Abstract
Objective
To describe similarities and differences in the number of civilian traumatic brain injury (TBI)-related hospitalizations and emergency department visits between national databases that capture US hospital data.
Participants
TBI-related hospitalizations included in the National Hospital Discharge Survey (NHDS) and Healthcare Cost and Utilization Project Nationwide Inpatient Sample (HCUP-NIS) and emergency department visits in the National Hospital Ambulatory Medical Care Survey (NHAMCS) and HCUP Nationwide Emergency Department Sample (HCUP-NEDS) for 2006–2010.
Design
Cross-sectional design.
Main Measures
Nationwide counts of TBI-related medical encounters.
Results
Overall, the frequency of TBI is comparable when comparing NHDS with HCUP-NIS and NHAMCS with HCUP-NEDS. However, annual counts in both NHDS and NHAMCS are consistently unstable when examined in smaller subgroups, such as by age group and injury mechanism. Injury mechanism is consistently missing from many more records in NHDS compared with HCUP-NIS.
Conclusion
Given the large sample size of HCUP-NIS and HCUP-NEDS, these data can offer a valuable resource for examining TBI-related hospitalization and emergency department visits, especially by subgroup. These data hold promise for future examinations of annual TBI counts, but ongoing comparisons with national probability samples will be necessary to ensure that HCUP continues to track with estimates from these data.
Keywords: emergency department visits, epidemiology, hospitalizations, traumatic brain injury
Traumatic brain injury (TBI) is an important public health problem in the United States. While most people recover, many experience lifelong disability or death as a result of TBI. Traumatic brain injury can result from a number of mechanisms, including, but not limited to, falls, motor vehicle crashes, and assault.1 Knowledge of the mechanisms by which TBIs occur in the population is important, as it drives TBI-related prevention efforts focusing on mechanism-based approaches. Characterizing the trends and major causes of TBI as well as the demographic characteristics of those affected is important for developing targeted TBI-related interventions. In addition, trends of TBI incidence are important measures by which to evaluate and monitor the effectiveness of TBI-related primary prevention efforts.
National estimates of TBI-related hospitalizations and ED visits provided by the Centers for Disease Control and Prevention (CDC) typically have been based on data from the National Hospital Discharge Survey (NHDS) and the National Hospital Ambulatory Medical Care Survey (NHAMCS), respectively.1,2 Although these data sources have provided stable overall estimates of TBI-related hospitalizations and ED visits, the relatively small samples have not permitted stable estimates by specific subgroups such as age and external mechanism of injury for individual years. As a result, previous estimates of the number of annual TBIs were calculated using average annual counts of TBI-related hospitalizations and ED visits from 5-year spans of data to increase the stability of the estimates for population subgroups. For example, the most recent in-depth national-level study on the frequency of TBI-related medical encounters, released by CDC in 2010, included hospitalization and ED visit data from NHDS and NHAMCS for years 2002–2006.1 Pooled years of data were required to achieve stability for stratified annual estimates.1
Using annual averages from pooled years of data can obscure year-to-year trends. A recent rise in TBI-related ED visits demonstrates the need to look more carefully at annual data in order to be able to more quickly respond to emergent trends in the causes of TBI.1,3 National Hospital Ambulatory Medical Care Survey frequently does not provide stable annual estimates when estimates are stratified by relevant demographic characteristics. Consequently, stable annual estimates of TBI-related medical encounters, stratified by relevant demographic characteristics, are needed to better target public health interventions in a timely manner.
To provide more stable annual estimates of TBI subgroups, we explored the possibility of using data sets from the Healthcare Cost and Utilization Project (HCUP) managed by the US Agency for Healthcare Research and Quality. The goal of this study was to examine the feasibility of using HCUP databases to produce annual counts of TBI-related hospitalizations and ED visits. Data on TBI-related deaths, also included in national estimates of TBI,1,2 come from the National Vital Statistics System. National Vital Statistics System is the standard for multiple cause-of-death data in the United States and will not be further described in this article.
METHODS
Case definitions
Cases of TBI were identified using the CDC’s TBI surveillance definition based on codes from the International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM).4 Specifically, cases were classified as a TBI where codes indicated skull fractures (codes 800–801, 803–804); intracranial injury, including concussion, contusion, laceration, and hemorrhage (850.0–854.1); injury to optic nerve and pathways (950.1–950.3); shaken baby syndrome (995.55); or unspecified head injury (959.01). Only records indicating TBI as any one of the listed diagnoses on a hospitalization or ED visit record were selected for analysis.
The mechanisms of TBI were defined by categories previously utilized by CDC to classify external causes of TBI using ICD-9-CM-based external cause of injury codes (E-codes).5 Mechanisms identified included motor vehicle traffic crashes (E810–E819); falls (E880–E886, E888, E987); strikes by or against an object (E916–E917); intentional injury, including assault and self-harm (E960–E969); and other and unspecified injuries (all other E-codes). Records may have several mechanisms of injury (E-codes) listed. Because the first-listed E-code should correspond to the most serious diagnosis,6 for purposes of this analysis, only the first-listed valid E-code was used in the analysis, and this code was assumed to be the principal mechanism of injury for the TBI. Valid E-codes are those that are correct in syntax (ie, they exist as collected within ICD-9-CM) and which describe a mechanism of injury rather than an activity or place of occurrence.
