Abstract
Background:
Hypertension is a common medical disease, occurring in about one third of young adults and almost two thirds of individuals over the age of 60. With the release of the Eighth Joint National Committee on Prevention, Detection, Evaluation, and Treatment (JNC-8) guidelines, there have been major changes in blood pressure management in the various subgroups.
Aim:
Optimal blood pressure management and markers of end-organ damage in African-American adult patients were compared between patients who were managed according to the JNC-8 hypertension management guidelines and those who were treated with other regimens.
Materials and Methods:
African-American patients aged 18 years or older with an established diagnosis of hypertension were included in the study who were followed up in our internal medicine clinic between January 1, 2013 and December 31, 2103; the data on their systolic and diastolic blood pressure readings, heart rate, body mass index (BMI), age, gender, comorbidities, and medications were recorded. Patients were divided into four groups based on the antihypertensive therapy as follows — Group 1: Diuretic only; Group 2: Calcium channel blocker (CCB) only; Group 3: Diuretic and CCB; Group 4: Other antihypertensive agent. Their blood pressure control, comorbidities, and associated target organ damage were analyzed.
Results:
In all 323 patients, blood pressures were optimally controlled. The majority of the patients (79.6%) were treated with either a diuretic, a CCB, or both. Intergroup comparison analysis showed no statistically significant difference in the mean systolic blood pressure, mean diastolic blood pressure, associated comorbidities, or frequency of target organ damage.
Conclusion:
Although diuretics or CCBs are recommended as first-line agents in African-American patients, we found no significant difference in the optimal control of blood pressure and frequency of end-organ damage compared to management with other agents.
Keywords: African-American, Blood pressure, calcium channel blocker (CCB), Cerebrovascular disease, Diabetes mellitus, Hypertension, Kidney disease, Myocardial infarction (MI), Thiazide, Thiazide diuretics
Introduction
Hypertension is a common medical disease, occurring in about one third of young adults, almost two thirds of individuals over the age of 60, and in approximately 75% of individuals older than 70 years.[1] In 2001, hypertension was attributed to 92 million disability-adjusted life years throughout the world.[2] Hypertension can lead to many complications, including myocardial infarction (MI), chronic kidney disease (CKD), cerebrovascular disease, retinopathy, and heart failure, and is an important player in metabolic syndrome.[3] Among patients with type 2 diabetes mellitus who were 45 years or older, approximately 40-60% had hypertension and among those with macroalbuminuria, only 60% were able to maintain a systolic blood pressure under 140 mmHg.[4,5] It is often referred to as the silent killer and remains one of the most significant contributors to chronic disease and mortality.[6]
Numerous classes of antihypertensive medications have been used to manage hypertension and reduce the various risks associated with it.[7] There have been controversial discussions regarding the most evidence-based blood pressure management guidelines after the release of the Eighth Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC-8) guidelines.[3,8] These guidelines, released in February of 2014, were constructed after completion of an evidence-based meta-analysis.[3] Our study focuses on the recommendation that states: “In the general black population, including those with diabetes, initial antihypertensive treatment should include a thiazide-type diuretic or calcium channel blocker (CCB).”[3] This recommendation stems from a large study, the Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) trial, which showed that thiazide-type diuretics are more effective in improving cerebrovascular, heart failure, and combined cardiovascular outcomes as compared to an angiotensin convertase enzyme inhibitor (ACE-I) in both diabetic and nondiabetic black patients.[9] Additionally, the study found that CCBs were less effective than thiazide-type diuretics in preventing heart failure.
Lastly, there were no differences between antihypertensive management with a CCB and that with a thiazide-type diuretic in their outcome; therefore, the recommendation remains that both drugs can be used as first-line therapy.[9] This becomes important because many older outcome trials have shown that a reduction in blood pressure reduces the risk of coronary heart disease and stroke.[10,11]
Our study compared the target blood pressure goals and frequency of end-organ damage in adult African-American patients who were in compliance with the new JNC-8 hypertension management guidelines compared those managed with antihypertensive medications other than a CCB and/or a thiazide-type diuretic.
