Abstract
Sleep is a restorative behavior essential for health. Poor sleep has been linked to adverse health outcomes among older adults, however, we know little about the social processes that affect sleep. Using innovative actigraphy data from the National Social Life, Health and Aging Project (N=727), we considered the role of marriage, positive marital relationship support, and negative marital relationship strain on older adults’ (aged 62–90) self-reported and actigraph-measured sleep characteristics. We found that married older adults had better actigraph-estimated but not self-reported sleep characteristics than the unmarried. However, among the married, those who reported more negative aspects of their marital relationship reported more insomnia symptoms, with the association reduced when psychosocial characteristics were added to the model. The married who reported more positive aspects of their marital relationship showed better actigraph-estimated sleep characteristics; taking characteristics of the physical and mental health and home environment into account reduced this association.
INTRODUCTION
On average, people spend from one-third to one-fourth of the 24-hour day sleeping. Adequate sleep is vital for individual health and well-being (Cappuccio et al. 2009; Knuston et al. 2006; Mallon, Broman, and Hetta 2002; Phillips and Mannino 2007; Schwartz et al. 1998). While sleep is an important health behavior with dramatic consequences for health and functioning, it has received relatively little attention from social scientists. This appears to have changed recently; in a series of papers, Burgard and Ailshire show that those with strained family relationships report more sleep problems (Ailshire and Burgard 2012) and differences in family responsibilities generate substantial gender gaps in sleep outcomes, including reports of more interrupted sleep and longer self-report sleep duration in women (Burgard 2011; Burgard and Ailshire 2009, 2013).
While these studies offer considerable insights into the role of family in sleep, marriage has not been a focus. Since marital status and relationship quality are strongly associated with mental and physical health and health behaviors (Umberson et al 2006; Waite and Gallagher 2001; Waite 1995), there is every reason to believe that they are associated with sleep. Furthermore, most prior studies pay little attention to the mechanisms through which family relationships influence sleep, and all used sleep characteristics as reported by the individual. Sleep is a multi-dimensional behavior, some aspects of which may not be captured in self reports. Finally, many of the prior studies focus on adults younger than 65 (Arber, Bote, and Meadows 2009; Ailshire and Burgard 2012; Burgard 2011; Burgard and Ailshire 2013; Hale 2005; Hill, Burdette, and Hale 2009; Knudsen, Ducharme, Roman 2007). Older adults comprise 13% of the U.S. population and the share is expected to rise to 19% by 2030 (Population Reference Bureau 2011). Sleep disorders and complaints about sleep are more common among older adults (Neikrug and Ancoli-Israel 2010) and poor sleep at older ages has been linked to many adverse cognitive and physical outcomes (Brassington, King, and Bliwise 2000; Faubel et al. 2009; Phillips and Mannino 2007). Understanding the social determinants of older adults’ sleep may also have practical significance in promoting the health and well-being of U.S. older adults
This study investigates the role of marital status and relationship quality and sleep characteristics among older adults. As relatively few older adults are cohabiting (n=25, 3.5% of the sample), we combine cohabitors with the married throughout and, for brevity, refer to them as “married”. This paper makes two unique contributions. First, we use sleep characteristics as measured by actigraphy (Lauderdale et al. 2014) in addition to self-assessments given in response to survey questions. Second, we theorize the processes through which marriage influence sleep and carefully consider characteristics that may mediate or confound the association between marital status, relationship quality and characteristics of older adults’ sleep. Results from this study contribute to our understanding of the social context of health among older adults and to a broader conceptualization of the social nature of human sleep.
BACKGROUND
An Introduction to Sleep
Sleep is a universal human behavior characterized by reduced consciousness and relatively suspended sensory activity of the body. All humans require sleep, which provides energy for the brain and for physical activities, although the physiological functions of sleep are not fully understood. Thus, sleep is one of the most important restorative behaviors for an individual’s health and well-being. While it seems intuitively obvious that sleep is essential to life, defining what constitutes a good night’s sleep is not straightforward. Sleep is a complicated behavior with multiple dimensions that include duration, consolidation, and restfulness. A good night’s sleep may mean adequate sleep time, few or no awakenings during the night, or feeling rested in the morning. While feeling rested requires self-evaluation, other sleep characteristics such as duration and consolidation are better obtained through direct assessments. Further, recent evidence suggests that characteristics of sleep as reported by the individual are not strongly associated with similar characteristics measured by actigraphy for that person (Chen et al., 2015). This suggests that a comprehensive evaluation of human sleep could be strengthened by investigation of people’s subjective evaluation of their sleep experience and external measurement of their sleep.
Sleep behaviors and outcomes often change with age. Complaints among older adults related to sleep are common, especially complaints about difficulty falling and staying asleep (Ancoli-Israel, 2009). A community study of 9,000 adults aged 65 or over found that nearly half of the respondents reported at least one insomnia symptom (Foley et al. 1995). The prevalence of sleep complaints at older ages may result from the biological aging process (Pace-Schott and Spencer 2011; Espiritu 2008; Vitiello 2006), the burden of physical illness at old ages (Foley, Ancoli-Istael, Britz, and Walsh 2004), or changes in the social environment and relationships over the life course (Ailshire and Burgard 2012; Burgard 2011; Burgard and Ailshire 2013). However, because of the difficulty in measuring multiple dimensions of sleep in surveys, the vast majority of sleep research with direct assessments of sleep outcomes is clinic-based, includes a non-representative patient population, and collects sleep data in a clinical sleep laboratory. We thus know more about the role of the human aging process and physical illness in older adults’ sleep outcomes than about the effects of social conditions. While a few studies suggest that older adults’ sleep outcomes are influenced by social processes and environment (Zepelin, McDonald, and Zammit 1984 ; Wilcox and King 1999), our knowledge of the social correlates and determinants of sleep remains limited.
Social processes, however, do not directly affect sleep in most cases. They determine sleep via their influence on key proximate factors of sleep which include the physical environment, and individuals’ own physical and mental health status. Yet, relatively few prior studies have considered the roles of these proximate factors in linking social processes and sleep. Furthermore, we propose that social processes can affect multiple dimensions of sleep. Prior studies on health point to the powerful role of social factors in shaping various dimensions of the same health construct. For example, studies have found that social relationships influence self-perceived stress and objective assessment of stress by cortisol level (Kawachi and Berkman 2001; Seeman et al. 1994), although the strength of association varies. It is quite likely that marriage influences multiple aspects of sleep outcomes. However, since our purpose is to understand how marital status influences sleep in a general way instead of comparing different aspects of each dimension of sleep in the older population, we use “sleep” as an overarching concept in the discussion of our conceptual framework. In the following section, to better understand the role of marriage on older adults’ sleep, we mobilize theoretical perspectives on marriage and health to argue that marriage can exert powerful effects on proximate factors of sleep, which in turn affect sleep characteristics of older adults.
Theoretical Perspectives on Marriage and Sleep: The Resource Model
Marriage is a key social relationship that affects almost every aspect of individual well-being over the life course, including emotional and physical health. One theoretical perspective links the social institution of marriage to health through the resources it brings to the partners. The long-term commitment and shared fate that lie at the core of the marriage bargain, recognized socially, legally and religiously, fosters shared resources. In literature, the discussion of resources often distinguished material and time resources from social and emotional resources associated with marriage. Since these two types of resources appear to affect sleep though different mechanisms, we discuss them separately.
Material and Time Resources
Marriage brings material resources and time investments in each other. Thus, the married tend to gain greater financial well-being, and companionship through increasing time in shared activities such as eating, leisure activities, and sexuality compared to the unmarried (Waite, 1995; Waite and Gallagher, 2001). The better material conditions of the married reduce exposure to many kinds of risks and stress and increase their ability to deal with it. Material resources tend to buffer against or decrease health consequences of unexpected events. Many of these benefits also accrue to cohabiting couples, although perhaps to a lesser extent (Waite & Gallagher 2001). Recent research has also pointed to the benefits of marriage for the order and cleanliness of the household through greater role clarity and specialization compared to other living arrangements (Cornwell, 2014), suggesting a favorable physical environment as another resource that is available for married people.
