Abstract
Septic arthritis of the temporomandibular joint (TMJ) is a rare event that has only been reported a few dozen times worldwide. This case is remarkable for septic arthritis of the TMJ joint in an otherwise healthy male.
Case Report:
A 24-year-old male presented to the emergency department with periauricular swelling, erythema, fever, myalgia's and generalized joint pain. He had previously sought medical attention and was placed on ciprofloxacin. However, he developed facial swelling and a rash and had to discontinue the antibiotic. On physical exam the patient had a large swelling and tenderness in his left periauricular area, with erythema and deviation of the right mandible which limited his ability to open the mouth. A computed tomography showed mild asymmetric soft tissue swelling in the left pharyngeal region but did not show joint effusion. Subsequent magnetic resonance imaging did show effusion of the joint space. The effusion was drained, and the synovial fluid was submitted for gram stain, culture, and sensitivity. The cultures grew menthicillin sensitive Staphyloccocus Aureus. The patient was discharged to complete a two week course of intravenous (IV) Ceftriaxone and IV Vancomycin via home infusion.
Conclusion:
Septic Arthritis of the TMJ is a rare event with very specific clinical symptoms. Due to the low sensitivity of the computed tomography scan, magnetic resonance imaging should be considered when computed tomography scan is negative for TMJ effusion.
Keywords: Computed tomography, magnetic resonance imaging, septic arthritis, temporomandibular joint
Introduction
Septic arthritis of the temporomandibular joint (TMJ) is a rare occurrence that has only been reported 33 times in literature.[1] While it is most often associated with Staphylococcus aureus, it can be associated with other bacteria, yeast, and spirochetes. Usually, it is associated with hematogenous spread of infection, local spread of infection, blunt trauma, autoimmune diseases, and iatrogenesis.[2] Failure to promptly treat septic arthritis of the TMJ may result in joint dysfunction, fibrosis, and alkylosis.[3] This report describes a case of TMJ septic arthritis in a healthy 24-year-old male that was promptly treated and resolved without any complications.
Case Presentation
A 24-year-old male presented to the emergency department with periauricular swelling, erythema, fever, myalgia, and generalized joint pain that had been present for 2–3 weeks. He had previously seen a primary care physician for his symptoms. At that time he was prescribed oral ciprofloxacin 750 mg and underwent computed tomography. He subsequently developed facial swelling and a rash that was considered to be an allergic reaction to ciprofloxacin. Ciprofloxacin was discontinued and the symptoms were treated with Benadryl and intravenous steroids. The jaw symptoms remitted for 1 week. The next week his primary care physician called to inform that computed tomography showed possible septic arthritis of the TMJ, and that he needed to go to the nearest emergency department.
He presented to the emergency room and was admitted. On physical examination, the patient had a large swelling and tenderness in his left periauricular area, with erythema and deviation of the right mandible. This limited the patient's ability to open the mouth to about 10-15 mm. His white blood cell count was elevated at 22.5 × 103 cells/ml. All other laboratory values were within normal limits. Antibiotic treatment was deferred until culture and susceptibility could be obtained. Computed tomography showed mild asymmetric soft tissue swelling in the left pharyngeal region and the palatine tonsils, but no soft tissue swelling, asymmetry, or erosive changes around the mandible were noted [Figure 1]. Magnetic resonance imaging was then ordered and a large left TMJ effusion was seen [Figure 2]. Two milliliters of turbid fluid was withdrawn from the joint space via needle aspiration. He reported immediate improvement in his symptoms s/p removal of this fluid. Gram stain (which was negative), culture, and sensitivity of the specimen was carried out, which showed coagulase-negative staphylococcus sensitive to vancomycin and ceftriaxone. On the 2nd day, the patient's white blood cell count dropped to 13.6 × 103 cells/ml. On the 3rd day of the hospital stay, all of the patient's laboratory values were within normal limits and he was discharged home in stable condition on intravenous vancomycin and ceftriaxone for 2 weeks with home care. Ceftriaxone was started for gram negative coverage and vancomycin for gram positive most notably methicillin-resistant Staphylococcus aureus.
Figure 1.