Materials and Methods
Study selection
Our study was a retrospective review of the electronic medical records of adult African-American patients with hypertension who were managed with one or more of the antihypertensive medications. This study was reviewed and approved by the Institutional Review Board of the Cooper Health System, Camden, New Jersey, USA. Permission was granted to use materials that were collected solely for research study purposes as per the Health Insurance Portability and Accountability Act (HIPAA) requirements, and the informed consent waivers were granted by the Institutional Review Board. We selected adult African-American patients aged 18 years or older with an established diagnosis of hypertension who followed up in our internal medicine clinic between January 1, 2013 and December 31, 2013. We hypothesized that adult African-American patients with hypertension who were treated with CCB and/or thiazide-type diuretic therapy as per the JNC-8 guidelines would have better optimal blood pressure control and lower association of target organ damage compared to adult African-American patients with hypertension managed with other antihypertensive medications. Comparing African-American individuals with history of hypertension who were treated by a CCB or a thiazide-type diuretic to those who were treated with other regimens might allow us to identify the long-term benefits and overall trends in the prevention of end-organ damage. The inclusion criteria were adult African-American patients with a diagnosis of hypertension and who were managed by an antihypertensive agent.
The exclusion criteria were patients under 18 years of age, no history of hypertension, non–African-American race, or those who had a diagnosis of hypertension but were not managed with an antihypertensive agent.
Data collection
We recorded the following data for each patient: Age; gender; systolic and diastolic blood pressure readings; heart rate; body mass index (BMI); comorbidities, including prior history of smoking, history of coronary artery disease (CAD), history of MI, history of transient ischemic attacks (TIA) or cerebrovascular accidents (CVA), history of CKD, history of hypertensive retinopathy, history of peripheral arterial disease (PAD), hyperlipidemia, or diabetes. Additionally, we evaluated each patient's medication history and collected whether the patients were on thiazide-type diuretics, CCBs, ACE-I, aldosterone receptor blockers (ARB), beta-blockers, alpha-blockers, or other antihypertensive medications.
Other antihypertensive medications were accounted for by writing down the name and dose of each medication.
Statistical study
We entered the patient data in a Microsoft Excel (2013, Redmond, Washington, USA) spreadsheet and analyzed them using SPSS (Statistical Package for the Social Sciences, version 15.01, IBM, Armonk, New York, USA). A sample size of greater than 300 patients was selected based on the estimated number of patients with a diagnosis of hypertension who were expected to visit the office within the study period. We divided our patients into four groups based on the antihypertensive therapeutic agent: Group 1 on a thiazide-type diuretic only; Group 2 on a CCB only; Group 3 on a thiazide-type diuretic and a CCB; and Group 4 on other antihypertensive agents that were neither thiazide-type diuretics nor CCBs. We compared the systolic and diastolic blood pressures within the four study groups by using one-way analysis of variance (ANOVA) analysis. When comparing the four groups between each other for baseline characteristics and evidence of end-organ damage, we used Pearson's chi-square test and Fisher's exact test. The Mann–Whitney U Test was used to analyze the unpaired data.
We used the Kruskal–Wallis test to determine if there were statistically significant differences between two or more groups of an independent variable on a continuous or ordinal dependent variable. Binomial logistic regression was used to analyze the dichotomous dependent variables.
Results
We identified 344 adult African-American patients with a diagnosis of hypertension. Twenty-one patients were excluded as they were managed conservatively without antihypertensive medication. The remaining 323 patients were included in the study. Among all patients, Group 1 demonstrated the largest group of the patients who were treated with a diuretic only (38.9%), while the majority of the patients (79.6%) were treated with either a diuretic and a CCB, a CCB alone, or another antihypertensive [Table 1]. The average ages of the patients in groups 1, 2, 3, and 4 were 60.9 years, 59.7 years, 62.8 years, and 58.5 years, with a predominantly female distribution; however, the differences in age and gender were not statistically significant [Table 1].