The greater resources that tend to be available to the married can be deployed to achieve better physical and mental health, which may improve sleep outcomes. Married individuals have better physical health outcomes than the unmarried, including fewer chronic conditions and mobility limitations at mid-life, and lower levels of both depressive symptoms (Hughes and Waite 2009) and loneliness (Hawkley et al. 2008). Because many chronic diseases or conditions affect sleep quantity and quality, older adults with fewer medical problems are less likely to report insomnia symptoms (Foley et al. 2004). In addition, marriage reduces risky health behaviors. Having a spouse to look after you matters for health behaviors. Prior studies observed a reduction of excess alcohol consumption and tobacco use associated with marriage (Duncan, Wilkerson, England 2006; Fleming, White, Catalano 2010; Leonard and Rothbard 1999). Clinical and epidemiological studies indicated that regular alcohol abuse and smoking can disrupt sleep (Roehrs and Roth 2001; Zhang et al. 2006). The lower level of risky health behaviors may also lead to better physical outcomes at older ages, which in turn may promote better sleep. Taken together, the spousal relationship is expected to improve older adults’ sleep outcomes because the material and time resources it brings into to the relationship promote better physical health and health-related behaviors.
Furthermore, the resource model suggests that the spousal relationship directly influences the housing environment in which older adults live. Married people tend to live in cleaner, quieter, tidier houses in better repair than the unmarried (Cornwell 2014). A disordered home environment can directly affect the residents’ sleep. In addition, married people are wealthier than the unmarried (Waite 1995; Wilmoth and Koso 2002) such that they tend to live in better neighborhoods. A large literature has documented the importance of neighborhood social conditions for individual health (Ross and Mirowsky 2001), including sleep (Hill, Burdette, and Hale 2009). As such, the environment of the home itself and of the neighborhood in which it is situated may be an important mechanism through which marriage promotes better sleep.
Emotional and Social Resources
A second set of resource brought by marriage is emotional support and social integration. Aside from material, time, and physical resources, the better health outcomes of married people also come from the provision of a sense of companionship and belonging. Married people are much more likely to have a confidant than the unmarried, and to have someone who listens to them and is concerned with their health and well-being. For a married man this person is usually his wife (Umberson, 1992). Being able to talk to another person about things that are bothering you reduces the effects of stress for both mental and physical health (Holt-Lunstadt and Birmingham 2008; Thoits 2011). Because individuals’ social networks shrink with age, older adults often have relatively few confidants (McPherson, Smith-Lovin, and Brashears 2006; Schnittker 2007). Older adults are less close to their network members, on average, and have fewer non-primary group ties than younger adults (Cornwell, Laumann, Schumm 2008). Thus older adults tend to be more dependent on their spouse or partner for social support and companionship, and reliance on marriage or marriage-related networks increases with age (Curan, McLanahan and Knab 2003). As the primary focus of social relationships gradually shifts with age, spousal relationships play a vital role in providing instrumental and emotional support and a sense of social integration. In fact, a large literature has pointed to the importance of spousal relationships for the health of older adults (Warner and Kelley-Moore 2012). As for younger adults, those who are married or live with a partner are in general healthier, happier, and live longer due in part to the emotional support, and companionship that marriage provides (Hughes and Waite 2002; Lund et al. 2002; Michael et al. 2001; Sarwari et al. 1998).
The provision of emotional support makes marriage an important determinant of psychological well-being (Brown 2000; Gove, Hughes, and Style 1983; Kim and McKenry 2002), which in turn promotes good sleep at night. A spouse or partner also offers companionship, which tends to reduce feelings of loneliness, depressive symptoms and social isolation (Hawkley et al 2008). Clinical and epidemiological studies demonstrate that loneliness undermines sleep quality (Cacioppo et al. 2002; Kurina et al. 2011). The companionship provided by a spouse/partner may support better sleep. Furthermore, a spouse or partner may provide emotional support, a sense of security, or information that buffers the effects of stressful events (Thoits, 2011), which seems to be particularly the case for mental health outcomes (Pearlin and Johnson 1977). While a lack of sleep may contribute to depression, it is well-documented that depression leads to sleep problems (Lopresti, Hood, and Drummond 2013). Additionally, given that insomnia is an important symptom of poor mental health (Harvey 2001), this may be a particularly important pathway from marriage to sleep outcomes; marriage may affect sleep via its influence on psychological well-being and mental health. Finally, a high level of social integration is tied to greater social control, which can promote positive health behaviors as well as better sleep habits (Umberson 1987), which may also promote better sleep outcomes of older adults.
Theoretical Perspectives on Marriage and Sleep: The Stress Model
While being married tends to provide material and other resources, emotional support and sense of social integration, all of which are important inputs to health, the quality of the relationship matters a great deal for both the resources and support available to the married and for their exposure to and recovery from stress. This leads to another theoretical perspective on marriage and health. The stress perspective points to the dark side of marriage (Thoits 2011; Robles and Kiecolt-Glaser 2003). Poor quality marriages produce less specialization, less investment, less companionship, and are themselves a source of stress due to conflict and demands, with consequences for immune function, illness and self-rated health (Coyne and Delongis 1986; Levenson and Gottman 1985; Seeman 2000). In addition, a poor spousal relationship seems to interact with the aging process to accelerate the decline of self-rated health with age (Umberson et al. 2006) and amplify the impact of physical illness and functional limitations on mental health (Bookwala and Franks 2005; Warner and Kelley-Moore, 2012).
From this perspective, while marriage can promote better sleep outcomes, the effect is conditional on marital quality. A negative marital relationship could also undermine sleep through its influence on physical health, psychological well-being, and the household environment. Relational conflicts and demands represent a major source of stress and diminish mental as well as physical health. Poor marital quality is associated with anxiety and depression (Cascardi, Langhinrichsen, and Vivian 1992; Choi and Marks 2008). Being in a poor marital relationship also increases the chances of functional impairment, inflammation, injuries, and poor self-rated health (Cascardi, Langhinrichsen, and Vivian 1992; Choi and Marks 2008; Donoho, Crimmings, and Seeman 2013; Umberson et al. 2006). In addition, conflictual or stressful interactions between spouses may lead to household disorder and make the household environment generally less favorable. All these changes can damage sleep and reduce sleep quality. Moreover, some studies suggest that the negative aspect of social relationships may be more consequential than positive dimensions for individual health (Ailshire and Burgard 2012). Thus, we expect that the relationship strain and demands that accompany poor marital quality increase the chances of sleep disturbances and sleep problems.
