Abstract
BACKGROUND:
Timely reperfusion in ST-segment elevation myocardial infarction (STEMI) improves outcomes. System delay is that between first medical contact and reperfusion therapy, comprising prehospital and hospital components. This study aimed to characterize prehospital system delay in Singapore.
METHODS:
A retrospective chart review was performed for 462 consecutive STEMI patients presenting to a tertiary hospital from December 2006 to April 2008. Patients with cardiac arrest secondarily presented were excluded. For those who received emergency medical services (EMS), ambulance records were reviewed. Time intervals in the hospital were collected prospectively. The patients were divided into two equal groups of high/low prehospital system delay using visual binning technique.
RESULTS:
Of 462 patients, 76 received EMS and 52 of the 76 patients were analyzed. The median system delay was 125.5 minutes and the median prehospital system delay was 33.5 minutes (interquartile range [IQR]=27.0, 42.0). Delay between call-received-by-ambulance and ambulance-dispatched was 2.48 minutes (IQR=1.47, 16.55); between ambulance-dispatch and arrival-at-patient-location was 8.07 minutes (IQR=1.30, 22.13); between arrival-at- and departure-from-patient-location was 13.12 minutes (IQR=3.12, 32.2); and between leaving-patient-location to ED-registration was 9.90 minutes (IQR=1.62, 32.92). Comparing patients with prehospital system delay of less than 35.5 minutes versus more showed that the median delay between ambulance-dispatch and arrival-at-patient-location was shorter (5.75 vs. 9.37 minutes, P<0.01). The median delay between arrival-at-patient-location and leaving-patient-location was also shorter (10.78 vs. 14.37 minutes, P<0.01).
CONCLUSION:
Prehospital system delay in our patients was suboptimal. This is the first attempt at characterizing prehospital system delay in Singapore and forms the basis for improving efficiency of STEMI care.
KEY WORDS: Myocardial infarction, Emergency medical services, Delay, First medical contact, Door to balloon
INTRODUCTION
In Singapore, ischemic heart disease is the second leading cause of death,[1] in parallel with worldwide trends.[2] Timely restoration of myocardial blood flow in ST-segment elevation myocardial infarction (STEMI) optimizes myocardial salvage[3,4] and reduces morbidity and mortality.[5,6] Treatment delay is the time between onset of symptoms of STEMI and the receipt of reperfusion therapy, typically primary percutaneous coronary intervention (PCI) or fibrinolytic therapy. A landmark study by De Luca et al[7] showed that every 30 minutes prolongation in treatment delay was associated with a relative risk for 1-year mortality of 1.075.
Door-to-balloon time (D2B) represents only a portion of the time that the STEMI patient is managed by the healthcare system. Figure 1 shows the components of delay in STEMI care. Management of STEMI starts at the point of first medical contact (FMC), defined as the point at which the patient makes first contact with the healthcare system either in the prehospital setting, or the Emergency Department (ED), if the patient did not activate emergency medical services (EMS). System delay is the delay between FMC and reperfusion therapy, and comprises prehospital and hospital components (D2B time). It reflects the organization and efficiency of the EMS and hospital respectively.
Figure 1.
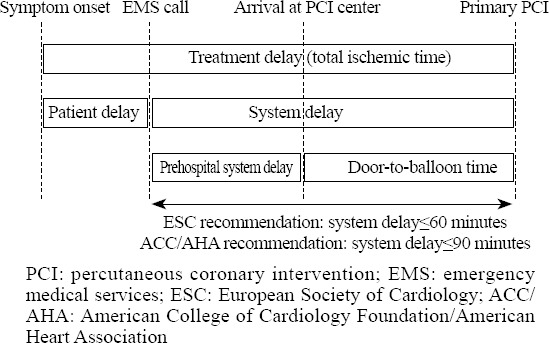
Components of delay in ST-segment elevation myocardial infarction and recommended time intervals by 2012 European Society of Cardiology (ESC) guideline and 2013 American College of Cardiology Foundation/American Heart Association (ACC/AHA).