Table 1.
Baseline characteristics and demographics of the four study groups
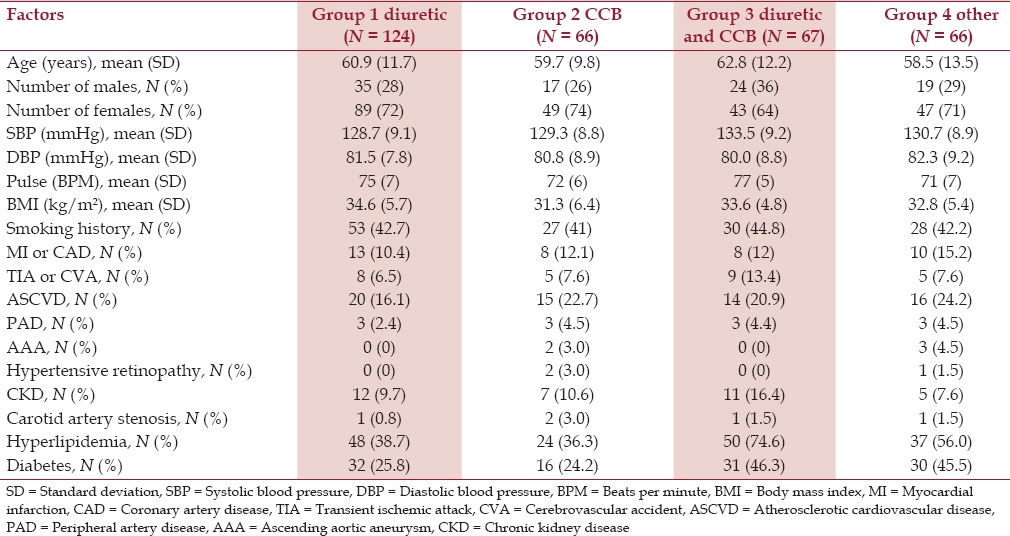
All groups had optimally controlled systolic blood pressures. The mean systolic blood pressure in the groups ranged 128.7-133.5 mmHg. There were no statistically significant differences between these groups (P = 0.190). All groups had optimally controlled mean diastolic blood pressures ranging 80.0-82.3 mmHg. There were no statistically significant differences between these groups (P = 0.599). The average pulse rates were well within the normal range of 71-77 per minute with no statistically significant difference [Table 1].
Obesity was a strong comorbid state. The average BMIs of the patients in groups 1-4 were 34.6 kg/m2, 31.3 kg/m2, 33.6 kg/m2, and 32.8 kg/m2, respectively. All BMIs were comparable [Table 1].
Association with hyperlipidemia was higher in certain groups compared to others, for example, in Group 1 compared to Group 3 (59.7% vs 38.7%, P = 0.005) [Table 3] and Group 3 compared to Group 2 (59.7% vs 36.4%, P = 0.007) [Table 5]. There was no significant difference between the other groups. Type 2 diabetes was another comorbid condition with a prevalence of 25.8%, 24.2%, 46.3%, and 45.5% in groups 1, 2, 3, and 4, respectively, which showed no statistically significant difference [Table 1].
Table 3.
Comparison of comorbid conditions and target organ involvement between groups 1 and 3
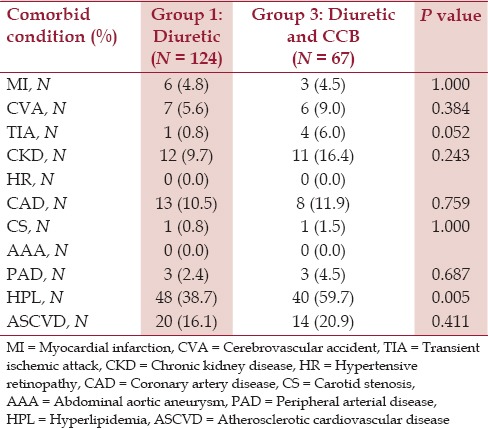
Table 5.
