Abstract
Adolescents psychiatrically hospitalized following a suicide attempt are at high risk for a repeat attempt or suicide completion, and substance use is consistently implicated as a risk factor for continued suicidal behavior in adolescents. Despite this knowledge, there have been few studies that have investigated the effectiveness of combined suicidality and substance use interventions within acute psychiatric care settings for suicidal youth with substance use problems. While social workers are well-positioned to deliver such interventions, greater emphasis on teaching integrated therapeutic techniques in social work curriculum and professional training is needed to ensure their implementation.
Keywords: adolescence, mental health, psychosocial intervention, social work, suicide, substance abuse
Suicide is the third leading cause of death for adolescents (aCenters for Disease Control and Prevention [CDC], 2012a), accounting for 13% of deaths in this age group (CDC, 2012a). From 2009 to 2011, the prevalence of having attempted suicide increased from 6.3% to 7.8% among high school students nationwide (CDC, 2012b). A prior suicide attempt is one of the strongest risk factors for a repeat suicide attempt and eventual completed suicide among adolescents (Bridge, Goldstein, & Brent, 2006; Goldston et al., 2003; Zahl & Hawton, 2004; Shaffer, Gould, Fisher, Trautman, & Moreau, 1996). Adolescents who have attempted suicide are almost 18 times more likely to attempt suicide again compared to those who have never made an attempt (Lewinsohn, Rohde, & Seeley, 1994) and it has been estimated that up to 11% of adolescents who attempt suicide will eventually commit suicide (Ho, 2003).
The weeks after discharge from psychiatric hospitalization represent an especially critical period for suicide risk (Hunt et al., 2009; Knesper, American Association of Suicidology, & Suicide Prevention Resource Center, 2010). In a study that included 106 adolescents hospitalized for a suicide attempt, almost two-thirds reported a subsequent suicide attempt in follow-up assessments conducted over 2 years (Groholt, Ekeberg, & Haldorsen, 2006). One of the more comprehensive studies of adolescent suicidality to date has been a study of 180 psychiatrically hospitalized adolescents repeatedly assessed for up to 13 years, which found the number of prior suicide attempts as the strongest predictor of post-hospitalization attempts (Goldston et al., 2003).
Substance use, especially alcohol use, is consistently implicated as a risk factor for continued suicidal behavior in adolescents (Brent & Perper, 1995). Comorbid affective and substance use disorders greatly increases the risk of suicide completion in adolescents (Bukstein et al., 1993) as well as suicide attempts, by as much as 25-fold (Miller et al., 2011; Wu et al., 2004). The disinhibition caused by alcohol intoxication can both facilitate suicidal ideation and increase the likelihood of acting on suicidal thoughts (Sher, 2006), and has been implicated in the use of more lethal suicide attempt methods (Brent, Perper, & Allman, 1987). As many as 46% of adolescents who have attempted suicide reported being under the influence of alcohol at the time of the attempt (Brent et al., 1987; Groholt et al., 2006; Kotila & Lonnqvist, 1988; Mean, Camparini-Righini, Narring, Jeannin, & Michaud, 2005; Vajda & Steinbeck, 2000). In the largest chart review to date of adolescents presenting to an urban general hospital after a suicide attempt, a substance use disorder was the only psychiatric diagnosis associated with suicide attempts of higher medical lethality (O'Brien & Berzin, 2012). Therefore, adolescents hospitalized for a suicide attempt who have a co-occurring substance use disorder are arguably at greatest risk for reattempting and/or completing suicide, relative to adolescents with suicidal ideation, suicide attempts, or substance use alone.
Unpublished data collected by Esposito-Smythers and colleagues (2012) of 188 adolescent psychiatric inpatients in a facility in the northeast United States found that 17% (n = 32) were admitted following a suicide attempt. Of this subset of attempters, 44% (n = 14) met criteria for an alcohol use disorder. Most notable, the presence of an alcohol use disorder in this subset of the sample admitted for a suicide attempt was twice as high as the entire sample (44% vs. 22%). These frequencies support prior research findings that demonstrate alcohol use and suicidality as functionally interrelated in adolescents (Bagge & Sher, 2008) and that the relationship strengthens as the severity of each problem increases (Esposito & Spirito, 2004; Esposito-Smythers et al., 2012; Goldston, 2004). A study by Wu et al. (2004) found adolescent suicide attempts to be strongly correlated with alcohol abuse and dependence, even after controlling for depression; however, the association between alcohol abuse and suicidal ideation was not significant after controlling for depression, suggesting the especially important role that alcohol abuse plays in suicidal behavior compared to suicidal ideation. These findings suggest that substance use may be a factor that predicts or hastens the transition from suicidal ideation to attempt in adolescents. Thus, integration of substance abuse interventions into the psychiatric treatment for adolescents who attempt suicide seems clear.
