Abstract
Dyslipidemias are one of the common metabolic disorders. A link between dermatological disorders like psoriasis and dyslipidemia has been established in the recent past. Many dermatological disorders could have a systemic inflammatory component which explains such association. Chronic inflammatory dermatological disorders could also have other metabolic imbalances that may contribute to dyslipidemia. Presence of such abnormal metabolism may justify routine screening of these disorders for associated dyslipidemia and other metabolic abnormalities and early treatment of such comorbidities to improve quality of life. Some of the drugs used by dermatologists such as retinoids are also likely to be a cause of dyslipidemia. Hence, it is imperative that the dermatologists obtain scientific knowledge on the underlying mechanisms involved in dyslipidemia and understand when to intervene with therapies. A systematic review of the English language literature was done by using Google Scholar and PubMed. In this review, attempts are made to list the dermatological disorders associated with dyslipidemia; to simplify the understanding of underlying mechanisms; and to give a brief idea about the interventions.
Keywords: Corticosteroids, cyclosporine A, dermatological disorders, dyslipidemia, lichen planus, pemphigus, psoriasis, retinoids, skin, statins, xanthomas
Introduction
Dyslipidemias are disorders of lipoprotein metabolism, including lipoprotein overproduction and deficiency. These disorders may be manifested by elevation of the serum total cholesterol, low-density lipoprotein (LDL) cholesterol, and triglyceride concentrations, and a decrease in the high-density lipoprotein (HDL) cholesterol concentration.[1] Abnormal blood lipids are an increasing health problem in the world. Studies from India have shown upward trend in the prevalence of dyslipidemia, even among the young adult population.[2] Dyslipidemia plays a crucial role in the development of cardiovascular diseases, which has become the leading cause of death in most developed as well as in developing countries.[3] It is now known that dermatological disorders, such as psoriasis are associated with dyslipidemias.[4] Some of the dermatological therapies are also known to predispose to lipid abnormalities. Comprehensive understanding of the pathogenesis of such events is necessary to give appropriate advices to the patients.
In this article, we aimed to review the dermatological disorders and drugs associated with dyslipidemia, dermatological manifestations of dyslipidemia, probable underlying mechanisms and interventions, based on evaluation of the manuscripts available on PubMed and Google Scholar using the Medical Subject Headings (MeSH) terms “dyslipidemias,” “skin,” “dermatological disorders”, “therapy for dyslipidemia”, and “drugs in dermatology”.
Pathogenesis of Dyslipidemias
Dyslipidemia may result from overproduction or lack of clearance of the lipoprotein particles, or may be related to other defects in the apolipoproteins or metabolic enzyme deficiencies. The pathways and means of lipid metabolism in the human body reflect interactions of genetics, complex biochemical processes influenced by medical disorders, medications, and/or environmental factors. Phenotyping these dyslipidemias is difficult and attempts are on, since many decades.[5]
A primary dyslipidemia (e. g., familial hypercholesterolemia) typically refers to a genetic defect in the lipid metabolism that causes abnormal lipid levels. A secondary dyslipidemia may be due to a variety of reasons like environmental factors (diet rich in saturated fat or a sedentary lifestyle), diseases (type 2 diabetes, hypothyroidism, obstructive jaundice, etc.), and medications (thiazide diuretics, progestins, anabolic steroids, etc.). Secondary dyslipidemias could be corrected or ameliorated by treating the underlying disorder. Dyslipidemia can be a result of combination of both genetic and secondary causes.[5]
Dyslipidemia and Skin
Many dermatological disorders are known to be associated with dyslipidemia. Most of these are chronic inflammatory diseases, and underlying mechanism may involve secretion of proinflammatory cytokines. Studies have shown an increased occurrence of dyslipidemia in skin disorders like psoriasis, lichen planus, pemphigus, granuloma annulare, histiocytosis, and connective tissues diseases like lupus erythematosus. Table 1 shows the lipid abnormalities associated with these disorders.
Table 1.
Dermatological disorders with dyslipidemia and the associated disease abnormalities
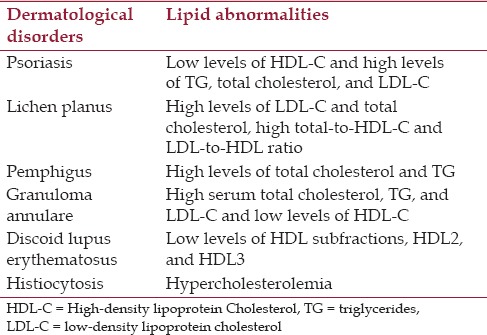
Psoriasis [Figure 1] is a chronic inflammatory, immune-mediated, skin disease affecting 2-3% of the population in which the most prominent microscopic abnormality is hyperproliferation and altered differentiation of keratinocytes.[6] The exact etiology of psoriasis is unknown, but it is believed to have an autoimmune basis with a strong genetic component (polygenic mode of inheritance). Multiple cardiovascular risk factors are also associated with psoriasis.[4,7] Several studies, although with relatively small patient populations, have demonstrated an atherogenic dyslipidemic profile consisting of increased levels of total cholesterol, triglycerides, LDL cholesterol, oxidatively modified lipids, and decreased levels of HDL cholesterol.[8,9,10] Recent studies have also demonstrated that the prevalence of metabolic syndrome is significantly higher in patients with psoriasis as compared to controls after the age of 40 years and psoriatic patients have an increased risk for the individual components of metabolic syndrome.[11,12,13] Components of metabolic syndrome include hyperglycemia, obesity, hypertension, and dyslipidemia.
