelian North eastern Nigeria. Niger J Clin Pract. 2007;10:111–115. [PubMed] [Google Scholar]
- 17.Riordan M, Rylance G, Berry K. Poisoning in children: painkillers. Arch Dis Child. 2002;87:397–399. doi: 10.1136/adc.87.5.397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Paudyal BP. Poisoning: pattern and profile of admitted cases in a hospital in central Nepal. J Nepal Med Assoc. 2005;44:92–96. [PubMed] [Google Scholar]
- 19.Demorest RA, Posner JC, Osterhoudt KC, Henretig FM. Poisoning prevention education during emergency department visits for childhood poisoning. Pediatr Emerg Care. 2004;20:281–284. doi: 10.1097/01.pec.0000125654.20443.33. [DOI] [PubMed] [Google Scholar]