Adolescent Inpatient Psychiatric Care: A Missed Opportunity for Integrated Interventions
Despite knowledge of elevated post-discharge rates of death by suicide, suicide attempts, and readmissions to acute care services in the weeks following acute psychiatric care of adolescents who have attempted suicide, there have been few systematic suicide prevention efforts in the United States that have focused on this vulnerable population during this high risk time period (Knesper et al., 2010). And despite the strong association between adolescent substance use and suicidal behaviors, few studies have investigated the effectiveness of combined interventions for these two problems (Conason, Oquendo, & Sher, 2006). Because the presence of a substance use disorder is significantly associated with readmission of adolescents to inpatient care (Fontanella, 2008), it is imperative that inpatient psychiatric facilities take action to adequately address substance use issues when they present in adolescents admitted due to suicidal behavior.
Suicidality and substance use are two phenomena that noticeably increase in adolescence, making this developmental period an especially critical one in which to intervene (Daniel & Goldston, 2009; Galaif, Sussman, Newcomb, & Locke, 2007). Despite the strong link between substance use and suicidality, the standard of care is to treat these two problems separately (Esposito-Smythers et al., 2012). Adolescent psychiatric hospitals most often only cursorily address substance use because of the short length of stay, making suicide risk the primary focus of treatment (Rowan, 2001). The lack of substance abuse training for many clinicians in the mental health field (Riggs, 2003) also lowers the likelihood of alcohol and other drug use being addressed on adolescent inpatient units. Given the significant role substance use plays in subsequent suicidal behaviors, greater attention to substance use interventions in adolescent inpatient psychiatric settings is critical.
While there is often debate about which disorder to treat first with these adolescents, research suggests the importance of implementing integrated services rather than conducting serial or parallel treatment for comorbid substance abuse and psychiatric disorders (Esposito-Smythers & Goldston, 2008; Hawkins, 2009; Sher & Zalsman, 2005). However, current service systems are generally inadequately prepared to meet these needs because of multiple clinical, administrative, and policy barriers (Hawkins, 2009), and because the average cost of treating youth with comorbid disorders can be more than double what it costs to treat an adolescent with just one disorder (King, Gaines, Lambert, Summerfelt, & Bickman, 2000). Brief and feasible empirically supported interventions can help to address substance use in inpatient psychiatric settings for adolescents, and new interventions that specifically address alcohol and other drug use as a risk factor for continued suicidal thoughts and behaviors are especially critical. Two interventions that demonstrate potential for use in acute care settings due to their ability to concurrently address issues of substance abuse and suicidality include Integrated Cognitive Behavioral Treatment (I-CBT; Esposito-Smythers, Spirito, Kahler, Hunt, & Monti, 2011) and Motivational Interviewing (MI).
Integrated Cognitive Behavioral Treatment
I-CBT is an intervention for adolescents with comorbid suicidality and substance abuse that demonstrated promising results in its initial trial (Esposito-Smythers et al., 2011). I-CBT is grounded in social cognitive learning theory and aims to promote change by helping individuals relearn adaptive ways of relating to themselves and others, as well as developing self-efficacy in their ability to implement these learned skills (Bandura, 1986). For I-CBT to effectively treat comorbid substance abuse and suicidality in adolescents, the protocol must target the common maladaptive behaviors and beliefs that underlie these two problems (Esposito-Smythers et al., 2011). Individually, this work must address an adolescent's cognitive distortions, coping style, and communication with peers and parents using cognitive restructuring, problem solving, affect regulation, and communication skills (Esposito-Smythers et al., 2011). To bolster its effectiveness, I-CBT includes parents as equal partners in treatment. Parent training and family sessions are regularly scheduled to address the adolescent's mental health and substance abuse treatment goals. Parent training sessions are helpful in teaching parental monitoring and addressing parent issues that may interfere with parenting. Family sessions can serve to enhance communication and behavioral contracting (Esposito-Smythers et al., 2011). Improvement in adolescent and parent skill development should lead to reductions in substance use and suicidality. In the only randomized trial testing an I-CBT intervention targeted at substance use and suicidality outcomes, Esposito-Smythers et al. (2011) found I-CBT, relative to enhanced treatment as usual (E-TAU), resulted in significantly fewer heavy drinking days and days of marijuana use. The adolescents receiving I-CBT also reported less global impairment as well as fewer suicide attempts, inpatient psychiatric hospitalizations, and emergency department visits than those receiving E-TAU.