Comparison of comorbid conditions and target organ involvement between groups 2 and 3
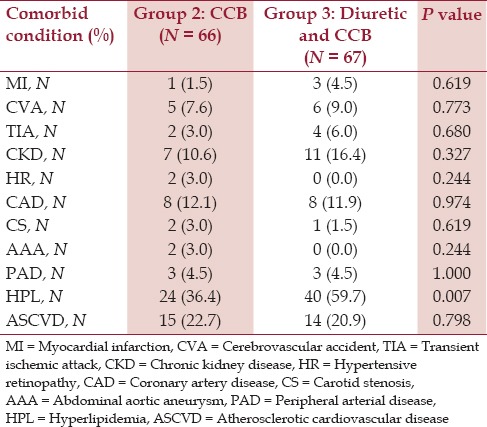
Table 4.
Comparison of comorbid conditions and target organ involvement between groups 1 and 4
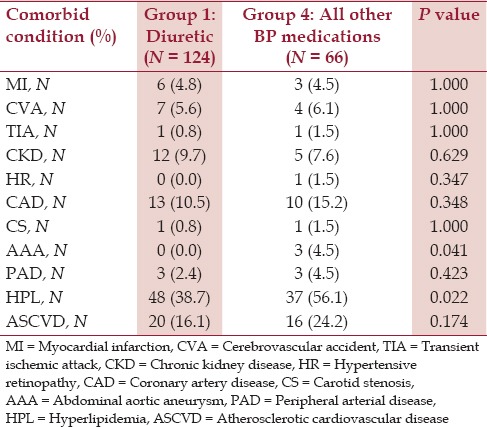
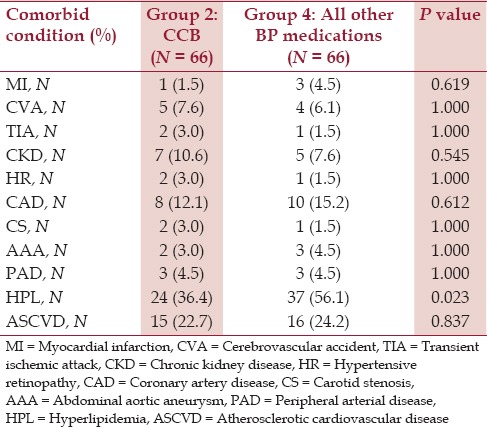
The overall prevalence of atherosclerotic cardiovascular disease (ASCVD) in each group ranged 16.1-24.2% but the differences were not statistically significant [Figure 1]. The prevalence of associated target organ involvement in the form of MI or CAD, TIA or CVA, PAD, CKD, hypertensive retinopathy, carotid artery stenosis, and abdominal aortic aneurysm between the four groups showed no statistically significant difference between the groups [Tables 2-7, Figure 2].
Figure 1.
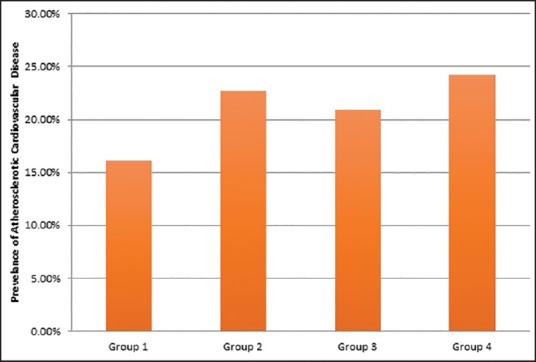
Prevalence of ASCVD in all groups
Table 2.
