Abstract
Mapping nerve deficits during a physical exam after trauma to the upper extremity can help determine not only if the brachial plexus was injured but also which nerve roots were involved. A 28-year-old male presented with simultaneous signs and symptoms of Erb’s (C5) and Klumpke’s (C8, T1) palsy, with sparing of the C6 and C7 roots. The patient presented several months ago to his local emergency room with shortness of breath, which was determined to be caused by left diaphragmatic paralysis through clinical and radiographical evidence. However, the etiology of the current nerve dysfunction in the upper extremity remained unknown. With persistent questioning and establishing the patient’s trust in the caregivers, it was revealed that the patient had attempted suicidal hanging. We describe the clinical features and the likely mechanism of injury leading to this previously unreported combination of brachial plexus injuries. The unique injuries to this patient’s brachial plexus can be explained by the sequence of events during the attempted suicidal hanging. The upper brachial plexus was injured during the initial moments where the neck was excessively stretched and the lower brachial plexus was injured due to the patient reaching up and holding himself by his arm for an extended period of time.
Keywords: Erb’s palsy, Klumpke’s palsy, Hanging injury
Core tip: This report describes a unique case in which only the upper and lower roots of the left brachial plexus were injured, sparing the C6 and C7 roots. Careful questioning revealed that the injury was caused during an attempted suicidal hanging. The damage to C5 occurred due to stretching of the neck and the damage to the C7 and C8 roots occurred after the patient reached up to free himself and hung by his arm for a period of time.
INTRODUCTION
The brachial plexus is a group of nerves from C5-T1 that provide motor and sensory innervation to the upper extremity. Injury to the brachial plexus usually results in a pattern of functional losses that indicate which region of the brachial plexus was injured. Traumatic brachial plexus injuries are the most common type of brachial plexus injury[1]. Total lesioning of the brachial plexus (C5-T1) occurs in 75% of traumatic brachial plexus injuries. Traumatic brachial plexus injuries are typically associated with motor vehicle collisions. The typical presentation of a total brachial plexus injury is the rupture of the C5 and C6 roots (distal to the dorsal root ganglia) and avulsion of C7-T1 roots (proximal to the dorsal root ganglia)[2]. It can be extrapolated from this that the lower brachial plexus is susceptible to greater injury in traumatic brachial plexus injuries.
Erb’s palsy or Erb-Duchenne palsy is an upper brachial plexus injury involving nerve roots C5 and C6. Klumpke’s palsy or Dejerine-Klumpke palsy describes injury to the lower roots (C8, T1). These are usually brought about by a specific injury mechanism resulting in stretch of either the upper plexus (due to widening of the angle between the shoulder and head) or the lower plexus (seen in hyperabduction of the arm), in a mutually exclusive manner[3].
We report a case of an initially puzzling neurological deficit consisting of both upper and lower brachial plexus injuries. We assume this is the first reported case of such a combination injury.
CASE REPORT
A young male patient was referred to the clinic with a history of weakness and numbness in his left arm. Complaints of shortness of breath when he presented to his local emergency room several months prior had prompted radiographic workup revealing slight elevation of the left hemi diaphragm. Detailed neuroimaging with MRI and MRA were normal.
On motor exam at the clinic, there was difficulty raising the left arm above the horizontal plane against resistance. Slight atrophy of both the deltoid and supraspinatus muscles along with atrophy and weakness of the hypothenar and intrinsic hand muscles of the left side were noted. Full strength and normal muscle bulk were demonstrated in the left biceps and triceps. On sensory exam, reduced sensation to light touch and pinprick were found along the upper lateral shoulder supporting left C5 nerve root involvement. In addition, sensory deficits of the ulnar aspect of the forearm, hypothenar and the fifth digit were consistent with left C8 and T1 nerve root involvement. Denervation and early regeneration potentials were also confirmed for the left C5, C8 and T1 roots at the trunk level of the brachial plexus.
The patient was initially evasive regarding the events leading up to his neurological defects. He had repeatedly denied any trauma. Serological exam did not reveal any inflammatory process. With persistent inquiry, the patient ultimately disclosed that several months ago he had attempted suicide by hanging, using a rope and jumping from height. He reported that just when the rope tightened, his neck was stretched upward. He then reached up and grabbed the rope. He remained hanging on his outstretched arm before he was able to free himself.
Conservative treatment including physical therapy was initiated, with gradual improvement of the deficits over several months. Psychological counseling and psychiatric care were established.
DISCUSSION
There are only a few case reports describing complications of hangings despite its high prevalence. One reason is the high rate of completion of this method of suicide[4]. Additionally, unless the clinician is able to develop a rapport with the patient, patients are less likely to reveal the true scenario which led to the presentation; another potential reason for under reporting.
