Abstract
BACKGROUND:
Survival from cardiac arrest is sensitive to the quality of delivered CPR. In 2010, updated international resuscitation guidelines emphasized deeper chest compressions and faster rates, yet it is unknown whether training laypersons using updated guidelines resulted in changed CPR performance. We hypothesized that laypersons taught CPR using the 2010 guidelines performed deeper and faster compressions than those taught using the 2005 materials.
METHODS:
This work represents a secondary analysis of a study conducted at eight hospitals where family members of hospitalized cardiac patients were trained in CPR. An initial cohort was trained using the 2005 guidelines, and a subsequent cohort was trained using the 2010 guideline materials. Post training, CPR skills were quantified using a recording manikin.
RESULTS:
Between May 2009 to August 2013, 338 subjects completed the assessment. Among the subjects, 176 received 2005 training and 162 underwent 2010 training. The mean compression rate in the 2005 cohort was 87 (95%CI 83–90) per minute, and in the 2010 cohort was 86 (95%CI 83–90) per minute (P=ns), while the mean compression depth was 34 (95%CI 32–35) mm in the 2005 cohort and 46 (95%CI 44–47) mm in the 2010 cohort (P<0.01).
CONCLUSIONS:
Training with the 2010 CPR guidelines resulted in a statistically significant increase in trainees’ compression depth but there was no change in compression rate. Nevertheless, the majority of CPR performed by trainees in both cohorts was below the guideline recommendation, highlighting an important gap between training goals and trainee performance.
KEY WORDS: Cardiopulmonary resuscitation, Cardiac arrest, Sudden death, Education, Guidelines
INTRODUCTION
Performance of high quality cardiopulmonary resuscitation (CPR) by members of the lay public before arrival of emergency medical services is a key factor in improving cardiac arrest survival. A number of observational clinical studies have demonstrated a positive correlation between CPR quality and survival from cardiac arrest.[1–5] Additionally, a recent meta-analysis of CPR performance investigations demonstrated that deeper chest compressions and rates closer to 85 to 100 compressions per minute were associated with improved survival from cardiac arrest.[6]
Taking into account the body of evidence supporting the importance of high quality CPR, the International Liaison Committee on Resuscitation (ILCOR) updated CPR guidelines recommendations in 2010. These updated guidelines recommended deeper chest compressions (>50 mm) and a faster compression rate (>100 per min).[7] Observational studies subsequent to these changes have demonstrated that incorporation of the updated guidelines is associated with improved cardiac arrest outcomes,[8,9] while other investigations have suggested that implementation of new CPR guidelines do not result in improved outcomes.[2,10,11] In addition to these conflicting findings among professional providers, little evidence exists to address whether lay bystanders trained in CPR following the 2010 CPR guidelines actually perform deeper or faster compressions.
As a secondary analysis of a prospective multicenter trial of CPR educational strategies, using an existing hospital-based family member CPR training program, conducted in collaboration with nursing personnel, we assessed the skills of subjects who learned CPR under the two most recent guidelines.[12,13] We hypothesized that subjects taught CPR using the 2010 ILCOR guidelines would perform deeper and faster chest compressions than those taught with the 2005 guidelines.
METHODS
Study population and setting
Our multicenter cohort study was approved by the Institutional Review Boards with jurisdiction over the study sites (University of Pennsylvania, Crozer-Keystone Health System, Albert Einstein Healthcare Network, Temple University, and the Chester County Hospital and Health System). Enrollment was conducted using a standard written informed consent process at eight hospitals affiliated to these health systems. Adult family members or friends of hospitalized patients on cardiology service lines, telemetry wards, step down units, and observation units were eligible for participation, with active enrollment conducted between May 2009 and August 2013.
CPR instruction was offered by nurses and pre-medical students to family members of hospitalized patients at each study site. Subjects were considered potential candidates for enrollment if they met the following criteria: 1) the family member or friend to be enrolled was physically present with the patient on the floor or unit; 2) the patient had an admission diagnosis related to coronary disease or significant cardiovascular risk factors; 3) the patient was in a stable condition; 4) the family member was over 18 years of age; and 5) the family member felt fit and able to perform moderate physical activity at the time of enrollment. Interested subjects who satisfied the inclusion criteria were enrolled using a standard written consent form, and completed a pre-training demographics survey.