Figure 1.

Psoriasis of palms. Psoriasis is a chronic inflammatory, immune-mediated, genetically-determined skin disease which affects skin, nails, and joints and has various systemic associations. The most prominent microscopic abnormality is hyperproliferation and altered differentiation of keratinocytes. The disease is associated with a high impact on the health-related quality of life and considerable cost
Lichen planus [Figure 2] is also a common chronic inflammatory skin disease. Association of lichen planus with dyslipidemia has been reported.[14,15,16] Chronic inflammation in patients with lichen planus may explain the association with dyslipidemia. Studies have reported that the individuals with lichen planus have significantly higher levels of various lipids compared to controls [Table 1].[15] Lipid levels screening in men or women with lichen planus may be useful to detect individuals at risk and to start preventive treatment against the development of cardiovascular disease.[16]
Figure 2.

Lichen planus. Lichen planus is a common chronic inflammatory disease of skin and mucosa which is characterized by a broad spectrum of clinical manifestations. Its classical clinical appearance involves purple polygonal plaques and papules
Pemphigus vulgaris [Figure 3] is a potentially fatal autoimmune mucocutaneous blistering disease, often requiring long-term, immunosuppressant therapies.[17] An association between pemphigus and dyslipidemia has been established in a case–control study done by utilizing the community-based medical database of a large healthcare provider organization in Israel. They observed an association between pemphigus and dyslipidemia with a specific serum lipid profile. Elevated serum total cholesterol and triglyceride levels were demonstrated in patients with pemphigus compared with controls. The associations were maintained when controlling confounders such as obesity, diabetes, and hypertension; but not after controlling corticosteroid intake. Neither LDL cholesterol nor HDL cholesterol were associated with pemphigus.[18]
Figure 3.

Pemphigus vulgaris. Pemphigus vulgaris is a potentially fatal autoimmune mucocutaneous blistering disease characterized by immunoglobulin G (IgG) autoantibodies against the stratified squamous epithelium
An interesting observation has been seen in relation to dyslipidemia in granuloma annulare. Recently, hypercholesterolemia, hypertriglyceridemia, elevated LDL cholesterol, and low HDL cholesterol were demonstrated. It has been found to be more common in generalized than in localized disease, and the annular lesion morphology is associated with hypercholesterolemia and dyslipidemia.[19]
Discoid lupus erythematosus (DLE) patients are also known to have lipid profile abnormalities, which is aggravated by disease activity. Also, there has been an increased risk of atherosclerosis due to the marked dyslipidemia associated with the disease.[20]
Among the other dermatological disorders, non-Langerhans cell histiocytosis may also have an associated dyslipidemia. Hyperlipidemia was also found to be one of the manifestations of cutaneous necrobiotic xanthogranuloma.[21,22] Sea blue histiocytosis is also reported to be associated with hyperlipidemia.[23]
Mechanisms Involved for Link between Skin Diseases and Dyslipidemias
Numerous mechanisms are speculated to explain the link between inflammation and dyslipidemia: Modulation of the enzymatic activity of lipoprotein lipase (LPL) by anti-LPL antibodies and decrease in LPL activity due to various pro-inflammatory cytokines such as tumor necrosis factor (TNF)-α, interleukin (IL)-1, IL-6, interferon-γ, and monocyte chemoattractant protein-1. Furthermore, atherogenic complexes of autoantibodies to oxidized LDL and to oxidized anticardiolipin are generated in response to an oxidative inflammatory effect which enhances the accumulation of LDL in the endothelial wall.[24]
Psoriasis is characterized by an increased immune activity of Th1 and Th17 cells. Cytokines like TNF α, IL-6, IL-17, IL-20, leptin, and vascular endothelial growth factor (VEGF) play a central role both in psoriasis and metabolic syndrome.[25] Conversely, metabolic syndrome itself could predispose an individual to developing psoriasis.[26,7] Lichen planus is associated with immunologic aberrations of delayed-type hypersensitivity immune reaction in which activated T cells and other inflammatory cells such as plasmatoid dendritic cells are key components.[27,28] These processes may explain the link between lichen planus and dyslipidemia, and other components of metabolic syndrome.