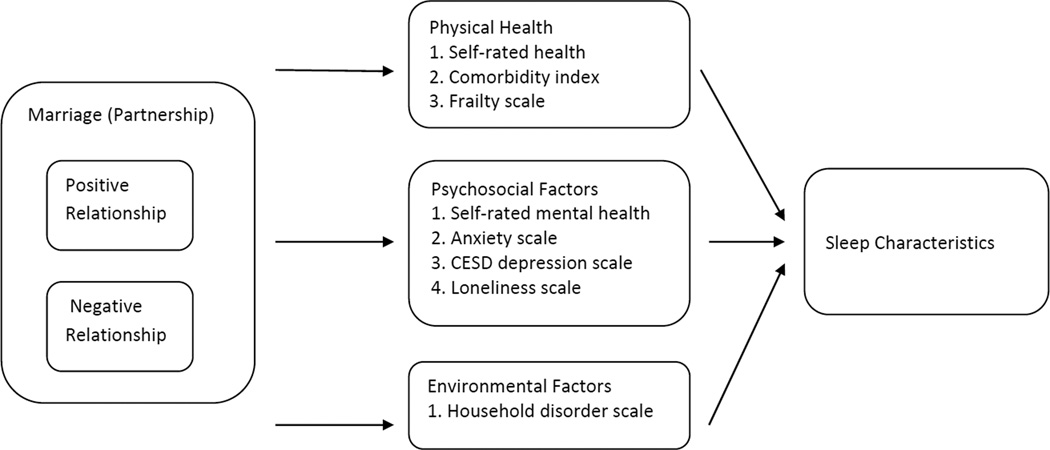
These theoretical perspectives linking marriage and health point to the powerful but complex processes through which spousal/partner relationships and relationship quality can affect health. These processes, as we have argued, also affect older adults’ sleep characteristics and sleep quality. In sum, previous studies suggest that better marital quality will improve sleep and poor marriage quality will harm sleep. Since the spousal/partner relationship can be a source of support or strain, these theoretical perspectives provides little guidance on the overall direction of the association between partnership status and sleep characteristics. Finally, given the strong evidence on the link between marriage and factors proximate to sleep, including physical health, psychological well-being, and the household environment, we expect that the associations between marital status, relationship quality and sleep will be to, some extent, mediated or confounded by these factors. Figure 1 illustrates and summarizes these mechanisms.1
Figure 1.
Proposed Pathway of Influence: Marriage/Partnership to Sleep Outcomes
METHODS
National Social Life, Health and Aging Project
The National Social Life, Health, and Aging Project (NSHAP) is a population-based, longitudinal study of health, social life, and well-being among older Americans (Waite et al., 2010). A nationally-representative probability sample of community-dwelling individuals aged 57–85 was selected from households across the U.S. screened in 2004. African-Americans, Latinos, men and the oldest-old (75–84 years at the time of screening) were over-sampled. The first wave of data collection was conducted in 2005– 2006 and the second wave was conducted in 2010–2011. The second wave of data collection also extended the sample to include the spouses and cohabiting partners of Wave 1 respondents. This yielded a total of 3,377 individuals (1,539 men and 1,838 women) with completed Wave 2 interview data.
The second wave of NSHAP included a new module on daytime activity and sleep, with a randomly selected one-third of the primary respondents and their spouses. Of 1117 selected individuals, 897 agreed (220 refused) to participate. A wrist actigraph and activity and sleep booklet then were mailed to each participant to collect information about the respondent’s sleep and activity levels over three full days (72 hours total). Eventually, 819 individuals completed this substudy, with usable actigraphy data obtained for 780. We exclude the 53 spouses or partners younger than 62 or older than 90 as not representative of U.S. older adults in our target age range, yielding a sample of 727 individuals aged 62 to 90. Detailed socio-demographic data on individuals were obtained from the Wave 2 master file and linked to the corresponding actigraphy data.
Measures
Self-reported sleep characteristics
Survey measures of sleep characteristics included self-reported hours of sleep and sleep quality. First, each respondent was asked to report his or her usual bedtime and wake up time, separately for weekdays and weekends: “What time do you usually go to bed and start trying to fall asleep?” and “What time do you usually wake up?”2 Using this information, we calculated each respondent’s usual sleep duration for weekdays and weekends separately. Next, we multiplied weekday sleep duration by five and weekend sleep duration by two and divided by seven to obtain an estimate of self-reported average weekly total sleep time. Second, NSHAP also included four questions on sleep quality, each asking about the frequency of a sleep characteristic. These four questions, drawn from the sleep questions module in the Health and Retirement Study (HRS), were: “How often do you have trouble falling asleep?”, “How often do you have trouble with waking up during the night?”, “How often do you have trouble with waking up too early and not being able to fall asleep again?”, and “How often do you feel really rested when you wake up in the morning?”. Response categories for these questions were: most of the time = 2, sometimes = 1, rarely or never = 0. Factor analysis showed that these five items loaded onto a single factor. We created a troubled sleep scale, ranging from 0 to 8, by summing all items (after reverse coding the last one). We standardized the score based on our final sample. The troubled sleep scale has an alpha of 0.66.
Actigraph-estimated sleep characteristics
The NSHAP used actigraphy to measure sleep characteristics of respondents. Actigraphy is a valid and unobtrusive approach to measuring sleep without disrupting routine behavior; sleep characteristics measured by actigraphy are moderately to highly correlated with those measured by polysomnography, (Ancoli-Israel et al. 2003 ; Blackwell et al. 2008). The Actiwatch (Philips/Respironics 2010) records intensity and frequency of movement using a piezoelectric linear accelerometer with 15-second epochs. The Actiwatch continually registers wrist movements, and the sum of all wrist movements during each 15-second epoch is saved as an activity score. Data from the Actiwatch were downloaded and analyzed using the manufacturer’s Actiware software version 5.59 (Philips/Respironics 2010). In the present study, we focused on four actigraph-estimated sleep characteristics that have often been used in previous studies (Chen et al., 2015; Lauderdale et al., 2014): (1) total sleep time (defined as the total duration of all epochs scored as sleep within the major sleep interval, that is the time from the first epoch scored as sleep to the last epoch scored as sleep for the primary sleep interval in each 24 hours, (2) percent sleep (defined as the percent of the sleep interval that is actual sleep), (3) sleep fragmentation index (ranging from 0–100), an indicator of sleep disruption that is the sum of two percentages: the percentage of the sleep interval spent moving and the percentage of immobile periods (i.e., contiguous epochs with no movement) that are no longer than one minute, and (4) wake after sleep onset (defined as the total minutes awake during the sleep interval). Percent sleep, sleep fragmentation, and wake after sleep onset are sleep quality indicators as measured by the actigraph. For each of the actigraph-estimated sleep characteristics, we calculated an average value over three nights for each respondent.
Partnership status and relationship quality
Each respondent was asked whether he or she lived with a spouse or unmarried partner in the household. The answer was used to create a binary indicator of partnership status. Since cohabitation was rare in this population (n=25, 3.5%), we combine the cohabiting with the married and simply refer to them all as “married.” We also performed sensitivity analyses that omitted the cohabiting. We followed the approach developed by Warner and Kelley-Moore (2012) and modified by Galinsky and Waite (2014) to create two factor scales of marital quality. These two scales were derived from 9 items. Each married respondent answered a series of questions assessing their spousal/partner relationship. These are: (1)” How often can you open up to your spouse if you need to talk about your worries?” (2) “How often can you rely on your spouse for help if you have a problem?” (3) “How often does your spouse make too many demands on you?” (4) “How often does your spouse criticize you?” and (5) “how often does your spouse get on your nerves?” The four responses categories ranged from “hardly ever or rarely = 1” to “often = 4”.
In addition, all partnered or married respondents were asked: (6) how close they felt their relationship with their spouse was, with answers from not very close, somewhat close, very close to extremely close, (7) how happy their relationship with their spouse was, with answers ranging from very unhappy (coded as 1) to very happy (coded as 7), (8) how they liked to spend their free time with options including doing things together with the spouse, doing some things together, and doing things separately, and (9) how emotionally satisfying they found their sexual relationship with their spouse or partner to be, with options of extremely satisfied, very satisfied, moderately satisfied, slightly satisfied, or not at all satisfied (Kim and Waite, 2014).
To form relationship quality scales, we performed exploratory factor analysis, which loaded these 9 items into 2 factors. We referred to the first factor as positive marital relationship (α =0.68) and the second factor as negative marital relationship (α =0.58). The positive relationship scale included five items: rely on partner, open up to partner, relationship happiness, relationship closeness, and time with partner. The negative relationship scale included three items: partner criticizing, making demands, and getting on nerves. Two factor scales were derived from the factor analysis.