Each subject viewed the VSI training and received either the 2005 or 2010 CPR guidelines training kit materials, depending on the time of enrollment in the study. Upon completion of the training, the subjects completed a post-training survey assessing their self-efficacy using their newly acquired CPR skills and perspectives on the training experience. Data from these surveys have been reported elsewhere.[13]
CPR training approach
We used a commercially available CPR video self-instruction (VSI) program (Family and Friends CPR Anytime, American Heart Association, Dallas, TX and Laerdal Medical Corporation, Stavanger, Norway), which has been validated in previous investigations.[14–16] This educational tool is packaged in a self-contained kit that includes an inflatable head/torso manikin and instructional DVD. The 2005 guidelines version of the DVD teaches compression depth performance at 38–50 mm and a rate of 100 compressions per minute. The inflatable head/torso manikin was engineered to give audio feedback (chest wall “click”) when an individual compressed at least 38 mm. The updated 2010 version of the instructional DVD teaches CPR performance with a depth of >50 mm at a rate of >100 compressions per minute. In this iteration, the manikin was engineered to click at 50 mm of compression depth. For simplicity of study design and analysis, all subjects were instructed in compression-only CPR (without ventilations). Manikins with the audio feedback were only used for the training phase and not subsequent testing.
Study design
This study was structured as a retrospective analysis evaluating the impact of guideline changes on CPR training and skill retention using data collected from two multi-center prospective hospital-based CPR training dissemination trials. Subjects enrolled from May 2009 to May 2010 were taught CPR using the 2005 guidelines training materials, whereas those enrolled from February 2012 to August 2013 were trained using the 2010 guidelines curriculum.
Post-training CPR quality evaluation
The post-training CPR quality evaluation protocols varied between cohorts due to a change in the study design outcome measure. Specifically, the second protocol was part of a large implementation project where immediate testing was not feasible. Since our hypothesis was that the change in guidelines improved CPR quality, immediate testing following training should yield better CPR quality than testing at six months as seen in the literature.[14] Subjects taught with the 2005 guidelines were asked by investigative staff to complete a two-minute skills assessment immediately following the in-hospital training and completion of the post-survey questionnaire. Subjects taught with the 2010 guidelines were contacted at six months post-initial enrollment and asked to complete a brief in-person interview. Once they completed the interview, the subject was asked to perform a two-minute skills test. Subjects who completed the skills assessment six months post-initial training were given $50 compensation for travel and their time.
Data from the CPR skills test in both groups were captured on a CPR recording manikin (Skillreporter ResusciAnne, Laerdal Medical) without direct audiovisual feedback to subjects or any interaction from study staff. CPR performance data were extracted from the recording software and imported into the study database for subsequent quantitative analysis.
Statistical approach and analysis
All data were compiled in a secure, internet-based database application (REDCap Software Version 5.5.21, Vanderbilt University, Nashville, TN) and analyzed using a statistical software package (STATA 13, Statacorp, College Station, TX). Nine subjects were excluded from the 2010 cohort and seven subjects were removed from the 2005 cohort due to missing covariates. Demographic data were examined using the chi-square test for categorical variables, whereas Student’s t test was applied to continuous variables. Resuscitation performance data (compression rate and depth) were assessed for approximate normality and Student’s t test was used due to the large sample size. We used ordered logistic regression and multiple linear regression to further assess resuscitation performance while controlling potentially confounding covariates. Additionally, we adjusted center-level confounding by adding site in the regression as a fixed-effect. We further analyzed resuscitation performance by classifying these data into three categories based on the ILCOR guidelines. We defined “excellent” rate as greater than 100 per minute, “good” rate between 80 to100 per minute, and “poor” rate as less than 80 per minute. Additionally, we defined “excellent” depth as above 50 mm, whereas “good” between 38 to 49 mm, and “poor” as less than 37 mm.