Comparison of comorbid conditions and target organ involvement between groups 1 and 2
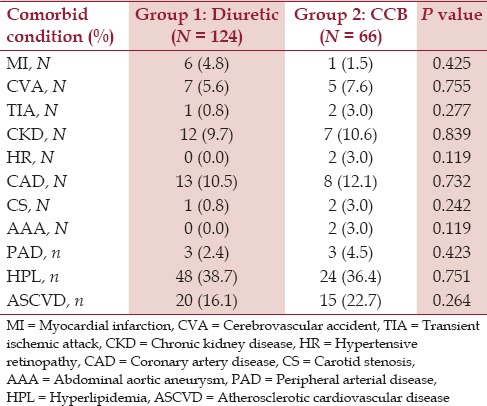
Table 7.
Comparison of comorbid conditions and target organ involvement between groups 3 and 4
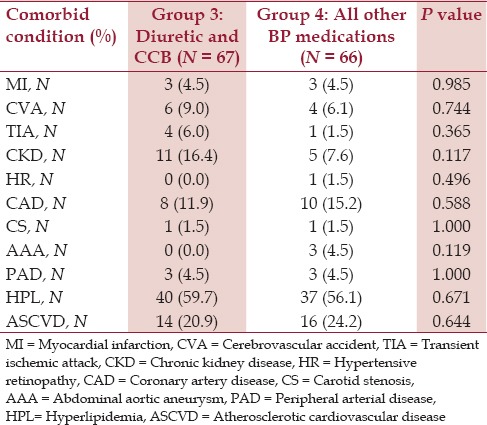
Figure 2.
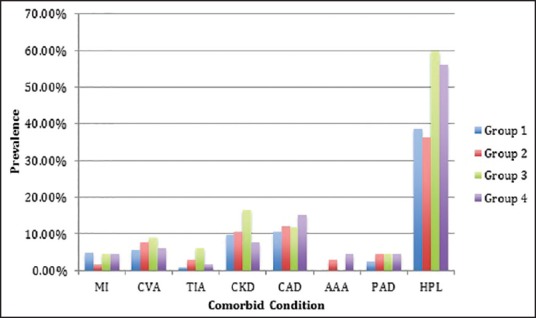
Frequency of comorbid conditions in all groups
Table 6.
Comparison of comorbid conditions and target organ involvement between groups 2 and 4
Discussion
Our study revealed two major observations. First, hypertension was optimally managed in adult African-American patients with either a thiazide-type diuretic, a CCB, a combination of both agents, or with other nondiuretic and non-CCB agents. Second, the prevalence of end-organ involvement and comorbid conditions in the adult African-American patients were not significantly different between the patients treated with a thiazide-type diuretic, a CCB, or other antihypertensive agents.
The ALLHAT trial[9] showed that thiazide-type diuretics are more effective in improving cerebrovascular outcome, heart failure, and combined cardiovascular outcomes as compared to an ACE-I in both diabetic and nondiabetic African-American patients; nonetheless, our findings show that optimum control of blood pressure was associated with comparable prevalence of end-organ involvement and comorbid conditions in the adult African-American patients who were treated with either a thiazide-type diuretic, a CCB, both a thiazide and a CCB, or other antihypertensive agents.
Our findings further suggest that although the thiazide-type diuretics and CCBs are very effective in the management of hypertension in the African-American patients, the other antihypertensive agents, which fall into the category of nondiuretic and non-CCB agents, are equally effective in the optimal control of blood pressure and show no difference in the prevalence of comorbid ASCVD. This raises a fundamental question: Is it the optimal control of the blood pressure that determines the cardiovascular event outcome irrespective of the antihypertensive agent, or is there a superiority of one specific class of antihypertensive agent over the other? Verdecchia et al. performed a meta-analysis of 28 randomized controlled trials where blood pressure-dependent and blood pressure-independent effects of ACE-I and CCB were studied in context of the prevention of coronary heart disease and stroke.[12] The trials compared ACE-I to diuretics, beta-blockers, and placebo. They also CCB with diuretics, beta-blockers, and placebo. The study found that the risk of coronary heart disease was decreased by blood pressure reduction and the use of ACE-I. Similarly, blood pressure reduction and the use of CCB independently reduced the incidence of stroke. The findings of this meta-analysis confirm that blood pressure lowering is fundamental for the prevention of coronary heart disease and stroke, irrespective of the antihypertensive agent or agents.