Physical Health and Behavior
We have included three indicators of older adults’ physical health: self-rated health, a modified Charlson Co-Morbidity Index, and a Frailty Scale. First, the self-rated health was assessed with the question: “Would you say your health is excellent, very good, good, fair, or poor?” We treated the variable as a continuous measure. Higher values indicated better health. Second, the NSHAP included a wealth of information on respondents’ chronic conditions. During the interview, each participant was asked “Has a medical doctor told you have (had) [condition]?” The list of conditions included heart attack/myocardial infarction, congestive heart failure, procedure for coronary artery disease, stroke/cerebrovascular disease, diabetes, leukemia/lymphoma, metastatic cancer, COPD/asthma, rheumatoid arthritis, and Alzheimer's dementia or another form of dementia. These chronic conditions were combined into a modified Charlson Co-Morbidity Index following the procedure described by Vasilopoulos et al. (2014). The original Charlson Co-Morbidity Index was developed to assess the severity of comorbid conditions based on its power to predict mortality. Conditions that were associated with higher mortality were given more weights in the calculation of the index score (Charlson, Pompei, Ales, MacKenzie 1987). The index can be produced by review of medical record or questionnaire. The questionnaire version of the Charlson index is highly correlated with the medical record-based version and allows for the assessment of the comorbidity of the general population of older adults (Katz, Chang, Sangha, Fossel, Bates 1996). Our modified index ranged from 0 to 16. Higher values indicated more serious conditions with higher mortality risk. Finally, there are several functional assessments in the NSHAP survey. Respondents were asked how often over the last week they felt (a) everything was an effort and (b) they could not get going. Response categories included: rarely/none of the time, some of the time, occasionally, and most of the time. Respondents who answered “occasionally” or “most of the time” to at least one of the questions were coded as having exhaustion. Respondents were also asked to report their frequency of participation in vigorous activity or exercise (defined as 30 minutes or more of sports, exercise classes, or physical labor). Answer choices included 5 or more times per week, 3 or 4 times per week, 1–2 times per week, 1–3 times per month, less than 1 time per month, and never. Respondents were considered as low physical activity if they reported “1–3 times per month”, “less than 1 time per month”, or “never”. In addition to the two survey questions, NHSAP included two direct assessments of respondents’ functional status: gait speed assessment and chair stand assessment. Detailed information of these two tests was described elsewhere (Huisingh-Scheetz et al. 2014). Drawing information from these survey questions and assessments, we created a 4-point frailty scale (Huisingh-Scheetz et al. 2014). Higher scores indicated a greater level of frailty.
Psychosocial Factors
The present study focused on four psychosocial factors: self-rated mental health, anxiety, depressive symptoms, and loneliness (Payne et al. 2014). First, respondents were asked to rate their mental health as excellent, very good, good, fair, or poor. We treated this as a continuous variable, recoding it so that higher values indicated better mental health. Second, NSHAP included 7 anxiety items from the Hospital Anxiety and Depression Scale (Zigmond and Snaith 1983). Higher value indicated high level of anxiety. Next, NSHAP included a shortened version of the Center for Epidemiologic Studies Depression Scale (CESD-10). The CESD-10 score ranged from 0–30 and is a widely used instrument for the identification of major depression in older adults (Irwin et al. 1999). Finally, NSHAP included items from the short loneliness scale developed by Hughes et al. (2004). These scales are described in Table 1 (Payne et al. 2014).
Table 1.
Weighted Descriptive Statistics, National Social Life, Health, and Aging Project 2010–2011
| Full sample | Married | Unmarried | |
|---|---|---|---|
| Mean or proportion | Mean or proportion | Mean or proportion | |
| Social and demographic characteristics | |||
| Female (proportion) | 0.54 | 0.52 | 0.66 |
| Age | 71.79 | 70.44 | 75.17 |
| Education | |||
| Less than high school (proportion) | 0.14 | 0.14 | 0.14 |
| High school of equivalent (proportion) | 0.30 | 0.28 | 0.33 |
| Some college (proportion) | 0.34 | 0.33 | 0.37 |
| College or higher (proportion) | 0.22 | 0.25 | 0.16 |
| Race and ethnicity | |||
| White (proportion) | 0.83 | 0.84 | 0.80 |
| African American (proportion) | 0.07 | 0.06 | 0.09 |
| Hispanic (proportion) | 0.06 | 0.06 | 0.07 |
| Others (proportion) | 0.04 | 0.04 | 0.04 |
| Median Household Income (thousand dollars) | 40 | 50 | 24 |
| Median Household Assets (thousand dollars) | 250 | 300 | 100 |
| Retired (proportion) | 0.74 | 0.73 | 0.77 |
| Physical Health | |||
| Self-rated physical health | |||
| Poor (proportion) | 0.04 | 0.03 | 0.04 |
| Fair (proportion) | 0.16 | 0.15 | 0.18 |
| Good (proportion) | 0.31 | 0.31 | 0.33 |
| Very good (proportion) | 0.34 | 0.34 | 0.32 |
| Excellent (proportion) | 0.15 | 0.16 | 0.12 |
| Charlson comorbidity index (0–16) | 1.01 | 0.97 | 1.08 |
| Frailty Scale (0–4) | 0.94 | 0.85 | 1.09 |
| Psychosocial Wellbeing | |||
| Self-rated mental health | |||
| Poor (proportion) | 0.01 | 0.01 | 0.02 |
| Fair (proportion) | 0.08 | 0.08 | 0.09 |
| Good (proportion) | 0.32 | 0.31 | 0.33 |
| Very good (proportion) | 0.39 | 0.41 | 0,34 |
| Excellent (proportion) | 0.21 | 0.20 | 0.22 |
| Anxiety scale (0–21) | 5.72 | 5.50 | 5.81 |
| CES-D (0–33) | 3.94 | 3.37 | 5.12 |
| Loneliness scale (0–9) | 6.23 | 5.92 | 6.82 |
| Household Environment | |||
| Household disorder scale (5–35) | 11.53 | 10.90 | 12.83 |
| Relationship characteristics | |||
| Married or lived with a partner (proportion) | 0.67 | na | na |
| Mean positive marital relationship factor score | na | 0.13 | na |
| Mean negative marital relationship factor score | na | −0.10 | na |
| Self-report sleep characteristics | |||
| Total sleep time | 493 | 494 | 491 |
| Troubled sleep scale (0–12) | 5.85 | 5.77 | 6.03 |
| Actigraph-estimated sleep characteristics | |||
| Total sleep time (minutes) | 435 | 436 | 432 |
| Sleep fragmentation | 14 | 14 | 16 |
| WASO (minutes) | 39 | 36 | 45 |
| Sample Size | 727 | 506 | 221 |
Household Environment
Lastly, we included an indicator of household disorder. At the end of the interview, every interviewer was instructed to rate the respondent’s housing conditions on the following dimensions: cleanliness, neatness and tidiness, noise, spaciousness, clutter, and odor. Ratings ranged from 1 to 5 for each dimension. We constructed a household disorder scale by summing all these items (positive items were reverse coded). This scale is a modified version of household disorder scale developed by Cornwell (2014) and has high reliability.
Other Covariates
Respondent’s education was categorized as less than high school, high school or equivalent, some college education, bachelor’s degree or higher. Race and ethnicity distinguished white, African American, Hispanic, and Other. A dichotomous variable indicated whether the respondent was retired at the time of the interview. Log household income and log household assets were used as indicators of respondents’ economic standing. We also controlled for gender3 and age.
Analytic strategy
We began with weighted descriptive statistics of older adults in the NSHAP sample. Next, we examined the relationship between marital status, relationship quality, and sleep characteristics adjusted for social and demographic characteristics using survey weighted ordinary least square regressions and clustered by families to account for the nesting of individuals within households. Because members of the same household (in this case, a husband and a wife) influence each other, this might violate the assumption of independent observations in traditional linear models which result in underestimation of standard errors. However, multilevel models were not ideal for NSHAP data for two main reasons. First, NSHAP data is not a multilevel data by design. Household is not a unit in the sample selection process. In the second wave, the survey team sampled eligible older adults and, if the selected respondent lived with a spouse or a partner, he or she was also invited to participate in the survey. As such, NSHAP does not have weights for households. Furthermore, since the sampling unit is individuals not households, the average number of level-1 observations per level-2 unit is very small. Here we had 727 older adults residing in 585 households. This resulted in only an average of 1.2 observations per household resulting in “data sparseness” when fitting the multilevel model. The problem of data sparseness can lead to overestimation of standard errors and reduce the ability to detect significant associations between (Clarke and Weaton 2007; Clarke 2008). Because of these issues, instead of fitting the data using multilevel models, we employ survey weighted least square regression models with clustering by household.