RESULTS
Demographics
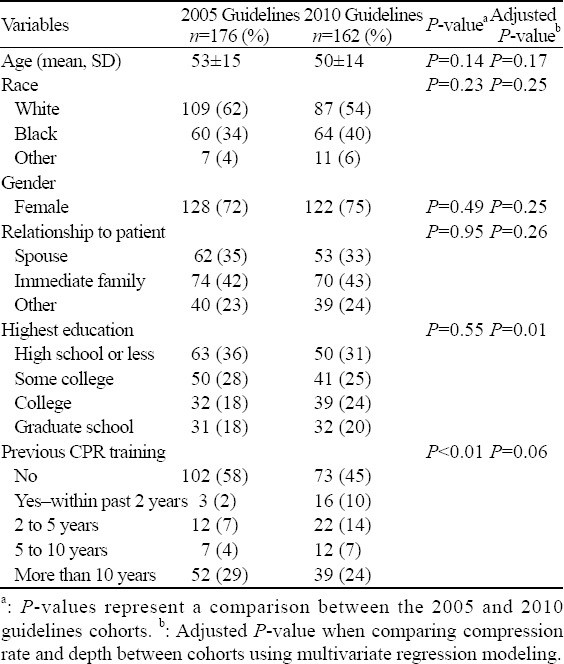
From May 2009 to August 2013, 402 subjects were trained in CPR at the eight study hospitals. Among the subjects, 176 received training with the 2005 guidelines and 226 underwent training with the 2010 guidelines. From this target group, 176/176 (100%) of the 2005 cohort and 162/226 (72%) from the 2010 cohort completed the skills assessment. Descriptive characteristics and demographics of the study population who completed the skills assessment are detailed in Table 1. Overall, the mean age of subjects was 52±15 years, and 250/338 (74%) of the subjects were female. The majority of subjects were white 196/338 (58%) or black 124/338 (37%), and 259/338 (77%) reported being the patient’s spouse or immediate family member. Of the subjects, 175/338 (52%) had never received CPR training, and an additional 91/338 (27%) had not been trained in more than 10 years. While there were statistically significant differences in terms of previous CPR training, there were no variations between study cohorts in regard to age, gender, race, subject’s relationship to the patient, and highest level of education attained.
Table 1.
Demographics
CPR skills assessment
After training, subjects were asked to complete a two-minute skills assessment on a CPR recording manikin. Three hundred and thirty-eight subjects completed this assessment and the results of the skills assessment are detailed in Table 2. The mean chest compression rate in the 2005 cohort was 87 (95%CI 83– 90) per minute and in the 2010 group was 86 (95%CI 83–90) per minute (P=ns), whereas the mean chest compression depth in the 2005 cohort was 34 (95%CI 32–35) mm and in the 2010 cohort was 46 (95%CI 44– 47) mm (P<0.01). These data are shown in Figure 1.
Table 2.
CPR skills assessment after training
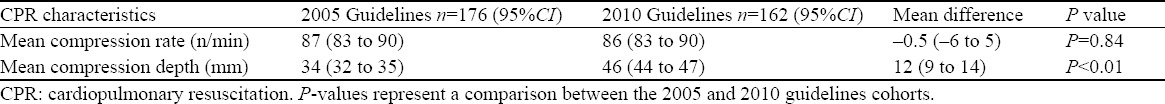
Figure 1.
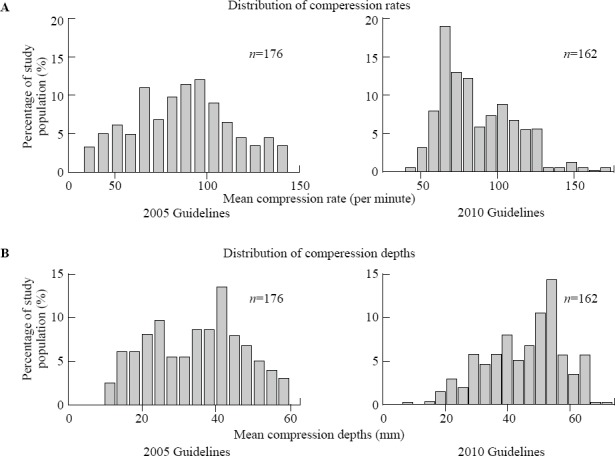
Distribution of subject chest compression rate (A) and depth (B) within both the 2005 and 2010 guidelines training cohorts. Skills data were quantified on a CPR-recording manikin.
We further analyzed these data categorically to examine the prevalence of poor, good, and excellent rate and depth within study cohorts (see Statistical Approach for detailed description). Adequacy of rate performance did not vary significantly between the cohorts (P=0.14), but adequacy of depth performance was found to be significantly different (P<0.01) (Figure 2). Of the 2005 cohort, 104/176 (59%) had “poor” depth compared with 42/162 (25%) of the 2010 cohort (P<0.01), and 59/176 (34%) of the 2005 cohort had “good” depth compared with 56/162 (35%) of the 2010 cohort (P>0.05). Additionally, 13/176 (7%) of the 2005 cohort had “excellent” depth compared with 64/162 (40%) of the 2010 cohort (P<0.01).