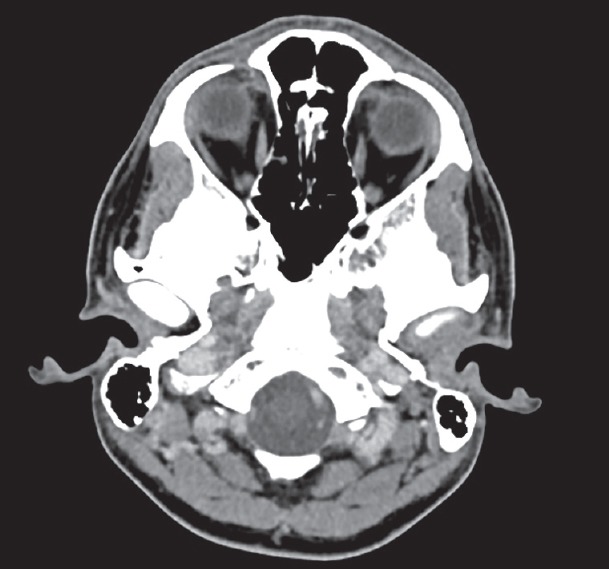
CT of TMJ Joints. CT = Computed tomography, TMJ = Temporomandibular joint
Figure 2.
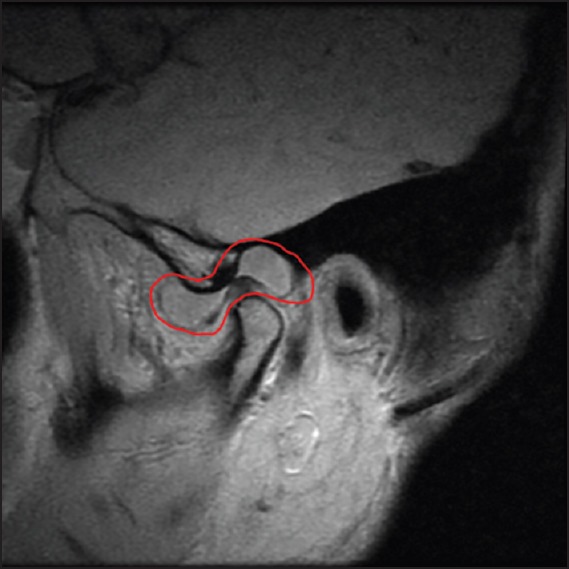
MRI of left TMJ joint with effusion circled. MRI = Magnetic resonance imaging
Discussion
The general term used to describe pain in the TMJ region with opening and closing of the mouth is temporomandibular disorder.[4] Osteoarthritis is the most common cause of temporomandibular disorder, though it can be caused by any type of arthritis.[5] In children, juvenile rheumatoid arthritis is the most common cause of temporomandibular disorder.[6] Septic arthritis of the TMJ is a rare occurrence that has only been reported 33 times in literature.[1]
Septic arthritis of the TMJ is an infectious process most often caused by Staphylococcus aureus, Streptococcus, Pseudomonas aeruginosa, and Escherichia coli. Symptoms typically present as swelling, erythema, pain, tenderness, and limited range of motion of the TMJ. Many patients may misidentify it as ipsilateral earache or temporal headache due to anatomical proximity. Pain may be worse at night if bruxism is present, and may wake the patient from sleep. Staphylococcal infections are associated with pustules and vesicles on the skin, while polyarticular involvement is associated with viral infection. Regardless of the site of infection, the differential diagnosis should include vasculitis, crystal-associated arthritis, drug-induced arthritis, and reactive arthritis.