System delay has been recognized as an indicator of quality of care and a predictor of outcomes. This was demonstrated in a large Dutch registry in 2010, where multivariate analysis showed that system delay was independently associated with mortality (adjusted hazard ratio, 1.10 [95% confidence interval, 1.04–1.16] per 1-hour delay) as its components: prehospital system delay and D2B delay.[8] Recent guidelines have begun to recommend targets for system delay beyond the conventional D2B. The 2012 European Society of Cardiology (ESC) guidelines on STEMI recommend system delay of less than 90 minutes for patients who initially arrive at or are transported to a non-PCI capable hospital, and 60 minutes for patients who initially arrive at or are transported to a PCI capable hospital.[9] The 2013 American College of Cardiology Foundation/American Heart Association (ACC/AHA) guidelines recommend corresponding intervals of 120 minutes and 90 minutes respectively.[10]
Srimahachota et al[11] and Song et al[12] reported that system delay in Asia remains poorly characterized. In Singapore, recent attempts at characterizing treatment delay intervals have found in one institution, a median treatment delay of 272 minutes.[13] In another institution, a median treatment delay of 145 minutes among STEMI patients who presented first to the EMS and 212.5 minutes among those who did not.[14] Both studies found that activation of the EMS was associated with a significant reduction of treatment delay, and even D2B time, via mechanisms currently unknown.
This study aimed to characterize FMC-to-door (FC2D) time among STEMI patients presenting to a tertiary hospital in Singapore.
METHODS
Setting
Singapore is an island city-state in the Southern tip of the Malay Peninsula with a population of 5.3 million over a land area of 715.1 square kilometers.[15] Singapore General Hospital (SGH) is the oldest and largest tertiary referral hospital on the island, and provides around-the-clock primary PCI service. EMS is provided by the Singapore Civil Defence Force (SCDF) fleet of 40 ambulances in a single tier system which is activated by a centralized “995” dispatching system[16] and utilizes computer aided dispatch protocols, global positioning satellite automatic vehicle location systems and road traffic monitoring systems. EMS is publicly funded and provided free of charge for all emergency cases. Average response time in 2001 was 12.6 minutes.[17] Paramedics are trained in basic life-support and adrenaline administration. All SCDF ambulances are fitted with automated external defibrillators. SCDF uses a catchment zone policy where patients from defined geographic areas will be conveyed to the public hospital nearest to the incident location. During the study period, prehospital 12-lead ECG transmission was not yet implemented.[18]
Study population
Consecutive patients presenting between December 2006 and April 2008 to SGH with an ED diagnosis of STEMI for whom the cardiovascular laboratory (CVL) was activated were considered. Patients who suffered a cardiac arrest before the activation of EMS were excluded. Patients who were institutionalized at the time of symptom onset, secondarily presented from another institution or who were already physically at SGH for an unrelated presentation such as clinic visit were excluded because these do not represent the intended presentation of a STEMI patient from the community.
Data collection and processing
Prehospital data were captured retrospectively from paramedic incident reports which include weather and traffic conditions, incident location and interventions. Ambulance monitors and paramedic watches were synchronized at the beginning of every shift to the dispatch central clock. Every ambulance also had a mobile data terminal with central time. Prehospital time variables to be collected were determined before the study: i) time of call to SCDF; ii) time of ambulance dispatch; iii) time of arrival at patient location; iv) time of departure from patient location; and v) time of arrival at hospital. Paramedics transferred the data from their incident reports to an electronic internet-based database after every incident.
After arrival at hospital, time variables were recorded prospectively by ED nurses on a study registration form which accompanied the patient to the CVL, including time of registration at ED. Parts of the form pertaining to first balloon inflation were recorded by the CVL staff.
This study was approved by the Central Institutional Review Board at SGH with a waiver of patient consent.
Statistical analysis
Data entry was performed using a spreadsheet application (Excel 2003, Microsoft Corp., Redmond, WA) and data analysis using IBM® SPSS® Statistics version 22 (SPSS, Chicago, IL). Missing data were excluded from the analysis.
Categorical and continuous data were presented as frequency with percentage and median with range, respectively. Associations between high or low prehospital system delay and categorical variables were assessed using the Chi-square test or Fischer’s exact test while non-parametric test (the Mann-Whitney U test) was used for continuous variables. Statistical significance was set at P<0.05.