The effects of different blood pressure agents have been studied exclusively in the African-American population because of the prevalence of earlier and more severe hypertension, which is known to be higher in this population. The consequences of earlier and more severe hypertension include higher risk of stroke, kidney disease, and heart disease.[13] Although many people may require combination therapy, monotherapy is often tried with one of the recommended thiazides or CCB agents initially. The JNC-8 guidelines do not recommend one over the other, but the Jackson Heart study by Harman et al. showed that African-American adults with hypertension had better blood pressure control on thiazide diuretic monotherapy compared to those on CCB monotherapy.[14]
Decreasing end-organ damage with blood pressure control has been the target of studies for many years. As for the CCB, Bakris et al. looked at African-American patients on CCB (sustained-release verapamil) against beta-blockers (atenolol) and examined the different effects on proteinuria and the progression of diabetic neuropathy. The study enrolled 34 patients who had a 5-year history of hypertension and diabetes, serum creatinine of more than 1.4 mg/dL, and proteinuria of greater than 1500 mg/day, and the researchers concluded that CCB slowed the rate of decline in creatinine clearance and induced a greater reduction in proteinuria compared with the atenolol group (−1.7 ± 0.9 mL/min vs −3.7 ± 1.4 mL/min per year per 1.73 m2, P < 0.01).[15] In another study by Pendergast et al. focusing on CCB, the effects of blood pressure control on diastolic dysfunction progression were looked at in a retrospective cohort study of 96 African-American adults with hypertension and diastolic dysfunction. The main outcome measured was a change in the diastolic function in comparison to time and medication classification. They found that CCBs were protective against the progression of diastolic heart failure [odds ratio (OR) for CCB users vs nonusers 0.28, 95% confidence interval (CI), 0.09-0.90, P < 0.05]. Hall et al. looked into the efficacy, safety, and tolerability of three different dihydropyridine CCBs: Amlodipine besylate, nifedipine coat-core (CC), and nifedipine gastrointestinal therapeutic system (GITS) in 192 African-American patients with hypertension across 10 study centers. Patients were randomized to monotherapy with amlodipine besylate, nifedipine CC, and nifedipine GITS, and blood pressures were monitored for 8 weeks with the primary end point of average reduction in 24-h ambulatory diastolic blood pressure. Secondary end points were 24-h ambulatory systolic blood pressure control, office systolic and diastolic blood pressure reduction, and the safety and tolerability of the drugs. They found that all three drugs were equivalent in African-American patients with stage 1 and 2 hypertension.[16]
Other focused studies looked at the management of African-American patients and hypertension control with ACE-I. In a small study by Guasch et al., 31 African-American patients with non-insulin–dependent diabetes mellitus and nephropathy (urine protein > 500 mg/day or = 500 mg/day) were studied for the effects of dihydropyridine CCB (isradipine) versus an ACE-I (captopril) on proteinuria. They found that the ACE-I group reduced proteinuria in the patients and the CCB group increased proteinuria in 6 months.[17] Agodoa et al. also conducted a randomized, double-blind trial looking at the incidence of end-stage renal disease (ESRD) due to hypertension and optimal strategies for blood pressure control in African-American patients aged 18-70 years with an ACE-I (ramipril), a dihydropyridine CCB (amlodipine), and a beta-blocker (metoprolol). The primary outcome was the rate of change in glomerular filtration rate (GFR) and the secondary outcome was a reduction in GFR, ESRD, or death. The ramipril group had a 36% slower mean decline in GFR over 3 years (P = 0.006) and a 48% reduced risk of clinical end points compared to the amlodipine group (95% CI, 20-66%). There was no difference in the mean GFR decline between groups (P = 0.38). They concluded that ramipril was superior to amlodipine in slowing renal disease progression in patients with hypertensive renal disease and proteinuria.[18]
The effects of ARB in the management of hypertension in African-American patients have not been well studied, hence regarded as less validated. One study showed that African-American patients had lower plasma renin activity levels compared to white patients (0.92 ng/mL/h vs 1.26 ng/mL/h, respectively, P < 0.05), which may explain a possible decreased effectiveness of the ARB agents in African-American patients with hypertension.[19]
The greatest strength of our study was the exclusion criteria, which helped us select only African-American patients with an established diagnosis of hypertension that required one or more modes of antihypertensive therapy. All patients had more than one office visit, which helped us to identify the effects of antihypertensive therapy over a period of time. There are some limitations to our analysis, such as the fact that our study does not take into account patients who may have missed, changed, or skipped their medications. Patients may not have taken their blood pressure medications prior to appearing for the doctor's appointment, thus leading to variable blood pressure readings.