Based on the radiographic findings and history, it was determined that partial diaphragmatic paralysis was responsible for the shortness of breath the patient experienced. Hanging has previously been shown to cause temporary bilateral diaphragmatic paralysis[5]. In addition, several other mechanisms that can give rise to shortness of breath have been reported in the literature and were considered in the differential diagnosis. Post-obstructive pulmonary edema (POPE) is a common finding in attempted hangings. Young men, such as this patient, are especially susceptible to POPE because of the greater negative intrapleural pressure that is generated in this patient group[4,6]. Lack of pulmonary opacities on radiography made this unlikely.
It is believed that the primary fatal component of suicidal hanging is not from a cervical fracture, airway compression, or sympathetic stimulation, but rather internal jugular vein and carotid artery compression. Venous and arterial compressions are then followed by airway compression that ultimately leads to global hypoxia[4,7,8]. This theory is further reinforced by cases of patients with tracheotomies completing suicide with ligatures above the tracheotomy. Perfusion with hypoxic blood has been shown to be sufficient to produce respiratory distress in animal models, which reinforces this hypothesis[8]. Deaths in attempted hangings are typically associated with respiratory failure or bronchopneumonia[4,8].
In attempted suicidal hangings that did not result in death, nerve lesions have been reported and are described as upper motor neuron lesions caused by damage to the basal ganglia due to cerebral anoxia. Patients present with muscle spasticity and hyperreflexia[9]. Nerve damage due to anoxia in this patient was ruled out during the physical exam, which showed atrophy and decreased strength in the involved muscles, indicating that the deficits were lower motor neuron type lesions. Lower motor neuron lesions without ongoing or past inflammatory episodes in a healthy individual suggests trauma. Although the patient denied any trauma during the initial encounters, it was still high on the differential diagnosis list.
Physical examination of the patient revealed left partial diaphragmatic paralysis with atrophy of the intrinsic muscles of the hand as well as the hypothenar, supraspinatus and deltoid muscles on the left side. The nerves involved in innervating these muscles were studied to determine if there was a pattern in the distribution of nerve loss that could be traced back to the brachial plexus. The diaphragm is innervated by the phrenic nerve from C3-C5. The hypothenar and intrinsic muscles of the hand are innervated by the ulnar nerve from C8-T1. The supraspinatus muscle is innervated by the suprascapular nerve from C5-C6. The deltoid muscle is innervated by the axillary nerve from C5-C6[10]. The pattern of these involved nerves indicate injuries in the distribution of the left C5, C8 and T1 nerve roots. This combination of deficits and electrophysiological findings point to a stretch injury to both the upper and lower plexus. It is noteworthy that the C7 and possibly C6 nerve roots were spared in the case described here. Therefore, it is likely the damages occurred due to successive movements during the course of the hanging attempt that stretched first the upper then the lower regions of the brachial plexus.
Figure 1 shows the likely injury mechanism that can lead to a similar clinical presentation. Tension on the upper plexus likely occurred when the neck was abruptly pulled upward by the tightening rope (Figure 1A). The survival instinct led the patient to reach up and transfer his weight to his outstretched arm, causing stretch of the lower trunk (Figure 1B).
Figure 1.
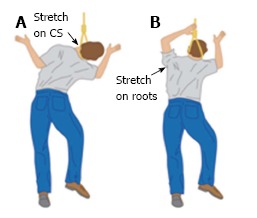
The likely injury mechanism can lead to a similar clinical presentation. A: Artist’s rendering of the upper brachial plexus stretch injury; B: Artist’s rendering of the lower brachial plexus stretch injury.
Traction injuries to the brachial plexus make up the majority of brachial plexus lesions. It is advised that the patient should be observed for up to 3-5 mo following the injury as edema should decrease and minor injuries resolve[11]. Natural recovery usually occurs within 6 mo, but recoveries without operative intervention are poorly documented[1]. As expected, this patient was also less symptomatic during subsequent follow-up appointments. Unfortunately we were unable to follow him long-term and address the physical and psychological issues completely, due to the poor compliance of the patient.
This patient’s injuries are consistent with a sequence of events resulting in first a lateral stretch of the neck followed by a stretch of the lower brachial plexus. The movements behind these injuries can be explained by the patient’s history of an attempted suicide followed by a survival response and extended period of time where the patient’s weight was suspended by his arm above his head.
ACKNOWLEDGMENTS
Authors would like to thank Mr. Bryan Moss for illustrations.
COMMENTS
Case characteristics
A young male with numbness and weakness in his left arm and previous difficulty breathing.
Clinical diagnosis
Left diaphragmatic paralysis with atrophy and weakness of the deltoid, supraspinatus, hypothenar and intrinsic hand muscles on the left side with reduced sensation to light touch and pinprick along the upper lateral shoulder, ulnar aspect of the forearm, hypothenar and the fifth digit.
Differential diagnosis
Brachial plexus trauma, nerve impingement.
Laboratory diagnosis
Serological studies did not reveal inflammatory processes.