Dermatological Drugs Inducing Dyslipidemia
Several medications used to treat dermatological diseases may precipitate or exacerbate dyslipidemia.[Table 2] Oral retinoids and immunosuppressants like cyclosporine used to treat skin diseases like psoriasis is known to exacerbate dyslipidemias in them.
Table 2.
Adverse lipid eff ects of agents used for the treatment of skin diseases
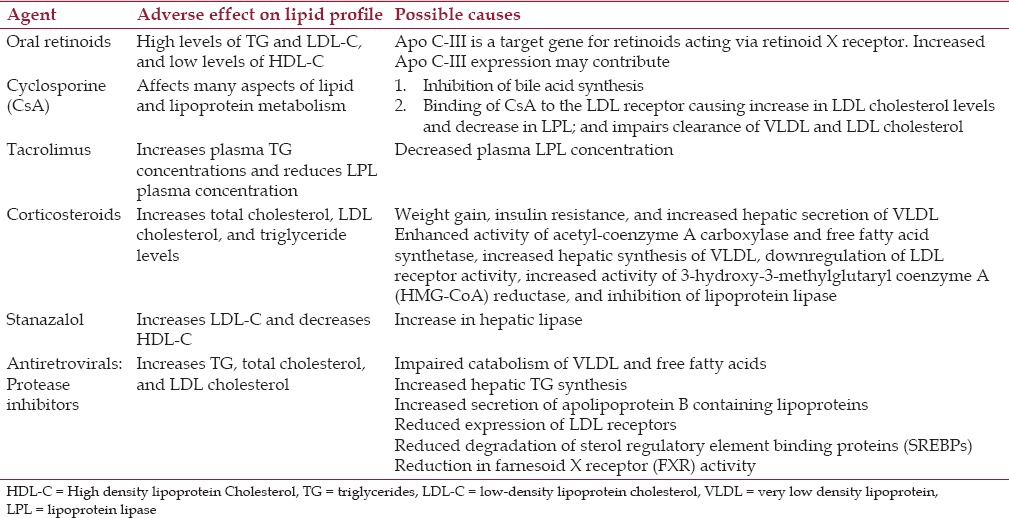
Hypertriglyceridemia is a metabolic complication of systemic retinoid therapy, which may occur in up to 17% of people.[29] Apo C-III appears to be a target gene for retinoids acting via retinoid X receptor. Increased Apo C-III expression may contribute to the hypertriglyceridemia and atherogenic lipoprotein profile observed after retinoid therapy.[29] Many of the current immunosuppressive drugs like cyclosporine, tacrolimus (TAC), and sirolimus are associated with an increase of one or more risk factors for the development of atherosclerosis.[30] Cyclosporin A (CsA), an immunosuppressant drug widely used in organ transplant recipients, is now popular in dermatological indications like psoriasis. Long-term treatment with CsA is associated with hyperlipidemia and an increased risk of atherosclerosis. Importantly, it is seen that hyperlipidemia normalizes when cyclosporine therapy is stopped, thus confirming its role.[31] Some of the probable causes for the hyperlipidemia could be inhibition of bile acid synthesis from cholesterol and transport of cholesterol to the intestines; binding of CsA to the LDL receptor, which increases LDL cholesterol levels; and marked reduction in post-heparin lipolytic activity with increased hepatic lipase activity and decreased LPL activity, which results in impaired clearance of very low-density lipoprotein and LDL cholesterol.[32,33] Binding of CsA to the LDL receptor via CsA-containing LDL cholesterol particles has also been proposed as the mechanism of cellular uptake of CsA.[34] CsA may also have a pro-oxidant effect on plasma LDL cholesterol, which may increase the risk of coronary artery disease (CAD), including the accelerated atherosclerosis seen in transplant recipients.[35]
TAC is known to significantly increase plasma triglyceride concentrations and reduce LPL plasma concentrations and activity in renal transplant patients, independent of any lipid lowering drug treatment the patients have received. Reduction in LPL activity, partly due to the decrease of plasma LPL concentration after TAC administration may be an explanation for hypertriglyceridemia observed in patients administered with TAC.[36] Currently, TAC has been used only in topical forms by dermatologists. Its cutaneous absorption is also minimal; hence dyslipidemia may not be an important consideration.
However, with respect to other immunosuppressive agents like mycophenolic acid (MPA) or azathioprine used in dermatology, there is no convincing data suggesting that they cause clinically significant increases in any lipid fractions.