Hospitalizations
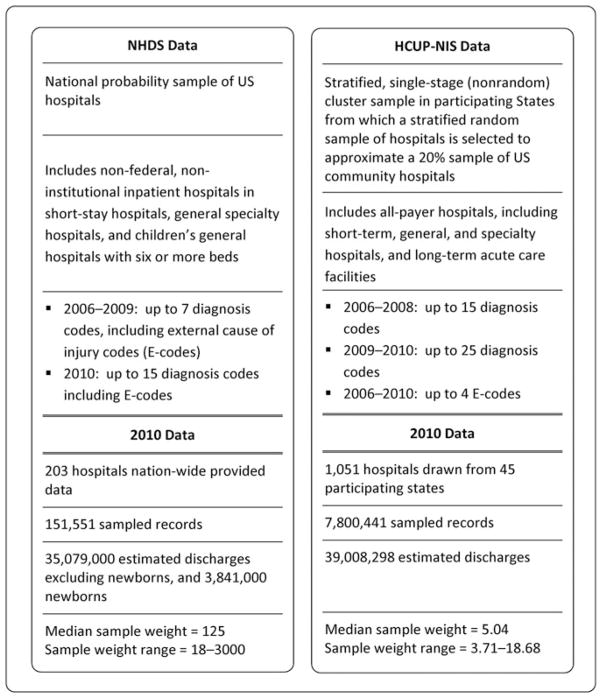
National Hospital Discharge Survey is a national probability sample survey conducted by the CDC’s National Center for Health Statistics gathering data on hospitalizations from more than 150 000 sample records in 2010 (see Figure 1). National Hospital Discharge Survey includes data from inpatient hospital discharges within the 50 States and the District of Columbia. Hospitals with average lengths of stay of 30 days or greater for all patients, hospitals with fewer than 6 beds staffed for patient use, and institutional, Federal, military, and Veterans Health Administration hospitals are excluded from the NHDS sample. For years 1988–2007, NHDS was a sample of approximately 270 000 inpatient hospitalization records from about 500 hospitals annually.7 For data collected in 2008–2010, the sample was reduced to 239 hospitals though not all sampled hospitals necessarily contribute to NHDS every year.7 The maximum number of diagnoses recorded as part of each record varies by year and ranges from 7 to 15 for the years included in this analysis.
Figure 1.
Characteristics of the NHDS and the HCUP-NIS. HCUP-NIS indicates Healthcare Cost and Utilization Project Nationwide Inpatient Sample; NHDS, National Hospital Discharge Survey.
National Hospital Discharge Survey data from 2006 through 2010 were included in the analysis. Centers for Disease Control and Prevention typically combines TBI-related hospitalizations, ED visits, and deaths for estimates of TBI. For each year, hospitalized patients who died during hospitalization or were transferred from another hospital were excluded from the analysis. These exclusions were done to reduce double counting as 2 hospitalizations in NHDS or as both a hospitalization in NHDS and a death in National Vital Statistics System when counts of TBI-related hospitalizations and deaths from National Vital Statistics System are summed. Because NHDS is discharge-level data and not patient-level data, there undoubtedly remains the potential for double counting of records, especially from persons who seek care multiple times for a single injury.
The Nationwide Inpatient Sample (HCUP-NIS), managed as part of the HCUP, is the largest publicly available all-payer hospitalization database containing data from approximately 8 million hospital stays in 2010 (Fig 1). Begun in 1988, HCUP-NIS is drawn from only those states participating in HCUP. The 2010 HCUP-NIS collected data from 45 states that include more than 95% of all discharges in the United States, though these States are not individually identifiable in the HCUP-NIS data.8,9 Unlike NHDS, HCUP-NIS is not a random sample of US hospitals but rather a stratified single-stage cluster sample—from participating hospitals in participating states—from which a random sample of hospitals is selected. All discharges from the selected hospitals are included in HCUP-NIS.9 In addition, some states impose restrictions on which hospitals can be included in HCUP-NIS.9 Like NHDS, the maximum number of diagnoses collected as part of each record varies by year, from 15 to 25 for the years examined, with all years including up to 4 external cause of injury codes (E-codes). The 2012 HCUP-NIS has been redesigned, so characteristics discussed in this manuscript may not be applicable to future data releases.
HCUP-NIS data for years 2006–2010 were analyzed. Hospitalized patients who died during hospitalization, were transferred from another hospital or readmitted from another unit, or were transferred from a different hospital were excluded from this analysis in an attempt to reduce double counting of admissions.