Motivational Interviewing
The transtheoretical model describes change as a process involving progress through a series of stages of change (Prochaska, DiClemente, & Norcross 1992). Prochaska et al. (1992) posit that addictive behavior change involves progression through five stages: pre-contemplation, contemplation, preparation, action, and maintenance, with the typical individual going through these stages many times before making a lasting change. In order for long term substance abuse treatment to be effective with adolescents, engagement in at least the contemplation stage of change is critical. However, because substance use is normative in adolescence and many do not recognize their substance use as a problem, many adolescents are in the pre-contemplation stage of change. In this stage they are not considering change, but often have adults telling them to do so. Therefore, it may be more effective to intervene with adolescents in the pre-contemplation stage using a brief intervention aimed at identifying and developing the motivation to change, rather than implementing an I-CBT protocol before the adolescent is ready for change. Because adolescents admitted to a psychiatric unit are in a state of crisis, the hospitalization may serve as an opportune moment to deliver such a brief motivational intervention.
MI is a brief treatment modality for adolescents with substance use disorders that is feasible to implement on psychiatric units. When adolescents are hospitalized due to their acute psychiatric symptoms, they may be more receptive than usual to acknowledging the role that alcohol and other drugs can play in their worsening mental health problems. Capitalizing on such, a “teachable moment” has been shown to be useful, for example, in alcohol-related Emergency Department (ED) visits (Monti et al., 1999; Spirito et al., 2004, 2011). Spirito and colleagues (2004) found that adolescents receiving a brief MI intervention in the ED reported less binge drinking and fewer drinking days per month at follow-up. MI is a client-centered, directive method for enhancing intrinsic motivation to change by exploring and resolving ambivalence (Miller & Rollnick, 2002). Originally, MI was developed for adult problem drinkers; however, it is currently being used with adolescents exhibiting a wide range of problem behaviors. MI is a promising therapeutic technique for use with adolescents who are using substances because it fosters a therapeutic environment that acknowledges choices and ambivalence, does not argue against resistance, and supports personal change goals rather than institutional or counselor-based goals. Additionally, because adolescents rarely admit to or recognize substance use problems, MI's use of a nonjudgmental and nonconfrontational style may be particularly useful for engaging adolescents who are at this stage and are experiencing low levels of motivation to change.
Given consistent findings in support of MI as an effective therapeutic technique with adolescents, integrating a brief MI intervention into an inpatient psychiatric hospitalization treatment protocol has the potential to enhance motivation to stop or reduce alcohol and other drug use, and possibly seek substance abuse treatment upon discharge. Despite the fact that MI interventions are versatile enough to be implemented in a variety of settings, only one known study has tested a MI intervention on an inpatient psychiatric unit. Brown et al. (2009) implemented a brief MI intervention with adolescents in a psychiatric hospital setting which specifically targeted smoking cessation. This study found that the MI intervention, relative to the control condition in which adolescent inpatients received brief advice about smoking cessation, was associated with better substance use outcomes during the first 6 months following psychiatric hospitalization. Despite these significant findings, along with the feasibility and acceptability of the protocol, no other studies have tested a brief MI intervention in an adolescent psychiatric unit.