Steroid intake has also been associated with dyslipidemia. Corticosteroids appear to elevate all the lipoprotein cholesterol levels.[37] This is explained in part due to the relative adrenocorticotropic hormone (ACTH) deficiency caused by long-term steroid intake. Corticosteroids are a main stay of therapy for pemphigus and many other autoimmune and inflammatory diseases. The major explanation for the association with dyslipidemia in pemphigus is the long-term corticosteroid use.[18] Corticosteroid-induced dyslipidemia is probably a result of weight gain, which leads to insulin resistance, increased hepatic secretion of very low-density lipoprotein, and increase in total cholesterol and triglyceride levels.[38,39,40] Studies have shown that anabolic androgen steroids like stanazalol can cause dyslipidemia by increasing LDL and decreasing HDL. A marked decrease in HDL cholesterol and HDL2 due to an increase in hepatic lipase has been noted.[41,42]
Antiretroviral therapy (ART) can also contribute to dyslipidemia. However, dyslipidemia does not develop in everyone who takes these medications, suggesting that host factors play a role. Protease inhibitor (PI)-based ART develop atherogenic changes in their lipoprotein profile, consisting of elevated triglyceride rich lipoproteins, total cholesterol, and LDL cholesterol; and an increased risk of CAD.[43,44] Non-nucleoside reverse transcriptase inhibitors (NNRTIs) show, in general, the best lipid profile of all ART drugs because they are associated with an increase in HDL.[44]
Biologics used in the treatment of skin diseases have also been linked to dyslipidemia. TNF blockers used for the treatment of psoriasis may have different effects on lipids. Long-term infliximab therapy may be proatherogenic, while etanercept and adalimumab may exert beneficial effects on lipids.[45]
Dermatological Manifestations of Dyslipidemias
Xanthomas are the dermatologic manifestations of underlying lipid abnormalities. They occur due to accumulations of lipid-laden macrophages. They are clinically classified as tendinous, tuberous, eruptive, and planar. They may be associated with familial or acquired disorders resulting in hyperlipidemia, with lyphoproliferative malignant neoplasms, or with no underlying disorder.[46] Xanthomas deposit in ligaments and tendons, although they may also be detected in periosteum and fascia.[47] Tendinous xanthomas occur along the tendons of hands and tendo Achilles. Tuberous xanthomas occur as yellow nodules; frequently associated with hypertriglyceridemia, and sometimes with hypercholesterolemia (type II).[48] Plane xanthomas are macular or slightly elevated lesions that can occur at any site, and can involve large areas of body. Generalized plane xanthomas can cover large regions of the body, including the face and neck. The most common presentation of planar xanthomas occurs on the eyelid or periorbital skin as yellowish plaques, referred to as xanthelasma.[49] Development of xanthomas on the palmar creases is commonly referred as xanthoma striatum palmare. It is known to be a rare but important sign of type III hyperlipoproteinemia.[50] Eruptive xanthomas present as orange-yellow papules, and they occur in hypertriglyceridemias and in uncontrolled diabetes.[51]
Therapy
Prevention of dyslipidemia
The essential principles of management of dyslipidemia involves, treating secondary or associated causes like diabetes, stopping the incriminating medication (consider alternate medication) or dosage reduction if feasible. Irrespective of the underlying dermatological disorder, cessation of cigarette smoking, and reduction of other modifiable risk factors are essential aspects of prevention of coronary heart disease.[1]
With steroid therapy, administering in the morning, keeping the dose to minimum, lifestyle modifications including exercise, weight control,[52] avoidance of fatty foods, and treatment of diabetes if present can all help complementing or even supplanting drug therapy. Insights in the management of CsA related dyslipidemia probably may best be obtained from its experience and evidence in renal transplant recipients. There has been conflicting evidence on whether CsA related dyslipidemia is dose related, with one large study showing no benefit.[53] Also the dermatological condition like psoriasis in which it is used has independent association with metabolic syndrome. Hence, may be prudent to be more proactive on treatment including pharmacotherapy for dyslipidemia and dysglycemia in these patients.
Hypertriglyceridemia remains the most common lipid abnormality among patients who have human immunodeficiency virus (HIV). Fenofibrate seems to be the fibrate of choice for HIV-infected patients who have hypertriglyceridemia, due to its lack of serious drug-drug interactions and data on better cardiovascular outcomes. Dual therapy with the addition of statins may be needed for the accompanying elevated LDL. Due to the multifactorial nature of HIV related dyslipidemia, altering treatment may not produce anticipated result.[54]
Eruptive xanthomas caused by hypertriglyceridemia respond well to lifestyle modification and lipid lowering pharmacotherapy with fibrates. Anecdotally, eruptive xanthomas typically appear to resolve within weeks of initiating systemic treatment, and tuberous xanthomas after some months, but tendinous xanthomas may take years to resolve or even persist indefinitely.[55]
Lifestyle modifications
Lifestyle approaches including dietary modifications form the main approach to treating children and youth. Physical activity offers a multitude of benefits by weight loss, decreased insulin resistance, decreased triglycerides, improved HDL cholesterol, and improved cardiovascular fitness and outcome. Dietary approaches include, use of non-fat (skim) and low-fat milk products, avoiding trans fats and animal fats and using vegetable fats in their place, limiting egg yolk consumption, and avoid prepared meats and lunch products with high saturated fat content (e. g., liver).[56] For elevated triglycerides; avoiding sugars, sweetened beverages, juices, and refined carbohydrates may be specifically useful.