Imaging diagnosis
Radiographic workup showed slight elevation of the left hemi diaphragm and magnetic resonance imaging/magnetic resonance angiography neuroimaging showed no abnormalities.
Treatment
Conservative treatment including physical therapy was initiated and psychological counseling and psychiatric care were established.
Related reports
To our knowledge, this is the first case report to describe both Erb’s and Klumpke’s palsy resulting from a suicidal hanging attempt.
Term explanation
Erb-Duchenne palsy refers to damage of the C5 and C6 nerve roots resulting in sensory and motor deficits in the distribution of commonly the suprascapular, musculocutaneous and axillary nerves. Dejerine-Klumpke palsy refers to damage of the C8 and T1 nerve roots resulting in sensory and motor deficits in the distribution of the ulnar nerve. Post-obstructive pulmonary edema is negative pressure, non-cardiogenic pulmonary edema that can occur during (type I) or after relief of (type II) a pulmonary obstruction.
Experiences and lessons
This case presents a unique distribution of nerve damage after attempted suicidal hanging that we do not believe has been previously described.
Peer-review
This is an interesting case of a combined upper and lower brachial plexus injury associated with an attempted suicide.
Footnotes
P- Reviewer: Lavranos GM S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
Institutional review board statement: This article meets the case report publication criteria, ethics requirements of Scott and White Health Care Temple, TX, United States.
Informed consent statement: Our institution does not need patient consent to publish a single case.
Conflict-of-interest statement: I am attaching a letter indicating that there aren’t any conflicts of intersts.
Open-Access: This article is an open-access article which was selected by an in-house editor and fully peer-reviewed by external reviewers. It is distributed in accordance with the Creative Commons Attribution Non Commercial (CC BY-NC 4.0) license, which permits others to distribute, remix, adapt, build upon this work non-commercially, and license their derivative works on different terms, provided the original work is properly cited and the use is non-commercial. See: http://creativecommons.org/licenses/by-nc/4.0/
Peer-review started: November 11, 2014
First decision: January 12, 2015
Article in press: August 14, 2015
References
- 1.Bromberg MB. Brachial Plexus Syndromes. UpToDate. Available from: http://www.uptodate.com/contents/brachial-plexus-syndromes.
- 2.Sakellariou VI, Badilas NK, Mazis GA, Stavropoulos NA, Kotoulas HK, Kyriakopoulos S, Tagkalegkas I, Sofianos IP. Brachial plexus injuries in adults: evaluation and diagnostic approach. ISRN Orthop. 2014;2014:726103. doi: 10.1155/2014/726103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jennett RJ, Tarby TJ, Krauss RL. Erb’s palsy contrasted with Klumpke’s and total palsy: different mechanisms are involved. Am J Obstet Gynecol. 2002;186:1216–1219; discussion 1219-1220. doi: 10.1067/mob.2002.123743. [DOI] [PubMed] [Google Scholar]
- 4.Berdai AM, Labib S, Harandou M. Postobstructive pulmonary edema following accidental near-hanging. Am J Case Rep. 2013;14:350–353. doi: 10.12659/AJCR.889415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Le Coz A, Laurent JF, Guivarch G, Coëtmeur D, Bousser J. [Temporary bilateral diaphragmatic paralysis after hanging. Management by mechanical nasal ventilation] Presse Med. 1992;21:269. [PubMed] [Google Scholar]
- 6.Herrick IA, Mahendran B, Penny FJ. Postobstructive pulmonary edema following anesthesia. J Clin Anesth. 1990;2:116–120. doi: 10.1016/0952-8180(90)90064-a. [DOI] [PubMed] [Google Scholar]
- 7.Nair S, Jacob J, Aaron S, Thomas M, Joseph M, Alexander M. Pulmonary distress following attempted suicidal hanging. Indian J Med Sci. 2009;63:53–57. [PubMed] [Google Scholar]
- 8.Fischman CM, Goldstein MS, Gardner LB. Suicidal hanging. An association with the adult respiratory distress syndrome. Chest. 1977;71:225–227. doi: 10.1378/chest.71.2.225. [DOI] [PubMed] [Google Scholar]
- 9.Kalita J, Mishra VN, Misra UK, Gupta RK. Clinicoradiological observation in three patients with suicidal hanging. J Neurol Sci. 2002;198:21–24. doi: 10.1016/s0022-510x(02)00056-4. [DOI] [PubMed] [Google Scholar]
- 10.Kattan AE, Borschel GH. Anatomy of the brachial plexus. J Pediatr Rehabil Med. 2011;4:107–111. doi: 10.3233/PRM-2011-0163. [DOI] [PubMed] [Google Scholar]
- 11.Bhandari PS, Maurya S. Recent advances in the management of brachial plexus injuries. Indian J Plast Surg. 2014;47:191–198. doi: 10.4103/0970-0358.138941. [DOI] [PMC free article] [PubMed] [Google Scholar]