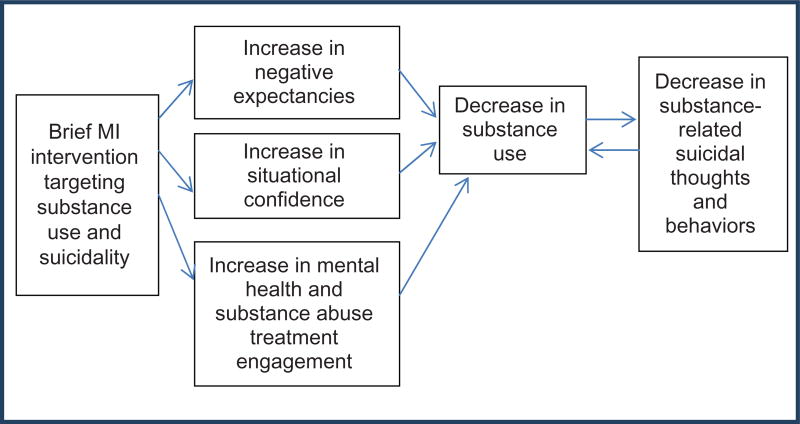
In addition to the feasibility and acceptability of MI, an advantage of MI interventions is the capacity to tailor feedback to the specific needs of the adolescent. This is especially critical in a high risk population such as adolescent inpatients who frequently present with complex co-occurring symptomatology. Adolescent inpatients might benefit from a MI approach that specifically tailors feedback to address substance use as a risk factor for continued suicidal thoughts and behaviors. This feedback can be designed to increase adolescents' motivation to alter alcohol and other drug use by helping them to recognize the potential link between their substance use and suicidal behaviors. In doing so, the MI intervention can serve to increase negative substance use expectancies, increase situational confidence in the ability to resist the urge to use alcohol and other drugs, and increase engagement in post-discharge substance abuse treatment when necessary. These potential mechanisms of change in reducing substance use may have a bidirectional influence on decreasing substance-related suicidal thoughts and behaviors (see Figure 1).
Figure 1.
A proposed mechanism of change model for adolescents receiving a brief motivational intervention for substance abuse in a psychiatric hospital following a suicide attempt (color figure available online).
Social Workers as Interventionists
Key determinants of the implementation of brief substance abuse interventions on adolescent inpatient units are feasibility and acceptability. Despite the severe consequences of these two co-occurring problems and the call for treatment of psychiatric and substance abuse problems in the same setting (Brent & Perper, 1995), inpatient treatment rarely addresses substance use, as the adolescent's suicidal risk is the primary focus of treatment. Social workers are well positioned to deliver such integrated interventions on adolescent inpatient units, as they frequently serve as clinicians in these facilities. Using MI as an integrative intervention is promising due to the inherent flexibility of the MI approach, and is supported by recent work demonstrating MI as useful intervention for social workers in school settings (Frey et al., 2011).
Employment of social workers is expected to grow by 25% from 2010 to 2020, faster than the average for all occupations (14%). Specifically, employment of mental health and substance abuse social workers is expected to grow by 31% (Bureau of Labor Statistics, U.S. Department of Labor, 2012). Because it is projected that social workers will be providing a greater percentage of substance abuse treatment than in the past, it is critical that substance abuse training be incorporated into MSW curriculum and continuing education training. A study by Bina et al. (2008) found that 65% of recent MSW graduates did not receive any formal substance abuse training in field work, academic courses, continuing education, or other specialty training. Social work curriculum and other professional training must address this deficiency by formalizing substance use requirements (Quinn & Straussner, 2010). Specifically, it will be critical to integrate substance use knowledge as a core component of the assessment and treatment of suicidal youth, in order for social workers to develop and implement more effective interventions.
Conclusion
A significant proportion of adolescents who attempt suicide have a comorbid substance use disorder. Substance use, particularly alcohol use, puts suicidal adolescents at greater risk for repeat suicide attempts and eventual suicide completion. Adolescents with comorbid substance use disorders and suicidality may benefit from the implementation of I-CBT techniques in inpatient psychiatric settings to address the co-occurring problems, especially those that utilize a family component. For adolescents who do not meet full criteria for a substance use disorder, or meet this criteria but are in the pre-contemplation stage of change, MI may be a more feasible and effective intervention to implement during their psychiatric hospitalization, as this inpatient stay can often serve as a critical teaching moment for adolescents who have just attempted suicide. In these teachable moments, interventions such as MI can be useful in helping the adolescents understand the relationship between their substance use and continued suicidal thoughts and behaviors, and in doing so prepare them for change. Social workers are well-positioned to deliver such interventions in acute care settings, but greater devotion to teaching such integrated interventions in social work curriculum and professional training is needed.