Figure 2.
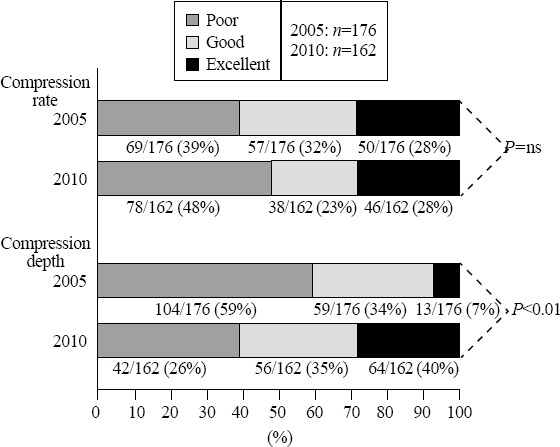
Proportion of subjects with poor, good, and excellent chest compression rate and depth within both the 2005 and 2010 guidelines training cohorts. P-value represents statistical significance between the 2005 and 2010 guidelines cohorts.
Adjustment for confounding
We used a multiple linear regression model to adjust for age, gender, education, prior training, and relationship to patient as potential confounders on the effect of guidelines training (2005 vs. 2010) on CPR performance. The adjusted P values from this multiple regression are detailed in Table 1. When controlling confounders, training with the 2005 or 2010 guidelines was not significantly associated with a change in rate. Increasing educational attainment was associated with deeper compression depth; even after adjustment for this potential confounder, subjects trained with the 2010 guidelines had mean levels of compression depth that were 12.46 mm (95%CI 15.3–9.58) deeper than those subjects trained with the 2005 guidelines (P<0.01).
Additionally, we used ordered logistic regression to analyze the categorically grouped compression data’s relationship with guidelines training while adjusting for education and prior training. When controlling for potential confounding, guidelines training was not found to be significantly related to compression rate. Compared to the 2010 guidelines, subjects trained with the 2005 guidelines have an 85% decreased likelihood of being in a higher depth category, while controlling for education and prior CPR training (P<0.01).
DISCUSSION
In the current work, we found that implementation of the 2010 CPR guidelines training materials resulted in a statistically significant increase in lay bystander’s performance of chest compression depth, while controlling other variables. However, despite this increase, mean depth was still less than the 50 mm threshold recommended by international resuscitation guidelines, highlighting the difficulty of achieving this quality goal.
The impact of CPR guidelines on training
Several studies have compared 2005 to 2010 guidelines training of healthcare providers and the subsequent impact on CPR quality during arrest simulations. Mayer et al[17] trained nurses and physicians using both guidelines recommendations and demonstrated improved CPR performance with the 2010 guidelines. Additionally, Jones et al[18] studied the impact of the 2010 guidelines on medical student CPR performance and found that subjects exhibited a faster rate when trained under the 2010 guidelines. In both studies, the subjects were taught using the standard CPR approach (i.e. 30 compressions: 2 ventilations).
There are limited data on the training of lay providers and the effect of guideline changes on educational effectiveness. A recent Chinese study randomized 88 undergraduate student volunteers to the 2005 or 2010 guidelines training using compressions-only CPR and found that the quality of CPR (both rate and depth) improved among the 2010 cohort.[19] Our study utilized an existing hospital-based layperson CPR training infrastructure, in which the subject cohort was older (mean age=52±15) and participants were tested six months after initial training. We found that the difference in chest compression rate was not statistically significant (P=0.84), which may be due to the guideline instructions for chest compression rate remaining similar from 2005 to 2010. Additionally, we demonstrated improved performance of chest compression depth within the 2010 cohort six months after initial training.
Despite guidelines, lay bystander CPR varies
While our data suggest an improvement in chest compression depth with the new guidelines implementation, it is important to note that there was wide variation in the quality of CPR performance among our trained lay subjects. This finding is consistent with the larger body of work that has highlighted the difficulty of achieving high-quality layperson CPR during both simulated and presumably actual resuscitation events as well.