ED visits
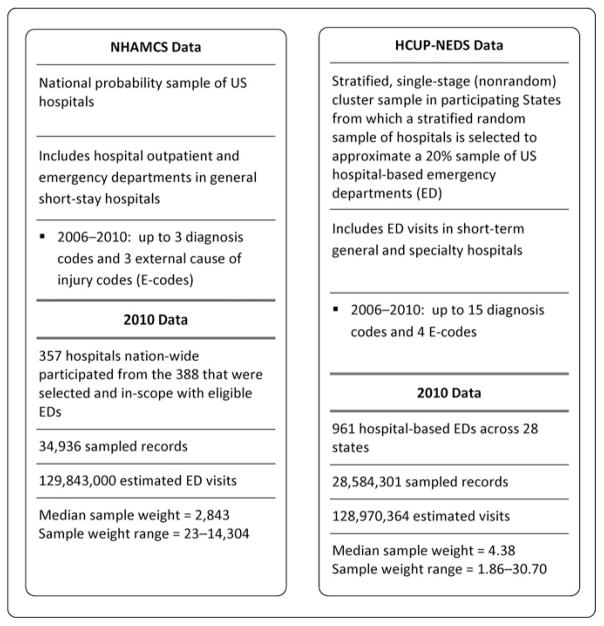
National Hospital Ambulatory Medical Care Survey, a national probability survey conducted by the CDC’s National Center for Health Statistics, includes data from visits to hospital outpatient and emergency departments located in noninstitutional general and short-stay hospitals, excluding Federal, military, and Veterans Health Administration hospitals, located in the 50 states and the District of Columbia (see Figure 2). While NHAMCS includes data from outpatient department visits, this analysis includes records identified only as ED visits. The 2010 NHAMCS included data from nearly 35 000 sampled records of emergency and outpatient department visits.10 For 2006–2010, the maximum number of diagnoses recorded was 3 plus up to 3 E-codes.
Figure 2.
Characteristics of the NHAMCS and the HCUP-NEDS. ED indicates emergency department; HCUP-NEDS indicates Healthcare Cost and Utilization Project Nationwide Emergency Department Sample; NHAMCS, National Hospital Ambulatory Medical Care Survey.
National Hospital Ambulatory Medical Care Survey data from 2006 through 2010 were included in the analysis. To reduce double counting, patients who may have been transferred between sampled hospitals were excluded from the analysis. Admissions which resulted from ED visits were excluded as they may be counted as hospitalizations. Deaths in the ED were excluded, as well, as these events would be included in TBI-related mortality statistics when counts for TBI-related ED visits, hospitalizations, and deaths are summed together to create the TBI estimates typically used by CDC. As with all of the other data sets examined, NHAMCS is visit-level data and not patient-level data; therefore, the potential for double counting of records remains, especially from persons who seek care multiple times.
HCUP National Emergency Department Sample (HCUP-NEDS) is the largest all-payer ED database in the United States, containing more than 28 million records in 2010. Like HCUP-NIS, HCUP-NEDS is a not random sample of US hospitals but rather a stratified single-stage cluster sample in which all discharges are selected from a stratified sample of hospitals (clusters) in participating States. In addition, some states impose restrictions on which data are included in HCUP-NEDS.11 Designed to approximate a 20% stratified sample of US hospital-based EDs, its sampling frame consists of non-Federal, short-term, general, and other specialty hospitals in each of the participating states (Fig 2). HCUP-NEDS was constructed drawing records from the HCUP state-based ED and inpatient visit data sets and includes ED visit data for visits in which the patient was treated and released, was admitted to the same hospital, transferred to another short-term hospital, died in the ED, or was discharged alive but to an unknown destination. In 2010, HCUP-NEDS sampled data from 28 states; these states included 66.7% of the US population and 64.8% of all ED visits.11 As with HCUP-NIS, states are not individually identifiable in the HCUP-NEDS data.11 For 2006–2010, the maximum number of diagnoses recorded was 15 plus up to 4 E-codes.
HCUP-NEDS for years 2006–2010 was analyzed. Records that indicated that a patient died, was hospitalized, or transferred to another hospital were excluded from this analysis in an attempt to reduce double counting.
Sampling weights
Records within each data source were weighted. The weight applied to each record is a complex combination of factors related to probabilities of sample selection, nonresponse, and population weighting ratios.9,11–13 NHDS and NHAMCS are national probability samples, so the weighted estimates are generalizable to the US population. The HCUP-NIS and HCUP-NEDS are drawn from samples from states participating in HCUP. The weighting is done to approximate what would be obtained from a probability sample. Larger sampling weights are required to approximate a nationally representative sample when the number of hospitals sampled is relatively small, which can result in unstable estimates that are more likely to fluctuate over time. In addition, a single record could be weighted to represent hundreds of weighted cases, so a change in 1 or 2 additional records could have a significant effect on the total weighted estimate. The range in sampling weights for all 4 data sources was described (Figs 1 and 2), as these weights affect the ability to provide stable annual estimates.