Patients who were conveyed by SCDF included for analysis were divided into two equal groups using SPSS’s visual binning facility, and into groups of high and low prehospital system delay.
RESULTS
Of the 476 patients, 14 were excluded (7 collapsed before EMS activation, 2 were in ED for non-related presentations such as trauma, 2 who had secondary presentations were from overseas, 1 was transferred from another institution for social reasons, and 1 was transferred from a nursing home). Of the patients eligible for analysis, 76 activated EMS as the first point of medical contact. Another 17 patients were excluded because of missing or incomplete ambulance run sheets precluding computation of time intervals.
Table 1 shows that the median age of these patients was 56.0 years (range=36.0, 79.0). Forty-three (82.7%) patients were male. Forty-five (86.5%) patients had “chest pain/discomfort” recorded as the presenting complaint. The mean pain score was 14.82. Twenty-nine (55.8%) incidents were from residential locations. Weather condition “sunny-fine” was noted in 46 (88.5%)incidents. Traffic condition was “moderate” in 43 (86.0%) incidents. Twenty-eight (53.8%) patients were treated with glyceryl trinitrate and 7 (13.5%) patients with aspirin. All patients received primary PCI.
Table 1.
Correlates of pre-hospital system delay (first medical contact to door time)
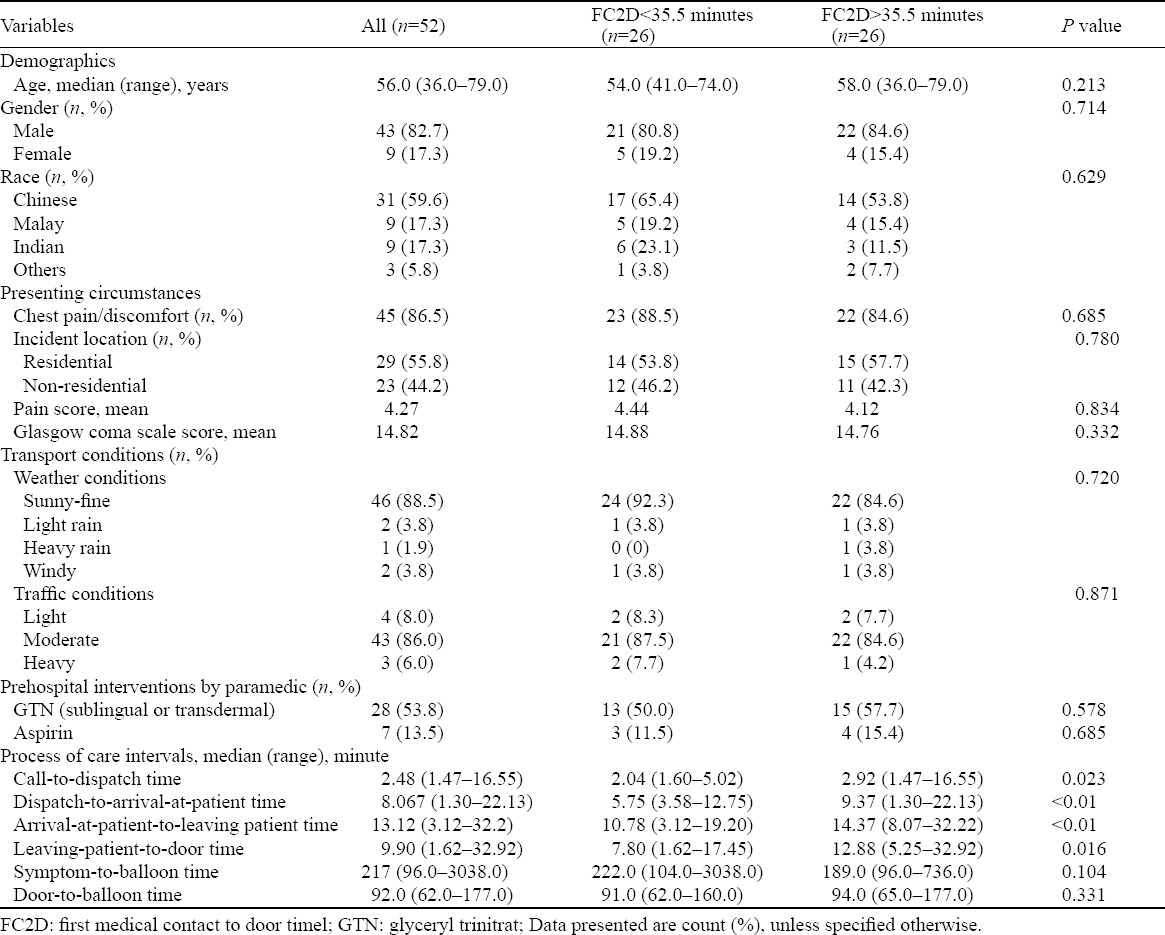
Median total system delay was 125.5 minutes. Median delay between call received by SCDF and registration at ED was 33.5 minutes (interquartile range [IQR]=27.0, 42.0). A breakdown of the components is shown in Figure 2. Delay between call received by SCDF and ambulance dispatched was 2.48 minutes (IQR=1.47, 16.55); between ambulance dispatch and arrival at patient location was 8.07 minutes (IQR=1.30, 22.13); between arrival at and departure from patient location was 13.12 minutes (IQR=3.12, 32.2); and between leaving patient location to registration at ED was 9.90 minutes (IQR=1.62, 32.92).
Figure 2.
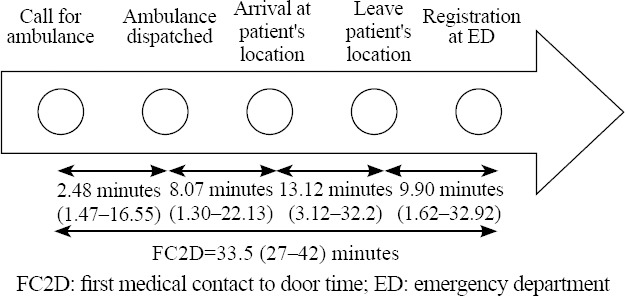
Breakdown of the components of prehospital system delay in the study population.