Rea et al[20] examined the CPR quality of 26 cases of cardiac arrest patients treated by trained layperson provider CPR as a sub-analysis from the public access defibrillation trial. In this retrospective cohort study, CPR quality varied and often did not reach guideline recommended quality targets. Similarly, in a simulation study assessing trained laypersons, Aufderheide et al[21] demonstrated that less than a third of subjects performed adequate compression depth. Our study found similar, poor CPR performance with less than a third of the subjects demonstrating excellent rate and depth.
Methods to improve layperson CPR
Since there is growing evidence that training alone may not be sufficient to ensure adequate layperson CPR performance, there may be potential value in considering other innovative approaches.[20,21] Recent investigations have suggested that dispatcher-assisted CPR instructions may provide a useful complement to CPR training for laypersons.[22] A recent study[23] found that dispatcher-assisted instructions with compressions-only CPR resulted in a trend towards better outcomes in clinical subgroups. Other investigations have explored the use of cell phone audio guidance for lay bystanders and found that audio guidance improved CPR quality in simulated settings.[24] Despite this, there may be situations where dispatcher assisted CPR or cell phone guidance are not readily available, thus other novel methods to increase CPR retention should be examined. Investigators may consider evaluating processes to encourage trainees to practice their skills more regularly such as through brief email reminders, SMS texts, or phone calls that prompt subjects to consider refreshing their skills. Additionally, it is reasonable to consider whether more testing or feedback is necessary during the training process to increase the rate of competent providers. These novel methods may be an attractive avenue for future investigations.
Limitations
This study has several limitations. First, subjects were selected as part of a larger ongoing multicenter study investigating various hospital-based CPR training dissemination strategies. Subjects were enrolled using a similar inclusion criteria and CPR training curriculum, but there were variations in the CPR skills test protocol. Specifically, those in the 2005 cohort were subjected to a CPR skills test immediately after the training, whereas subjects in the 2010 cohort were given a six-month post-initial training for skill assessment. Despite the lag in follow-up assessment among those trained using 2010 guidelines, compression depth was significantly deeper in this group, supporting the finding that the change was related to the guidelines training curriculum. Furthermore, the six-month skills test was integrated into an in-person follow-up interview where subjects were not notified beforehand that they were being asked to complete a skills check (i.e., the skills check was a “surprise”). This method made it more probable that the subject did not practice immediately before the follow-up assessment, thus supporting the likelihood that the improvement in chest compression depth was related to the guidelines training curriculum. Despite this, it is worth noting that the potential bias introduced by different follow-up periods may actually mask the true difference between cohorts. Future studies may consider re-examining the relationship between CPR performance and guidelines change with similar follow-up periods.
In conclusion, we have shown that implementation of the 2010 CPR guidelines for layperson training resulted in a statistically significant increase in the performance of chest compression depth six months after initial training, compared with the training using the 2005 guidelines materials. Despite the improvement, mean chest compression depth was still below the 50 mm threshold recommended by ILCOR guidelines. These findings have important implications for future development of CPR training materials. Additionally, these findings demonstrate the impact of guideline training on laypersons simulated performance of CPR skills.
ACKNOWLEDGEMENTS
We thank the participants in Cardiopulmonary Resuscitation Hospital-based Implementation Project (CHIP) Research Group and collaborators to the work reported in this publication including: Gail Delfin, MSN, RN, Marisa Cinousis, Madalyn Karamooz, Linda Hoke, PhD, RN, Jim Kurtz, MPH, BSN, RN, Ryan Dos Reis, BSN, RN, Laura Solano, BSN, RN, Maria Rupp, BSN, RN, Patty Baroni, BSN, RN, Jackie Copeland, BSN, RN, Kenneth Deitch, DO, Kathia Damiron, Manish Goyal, MD, Kimberly Dehnkamp, BSN, RN, Kathy Lehman, RN, Judy Lieberman, MA, Donna Taylor, BSN, RN, Janice Baker, BSN, RN, Sharon Delany, MSN, RN, and Julie Hartman, MPH.
Footnotes
Funding: This work was supported by a grant from the National Institutes of Health (R18HL107217).
Ethical approval: This work was approved by the Institutional Review Board at the University of Pennsylvania and was presented as an abstract at American Heart Association’s Resuscitation Science Symposium in Dallas, TX, November 16, 2013.