Pharmacotherapy
Statins have been shown to reduce the risk of cardiovascular disease and cardiovascular mortality significantly and have more or less superseded bile acid resins due to their side effects. Statins mainly help in reducing LDL cholesterol. Rosuvastatin is more potent than atorvastatin or pravastatin and also more effective in additionally reducing triglyceride levels. Statins decrease the endogenous cholesterol production by inhibiting the key enzyme 3-hydroxy-3-methylglutaryl coenzyme A (HMG-CoA) reductase. They are generally well-tolerated, but one needs to be aware of possible adverse effects of liver injury, muscle cramps, and rhabdomyolysis. They are also known to cause cutaneous side effects like autoimmune reactions, reactions due to dryness of the skin, severe reactions like drug rash with eosinophilia and systemic symptoms (DRESS), and allergic reactions.[57] Diligently, avoid statins during actual or possible pregnancy as they are teratogenic. Ezetimbe can be a useful adjunct in severe cases. Fibrates form the sheet anchor of treating hypertriglyceridemia and are way ahead of niacin, which is poorly tolerated by many patients. Omega-3 fatty acids can be used additionally or alternatively when fibrates cannot be used as in pregnancy.
The evidence base for pharmacologic intervention for dyslipidemia in childhood is limited and is in general reserved for those at highest risk, that is, children at least 10 years of age who have LDL levels of 190 mg/dl or higher or of 160 mg/dl or higher and other risk factors such as diabetes, etc.
Drugs that interfere with chylomicron production such as orlistat are also useful for hypertriglyceridemic patient.[58] Insulin/dextrose infusion or therapeutic apheresis in combination with other strategies may be needed in extreme cases of dyslipidemia and/or pancreatitis.
Conclusion
Dyslipidemia may be more common than expected in dermatological disorders. Many of them are discussed in this article, but more diseases may be added to this list in the future. Management of them may involve lifestyle modifications and pharmacotherapy. Dietary counseling may help in the control of the primary disorder and enable them to reduce the cardiovascular and metabolic risks. Dermatologists treating these disorders shall have a comprehensive knowledge on this subject and manage holistically.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Ahmed SM, Clasen ME, Donnelly JE. Management of dyslipidemia in adults. Am Fam Physician. 1998;57:2192. [PubMed] [Google Scholar]
- 2.Sawant AM, Shetty D, Mankeshwar R, Ashavaid TF. Prevalence of dyslipidemia in young adult Indian population. J Assoc Physicians India. 2008;56:99–102. [PubMed] [Google Scholar]
- 3.Misra A, Luthra K, Vikram NK. Dyslipidemia in Asian Indians: Determinants and significance. J Assoc Physicians India. 2004;52:137–42. [PubMed] [Google Scholar]
- 4.Mazlin MB, Chang CC, Baba R. Comorbidities associated with psoriasis – data from the malaysian psoriasis registry. Med J Malaysia. 2012;67:518–21. [PubMed] [Google Scholar]
- 5.Fredrickson DS, Lees RS. A system for phenotyping hyperlipoproteinaemia. Circulation. 1965;31:321–7. doi: 10.1161/01.cir.31.3.321. [DOI] [PubMed] [Google Scholar]
- 6.Gisondi P, Ferrazzi A, Girolomoni G. Metabolic comorbidities and psoriasis. Acta Dermatovenerol Croat. 2010;18:297–304. [PubMed] [Google Scholar]
- 7.Neimann AL, Shin DB, Wang X, Margolis DJ, Troxel AB, Gelfand JM. Prevalence of cardiovascular risk factors in patients with psoriasis. J Am Acad Dermatol. 2006;55:829–35. doi: 10.1016/j.jaad.2006.08.040. [DOI] [PubMed] [Google Scholar]
- 8.Ma C, Harskamp CT, Armstrong EJ, Armstrong AW. The association between psoriasis and dyslipidaemia: A systematic review. Br J Dermatol. 2013;168:486–95. doi: 10.1111/bjd.12101. [DOI] [PubMed] [Google Scholar]