We performed two sets of analyses. The first set assessed the association between marital status and self-reported and actigraph-estimated sleep characteristics. The second set of analyses examined the associations between relationship quality (as measured by positive relationship and negative relationship scales) and sleep characteristics among those married or partnered. We used multiple imputation to account for potential biases resulting from missing data in the control variables and mediators. Multiple imputation involves replacing missing values with predictions based on other observed variables using Monte Carlo techniques (Rubin 1987). In contrast to single imputation, which replaces each missing value with a predicted value, multiple imputation replaces several missing values with repeated imputations using available covariates, creating several complete datasets. The combined results produce better estimates of the missing values that create uncertainty around the missing data (Allison 2001; Hawkley et al. 2014). All regression analyses were survey weighted using Stata 13 (StataCorp 2011).
RESULTS
Descriptive statistics
Table 1 presents weighted descriptive statistics. The first column shows the descriptive statistics for 727 respondents. About 54% of the sample was female. The average age was 72. A majority of respondents were White (83%), retired (74%), and had at least a high school level of education (86%). The respondents had a median household income of approximately forty thousand dollars and median household assets of approximately two hundred and fifty thousand dollars. The great majority of respondents reported their physical and mental health as good, very good, or excellent.
On average, respondents reported bedtimes and wake times that produced a usual total sleep time of 493 minutes (or 8.27 hours). The mean troubled sleep scale score was 5.85 on a scale from 0–12. Turning to the actigraph-estimated sleep characteristics, the average sleep duration was 435 minutes (or 7.25 hours), respondents spent 82% of the sleep interval asleep (percent sleep), the average wake time after sleep onset (WASO) was 39 minutes, and the mean sleep fragmentation index was 14 on a scale from 0–100. Two-thirds of respondents were currently married or living with a partner. Among those married or living with a partner, the average rating of positive relationship quality was 8.08 (on a scale ranging from 0 to 10) and of negative relationship quality 1.54 (on a scale ranging from 0 to 6) showing relatively high levels of relationship quality and low levels of strain.
The second and third columns show descriptive statistics for the married and unmarried samples in the actigraphy substudy. The married sample is younger, with a higher proportion male, a higher proportion college graduates, a lower score on the frailty index. Differences between the samples in health are modest, and differences in income and assets can be accounted for by household size. The married sample shows lower scores on scales of anxiety, depressive symptoms, and loneliness and also household disorder. Differences in sleep characteristics are small to moderate. The married also show higher median income and household assets.
Marital status, relationship quality and sleep
Table 2 presents results of regressions of self-reported sleep characteristics on being married versus not married. The first model includes marital status and controls for all previously described demographic variables. The second model adds the three sets of mediators: physical health and health behaviors; psychological health; and characteristics of the household environment. Our estimates show that being married is associated with self-reported sleep duration but not associated with the troubled sleep scale. Adding demographic variables and mediators does not change the results. Married older adults report longer sleep duration but not better sleep quality. Similar to prior studies using samples of young adults, we found that marriage correlates significantly with self-report sleep duration, and the association became insignificant with the inclusion of proximate factors; nevertheless, we did not find the significant association between being married and better sleep quality, as has been reported in prior studies of younger adults (Arber, Bote, and Meadows 2009; Hale 2005).
Table 2.
Effects of Partnership Status on Self-Report Sleep Characteristics (N=727)
| Total sleep time (minutes) |
Troubled sleep scale | |||
|---|---|---|---|---|
| Model 1 | Model 2 | Model 1 | Model 2 | |
| Married or lived with a partner | 15.34† (8.60) | 12.96 (8.62) | 0.04 (0.13) | 0.12 (0.12) |
| Female | 10.65 (6.76) | 12.86 (7.61) | 0.07 (0.10) | 0.11 (0.08) |
| Age | 0.63 (0.52) | 0.47 (0.55) | 0.00 (0.01) | −0.00 (0.01) |
| Education | −11.74** (3.99) | −12.32** (3.95) | −0.04 (0.06) | 0.00 (0.05) |
| Race (Ref = White) | ||||
| African American | −19.44† (11.29) | −16.14 (12.89) | −0.00 (0.12) | −0.04 (0.13) |
| Hispanic | −25.82† (14.07) | −17.39 (14.81) | −0.28† (0.16) | −0.22 (0.16) |
| Other | 10.23 (18.29) | 10.75 (17.77) | −0.11 (0.26) | −0.03 (0.23) |
| Log household income | −10.39† (5.74) | −8.08 (6.18) | −0.11 (0.07) | −0.05 (0.07) |
| Log household assets | 0.90 (1.44) | 1.36 (1.65) | 0.02 (0.02) | 0.04* (0.02) |
| Retired | 11.43 (6.95) | 11.29 (7.24) | −0.03 (0.12) | 0.07 (0.10) |
| Physical Health | ||||
| Self-rated health | 3.68 (4.62) | −0.13** (0.05) | ||
| Charlson comorbidityiIndex | 7.15† (3.70) | 0.04 (0.03) | ||
| Frailty score | 5.97 (4.53) | 0.01 (0.05) | ||
| Psychosocial Wellbeing | ||||
| Self-rated mental health | −9.97† (5.17) | −0.08 (0.06) | ||
| Anxiety scale | 0.22 (1.39) | 0.02 (0.02) | ||
| CESD score | −0.40 (1.31) | 0.06*** (0.01) | ||
| Loneliness scale | −0.39 (2.01) | 0.05* (0.02) | ||
| Household Environment | ||||
| Household disorder scale | −1.01 (0.87) | −0.02 (0.11) | ||
| Intercept | 584.10*** (78.44) | 569.52*** (82.08) | 1.32 (1.18) | −0.40 (1.22) |
Note: Figures shown are coefficients with standard errors in parentheses. All regressions were survey-weighted and clustered by household.
p < .001,
p< .01,
p< .05,
p< .1 for two-tailed test.
Table 3 presents estimates of the associations between marital status and actigraphic sleep measures. Associations for these actigraphic measures were stronger: married individuals had longer total sleep time, and less time awake after sleep onset than the unmarried. Here we found significant associations for both sleep duration and sleep quality. The associations were statistically significant after the inclusion of demographic variables. While marital status was not associated with better self-reported sleep quality, those with a spouse or partner actually had longer total sleep time and better sleep quality as indicated by actigraph measures. However, the patterns remained almost unchanged after the inclusion of the series of mediators. There was little statistical evidence that the relationship between marital status and sleep characteristics measured by actigraph was mediated by physical health, health behaviors, psychological well-being, or the household environment.
Table 3.