Future studies could include further subanalysis on patients taking equal doses of the antihypertensive medications with more frequent blood pressure checks. A prospective study with the ability to measure multiple blood pressure readings and medication compliance would be informative and vital to further research.
Conclusion
We conclude that in the adult African-American patients in our study, hypertension was optimally and equally well managed with either a thiazide-type diuretic, a CCB, or with other nondiuretic and non-CCB antihypertensive agents. Similarly, the prevalence of end-organ involvement and of comorbid conditions in adult African-American patients were not significantly different between the patients who were treated with a thiazide-type diuretic, with CCB, and with any other antihypertensive agent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors thank Christine Rickette RN (study coordinator) for her contribution to this study.
References
- 1.Explore High Blood Pressure. Bethesda, Maryland: National Heart, Lung, and Blood Institute: National Heart, Lung and Blood Institute; 2012. [Accessed May 21, 2015]. at http://www.nhlbi.nih.gov/health/health-topics/topics/hbp/ [Google Scholar]
- 2.Kotchen TA. Hypertensive vascular disease. In: Longo DL, Fauci AS, Kasper DL, Hauser SL, Jameson J, Loscalzo J, editors. Harrison's Principles of Internal Medicine. 17th ed. New York, NY: McGraw Hill Medical; 2012. pp. 2042–59. [Google Scholar]
- 3.James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: Report from the panel members appointed to the Eight Joint National Committee (JNC 8) JAMA. 2014;311:507–20. doi: 10.1001/jama.2013.284427. [DOI] [PubMed] [Google Scholar]
- 4.Joven MH, Anderson RJ. Update on blood pressure control and renal outcomes in diabetes mellitus. Curr Diab Rep. 2015;15:44. doi: 10.1007/s11892-015-0613-6. [DOI] [PubMed] [Google Scholar]
- 5.Hill CJ, Cardwell CR, Patterson CC, Maxwell AP, Magee GM, Young RJ, et al. Chronic kidney disease and diabetes in the National Health Service: A cross-sectional survey of the U. K. national diabetes audit. Diabet Med. 2014;31:448–54. doi: 10.1111/dme.12312. [DOI] [PubMed] [Google Scholar]
- 6.Nwankwo T, Yoon SS, Burt V, Gu Q. Hyattsville, MD: National Center for Health Statistics, Centers for Disease Control and Prevention, US Dept of Health and Human Services; 2013. [Accessed May 21, 2015]. Hypertension among Adults in the US: National Health and Nutrition Examination Survey, 2011-2012. NCHS Data Brief, No. 133. at http://www.cdc.gov/bloodpressure/ [Google Scholar]
- 7.Masuo K. Treatments for hypertension in type 2 diabetes-non-pharmacological and pharmacological measurements. Curr Hypertens Rev. 2015;11:61–77. doi: 10.2174/1573402111666150416124617. [DOI] [PubMed] [Google Scholar]
- 8.Makridakis S, DiNicolantonio JJ. Hypertension: Empirical evidence and implications in 2014. Open Heart. 2014;1:e000048. doi: 10.1136/openhrt-2014-000048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Furberg CD, Wright JT, Davis BR, Cutler JR, Alderman M, Black H, et al. Major outcomes in high-risk hypertensive patients randomized to angiotensin-converting enzyme inhibitor or calcium channel blocker vs diuretic: The Antihypertensive and Lipid-Lowering Treatment to Prevent Heart Attack Trial (ALLHAT) JAMA. 2002;288:2981–97. doi: 10.1001/jama.288.23.2981. [DOI] [PubMed] [Google Scholar]