References
- Bagge C, Sher KJ. Adolescent alcohol involvement and suicide attempts: Toward the development of a conceptual framework. Clinical Psychology Review. 2008;28:1283–1296. doi: 10.1016/j.cpr.2008.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bandura A. Social foundations of thought and action: A social cognitive theory. Saddle River, NJ: Prentice-Hall; 1986. [Google Scholar]
- Bina R, Hall D, Mollette A, Smith-Osborne A, Yum J, Sowbel L, Jani J. Substance abuse training and perceived knowledge: Predictors of perceived preparedness to work in substance abuse. Journal of Social Work Education. 2008;44(3):7–20. [Google Scholar]
- Brent DA, Perper JA. Research in adolescent suicide: Implications for training, service delivery, and public policy. Suicide and Life-Threatening Behavior. 1995;25(2):222–230. [PubMed] [Google Scholar]
- Brent DA, Perper JA, Allman C. Alcohol, firearms, and suicide among youth: Temporal trends in Allegheny County, Pennsylvania, 1960 to 1983. Journal of the American Medical Association. 1987;257:3369–3371. [PubMed] [Google Scholar]
- Bridge JA, Goldstein TR, Brent DA. Adolescent suicide and suicidal behavior. Journal of Child Psychology and Psychiatry. 2006;47(3–4):372–394. doi: 10.1111/j.1469-7610.2006.01615.x. [DOI] [PubMed] [Google Scholar]
- Brown RA, Strong DR, Abrantes AM, Myers MG, Ramsey SE, Kahler CW. Effects on substance use outcomes in adolescents receiving motivational interviewing for smoking cessation during psychiatric hospitalization. Addictive Behaviors. 2009;34(10):887–891. doi: 10.1016/j.addbeh.2009.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bukstein OG, Brent DA, Perper JA, Moritz G, Baugher M, Schweers J, Roth C, Balach L. Risk factors for completed suicide among adolescents with a lifetime history of substance abuse: A case-control study. Acta Psychiatrica Scandanavica. 1993;88:403–408. doi: 10.1111/j.1600-0447.1993.tb03481.x. [DOI] [PubMed] [Google Scholar]
- Bureau of Labor Statistics; U.S. Department of Labor. Occupational outlook handbook, 2012–13 edition, social workers. 2012 Retrieved from http://www.bls.gov/ooh/community-and-social-service/social-workers.htm.
- Centers for Disease Control and Prevention (CDC) Web-based injury statistics query and reporting system (WISQARS) 2012a Retrieved from http://www.cdc.gov/injury/wisqars/LeadingCauses.html.
- Centers for Disease Control and Prevention (CDC) Youth risk behavior surveillance—United States. Morbidity and Mortality Weekly Report. 2012b;2011;61(4):1–162. [PubMed] [Google Scholar]
- Conason AH, Oquendo MA, Sher L. Psychotherapy in the treatment of alcohol and substance abusing adolescents with suicidal behavior. International Journal of Adolescent Medicine and Health. 2006;18(1):9–13. doi: 10.1515/ijamh.2006.18.1.9. [DOI] [PubMed] [Google Scholar]
- Daniel SS, Goldston DB. Interventions for suicidal youth: A review of the literature and developmental considerations. Suicide and Life Threatening Behavior. 2009;39(3):252–268. doi: 10.1521/suli.2009.39.3.252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esposito C, Spirito A. Adolescent substance use and suicidal behavior: A review with implications for treatment research. Alcoholism: Clinical and Experimental Research. 2004;28:775–785. doi: 10.1097/01.alc.0000127417.99752.87. [DOI] [PubMed] [Google Scholar]