Conflicts of interest: Ms. Blewer has equity in Resuscor LLC, a resuscitation education company. Ms. Leary serves on the advisory committee of the American Heart Association’s Emergency Cardiovascular Care Committee and has equity in Resuscor LLC. Ms. Leary has received research funding from the American Heart Association. Dr. Becker has received research funding from Philips Healthcare and PhysioControl, as well as the Medtronic Foundation. Dr. Abella has received research funding and honoraria from Philips Healthcare, in-kind research support from Laerdal Medical Corporation and research funding from Medtronic Foundation. Dr. Abella has equity in Resuscor LLC.
Contributors: Blewer AL proposed and wrote the study. All authors contributed to the design and interpretation of the study, and approved the final manuscript.
REFERENCES
- 1.Hostler D, Everson-Stewart S, Rea TD, Stiell IG, Callaway CW, Kudenchuk PJ, et al. Effect of real-time feedback during cardiopulmonary resuscitation outside hospital: prospective, cluster-randomised trial. Brit Med J. 2011;342:d512. doi: 10.1136/bmj.d512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stiell IG, Brown SP, Christenson J, Cheskes S, Nichol G, Powell J, et al. What is the role of chest compression depth during out-of-hospital cardiac arrest resuscitation?Crit Care Med. 2012;40:1192–1198. doi: 10.1097/CCM.0b013e31823bc8bb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Christenson J, Andrusiek D, Everson-Stewart S, Kudenchuk P, Hostler D, Powell J, et al. Chest compression fraction determines survival in patients with out-of-hospital ventricular fibrillation. Circulation. 2009;120:1241–1247. doi: 10.1161/CIRCULATIONAHA.109.852202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Abella BS, Alvarado JP, Myklebust H, Edelson DP, Barry A, O'Hearn N, et al. Quality of cardiopulmonary resuscitation during in-hospital cardiac arrest. J Amer Med Assoc. 2005;293:305–310. doi: 10.1001/jama.293.3.305. [DOI] [PubMed] [Google Scholar]
- 5.Edelson DP, Litzinger B, Arora V, Walsh D, Kim S, Lauderdale DS, et al. Improving in-hospital cardiac arrest process and outcomes with performance debriefing. Arch Intern Med. 2008;168:1063–1069. doi: 10.1001/archinte.168.10.1063. [DOI] [PubMed] [Google Scholar]
- 6.Wallace SK, Abella BS, Becker LB. Quantifying the effect of cardiopulmonary resuscitation quality on cardiac arrest outcome: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2013;6:148–156. doi: 10.1161/CIRCOUTCOMES.111.000041. [DOI] [PubMed] [Google Scholar]
- 7.Travers AH, Rea TD, Bobrow BJ, Edelson DP, Berg RA, Sayre MR, et al. Part 4: CPR overview:2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2010;122:S676–684. doi: 10.1161/CIRCULATIONAHA.110.970913. [DOI] [PubMed] [Google Scholar]
- 8.Sayre MR, Cantrell SA, White LJ, Hiestand BC, Keseg DP, Koser S. Impact of the 2005 American Heart Association cardiopulmonary resuscitation and emergency cardiovascular care guidelines on out-of-hospital cardiac arrest survival. Prehosp Emerg Care. 2009;13:469–477. doi: 10.1080/10903120903144965. [DOI] [PubMed] [Google Scholar]
- 9.Salmen M, Ewy GA, Sasson C. Use of cardiocerebral resuscitation or AHA/ERC 2005 Guidelines is associated with improved survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. BMJ Open. 2012 Oct 3;2(5):ii. doi: 10.1136/bmjopen-2012-001273. e001273. doi:10.1136/bmjopen-2012-001273. Print 2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Deasy C, Bray JE, Smith K, Wolfe R, Harriss LR, Bernard SA, et al. Cardiac arrest outcomes before and after the 2005 resuscitation guidelines implementation: evidence of improvement?Resuscitation. 2011;82:984–988. doi: 10.1016/j.resuscitation.2011.04.005. [DOI] [PubMed] [Google Scholar]