- 10.MacMahon S, Peto R, Cutler J, Collins R, Sorlie P, Neaton J, et al. Blood pressure, stroke and coronary heart disease. Part 1, prolonged differences in blood pressure: Prospective observational studies corrected for the regression dilution bias. Lancet. 1990;335:765–74. doi: 10.1016/0140-6736(90)90878-9. [DOI] [PubMed] [Google Scholar]
- 11.Collins R, Peto R, MacMahon S, Hebert P, Fiebach NH, Eberlein KA, et al. Blood pressure, stroke, and coronary heart disease: Part 2, short-term reductions in blood pressure: Overview of randomized drug trials in their epidemiological context. Lancet. 1990;335:827–38. doi: 10.1016/0140-6736(90)90944-z. [DOI] [PubMed] [Google Scholar]
- 12.Verdecchia P, Reboldi G, Angeli F, Gattobigio R, Bentivoglio M, Thijs L, et al. Angiotensin-converting enzyme inhibitors and calcium channel blockers for coronary heart disease and stroke prevention. Hypertension. 2005;46:386–92. doi: 10.1161/01.HYP.0000174591.42889.a2. [DOI] [PubMed] [Google Scholar]
- 13.Ferdinand KC, Armani AM. The management of hypertension in African Americans. Crit Pathw Cardiol. 2007;6:67–71. doi: 10.1097/HPC.0b013e318053da59. [DOI] [PubMed] [Google Scholar]
- 14.Harman J, Walker ER, Charbonneau V, Akylbekova EL, Nelson C, Wyatt SB. Treatment of hypertension among African Americans: The Jackson Heart Study. J Clin Hypertens (Greenwich) 2013;15:367–74. doi: 10.1111/jch.12088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bakris GL, Mangrum A, Copley JB, Vicknair N, Sadler R. Effect of calcium channel or B-blockade on the progression of diabetic nephropathy in African Americans. Hypertension. 1997;29:744–50. doi: 10.1161/01.hyp.29.3.744. [DOI] [PubMed] [Google Scholar]
- 16.Prendergast HM, Dudley S, Brown M, Daviglus M, Kane J, Bradshaw Bunney E, et al. Antihypertensive medications and diastolic dysfunction progression in an African American population. High Blood Press Cardiovasc Prev. 2014;21:269–74. doi: 10.1007/s40292-014-0064-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Guasch A, Parham M, Zayas CF, Campbell O, Nzerue C, Macon E. Contrasting effects of calcium channel blockade versus converting enzyme inhibition on proteinuria in African Americans with non-insulin-dependent diabetes mellitus and nephropathy. J Am Soc Nephrol. 1997;8:793–8. doi: 10.1681/ASN.V85793. [DOI] [PubMed] [Google Scholar]
- 18.Agodoa LY, Appel L, Bakris GL, Beck G, Bourgoignie J, Briggs JP, et al. African American Study of Kidney Disease and Hypertension (AASK) Study Group. Effect of ramipril vs amlodipine on renal outcomes in hypertensive nephrosclerosis: A randomized controlled trial. JAMA. 2006;285:2719–28. doi: 10.1001/jama.285.21.2719. [DOI] [PubMed] [Google Scholar]
- 19.He J, Klag MJ, Appel LJ, Charleston J, Whelton PK. The renin-angiotensin system and blood pressure: Differences between blacks and whites. Am J Hypertens. 1999;12:555–62. doi: 10.1016/s0895-7061(99)00030-8. [DOI] [PubMed] [Google Scholar]