- Esposito-Smythers C, Goldston DB. Challenges and opportunities in the treatment of adolescents with substance use disorder and suicidal behavior. Substance Abuse. 2008;29(2):5–17. doi: 10.1080/08897070802092835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esposito-Smythers C, Spirito A, Kahler CW, Hunt J, Monti P. Treatment of co-occurring substance abuse and suicidality among adolescents: A randomized trial. Journal of Consulting and Clinical Psychology. 2011;79(6):728–739. doi: 10.1037/a0026074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Esposito-Smythers C, Walsh A, Spirito A, Rizzo C, Goldston D, Kaminer Y. Working with the suicidal client who also abuses substances. Cognitive and Behavioral Practice. 2012;19:244–255. doi: 10.1016/j.cbpra.2010.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fontanella CA. The influence of clinical, treatment, and healthcare system characteristics on psychiatric readmission of adolescents. American Journal of Orthopsychiatry. 2008;78(2):187–198. doi: 10.1037/a0012557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frey AJ, Cloud RN, Lee J, Small JW, Seeley JR, Feil EG, Walker HM, Golly A. The promise of motivational interviewing in school mental health. School Mental Health. 2011;3:1–12. [Google Scholar]
- Galaif ER, Sussman S, Newcomb MD, Locke TF. Suicidality, depression, and alcohol use among adolescents: A review of empirical findings. International Journal of Adolescent Medical Health. 2007;19(1):27–35. doi: 10.1515/ijamh.2007.19.1.27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldston DB. Conceptual issues in understanding the relationship between suicidal behavior and substance use in adolescence. Drug and Alcohol Dependence. 2004;76(Suppl):79–91. doi: 10.1016/j.drugalcdep.2004.08.009. [DOI] [PubMed] [Google Scholar]
- Goldston DB, Reboussin BA, Kancler C, Daniel SS, Frazier PH, Harris AE, … Reboussin DM. Rates and predictors of aftercare services among formerly hospitalized adolescents: A prospective naturalistic study. Journal of the American Academy of Child and Adolescent Psychiatry. 2003;42(1):49–56. doi: 10.1097/00004583-200301000-00010. [DOI] [PubMed] [Google Scholar]
- Groholt B, Ekeberg O, Haldorsen T. Adolescent suicide attempters: What predicts future suicidal acts? Suicide and Life-Threatening Behavior. 2006;36(6):638–650. doi: 10.1521/suli.2006.36.6.638. [DOI] [PubMed] [Google Scholar]
- Hawkins EH. A tale of two systems: Co-occurring mental health and substance abuse disorders treatment for adolescents. Annual Review of Psychology. 2009;60:197–227. doi: 10.1146/annurev.psych.60.110707.163456. [DOI] [PubMed] [Google Scholar]
- Ho TP. The suicide risk of discharged psychiatric patients. Journal of Clinical Psychiatry. 2003;64(6):702–707. doi: 10.4088/jcp.v64n0613. [DOI] [PubMed] [Google Scholar]
- Hunt IM, Kapur N, Webb R, Robinson J, Burns J, Shaw J, Appleby L. Suicide in recently discharged psychiatric patients: A case-control study. Psychological Medicine. 2009;39(3):443–449. doi: 10.1017/S0033291708003644. [DOI] [PubMed] [Google Scholar]
- King RD, Gaines LS, Lambert EW, Summerfelt WT, Bickman L. The co-occurrence of psychiatric and substance abuse diagnoses in adolescents in different service systems: Frequency, recognition, cost, and outcomes. Journal of Behavioral Health Services & Research. 2000;27:417–430. doi: 10.1007/BF02287823. [DOI] [PubMed] [Google Scholar]
- Knesper DJ American Association of Suicidology; Suicide Prevention Resource Center. Continuity of care for suicide prevention and research: Suicide attempts and suicide deaths subsequent to discharge from the emergency department or psychiatry inpatient unit. Newton, MA: Education Development Center; 2010. [Google Scholar]
- Kotila L, Lonnqvist J. Adolescent suicide attempts: Sex differences predicting suicide. Acta Psychiatrica Scandinavica. 1988;77(3):264–270. doi: 10.1111/j.1600-0447.1988.tb05119.x. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Rohde P, Seeley JR. Psychosocial risk factors for future adolescent suicide attempts. Journal of Consulting and Clinical Psychology. 1994;62:287–305. doi: 10.1037//0022-006x.62.2.297. [DOI] [PubMed] [Google Scholar]
- Mean M, Camparini-Righini N, Narring F, Jeannin A, Michaud P. Substance use and suicidal conduct: A study of adolescents hospitalized for suicide attempt and ideation. Acta Paediatrica. 2005;94(7):952–959. doi: 10.1111/j.1651-2227.2005.tb02016.x. [DOI] [PubMed] [Google Scholar]