Data analyses
A comparability ratio (CR) was calculated to quantify differences between both TBI-related hospitalizations (NHDS and HCUP-NIS) and ED visits (NHAMCS and HCUP-NEDS). The CR is the ratio of the weighted counts of NHDS (or NHAMCS) divided by the weighted counts of HCUP-NIS (or HCUP-NEDS) for overall totals and subgroups; 95% confidence intervals (CIs) were calculated using the method proposed by Kish to compute the variance of a ratio estimate.14 A CR less than 1.00 indicates a smaller sum of weighted counts for a given grouping of medical encounters collected from NHDS (NHAMCS) when compared with HCUP-NIS (HCUP-NEDS). A CR greater than 1.00 indicates a larger sum of weighted counts in the NHDS (NHAMCS) data than in the HCUP-NIS (HCUP-NEDS) data. Counts were considered comparable if the 95% CI included 1.00.
Based on the complex sample design of the NHDS and NHAMCS, if the unweighted sample size was 30 to 59, the value of the estimate was reported but should not be assumed to be stable. If the unweighted sample size was less than 30, or the relative standard error was more than 30% regardless of the unweighted sample size, the corresponding estimate was considered unstable and was not reported.15 As done in previously published HCUP reports, HCUP data sets with relative standard errors larger than 30% or standard errors equal to zero were considered unstable and were not reported.16 Comparability ratios were not reported when one or more of the estimates used to calculate the CR were unstable or potentially unstable.
Weighted counts were compared using CRs for both hospitalization and ED visits overall by ICD-9-CM code and year-specific counts by TBI category, E-code category, and age group. In addition to the CRs, hospitalization and ED visit data sets were examined with respect to the proportion of records missing identified injury mechanisms (E-codes), sample weighting and sample size-related stability measures, demographic characteristics, and fluctuations of weighted counts across consecutive years of data.
Data were presented as annual average estimates for the years studied, though individual years of data were examined and are discussed without presented data, as appropriate.
RESULTS
Overall, annual average frequencies of TBI-related hospitalizations were comparable between NHDS and HCUP-NIS (see Table 1) for categories of sex and age group. While categories of ICD-9-CM nature of injury codes were comparable between NHDS and HCUP-NIS, estimates for shaken baby syndrome could not be compared since only estimates from HCUP-NIS were stable.
TABLE 1.
Annual average frequencies of patient characteristics for traumatic brain injury–related hospitalizations and ED visits with CRs with 95% CIs comparing data from the NHDS with the HCUP-NIS and data from the NHAMCS with the HCUP-NEDS—United States, 2006–2010
| Hospitalizations
|
ED visits
|
|||||
|---|---|---|---|---|---|---|
| NHDS | HCUP-NIS | CR (95% CI) | NHAMCS | HCUP-NEDS | CR (95% CI) | |
| Sex | ||||||
| Male | 172 252 | 178 941 | 0.96 (0.87–1.06) | 1 020 043 | 983 147 | 1.04 (0.90–1.17) |
| Female | 116 910 | 114 454 | 1.02 (0.93–1.11) | 774 774 | 824 902 | 0.94 (0.81–1.07) |
| Unknown | 1249 | a | ||||
| Age group | ||||||
| 0–4 y | 13 382 | 11 341 | 1.18 (0.90–1.46) | 343 789 | 262 614 | 1.31 (1.07–1.55)b |
| 5–14 y | 13 475 | 12 219 | 1.10 (0.86–1.34) | 289 743 | 253 826 | 1.14 (0.91–1.38) |
| 15–24 y | 40 673 | 41 663 | 0.98 (0.83–1.12) | 364 665 | 372 139 | 0.98 (0.83–1.13) |
| 25–44 y | 59 687 | 59 391 | 1.00 (0.87–1.14) | 340 808 | 378 367 | 0.90 (0.75–1.06) |
| 45–64 y | 64 970 | 65 303 | 0.99 (0.88–1.11) | 242 524 | 269 489 | 0.90 (0.76–1.04) |
| 65+ y | 96 974 | 104 193 | 0.93 (0.85–1.01) | 213 288 | 272 280 | 0.78 (0.64–0.92)b |
| Age not specified | 534 | 171 | ||||
| ICD-9-CM nature of injury code range | ||||||
| 800–801, 803–804 (fractures of the skull) | 64 492 | 63 049 | 1.02 (0.89–1.16) | 30 223c | 41 162 | d |
| 850.0–854.1 (intracranial injury) | 190 831 | 197 648 | 0.97 (0.87–1.06) | 419 962 | 540 691 | 0.78 (0.65–0.90)b |
| 995.55 (shaken baby syndrome) | e | 470 | d | 242 | ||
| 959.01 (unspecified head injury) | 35 548 | 36 676 | 0.97 (0.85–1.09) | 1 383 410 | 1 251 376 | 1.11 (0.95–1.26) |
| Totalf | 289 162 | 294 644 | 0.98 (0.90–1.06) | 1 794 817 | 1 808 886 | 0.99 (0.87–1.11) |
Abbreviations: CI indicates confidence interval; CR, comparability ratio; ED, emergency department; HCUP-NEDS, Healthcare Cost and Utilization Project Nationwide Emergency Department Sample; HCUP-NIS, Healthcare Cost and Utilization Project Nationwide Inpatient Sample; ICD-9-CM, International Classification of Diseases, Ninth Revision, Clinical Modification; NHAMCS, National Hospital Ambulatory Medical Care Survey; NHDS, National Hospital Discharge Survey.