Effects of Partnership Status on Actigraphis Sleep Characteristics (N=727)
| Total sleep time (minutes) |
Sleep fragmentation | WASO (minutes) |
||||
|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 1 | Model 2 | Model 1 | Model 2 | |
| Married or lived with a partner | 16.85* (8.51) | 15.33† (8.87) | −1.31† (0.69) | 1.22† (0.70) | −5.86* (2.65) | −5.25† (2.73) |
| Female | 22.93** (7.26) | 24.15** (7.51) | −1.95*** (0.48) | −1.93*** (0.49) | −3.28 (2.05) | −3.12 (1.96) |
| Age | 1.31* (0.50) | 1.19* (0.47) | 0.07 (0.05) | 0.05 (0.04) | 0.21 (0.13) | 0.15 (0.14) |
| Education | −2.18 (3.52) | −2.79 (3.48) | −0.25 (0.34) | −0.16 (0.34) | −2.10† (1.07) | −1.89† (1.01) |
| Race (Ref = White) | ||||||
| African American | −7.28 (11.81) | −1.91 (12.15) | 2.41** (0.70) | 2.19** (0.71) | 9.06** (3.17) | 8.86* (3.57) |
| Hispanic | −1.47 (8.53) | 3.58 (9.60) | 0.11 (0.78) | 0.12 (0.73) | 2.32 (3.79) | 2.98 (3.75) |
| Other | −58.75* (23.57) | −55.69* (25.41) | 0.52 (1.70) | 0.73 (1.80) | −5.21 (3.91) | −4.65 (4.08) |
| Log household income | −3.99 (4.58) | −4.81 (5.13) | −0.41 (0.41) | −0.28 (0.40) | −1.69 (1.50) | −1.49 (1.44) |
| Log household assets | 1.42 (1.46) | 1.08 (1.49) | −0.21* (0.98) | −0.16 (0.10) | −0.68 (0.42) | −0.55 (0.41) |
| Retired | 11.48 (9.07) | 11.59 (8.87) | −0.62 (0.71) | −0.43 (0.69) | −0.65 (2.46) | 0.08 (2.44) |
| Physical Health | ||||||
| Self-rated health | 4.48 (3.40) | −0.21 (0.34) | −0.51 (1.11) | |||
| Charlson comorbidityiIndex | 4.70 (3.15) | 0.23 (0.26) | 0.62 (1.05) | |||
| Frailty score | 1.02 (5.67) | 0.72* (0.33) | 1.95† (1.05) | |||
| Psychosocial Wellbeing | ||||||
| Self-rated mental health | −3.19 (4.02) | 0.21 (0.37) | −0.34 (1.32) | |||
| Anxiety scale | 0.56 (1.35) | 0.00 (0.10) | 0.12 (0.43) | |||
| CESD score | −0.76 (0.98) | 0.04 (0.08) | −0.07 (0.30) | |||
| Loneliness scale | −0.72 (1.71) | 0.04 (0.13) | 0.54 (0.58) | |||
| Household Environment | ||||||
| Household disorder scale | 0.11 (1.00) | 0.04 (0.06) | 0.25 (0.24) | |||
| Intercept | 332.26*** (66.55) | 347.06*** (71.41) | 20.00*** (4.84) | 16.65** (5.08) | 64.42** (19.41) | 48.66* (19.16) |
Note: Figures shown are coefficients with standard errors in parentheses. All regressions were survey-weighted and clustered by household.
p < .001,
p< .01,
p< .05,
p< .1 for two-tailed test.
We turn next to the association of relationship quality and sleep characteristics among those with a spouse or a partner. Table 4 and Table 5 present the results. As Table 4 shows, neither positive relationship quality nor negative relationship quality was associated with self-reported sleep time. Yet, we observed some interesting patterns for self-report sleep quality. Married older adults who reported more negative aspects of their relationship showed higher scores on the troubled sleep scale. This is consistent with the stress model of the relationship between marriage and health, in which poor marital quality is a source of stress, which interferes with sleep. Psychosocial characteristics, particularly self-rated mental health, depression, and loneliness, explained this result. This result is consistent with the emotional support perspective on marriage and health. However, positive relationship quality showed no association with scores on the troubled sleep scale. Thus, among married older adults, negative features of the marital relationship were more consequential than positive aspect for self-reported sleep quality, and the association between negative relationship quality and the troubled sleep scale was attenuated when measures of psychosocial well-being were added to the model.
Table 4.
Effects of Relationship Quality on Self-Report Sleep Characteristics among Married and Partnered Older Adults (N=506)
| Total sleep time (minutes) |
Troubled sleep scale | |||
|---|---|---|---|---|
| Model 1 | Model 2 | Model 1 | Model 2 | |
| Negative marital relationship | 8.09 (6.95) | 7.77 (7.22) | 0.03 (0.09) | −0.08 (0.09) |
| Positive marital relationship | −2.24 (6.90) | 1.89 (7.04) | −0.16† (0.09) | 0.07 (0.09) |
| Female | 14.47† (8.51) | 16.95† (8.97) | −0.01 (0.14) | −0.02 (0.10) |
| Age | 2.03*** (0.54) | 1.88** (0.59) | −0.01 (0.01) | −0.02* (0.01) |
| Education | −8.81† (4.52) | −9.13† (5.05) | −0.01 (0.07) | 0.01 (0.06) |
| Race (Ref = White) | ||||
| African American | −11.42 (13.51) | 0.06 (13.47) | −0.07 (0.16) | −0.17 (0.19) |
| Hispanic | 2.37 (11.12) | 12.04 (11.54) | −0.26 (0.19) | −0.23 (0.21) |
| Other | −23.16 (15.18) | −10.44 (16.04) | 0.01 (0.23) | 0.04 (0.22) |
| Log household income | −3.44 (6.42) | −2.02 (6.11) | −0.15 (0.10) | −0.10 (0.08) |
| Log household assets | −1.27 (1.77) | −1.47 (1.68) | 0.03 (0.03) | 0.04 (0.03) |
| Retired | 17.22† (9.37) | 16.03† (9.19) | 0.10 (0.14) | 0.23† (0.13) |
| Physical Health | ||||
| Self-rated health | 1.34 (5.23) | −0.12* (0.05) | ||
| Charlson comorbidityiIndex | 4.10 (4.04) | 0.02 (0.04) | ||
| Frailty score | 8.22 (5.31) | 0.05 (0.07) | ||
| Psychosocial Wellbeing | ||||
| Self-rated mental health | −11.07† (5.95) | −0.06 (0.06) | ||
| Anxiety scale | 0.56 (1.67) | 0.04 (0.03) | ||
| CESD score | −0.86 (1.49) | 0.06** (0.02) | ||
| Loneliness scale | 0.43 (2.14) | 0.05* (0.02) | ||
| Household Environment | ||||
| Household disorder scale | −1.31 (1.05) | −0.01 (0.01) | ||
| Intercept | 433.77***(79.03) | 411.13*** (85.43) | 2.04 (1.48) | 0.01 (1.58) |
Note: Figures shown are coefficients with standard errors in parentheses. All regressions were survey-weighted and clustered by household.
p < .001,
p< .01,
p< .05,
p< .1 for two-tailed test.
Table 5.