- 9.Akhyani M, Ehsani AH, Robati RM, Robati AM. The lipid profile in psoriasis: A controlled study. J Eur Acad Dermatol Venereol. 2007;21:1330–2. doi: 10.1111/j.1468-3083.2007.02260.x. [DOI] [PubMed] [Google Scholar]
- 10.Javidi Z, Meibodi NT, Nahidi Y. Serum lipid abnormalities and psoriasis. Indian J Dermatol. 2007;5:89–92. [Google Scholar]
- 11.Gisondi P, Tessari G, Conti A, Piaserico S, Schianchi S, Peserico A, et al. Prevalence of metabolic syndrome in patients with psoriasis: A hospital-based case-control study. Br J Dermatol. 2007;157:68–73. doi: 10.1111/j.1365-2133.2007.07986.x. [DOI] [PubMed] [Google Scholar]
- 12.Malhotra SK, Dhaliwal GS, Puri KJ, Gambhir ML, Mahajan M. An insight into relationship between psoriasis and metabolic syndrome. EDOJ. 2011;7:1–12. [Google Scholar]
- 13.Madanagobalane S, Anandan S. Prevalence of metabolic syndrome in south Indian patients with psoriasis vulgaris and the relation between disease severity and metabolic syndrome: A hospital-based case-control study. IJD. 2012;57:353–7. doi: 10.4103/0019-5154.100474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dreiher J, Shapiro J, Cohen AD. Lichen planus and dyslipidemia: A case-control study. Br J Dermatol. 2009;161:626–9. doi: 10.1111/j.1365-2133.2009.09235.x. [DOI] [PubMed] [Google Scholar]
- 15.Albert H. Chronic inflammation may explain dyslipidemia in lichen planus patients. Am J Med. 2011;124:543–8. [Google Scholar]
- 16.Arias-Santiago S, Buendia-Eisman A, Aneiros-Fernandez J, Giron-Prieto MS, Gutierrez-Salmeron MT, Mellado VG, et al. Cardiovascular risk factors in patients with lichen planus. Am J Med. 2011;124:543–8. doi: 10.1016/j.amjmed.2010.12.025. [DOI] [PubMed] [Google Scholar]
- 17.Ahmed AR, Spigelman Z, Cavacini LA, Posner MR. Treatment of pemphigus vulgaris with rituximab and intravenous immune globulin. N Engl J Med. 2006;355:1772–9. doi: 10.1056/NEJMoa062930. [DOI] [PubMed] [Google Scholar]
- 18.Wohl Y, Dreiher J, Cohen AD. Pemphigus and dyslipidaemia: A case-control study. Br J Dermatol. 2009;161:1418–20. doi: 10.1111/j.1365-2133.2009.09474.x. [DOI] [PubMed] [Google Scholar]
- 19.Wu W, Robinson-Bostom L, Kokkotou E, Jung HY, Kroumpouzos G. Dyslipidemia in granuloma annulare: A case-control study. Arch Dermatol. 2012;148:1131–6. doi: 10.1001/archdermatol.2012.1381. [DOI] [PubMed] [Google Scholar]
- 20.Lagogianni I, Papapanagiotou A, Piperi C, Kalofoutis C, Troupis G, Zachari A, et al. Evidence of reduced plasma HDL subfractions in patients with cutaneous discoid lupus erythematosus. Clin Biochem. 2005;38:286–90. doi: 10.1016/j.clinbiochem.2004.10.006. [DOI] [PubMed] [Google Scholar]
- 21.Ansari NA, Al-Ratrout JT. Non-Langerhans cell histiocytoses of the skin. Saudi Med J. 2003;24:1296–9. [PubMed] [Google Scholar]
- 22.Kossard S, Winkelmann RK. Necrobiotic xanthogranuloma with paraproteinemia. J Am Acad Dermatol. 1980;3:257–70. doi: 10.1016/s0190-9622(80)80189-7. [DOI] [PubMed] [Google Scholar]
- 23.Parker AC, Bain AD, Brydon WG, Harkness RA, Smith AF, Smith II, et al. Sea-blue histiocytosis associated with hyperlipidaemia. J Clin Pathol. 1976;29:634–8. doi: 10.1136/jcp.29.7.634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hahn BH, Grossman J, Chen W, Mc Mahon M. The pathogenesis of atherosclerosis in autoimmune rheumatic diseases: Roles of inflammation and dyslipidemia. J Autoimmun. 2007;28:69–75. doi: 10.1016/j.jaut.2007.02.004. [DOI] [PubMed] [Google Scholar]
- 25.Gottleib A, Dann F, Menter A. Psoriasis and the metabolic syndrome. J Drugs Dermatol. 2008;7:563–72. [PubMed] [Google Scholar]
- 26.Naldi L, Chatenoud L, Linder D, Belloni Fortina A, Peserico A, Virgili AR, et al. Cigarette smoking, body mass index, and stressful life events as risk factors for psoriasis: Results from an Italian case- control study. J Invest Dermatol. 2005;125:61–7. doi: 10.1111/j.0022-202X.2005.23681.x. [DOI] [PubMed] [Google Scholar]