The relative standard error was more than 30% or the standard error = 0; the value of the estimate was considered unreliable and was not reported.
The 95% confidence interval did not include 1. Estimates were not comparable between data sets.
Sample size was 30–59; the value of the estimate was reported but should not be assumed reliable.
Comparability ratios were not calculated if estimate was considered unreliable or potentially unreliable.
Sample size was less than 30 or the relative standard error was more than 30%; the value of the estimate was considered unreliable and was not reported.
Category-level code counts do not directly sum to the total counts, as records may include more than 1 traumatic brain injury–related diagnosis. Total counts include optic nerve injuries that were rare and present only in HCUP-NIS and HCUP-NEDS.
Annual average frequencies for TBI-related ED visits were mostly comparable between NHAMCS and HCUP-NEDS, though a few aberrations were present. Sex-stratified estimates were comparable. Estimates in both the youngest age group (0–4 years) and the oldest age group (≥65 years) were not comparable between NHAMCS and HCUP-NEDS, though all other age groups were comparable (Table). Comparing HCUP-NEDS with NHAMCS, the estimate for TBI-related ED visits was 31% higher in those aged 0 to 4 years (CR, 1.31; 95% CI, 1.07–1.55) and lower in persons 65 years and older (CR, 0.78; 95% CI, 0.64–0.92).
Traumatic brain injuries were examined within nature of injury code categories (skull fracture, intracranial injury, etc). The NHAMCS estimate of skull fractures present in ED visits was unstable preventing the calculation of a CR (Table). In addition, NHAMCS produced a lower number of intracranial injuries than HCUP-NEDS (CR, 0.78; 95% CI, 0.65–0.90). Data for shaken baby syndrome were unstable for estimates from both NHDS and NHAMCS but stable for those produced by HCUP-NIS and HCUP-NEDS.
When examined at the individual ICD-9-CM code level, data from HCUP data sources were more frequently stable than those from NHDS and NHAMCS. In fact, there was no instance in which HCUP data were unstable, but the corresponding nature of injury code was stable in either NHDS or NHAMCS. In contrast, there were many instances—especially in less common diagnosis categories—in which HCUP data were stable but both NHDS and NHAMCS data could not be presented because of stability or did not contain any cases on which to base estimates (data not presented).
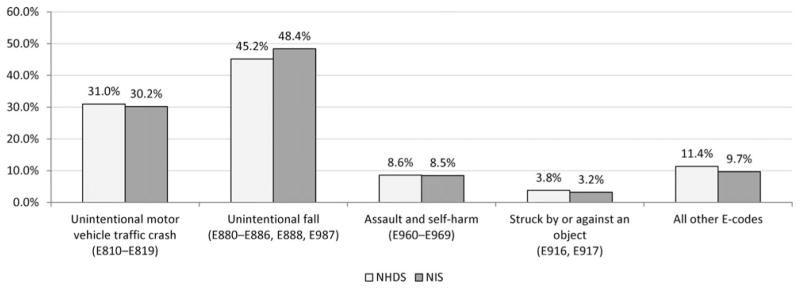
The frequencies of TBI-related hospitalizations by mechanism of injury (eg, motor vehicle crashes, falls, etc) were not statistically compared across the 2 data sources because of the large number of the NHDS records having no E-code specifying an external cause of injury. In fact, after applying statistical weights, 43.9% of the NHDS hospitalizations, on average for 2006–2010, had no E-codes compared with 11.0% of HCUP-NIS. However, when examining only those records with valid E-codes, the proportions of mechanism categories were comparable between NHDS and HCUP-NIS (see Figure 3).
Figure 3.
Annual average percent distribution of injury mechanisms among traumatic brain injury–related hospitalization records with valid external cause of injury codes (E-codes) comparing data from the NHDS with the HCUP-NIS—United States, 2006–2010. HCUP-NIS indicates Healthcare Cost and Utilization Project Nationwide Inpatient Sample; NHDS, National Hospital Discharge Survey.