Effects of Relationship Quality on Actigraphic Sleep Characteristics among Married and Partnered Older Adults (N=506)
| Total sleep time (minutes) |
Sleep fragmentation | WASO (minutes) |
||||
|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 1 | Model 2 | Model 1 | Model 2 | |
| Negative marital relationship | 0.75 (7.39) | 1.58 (8.04) | −0.26 (0.55) | −0.36 (0.57) | −1.18 (1.81) | −1.54 (1.82) |
| Positive marital relationship | 0.74 (6.52) | 1.65 (6.74) | −0.95† (0.49) | −0.73 (0.50) | −4.64* (1.90) | −3.76†(1.94) |
| Female | 13.64 (8.80) | 16.63† (9.05) | −1.39** (0.48) | −1.44** (0.49) | −2.77† (1.55) | −2.55 (1.64) |
| Age | 1.28 (0.79) | 1.00 (0.77) | 0.08+ (0.04) | 0.05 (0.04) | 0.10 (0.16) | 0.03 (0.17) |
| Education | 1.85 (5.00) | 1.11 (4.63) | −0.10 (0.33) | −0.02 (0.32) | 0.81 (1.19) | −0.78 (1.13) |
| Race (Ref = White) | ||||||
| African American | −7.38 (15.67) | 2.39 (13.26) | 1.19 (0.77) | 1.15 (0.87) | 4.31 (3.49) | 5.06 (3.67) |
| Hispanic | 3.69 (12.55) | 13.78 (13.30) | −0.94 (0.97) | −0.95 (1.08) | 0.40 (4.70) | 1.71 (4.91) |
| Other | −39.97 (24.69) | −31.18 (23.55) | −0.92 (1.65) | −0.84 (1.62) | −1.30 (6.13) | −0.86 (5.91) |
| Log household income | −4.35 (6.08) | −5.98 (6.68) | −0.52 (0.51) | −0.35 (0.51) | −2.02 (1.67) | −2.00 (1.67) |
| Log household assets | −0.33 (1.91) | −0.57 (1.85) | −0.31* (0.12) | −0.28* (0.13) | −1.05* (0.49) | −1.00* (0.50) |
| Retired | 14.27 (12.59) | 14.69 (11.84) | −0.73 (0.68) | −0.41 (0.71) | 0.31 (2.56) | 1.46 (2.59) |
| Physical Health | ||||||
| Self-rated health | 6.43 (4.90) | −0.24 (0.35) | 0.39 (1.11) | |||
| Charlson comorbidityiIndex | 6.32 (4.04) | 0.02 (0.28) | 0.57 (1.07) | |||
| Frailty score | 5.29 (7.71) | 0.66 (0.41) | 1.54 (1.26) | |||
| Psychosocial Wellbeing | ||||||
| Self-rated mental health | −8.34† (4.69) | −0.09 (0.35) | −1.29 (1.42) | |||
| Anxiety scale | 1.56 (1.73) | −0.08 (0.08) | −0.15 (0.33) | |||
| CESD score | −2.25 (1.35) | 0.12 (0.10) | 0.11 (0.35) | |||
| Loneliness scale | 0.34 (1.89) | −0.06 (0.17) | 0.27 (0.63) | |||
| Household Environment | ||||||
| Household disorder scale | −0.12 (1.30) | 0.02 (0.07) | 0.19 (0.29) | |||
| Intercept | 375.30*** (83.08) | 384.86*** (88.67) | 20.59** (6.05) | 17.15** (6.47) | 70.02** (25.35) | 58.45* (25.97) |
Note: Figures shown are coefficients with standard errors in parentheses. All regressions were survey-weighted and clustered.
p < .001,
p< .01,
p< .05,
p< .1 for two-tailed test.
Turning to actigraph-estimated sleep characteristics (Table 5), we observe different patterns. First, although we hypothesized a negative effect of poor marital relationship on sleep outcomes, our estimates showed no statistically significant associations between the negative relationship quality scale and actigraph-estimated sleep characteristics. A poor marital relationship did not appear to compromise sleep time or sleep quality. Second, as expected, positive relationship quality was associated with more favorable sleep outcomes. Specifically, those who reported higher levels of spousal support also showed less sleep fragmentation and lower levels of wake time after sleep onset. Third, the significant association between relationship support and wake time after sleep onset was partially explained by the mediators. Spousal support remained negatively associated with wake time after sleep onset after physical health, psychosocial characteristics, and the household environment were taken into account. However, the association between positive relationship and sleep fragmentation was substantially reduced with the inclusion of proximate factors, particularly home environment. This is consistent with the model of marriage and health in which financial resources and the spousal relationship facilitate household order. Taken together, these findings suggest that negative aspects of the relationship are more consequential for subjective sleep quality than are positive features among partnered older adults. For sleep quality measured by actigraph, we observed the opposite: positive relationship quality is more influential than negative relationship quality. Thus relationship quality seems to influence perceptions of sleep problems and actigraph-measured sleep quality in quite different ways.
Additional Analysis
We included positive and negative aspects of marital relationships in the same models. We replicated all models with positive relationship quality but not negative aspects, and with negative relationship quality but not positive aspects, because of the correlation between them. Coefficients of these measures were relatively unchanged, suggesting that both dimensions of marital quality have independent effects on older adults’ sleep. Finally, a few prior epidemiologic studies suggest that long sleep duration or short duration comprise risk factors for poor health and mortality4. As such, the relationship between partnership status and relationship quality and total sleep time may be U-shaped rather than linear. To address this issue, we first transformed self-reported and actigraph-estimated total sleep time into ordinal variables with three categories: short sleep duration, intermediate sleep duration, and long sleep duration. We then used multinomial logistic regression to examine the association of marital status and relationship quality with the odds of short sleep duration and long sleep duration and found no association for either marital status or the relationship quality measures for either self-reported or actigraph-estimated measured sleep duration.
DISCUSSION AND CONCLUSION
This study provides an examination of the links between marital status, relationship quality and measures of multiple dimensions of sleep, both subjective experience of sleep as well as direct assessment of sleep characteristics using actigraphy, in a nationally-representative population of older adults. While sleep is a universal health behavior, the effect of the social world on the quantity and quality of sleep is too often overlooked. The innovative design of NSHAP allows for an in-depth investigation of the association between marital relationships and multiple dimensions of sleep characteristics at older ages. The present study adds actigraph-measured characteristics of sleep in a nationally-representative population of older adults to the prior literature that has focused mostly on survey reports about sleep among younger adults.
Motivated by theories and prior studies of marriage and health, we explored several research questions. First, we asked whether marriage is associated with sleep outcomes among older adults. Second, we asked whether positive aspects of the marital relationship were associated with more optimal sleep outcomes and whether negative aspects of the marital relationship undermine sleep. Finally, we also examined whether the associations of marriage and relationship quality with sleep were reduced by the addition of important proximate factors, including physical health, functional status, psychosocial well-being, and the household environment.
We found that older adults with spouses or partners had, on average, longer sleep duration and better sleep quality than those without. The associations might be explained by the theoretical models we discussed earlier, in particular, the resource model; but the associations were only observed for actigraph-measured sleep characteristics. More specifically, the married showed longer total sleep time, less sleep fragmentation, and less wake time after sleep onset than the unmarried, but did not differ in the self-assessments of their sleep. Further, the proposed proximate factors explained only a small proportion of the association between marriage and better actigraph-measured sleep outcomes. Hence, while we found positive associations between marriage and sleep, we found no strong evidence that this association worked through the proximate factors we considered.
We also found among married older adults, reports of troubled sleep were more prevalent among those with higher negative relationship quality, but were not less prevalent among those in more positive and supportive relationships. Yet, for actigraph-measured sleep outcomes, it was different. Higher scores on the scale of positive relationship quality were associated with better sleep quality as indicated by less wake time after sleep onset whereas the negative relationship scale showed little impact on any sleep characteristics measured by actigraphy. Further, we found proximate factors explained the relationship between negative relationship quality and self-report sleep quality, and partially explained the relationship between positive relationship quality and actigraphic sleep characteristics. These appeared to partially support the proposed pathways of influence by both models: resources, emotional connection and stress. Finally, comparing Table 2 with Table 4 and Table 3 with Table 5, it appeared that the benefits of marriage for sleep primarily came from positive aspects of the marital relationship. The effects were manifested in actigraph-measured outcomes instead of subjective sleep experience. However, since the second set of analyses involves married older adults only, direct comparison across tables must be done with care.