Among patients with prehospital system delay of less than 35.5 minutes, the median delay between ambulance dispatch and arrival at patient location was 5.75 minutes (IQR=3.58, 12.75), which was significantly lower than in patients with prehospital system delay of more than 35.5 minutes, which was 9.37 minutes (IQR=1.30, 22.13), P<0.01.
Similarly, among patients with prehospital system delay of less than 35.5 minutes, the median delay between arrival at patient location and leaving patient location was 10.78 minutes (IQR=3.12, 19.20), which was significantly lower than in patients with prehospital system delay of more than 35.5 minutes, which was 14.37 minutes (IQR=8.07, 32.22) (P<0.01).
Comparing patients with prehospital system delay of less than 35.5 minutes with those more than 35.5 minutes showed that there were no significant differences in age, gender or race. Neither group was more likely to present with chest pain to the EMS, there were no significant differences in transport conditions (traffic and weather) or type of incident location (residential vs. non-residential). Administration of aspirin or nitroglycerin by paramedics in the ambulance did not significantly affect prehospital treatment delay.
DISCUSSION
This is to the our knowledge the first attempt to characterize prehospital system delay in Singapore using EMS data. The median prehospital delay time of 33.5 minutes among STEMI patients seems to mirror that for out-of-hospital cardiac arrest patients in the same population of 35.5 minutes.[16]
The data suggest that in this population, the delays between ambulance dispatched and arrival at patient location, and that between arrival at patient location to leaving patient location contributed significantly to prehospital system delay.
The mean system delay of 125.5 minutes fell short of both the 60 minutes recommended by the ESC and 90 minutes recommended by the ACC/AHA.
A key limitation of this study lies in that it is underpowered to detect correlates and adverse outcomes such as mortality. Despite a good duration studied and sizeable sample size, the low EMS utilization rate of 16.5% produced a very small subgroup for analysis. Future studies would benefit from data pooled from multiple centers that also receive STEMI patients from SCDF.