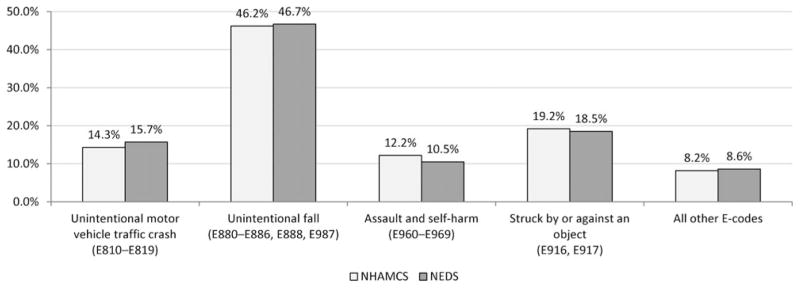
In contrast, E-codes examining external causes of TBI in ED visits could be examined because of the comparable ratios of missing E-code data (5.7% and 6.6% in NHAMCS and HCUP-NEDS, respectively). When examined, NHAMCS and HCUP-NEDS had comparable estimates for all categories examined: unintentional motor vehicle traffic crash (CR, 0.91; 95% CI, 0.75–1.08), unintentional fall (CR, 0.99; 95% CI, 0.86–1.12), assault and self-harm (CR, 1.16; 95% CI, 0.94–1.38), struck by or against an object (CR, 1.04; 95% CI, 0.84–1.24), and all other specified mechanisms (CR, 0.95; 95% CI, 0.74–1.16). Weighted estimates of TBI-related ED visits by external mechanism of injury included a similar proportion of the ED visits with missing valid E-codes for NHAMCS (5.7%) and HCUP-NEDS (6.6%) (CR, 0.85; 95% CI, 0.55–1.15). Proportions of mechanism of injury categories were comparable when those with valid E-codes were compared (see Figure 4).
Figure 4.
Annual average percent distribution of injury mechanisms among traumatic brain injury–related emergency department visit records with valid external cause of injury codes (E-codes) comparing data from the NHAMCS with the HCUP-NEDS—United States, 2006–2010. HCUP-NEDS indicates Healthcare Cost and Utilization Project Nationwide Emergency Department Sample; NHAMCS, National Hospital Ambulatory Medical Care Survey.
When examining data stratifications (eg, sex, age group, nature of injury category) by individual year, for all instances of unstable HCUP estimates, estimates from NHDS and NHAMCS were also unstable or absent due to a lack of cases present in the data source (data not presented). With respect to TBI-related hospitalizations, annual estimates from HCUP-NIS had many fewer unstable estimates when examined by subgroups of nature and mechanism of injury, age group, and sex compared to NHDS (data not presented). Similarly, many more annual estimates from HCUP-NEDS were stable compared with NHAMCS when stratified into similar subgroups (data not presented).
DISCUSSION
Comparisons between the data sources for TBI-related hospitalizations (NHDS and HCUP-NIS) and ED visits (NHAMCS and HCUP-NEDS) demonstrate that the different sources were generally comparable for overall average estimates for 2006–2010 as well as estimates for most categories of age, sex, nature of injury, and external cause of injury. While some estimates for the oldest and youngest ages with ED visits were not comparable, wide fluctuations observed between individual years of data within NHAMCS—possibly due to larger sample weights—may have contributed to these divergent averages and subsequent CRs. HCUP-NIS and HCUP-NEDS data sources provided fewer instances of unstable estimates within single year examinations. All unstable HCUP estimates were also considered unstable in NHDS or NHAMCS for all examined subgroups of demographics and injury characteristics. While the overall estimates are comparable, HCUP-NIS and HCUP-NEDS provide better sources for examining stable and reliable year-to-year trends.
Because only a few hundred thousand TBI-related hospitalizations occur each year, it is important that weighted estimates are stable to adequately describe subgroups of the population with these injuries. The larger sample size of the HCUP data sets allows for smaller sample weights, which results in an increased ability to provide stable annual estimates of TBI overall and within subgroups, including smaller age groups and more descriptive categories of external mechanism of injury. More stable estimates can also allow for an increased ability to examine up to 5-digit codes, which can describe important features of TBI-related injury such as length of loss of consciousness. In addition, HCUP can provide an increased ability to detect rare TBI-related diagnoses, such as shaken baby syndrome.
In addition to improved stability of estimates, the frequency of the inclusion of E-codes as part of the record is an important distinction between NHDS and HCUP-NIS. Over the years studied, NHDS consistently had 2.5-times more records with missing E-codes than HCUP-NIS records. For ED visits, the percentage of records with missing E-codes was comparable. National Hospital Discharge Survey records do contain a smaller maximum number of diagnosis codes than HCUP-NIS and do not collect E-codes separately from diagnosis codes as HCUP-NIS does, and this may contribute to these differences as well as the varying requirements of states with respect to E-code reporting.17 Regardless, having a more precise breakdown of how TBIs occur, through a specified mechanism of injury, is an important piece of information for TBI prevention efforts. The limited inclusion of diagnostic codes in NHDS and NHAMCS (7 and 3 diagnostic codes collected in 2010, respectively) may limit the ability to detect TBIs if more serious injuries are described with diagnostic codes in those limited number of spaces/variables.