- 27.Sezer E, Ozugurlu F, Ozyurt H, Sahin S, Etikan I. Lipid peroxidation and antioxidant status in lichen planus. Clin Exp Dermatol. 2007;32:430–4. doi: 10.1111/j.1365-2230.2007.02436.x. [DOI] [PubMed] [Google Scholar]
- 28.de Mattos Camargo Grossmann S, de Aguiar MC, Teixeira R, do Carmo MA. Oral lichen planus and chronic hepatitis C: A controversial association. Am J Clin Pathol. 2007;127:800–4. doi: 10.1309/HDWCT36P0GMGP40V. [DOI] [PubMed] [Google Scholar]
- 29.Bershad S, Rubinstein A, Paterniti JR, Le NA, Poliak SC, Heller B, et al. Changes in plasma lipids and lipoproteins during isotretinoin therapy for acne. N Engl J Med. 1985;313:981–5. doi: 10.1056/NEJM198510173131604. [DOI] [PubMed] [Google Scholar]
- 30.Vu-Dac N, Gervois P, Torra IP, Fruchart JC, Kosykh V, Kooistra T, et al. Retinoids increase human Apo C-III expression at the transcriptional level via the retinoid X receptor. Contribution to the hypertriglyceridemic action of retinoids. J Clin Invest. 1998;102:625–32. doi: 10.1172/JCI1581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shupack J, Abel E, Bauer E, Brown M, Drake L, Freinkel R, et al. Cyclosporine as maintenance therapy in patients with severe psoriasis. J Am Acad Dermatol. 1997;36:423–32. doi: 10.1016/s0190-9622(97)80219-8. [DOI] [PubMed] [Google Scholar]
- 32.Kobashigawa JA, Kasiske BL. Hyperlipidemia in solid organ transplantation. Transplantation. 1997;63:331–8. doi: 10.1097/00007890-199702150-00001. [DOI] [PubMed] [Google Scholar]
- 33.Derfler K, Hayde M, Heinz G, Hirschl MM, Steger G, Hauser AC, et al. Decreased postheparin lipolytic activity in renal transplant recipients with cyclosporin A. Kidney Int. 1991;40:720–7. doi: 10.1038/ki.1991.266. [DOI] [PubMed] [Google Scholar]
- 34.de Groen PC. Cyclosporine, low-density lipoprotein, and cholesterol. Mayo Clin Proc. 1988;63:1012–21. doi: 10.1016/s0025-6196(12)64916-7. [DOI] [PubMed] [Google Scholar]
- 35.Apanay DC, Neylan JF, Ragabn MS, Sgoutas DS. Cyclosporine increases the oxidizability of low-density lipoproteins in renal transplant recipients. Transplantation. 1994;58:663–9. [PubMed] [Google Scholar]
- 36.Tory R, Sachs-Barrable K, Goshko CB, Hill JS, Wasan KM. Tacrolimus-induced elevation in plasma triglyceride concentrations after administration to renal transplant patients is partially due to a decrease in lipoprotein lipase activity and plasma concentrations. Transplantation. 2009;88:62–8. doi: 10.1097/TP.0b013e3181aa7d04. [DOI] [PubMed] [Google Scholar]
- 37.Henkin Y, Como JA, Oberman A. Secondary dyslipidemia. Inadvertent effects of drugs in clinical practice. JAMA. 1992;267:961–8. doi: 10.1001/jama.267.7.961. [DOI] [PubMed] [Google Scholar]
- 38.Blum A, Aravot D. Heart transplantation – An update. Clin Cardiol. 1996;19:930–8. doi: 10.1002/clc.4960191206. [DOI] [PubMed] [Google Scholar]
- 39.Kirk JK, Dupuis RE. Approaches to the treatment of hyperlipidemia in the solid organ transplant recipient. Ann Pharmacother. 1995;29:879–91. doi: 10.1177/106002809502900911. [DOI] [PubMed] [Google Scholar]
- 40.Chan MK, Varghese Z, Persaud JW, Fernando ON, Moorhead JF. The role of multiple pharmaco-therapy in the pathogenesis of hyperlipidemia after renal transplantation. Clin Nephrol. 1981;15:309–13. [PubMed] [Google Scholar]
- 41.Lenders JW, Demacker PN, Vos JA, Jansen PL, Hoitsma AJ, van ‘t Laar A, et al. Deleterious effects of anabolic steroids on serum lipoproteins, blood pressure, and liver function in amateur body builders. Int J Sports Med. 1988;9:19–23. doi: 10.1055/s-2007-1024972. [DOI] [PubMed] [Google Scholar]
- 42.Thompson PD, Cullinane EM, Sady SP, Chenevert C, Saritelli AL, Sady MA, et al. Contrasting effects of testosterone and stanozolol on serum lipoprotein levels. JAMA. 1989;261:1165–8. [PubMed] [Google Scholar]