While the delay between symptom onset and reperfusion time (ischemic time) is the most important from the patient’s perspective, characterizing system delay (Figure 1) is meaningful as it reflects the collective efficiency of the EMS and hospital system, which involves a complex sequence of collaborative care delivered by personnel ranging from paramedics and emergency physicians to the interventional cardiologist. This study offers a first glimpse at the relative contributions of various components to system delay.
Amidst immense attention to reduce D2B, quality improvements have in recent years reduced nationwide median D2B time from 75 minutes to 51 minutes.[18] However, if the aim is to reduce total ischemic time, which is the principal determinant of outcome, broader initiatives at a system level are required, bringing to the forefront the role of prehospital care. In fact, the benefit of a short D2B time appears to be limited to patients with a short prehospital delay.[5] Prehospital diagnosis, triage and initial emergency treatment in the ambulance have been shown to be associated with greater use of reperfusion therapies, reduced delays and improved outcomes.[8,19] The traditional division of responsibility between the EMS and the hospital is increasingly blurred in this regard and this is demonstrated most clearly with prehospital 12-lead ECG transmission[18] and proposals to bypass the ED for CVL activation.[9]
It is hoped that this attempt at characterization of the prehospital process of STEMI care will enable the organization of efforts to improve its efficacy and efficiency.
In a community where STEMI patients underutilize EMS,[13,14] it is hypothesized by the authors that efforts to reduce system delay must be accompanied by public health efforts to increase EMS utilization rate in order to see the effects of such efforts.
In conclusion, this study characterizes prehospital system delay among STEMI patients presenting to the ED of a tertiary referral hospital in Singapore. Prehospital system delay in this population appears to be suboptimal judging by international guidelines. This is to the best of our knowledge the first attempt at examining prehospital component of system delay in STEMI patients in Singapore.
Footnotes
Funding: None.
Ethical approval: The Central Institutional Review Board at SGH approved this study with a waiver of patient consent.
Conflicts of interest: The authors declare that there is no conflict of interest.
Contributors: Andrew Fu Wah Ho proposed the study. All authors contributed to the design and interpretation of the study, and approved the final manuscript.
REFERENCES
- 1.Health Facts Singapore. Ministry of Health Singapore. 2012. [Accessed November 27 2013]. http://www.moh.gov.sg/content/moh_web/home/statistics/Health_Facts_Singapore/Principal_Causes_of_Death.html.
- 2.The top 10 causes of death. World Health Organization Fact Sheets. [Accessed November 27 2013]. http://www.who.int/mediacentre/factsheets/fs310/en/index3.html.
- 3.Reimer KA, Jennings RB. The “wavefront phenomenon” of myocardial ischemic cell death. II. Transmural progression of necrosis within the framework of ischemic bed size (myocardium at risk) and collateral flow. Lab Invest. 1979;40:633–644. [PubMed] [Google Scholar]
- 4.Gersh BJ, Stone GW, White HD, Holmes DR. Pharmacological facilitation of primary percutaneous coronary intervention for acute myocardial infarction: is the slope of the curve the shape of the future?JAMA. 2005;293:979–986. doi: 10.1001/jama.293.8.979. [DOI] [PubMed] [Google Scholar]
- 5.Shiomi H, Nakagawa Y, Morimoto T, Furukawa Y, Nakano A, Shirai S, et al. Association of onset to balloon and door to balloon time with long term clinical outcome in patients with ST elevation acute myocardial infarction having primary percutaneous coronary intervention: observational study. BMJ. 2012;3257:1–14. doi: 10.1136/bmj.e3257. [DOI] [PubMed] [Google Scholar]