Although annual estimates of TBI-related hospitalizations and ED visits, using NHDS and NHAMCS data, were feasible for overall TBI counts and for stratification into large subgroups, such as sex,1 stratification by many of the subgroups, such as age group and external cause of injury, resulted in unstable estimates. This poses an important limitation to public health practitioners who rely on stratification by factors such as age, sex, and external cause of injury to develop targeted interventions. In addition, annual estimates allow public health professionals involved in prevention efforts to better monitor changes in TBI-related ED visits and hospitalizations and more quickly determine trends that can be used to target prevention efforts. While 5-year trends do provide informative data, an annual estimate allows for earlier identification of trends and a more rapid and targeted public health response, when needed. In 2010, the NHDS was discontinued. Beginning in 2011, inpatient stay data will be collected as part of the National Hospital Care Survey.7 As the methodology and sampling for NHCS differs from NHDS, it is important to note that the results of the comparisons presented in this article do not apply to NHCS, but this emerging data source can be evaluated when it is available.
This examination of TBI-related hospitalizations and ED visits is limited because of the inherent limitations of administrative data, such as NHDS and HCUP. Diagnoses abstracted from these sources are based on hospital reports for billing purposes and are not specifically designed for public health surveillance, while NHAMCS data are compiled from ED patient medical records and coded by NCHS. The data quality of discharge disposition and admission source was not examined in this analysis, so the ability to reduce double counting using these sources may be limited. All data sources examined are discharge- or visit-level data meaning that a person may seek treatment at multiple providers and have multiple records (discharges or visits) included in these databases for a single TBI. Exclusion criteria are applied to reduce double counting of these records, but there are most likely some included, as the discharge-level data used in this analysis do not allow for the exclusion of patients who present for care multiple times for a single injury. Furthermore, persons may have incurred multiple, isolated TBIs and sought care for each in individual medical encounters. This analysis cannot exclude these persons, and population estimates may be affected by the inclusion of these individual patients multiple times. Diagnoses included as part of the hospital record can be affected by billing policies and practices of healthcare providers as well as laws and policies governing billing and payer requirements. These practices could affect the quality and accuracy of the data for all 4 data sources. In addition, the use of these healthcare encounter data for examination of TBI inherently precludes counting of persons who do not seek care for treatment of a TBI or who receive care in an outpatient setting outside of an ED visit. Injury-related severity and outcomes are not available as part of these data, thereby limiting their description in this work. In addition, patients may have more than 1 injury, and TBI may not be the primary reason for seeking care. This may have impacted the collection of TBI as a diagnosis by the varying surveys because the number of diagnoses collected by each varied. In spite of these limitations, the use of administrative databases has been found to be useful for monitoring trends and characterizing common injury characteristics across states to set priorities for prevention.18 Finally, this evaluation compared data for the selected 5-year period, though it is possible that data from years of data outside this analysis may not be as comparable, especially for prior years of data for which fewer states may have participated in HCUP. Additional benchmarking for other years of data is appropriate and should be done to ensure that the comparability between HCUP-NIS and HCUP-NEDS and national probability samples remains acceptable over time.
Given the large sample size of the HCUP-NIS and HCUP-NEDS, these data can provide a useful resource for examining TBI-related hospitalization and ED visits. While all 4 data sources studied allowed for stable annual estimates of total TBI-related hospitalizations and ED visits, only HCUP-NIS and HCUP-NEDS provided stable annual estimates by demographic (eg, age and sex) and injury (nature and mechanism) subgroups within all stratifications examined. While NHAMCS data are drawn from a nationwide sample of EDs, HCUP-NEDS is sampled from only 28 participating states, which may limit its representativeness in describing national level TBI-related medical encounters. In addition, because HCUP-NIS and HCUP-NEDS are not random samples and do not sample from every state, it is unclear whether the estimates provided are biased, especially for discharge or visit characteristics not examined in this analysis. However, because the vast majority of the estimates provided by HCUP data are comparable with those produced by NHDS and NHAMCS, it lends credibility to the use of HCUP for analysis of TBI in subgroups where NHDS and NHAMCS estimates are not stable. However, comparing HCUP data to national probability samples is appropriate, especially given only 28 states provided data to HCUP-NEDS in 2010 and may be more affected by variations in data within non-represented states. Because of the recent annual trend of increasing numbers of TBI-related ED visits, it is important to examine characteristics of this seeking treatment in order to better understand this trend and describe its annual change. Conversely, the use of HCUP data may offer no advantage over NHDS or NHAMCS when calculating overall counts without regard to population demographics or when data pooling is purposeful, such as when determining multiyear cumulative incidence, though these scenarios were not directly examined in this study.
While CDC has traditionally used NHDS and NHAMCS data for providing national-level estimates of TBI in the United States, comparisons of HCUP-NIS and HCUP-NEDS with NHDS and NHAMCS, respectively, demonstrates that HCUP has also produced stable national estimates of TBI-related hospitalizations and ED visits. With HCUP, larger sample size and relatively smaller sample weights allow for the calculation of stable annual estimates, by demographic group, without the pooling of multiple years of data. Although the estimates examined are at a national level, states can compare their data with national trends to further help them target interventions. Although there are limitations to these data, HCUP data allow the examination of TBI-related trends on an annual basis. With the considerable increase in the number of TBI-related ED visits over recent years, it is important to monitor these yearly trends to identify the groups at highest risk as well as describe the most common causes of TBI. In addition, HCUP-NIS has the added benefit of having more complete E-coding of records than NHDS. These data hold promise for future examinations of annual TBI counts in the United States, but ongoing comparisons with national probability samples will be necessary to ensure that HCUP continues to track with estimates from these data.