- 43.van der Valk M, Reiss P. Lipid profiles associated with antiretroviral drug choices. Curr Opin Infect Dis. 2003;16:19–23. doi: 10.1097/00001432-200302000-00004. [DOI] [PubMed] [Google Scholar]
- 44.Estrada V, Portilla J. Dyslipidemia related to antiretroviral therapy. AIDS Rev. 2011;13:49–56. [PubMed] [Google Scholar]
- 45.Kerekes G, Soltesz P, Der H, Veres K, Szabo Z, Vegvari A, et al. Effects of biologics on vascular function and atherosclerosis associated with rheumatoid arthritis. Ann N Y Acad Sci. 2009;1173:814–21. doi: 10.1111/j.1749-6632.2009.04645.x. [DOI] [PubMed] [Google Scholar]
- 46.Murphy GF, Sellheyer K, Mihm MC. The skin. In: Kumar V, Abbas AK, Fausto N, editors. Robbins and Cotran Pathologic Basis of Disease. 7th ed. Philadelphia: Elsevier; 2004. p. 1248. [Google Scholar]
- 47.Miller M, Vogel RA. Clinical signs and syndromes associated with premature coronary artery disease. In: Miller M, Vogel RA, editors. The Practice of Coronary Disease Prevention. 8th ed. Baltimore, Md: Williams & Wilkins; 1996. pp. 24–35. [Google Scholar]
- 48.Bolognia JL, Braverman IM. Skin manifestation of internal disease. In: Kasper DL, et al., editors. Harrison's Principles of Internal Medicine. 16th ed. New York: McGraw-Hill; 2005. pp. 296–311. [Google Scholar]
- 49.Bergman R, Kasif Y, Aviram M, Maor I, Ullman Y, Gdal-On M, et al. Normo lipidemic xanthelasma palpebrarum: Lipid composition, cholesterol metabolism in monocyte-derived macrophages, and plasma lipid peroxidation. Acta Derm Venereol. 1996;76:107–10. doi: 10.2340/0001555576107110. [DOI] [PubMed] [Google Scholar]
- 50.Hsu JC, Su TC, Chen MF, Liau CS, Lee YT. Xanthoma striatum palmare in a patient with primary biliary cirrhosis and hypercholesterolemia. J Gastroenterol Hepatol. 2005;20:1799–800. doi: 10.1111/j.1440-1746.2005.03989.x. [DOI] [PubMed] [Google Scholar]
- 51.Digby M, Belli R, McGraw T, Lee A. Eruptive xanthomas as a cutaneous Manifestation of hypertriglyceridemia; A case report. J Clin Aesthet Dermatol. 2011;4:44–6. [PMC free article] [PubMed] [Google Scholar]
- 52.Summary of the second report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel II) JAMA. 1993;269:3015–23. [PubMed] [Google Scholar]
- 53.Hosseini MS, Rostami Z, Einollahi B. Dyslipidemia after kidney transplantation and correlation with cyclosporine level. Nephrourol Mon. 2013;5:831–4. doi: 10.5812/numonthly.11890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Dube MP, Stein JH, Aberg JA, Fichtenbaum CJ, Gerber JG, Tashima KT, et al. Adult AIDS Clinical Trials Group Cardiovascular Subcommittee. HIV Medical Association of the Infectious Disease Society of America. Guidelines for the evaluation and management of dyslipidemia in human immunodeficiency virus (HIV)-infected adults receiving antiretroviral therapy: Recommendations of the HIV Medical Association of the Infectious Disease Society of America and the Adult AIDS Clinical Trials Group. Clin Infect Dis. 2003;37:613–27. doi: 10.1086/378131. [DOI] [PubMed] [Google Scholar]
- 55.White LE, Horenstein MG, Shea CR. Xanthomas. In: Lebwohl MG, Heymann WR, Berth-Jones J, Coulsan I, editors. Treatment of skin disease. 4th ed. Elsevier Saunders; 2006. p. 804. [Google Scholar]
- 56.Zappalla FR, Gidding SS. Lipid management in children. Endocrinol Metab Clin North Am. 2009;38:171–83. doi: 10.1016/j.ecl.2008.11.006. [DOI] [PubMed] [Google Scholar]
- 57.Dobritoiu AM, Forsea DG. Statins and the skin. Ther Pharmacol Clin Toxicol. 2011;15:98–104. [Google Scholar]
- 58.Filippatos TD, Elisaf MS. Recommendations for severe hypertriglyceridemia treatment, are there new strategies? Curr Vasc Pharmacol. 2014;12:598–616. doi: 10.2174/15701611113119990133. [DOI] [PubMed] [Google Scholar]