- 6.Anderson JL, Karagounis La, Califf RM. Meta-analysis of five reported studies on the relation of early coronary patency grades with mortality and outcomes after acute myocardial infarction. Am J Cardiol. 1996;78:1–8. doi: 10.1016/s0002-9149(96)00217-2. [DOI] [PubMed] [Google Scholar]
- 7.De Luca G, Suryapranata H, Ottervanger JP, Antman EM. Time delay to treatment and mortality in primary angioplasty for acute myocardial infarction: every minute of delay counts. Circulation. 2004;109:1223–1225. doi: 10.1161/01.CIR.0000121424.76486.20. [DOI] [PubMed] [Google Scholar]
- 8.Terkelsen CJ, Sørensen JT, Maeng M, Jensen LO, Tilsted HH, Trautner S, et al. System delay and mortality among patients with STEMI treated with primary percutaneous coronary intervention. JAMA. 2010;304:763–771. doi: 10.1001/jama.2010.1139. [DOI] [PubMed] [Google Scholar]
- 9.Steg PG, James SK, Atar D, Badano LP, Blömstrom-Lundqvist C, Borger MA, et al. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation. Eur Heart J. 2012;33:2569–2619. doi: 10.1093/eurheartj/ehs215. [DOI] [PubMed] [Google Scholar]
- 10.O'Gara PT, Kushner FG, Ascheim DD, Casey DE, Jr, Chung MK, de Lemos JA, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;127:e362–425. doi: 10.1161/CIR.0b013e3182742cf6. [DOI] [PubMed] [Google Scholar]
- 11.Srimahachota S, Kanjanavanit R, Boonyaratavej S, Boonsom W, Veerakul G, Tresukosol D, et al. Demographic, management practices and in-hospital outcomes of Thai Acute Coronary Syndrome Registry (TACSR): the difference from the Western world. J Med Assoc Thai. 2007;90(Suppl 1):1–11. [PubMed] [Google Scholar]
- 12.Song L, Yan H, Hu D, Yang J, Sun Y. Pre-hospital care-seeking in patients with acute myocardial infarction and subsequent quality of care in Beijing. Chin Med J (Engl) 2010;123:664–669. [PubMed] [Google Scholar]
- 13.Ho AFW, Fook-Chong S, Pek PP, Ng YY, Wong ASL, Ong MEH. Prehospital presentation of patients with ST-segment elevation myocardial infarction in Singapore. Int J Cardiol. 2013;168:4273–4276. doi: 10.1016/j.ijcard.2013.04.204. [DOI] [PubMed] [Google Scholar]
- 14.Tan LL, Wong HB, Poh CL, Chan MY, Seow SC, Yeo TC, et al. Utilisation of emergency medical service among Singapore patients presenting with ST-segment elevation myocardial infarction: prevalence and impact on ischaemic time. Intern Med J. 2011;41:809–814. doi: 10.1111/j.1445-5994.2010.02278.x. [DOI] [PubMed] [Google Scholar]
- 15.Statistics Singapore. Department of Statistics Singapore. [Accessed November 27 2013]. http://www.singstat.gov.sg/statistics/latest_data.html#14.
- 16.Shin SD, Ong MEH, Tanaka H, Ma MH, Nishiuchi T, Alsakaf O, et al. Comparison of emergency medical services systems across Pan-Asian countries: a Web-based survey. Prehosp Emerg Care. 2012;16:477–496. doi: 10.3109/10903127.2012.695433. [DOI] [PubMed] [Google Scholar]
- 17.Ong MEH, Chan YH, Anantharaman V, Lau ST, Lim SH, Seldrup J. Cardiac arrest and resuscitation epidemiology in Singapore (CARE I study) Prehosp Emerg Care. 2003;7:427–433. doi: 10.1080/312703002120. [DOI] [PubMed] [Google Scholar]
- 18.Ong MEH, Wong ASL, Seet CM, Teo SG, Lim BL, Ong PJ, et al. Nationwide improvement of door-to-balloon times in patients with acute ST-segment elevation myocardial infarction requiring primary percutaneous coronary intervention with out-of-hospital 12-lead ECG recording and transmission. Ann Emerg Med. 2013;61:339–347. doi: 10.1016/j.annemergmed.2012.08.020. [DOI] [PubMed] [Google Scholar]
- 19.Huber K, De Caterina R, Kristensen SD, Verheugt FW, Montalescot G, Maestro LB, et al. Pre-hospital reperfusion therapy: a strategy to improve therapeutic outcome in patients with ST-elevation myocardial infarction. Eur Heart J. 2005;26:2063–2074. doi: 10.1093/eurheartj/ehi413. [DOI] [PubMed] [Google Scholar]