Acknowledgments
The authors gratefully acknowledge J. Lee Annest for his insight during the drafting of this manuscript.
Footnotes
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
The authors declare no conflicts of interest.
References
- 1.Faul M, Xu L, Wald MM, Coronado VG. Traumatic Brain Injury in the United States: Emergency Department Visits, Hospitalizations, and Deaths 2002–2006. Atlanta, GA: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2010. [Google Scholar]
- 2.Langlois J, Rutland-Brown W, Thomas K. Traumatic Brain Injury in the United States: Emergency Department Visits, Hospitalizations, and Deaths. Atlanta, GA: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2006. [Google Scholar]
- 3.Coronado VG, McGuire LC, Sarmiento K, et al. Trends in traumatic brain injury in the U.S. and the public health response: 1995–2009. J Safety Res. 2012;43(4):299–307. doi: 10.1016/j.jsr.2012.08.011. [DOI] [PubMed] [Google Scholar]
- 4.Marr A, Coronado V, editors. Central Nervous System Injury Surveillance Data Submission Standards—2002. Atlanta, GA: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2004. [Google Scholar]
- 5.Centers for Disease Control and Prevention. Recommended framework for presenting injury mortality data. MMWR Morb Mortal Wkly Rep. 1997;46(RR-14):1–30. [PubMed] [Google Scholar]
- 6.Centers for Medicare & Medicaid Services, Statistics NCfH. ICD-9-CM official guidelines for coding and reporting. [Accessed August 4, 2014];Effective. 2011 Oct 1; http://www.cdc.gov/nchs/data/icd/icd9cm_guidelines_2011.pdf.
- 7.Centers for Disease Control and Prevention. [Accessed November 4, 2013];About the hospital care surveys. http://www.cdc.gov/nchs/nhds/about_nhds.htm.
- 8.Pfuntner A, Wier LM, Elixhauser A. Overview of hospitals stays in the United States. [Accessed September 18, 2014];HCUP Statistical Brief #144. 2010 http://www.hcup-us.ahrq.gov/reports/statbriefs/sb144.pdf. Published 2012.
- 9.Agency for Healthcare Research and Quality. [Accessed December 5, 2013];Introduction to the 2010 HCUP Nationwide Inpatient Sample (NIS) http://www.hcup-us.ahrq.gov/db/nation/nis/NIS_Introduction_2010.jsp. Published 2012.
- 10.National Hospital Ambulatory Medical Care Survey. Public-Use Data File Documentation: 2010. Hyattsville, MD: Centers for Disease Control and Prevention National Center for Health Statistics; 2010. [Google Scholar]
- 11.Agency for Healthcare Research and Quality. [Accessed December 5, 2013];Introduction to the 2010 HCUP Nationwide Emergency Department Sample (NEDS) http://www.hcup-us.ahrq.gov/db/nation/neds/NEDS_Introduction_2010.jsp. Published 2012.
- 12.Dennison C, Pokras R. Design and operation of the National Hospital Discharge Survey: 1988 redesign. Vital Health Stat. 2000;1(39):1–42. [PubMed] [Google Scholar]
- 13.Centers for Disease Control and Prevention. [Accessed November 4, 2013];Estimation procedures. http://www.cdc.gov/nchs/ahcd/ahcd_estimation_procedures.htm.
- 14.Kish L. Survey Sampling. New York, NY: John Wiley & Sons, Inc; 1965. Unequal clusters; pp. 182–216. [Google Scholar]
- 15.National Hospital Discharge Survey. Public-Use Data File Documentation: 2010. Hyattsville, MD: Centers for Disease Control and Prevention National Center for Health Statistics; 2010. [Google Scholar]
- 16.Levit K, Ryan K, Elixhauser A, Stranges E, Kassed C, Coffey R. HCUP Facts and Figures: Statistics on Hospital-Based Care in the United States in 2005. Rockville, MD: Agency for Healthcare Research and Quality; 2007. [Google Scholar]
- 17.Barrett M, Steiner C. Healthcare Cost and Utilization Project (HCUP) External Cause of Injury Code (E Code) Evaluation Report (Updated with 2011 HCUP Data) [Accessed September 18, 2014];HCUP methods series report # 2014-01 ONLINE. http://www.hcup-us.ahrq.gov/reports/methods/2014-01.pdf. Published March 14, 2014.
- 18.Johnson RL, Thomas RG, Thomas KE, Guzman BR. State Injury Indicators Report: Fifth Edition—2006 Data. Atlanta, GA: Centers for Disease Control and Prevention, National Center for Injury Prevention and Control; 2010. [Google Scholar]