- Miller M, Borges G, Orozco R, Mukamal K, Rimm EB, Benjet C, Medina-Mora ME. Exposure to alcohol, drugs and tobacco and the risk of subsequent suicidality: Findings from the Mexican Adolescent Mental Health Survey. Drug and Alcohol Dependence. 2011;113(2–3):110–117. doi: 10.1016/j.drugalcdep.2010.07.016. [DOI] [PubMed] [Google Scholar]
- Miller WR, Rollnick S. Motivational interviewing: Preparing people for change. 2nd. New York, NY: Guilford Press; 2002. [Google Scholar]
- Monti P, Colby S, Barnett N, Spirito A, Rohsenow D, Myers M, Woolard R, Lewander W. Brief intervention for harm reduction with alcohol-positive older adolescents in a hospital emergency department. Journal of Consulting and Clinical Psychology. 1999;67:989–994. doi: 10.1037//0022-006x.67.6.989. [DOI] [PubMed] [Google Scholar]
- O'Brien K, Berzin SC. Examining the impact of psychiatric diagnosis and comorbidity on the medical lethality of adolescent suicide attempts. Suicide and Life Threatening Behavior. 2012;42(4):437–444. doi: 10.1111/j.1943-278X.2012.00102.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prochaska JO, DiClemente CC, Norcross JC. In search of how people change: Applications to addictive behaviors. American Psychologist. 1992;47(9):1102–1114. doi: 10.1037//0003-066x.47.9.1102. [DOI] [PubMed] [Google Scholar]
- Quinn G, Straussner SLA. Licensure and continuing education requirements for substance abuse training in social work. Journal of Social Work Practice in the Addictions. 2010;10:433–437. [Google Scholar]
- Riggs PD. Treating adolescents for substance abuse and comorbid psychiatric disorders. Science & Practice Perspectives. 2003;2(1):18–29. doi: 10.1151/spp032118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rowan AB. Adolescent substance abuse and suicide. Depression and Anxiety. 2001;14(3):186–191. doi: 10.1002/da.1065. [DOI] [PubMed] [Google Scholar]
- Shaffer D, Gould M, Fisher P, Trautman P, Moreau D. Psychiatric diagnosis in child and adolescent suicide. Archives of General Psychiatry. 1996;53:339–348. doi: 10.1001/archpsyc.1996.01830040075012. [DOI] [PubMed] [Google Scholar]
- Sher L. Alcohol consumption and suicide. Quarterly Journal of Medicine. 2006;99(1):57–61. doi: 10.1093/qjmed/hci146. [DOI] [PubMed] [Google Scholar]
- Sher L, Zalsman G. Alcohol and adolescent suicide. International Journal of Adolescent Medical Health. 2005;17(3):197–203. doi: 10.1515/ijamh.2005.17.3.197. [DOI] [PubMed] [Google Scholar]
- Spirito A, Monti PM, Barnett NP, Colby SM, Sindelar H, Rohsenow DJ, … Myers M. A randomized clinical trial of a brief motivational intervention for alcohol-positive adolescents treated in an emergency department. Journal of Pediatrics. 2004;145(3):396–402. doi: 10.1016/j.jpeds.2004.04.057. [DOI] [PubMed] [Google Scholar]
- Spirito A, Sindelar-Manning H, Colby SM, Barnett NP, Lewander W, Rohsenow DJ, Monti PM. Individual and family motivational interventions for alcohol-positive adolescents treated in an emergency department: Results of a randomized clinical trial. Archives of Pediatric Adolescent Medicine. 2011;165(3):269–274. doi: 10.1001/archpediatrics.2010.296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vajda J, Steinbeck K. Factors associated with repeat suicide attempts among adolescents. Australian and New Zealand Journal of Psychiatry. 2000;34(3):437–445. doi: 10.1080/j.1440-1614.2000.00712.x. [DOI] [PubMed] [Google Scholar]
- Wu P, Hoven CW, Liu X, Cohen P, Fuller CJ, Shaffer D. Substance use, suicidal ideation and attempts in children and adolescents. Suicide and Life-Threatening Behavior. 2004;34(4):408–420. doi: 10.1521/suli.34.4.408.53733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zahl D, Hawton K. Repetition of deliberate self-harm and subsequent suicide risk: Long-term follow-up study of 11 583 patients. British Journal of Psychiatry. 2004;185:70–75. doi: 10.1192/bjp.185.1.70. [DOI] [PubMed] [Google Scholar]