- 11.Bigham BL, Koprowicz K, Rea T, Dorian P, Aufderheide TP, Davis DP, et al. Cardiac arrest survival did not increase in the Resuscitation Outcomes Consortium after implementation of the 2005 AHA CPR and ECC guidelines. Resuscitation. 2011;82:979–983. doi: 10.1016/j.resuscitation.2011.03.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Blewer AL, Leary M, Decker CS, Andersen JC, Fredericks AC, Bobrow BJ, et al. Cardiopulmonary resuscitation training of family members before hospital discharge using video self-instruction: A feasibility trial. J Hosp Med. 2011;6:428–432. doi: 10.1002/jhm.847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Blewer AL, Leary M, Esposito EC, Gonzalez M, Riegel B, Bobrow BJ, et al. Continuous chest compression cardiopulmonary resuscitation training promotes rescuer self-confidence and increased secondary training: a hospital-based randomized controlled trial*. Crit Care Med. 2012;40:787–792. doi: 10.1097/CCM.0b013e318236f2ca. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Einspruch EL, Lynch B, Aufderheide TP, Nichol G, Becker L. Retention of CPR skills learned in a traditional AHA Heartsaver course versus 30-min video self-training: a controlled randomized study. Resuscitation. 2007;74:476–486. doi: 10.1016/j.resuscitation.2007.01.030. [DOI] [PubMed] [Google Scholar]
- 15.Isbye DL, Rasmussen LS, Lippert FK, Rudolph SF, Ringsted CV. Laypersons may learn basic life support in 24min using a personal resuscitation manikin. Resuscitation. 2006;69:435–442. doi: 10.1016/j.resuscitation.2005.10.027. [DOI] [PubMed] [Google Scholar]
- 16.Lynch B, Einspruch EL, Nichol G, Becker LB, Aufderheide TP, Idris A. Effectiveness of a 30-min CPR self-instruction program for lay responders: a controlled randomized study. Resuscitation. 2005;67:31–43. doi: 10.1016/j.resuscitation.2005.04.017. [DOI] [PubMed] [Google Scholar]
- 17.Mayer V, Schulz CM, Kreuzer M, Wagner KJ, Schneider G, Kochs EF. Cardiopulmonary resuscitation performance during simulator-based trainings: a comparative retrospective analysis of adherence to 2005 and 2010 guidelines. Minerva Anestesiol. 2013;79:264–273. [PubMed] [Google Scholar]
- 18.Jones CM, Thorne CJ, Hulme J. Effect of a rescuer's side of approach on their performance of conventional cardiopulmonary resuscitation. Resuscitation. 2012;83:e235. doi: 10.1016/j.resuscitation.2012.09.013. [DOI] [PubMed] [Google Scholar]
- 19.Yang Z, Li H, Yu T, Chen C, Xu J, Chu Y, et al. Quality of chest compressions during compression-only CPR: a comparative analysis following the 2005 and 2010 American Heart Association guidelines. Am J Emerg Med. 2014;32:50–54. doi: 10.1016/j.ajem.2013.09.043. [DOI] [PubMed] [Google Scholar]
- 20.Rea TD, Stickney RE, Doherty A, Lank P. Performance of chest compressions by laypersons during the Public Access Defibrillation Trial. Resuscitation. 2010;81:293–296. doi: 10.1016/j.resuscitation.2009.12.002. [DOI] [PubMed] [Google Scholar]
- 21.Aufderheide TP, Pirrallo RG, Yannopoulos D, Klein JP, von Briesen C, Sparks CW, et al. Incomplete chest wall decompression: a clinical evaluation of CPR performance by trained laypersons and an assessment of alternative manual chest compression-decompression techniques. Resuscitation. 2006;71:341–351. doi: 10.1016/j.resuscitation.2006.03.021. [DOI] [PubMed] [Google Scholar]
- 22.Rea TD, Eisenberg MS, Culley LL, Becker L. Dispatcher-assisted cardiopulmonary resuscitation and survival in cardiac arrest. Circulation. 2001;104:2513–2516. doi: 10.1161/hc4601.099468. [DOI] [PubMed] [Google Scholar]
- 23.Rea TD, Fahrenbruch C, Culley L, Donohoe RT, Hambly C, Innes J, et al. CPR with chest compression alone or with rescue breathing. N Engl J Med. 2010;363:423–433. doi: 10.1056/NEJMoa0908993. [DOI] [PubMed] [Google Scholar]
- 24.Merchant RM, Abella BS, Abotsi EJ, Smith TM, Long JA, Trudeau ME, et al. Cell phone cardiopulmonary resuscitation: audio instructions when needed by lay rescuers: a randomized, controlled trial. Ann Emerg Med. 2010;55:538–543. doi: 10.1016/j.annemergmed.2010.01.020. e531. [DOI] [PubMed] [Google Scholar]