If septic arthritis is suspected, a prompt computed tomography is recommended, because it carries a high rate of morbidity if not promptly treated. Further evaluation should be done with magnetic resonance imaging if the computed tomography is negative and there is a high clinical suspicion. If radiological imaging confirms the presence of an effusion, the joint should be aspirated. The aspirate should be examined for color and turbidity and sent to the lab for gram stain, culture, and sensitivity. Although gram stain is less than 60% sensitive for detecting bacteria in the synovial fluid, cultures are positive more than 90% of the time and are considered to be the only way to definitively diagnose septic arthritis.[7] It is important to note that culture is only positive about 25% of the time in gonococcal arthritis which can present with similar symptoms. In this case, polymerase chain reaction testing should be used as it has a 96% specificity for Neisseria gonorrhea.[8] Urine PCR for gonorrhea and chlamydia urine polymerase chain reaction were negative for this patient. Other rare causes that may present with similar symptoms include fungal infection and Lyme disease.[9,10]
Although joint aspiration is needed to make a diagnosis, it is also a part of the treatment. Empiric antibiotics should be held until the joint aspiration is performed, as it may result in negative culture. Vancomycin, ceftriaxone, and ceftazidime are used to treat gram positive cocci, gram negative cocci, and gram negative rods, respectively. Additionally, ceftriaxone is used in the treatment of gonococcal arthritis. Although septic arthritis results in some loss of joint function in roughly 40% of all cases, septic arthritis of the TMJ seems to have a better prognosis, with most cases having complete recovery.[11] Prompt treatment is still of utmost importance, as any complications lead to a significant decrease in the ability to open the mouth.[12]
Conclusion
Although overall septic arthritis of the TMJ is rare, it seems to have a more favorable prognosis than septic arthritis of other joints. Complications often results in a significant inability to open the mouth, which has a significant impact on lifestyle. If suspected, prompt treatment, prompt computed tomography or magnetic resonance imaging, followed by arthocentesis is advised for diagnosis and treatment.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest
References
- 1.Goldschmidt MJ, Butterfield KJ, Goracy ES, Goldberg MH. Streptococcal infection of the temporomandibular joint of hematogenous origin: A case report and contemporary therapy. J Oral Maxillofac Surg. 2002:1347–53. doi: 10.1053/joms.2002.35736. [DOI] [PubMed] [Google Scholar]
- 2.Sembronio S, Albiero AM, Robiony M, Costa F, Toro C, Politi M. Septic arthritis of the temporomandibular joint successfully treated with arthroscopic lysis and lavage: Case report and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:e1–6. doi: 10.1016/j.tripleo.2006.08.028. [DOI] [PubMed] [Google Scholar]
- 3.Kim HM, Kim TW, Hwang JH, Lee DJ, Park NR, Song SI. Infection of the temporomandibular joint: A report of three cases. J Korean Assoc Oral Maxillof Surg. 2011;37:510–14. [Google Scholar]
- 4.National of Dental and Craniofacial Research, TMJ Disorders. [Accessed March 24, 2015]. at http://www.nidcr.nih.gov/oralhealth/Topics/TMJ/TMJDisorders.htm .
- 5.de Souza RF, Lovato da Silva CH, Nasser M, Fedorowicz Z, Al-Muharraqi MA. Interventions for the management of temporomandibular joint osteoarthritis. Cochrane Database Syst Rev. 2012;4:CD007261. doi: 10.1002/14651858.CD007261.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ringold S, Cron RQ. The temporomandibular joint in juvenile idiopathic arthritis: Frequently used and frequently arthritic. Pediatr Rheumatol Online J. 2009;7:11. doi: 10.1186/1546-0096-7-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Faraj AA, Omonbude OD, Godwin P. Gram staining in the diagnosis of acute septic arthritis. Acta Orthop Belg. 2002;68:388–91. [PubMed] [Google Scholar]
- 8.Center of Disease Control and Prevention. Recommendations for the laboratory-based detection of Chlamydia trachomatis and Neisseria gonorrhoeae--2014. MMWR Recomm Rep. 2014;63:1–19. [PMC free article] [PubMed] [Google Scholar]
- 9.Willis AA, Widmann RF, Flynn JM, Green DW, Onel KB. Lyme arthritis presenting as acute septic arthritis in children. J Pediatr Orthop. 2003;23:114–8. [PubMed] [Google Scholar]
- 10.Bariteau JT, Waryasz GR, McDonnell M, Fischer SA, Hayda RA, Born CT. Fungal osteomyelitis and septic arthritis. J Am Acad Orthop Surg. 2014;22:390–401. doi: 10.5435/JAAOS-22-06-390. [DOI] [PubMed] [Google Scholar]
- 11.Shirtliff ME, Mader JT. Acute septic arthritis. Clin Microbiol Rev. 2002;15:527–44. doi: 10.1128/CMR.15.4.527-544.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gayle EA, Young SM, McKenna SJ, McNaughton CD. Septic arthritis of the temporomandibular joint: Case reports and review of the literature. J Emerg Med. 2013;45:674–8. doi: 10.1016/j.jemermed.2013.01.034. [DOI] [PMC free article] [PubMed] [Google Scholar]