What might explain why we found marriage benefits for measured sleep but individuals did not report them? One reason could be that marriage at old ages benefited sleep consolidation which respondents were less likely to report. Prior studies suggest that the survey questions and the actigraph measures are not equivalent to each other, even when they seem to measure the same thing. Specifically, the question about waking up during the night would seem to be similar to the number of minutes awake after sleep onset as measured by actigraphy, and they are correlated (Chen et al., 2015). However, there is a key difference in that the actigraph measure sums up all episodes of being awake during the night, which could include many shorter awake bouts of which the individual is unaware in the morning, whereas the survey response may correspond to long awake intervals only. If at older ages marriage has a greater influence on the type of sleep, whether it is deep sleep or light sleep, than on sleep behaviors, then one might see this pattern. Evidence from neuropsychology suggests that even among the healthy elderly, sleep architecture, the episodic pattern of deep sleep, light sleep and REM sleep throughout the night, becomes more and more fragile as people age (Pace-Schott and Spencer 2011; Espiritu 2008; Vitiello 2006). As people age, time in deep sleep (i.e., slow wave sleep) shortens and the distribution of this sleep stage across the sleep interval is more concentrated in early sleep than throughout the night, as is more the case for young adults (Lombardo et al. 1998). Short awake bouts are unlikely to occur during deep sleep. If the benefits of marriage for older adults’ sleep are primarily to strengthen amount of time in deeper sleep, then actigraph measures of sleep consolidation (fragmentation and wake after sleep onset) would show an effect when the survey questions about sleep quality do not. Thus, even though married older adults do not perceived that they sleep better, their sleep outcomes may be better specifically in ways captured by actigraphy.
A second possible reason is that being married or, more specifically, co-sleeping might directly influence how people experience and report their sleep. Note that virtually all those with partners usually sleep with that person, making it impossible to separate the two. The presence of a spouse may influence older adults’ perception of their own sleep in a number of ways. Married older adults may be more likely to remember sleep disturbances than those without a partner because, while they are awake, they notice their spouse’s breathing, snoring or getting up, to which they may, correctly or incorrectly, ascribe their own wakefulness. This could also be related to why negative relationships are related to perceptions of sleep problems, but not to worse measured sleep quality. They also may judge their own sleep experience compared to their spouse’s sleep. In contrast, single older adults rely solely on their own experience and memory in answering these questions. As such, married older adults may be more sensitive and have a lower bar for sleep problems as compared to single older adults, resulting in smaller differences between married and single’s self-reports of sleep outcomes than if everyone were using the same standards in answering the questions. To the extent that this is the case, our estimates of the effects of marriage on self-report outcomes are attenuated, and prior sociological studies of sleep using self-report measures may underestimate the impact of various social relationships and factors on human sleep. While this hypothesis deserves further exploration, we were unable to examine it as this moment. Nearly 90% of married older adults co-slept with their spouses in the NSHAP sample. The high degree of collinearity makes us not able to further explore the role of co-sleeping on sleep at the same time. Further data collection with larger samples and better information of sleep habits may allow for a detailed investigation of this hypothesis.
Our findings that positive aspects of the marital relationship are more consequential for older adults’ actigraphic sleep characteristics are consistent with, and also add to, the emerging literature on the link between marital quality and changes in health at older ages (Liu and Waite, 2014; Umberson et al., 2006). One key feature of the last third of life is loss of function, particularly declines in physical health, sensory function, mobility and social connections. Successful aging entails coping well with these losses. Those in high-quality marriages seem to adjust to loss of functional health better than those in poor-quality marriages (Warner and Kelley-Moore, 2012), be less likely to show poor quality of life in the face of loss of vision (Bookwala 2011), and, as our results show, to sleep better at older ages, when sleep often becomes problematic. Together these findings point to the particular importance of high-quality marriage in the later period of life.
Seen through this lens, our results are not unexpected. Instead, these findings have broad implications for the sleep literature in particular and for medical sociology more generally. The emerging field of sociology of sleep has documented strong associations between precarious employment, women’s caregiving responsibilities and poor sleep outcomes using qualitative or quantitative approaches (Burgard 2011; Burgard and Ailshire 2009, 2013; Venn et al. 2008). Here, we advance the literature by providing a life course and sociobiological approach by taking the aging process and physiologic aspects of sleep into consideration. Our findings suggest that the study of human sleep needs to consider the nature of change in dimensions of sleep that individuals cannot report, but which may be consequential for health. Marriage may have the potential to strengthen the structure of sleep at older ages as manifested in its associations with actigraphic measures of sleep consolidation. With this in mind, it is not difficult to place our findings in relation to prior sociological studies of sleep which found a protective effect of marriage on self-report sleep outcomes among adults (Aber, Bote, and Meadows 2009; Hale 2005; Knudsen, Ducharme, Roman 2007). The relationship between marriage and sleep may not be static over the life course. Strong associations among young adults may not indicate the same associations at older ages. As such, this study not only fills the gap in the sociology of sleep literature but also points to the need for a more sophisticated theoretical model that includes the changing nature of social processes and sleep over the life course.
More importantly, results from this study points to the need for a reconsideration of the relationship between social processes and health in research design and theory in medical sociology. Earlier works in medical sociology predominantly focus on self-report health outcomes. During the past few years, researchers are, to an increasing extent, combining disparate types of data to address complex questions. For example, full neuropsychological testing has been done on subsamples of the Health and Retirement Survey in the ADAMS study (Crimmins et al 2011), and biomeasures administered to NSHAP respondents have been used to address the effects of marital loss on inflammation (Sbarra, 2009) and the role of social networks in the development and treatment of hypertension (Cornwell & Waite, 2012). The growing number of surveys with innovative biomedical data shift medical sociologists’ focus to more objective health measures with the goal to further understand how social processes affect human physiology. However, for sociologists, it is too simplistic to argue that these external measures are of greater theoretical importance than self-report measures. On the one hand, for social processes to influence health, they must affect physiologic processes, either directly or indirectly. On the other hand, biology is not destiny. A comprehensive definition of health encompasses psychological and social wellbeing and not merely the absence of morbidity (e.g., World Health Organization 2012). As such, neither the focus on self-report outcomes nor the emphasis on objective measures is adequate to understand the role of social processes in human health. The increasing availability of both subjective and objective measures of health in datasets offers great potential for in-depth examination of the complex web of social mechanisms that chart the movements of health over the life course. Our study serves as an example by revealing the differential roles of marriage in affecting older adults’ subjective sleep experience and sleep architecture.
Despite the strength and novelty of these findings, we acknowledge several limitations of the study. First, the results should be interpreted as associational rather than causal. While the study controlled for a wide range of confounders, we cannot establish a causal relationship with cross-sectional data. Sleep quality may affect as well as being affected by relationship quality. To the extent that poor sleepers are also more difficult to live with because they are often tired and cranky, poor sleep quality may lead to an increase in relationship demands or conflicts or a decline in emotional support.
Second, because older adults living in institutions were not included in the survey, results from the present study cannot be generalized to that population (O’Muirchaitaigh et al., 2014). This also means that respondents in NSHAP are relatively healthy as compared to those in clinical studies of older adults. Thus, we might have fewer respondents with severe sleep problems, which could mean weaker associations between explanatory variables and sleep outcomes. However, this would give us conservative estimates. And these data offered the opportunity to examine sleep outcomes in a representative sample of community-dwelling older adults. Also, the study relied on cross-sectional data. The lack of sleep measures in Wave 1 data precluded our taking full advantage of the longitudinal feature of NSHAP. Future studies may update our analysis with the availability of longitudinal data on older adults’ sleep.
Third, some of the coefficients between control variables and sleep variables appeared to be in unexpected directions as compared to coefficients reported in previous studies. For example, we found that women got less disrupted sleep which was opposite of some previous studies found (e.g., Burgard 2011; Burgard & Ailshire 2013). However, we wanted to point out that that many of the seemingly unexpected coefficients were found in our analysis of actigraphic sleep characteristics. Since all previous sociological studies were used self-report sleep outcomes, we did not consider they were contradictory findings. In contrast, we believed these results pointed to the fact that future research of sleep needs to attend to multidimensional nature of human sleep and the possibility that social processes may act on different aspect of sleep differently.
Finally, as previously discussed, health can act as either a mediator or a confounder of the relationship between marriage and sleep. With only one wave of data, we were unable to empirically distinguish between these alternatives. However, our results suggested that the associations between marriage and sleep generally changed very little with the inclusion of measures of health. Thus, health seems to act neither as a mediator nor as a confounder. Instead, results suggest that it is the home environment and emotional and social support that play a role.
In sum, in this study, we brought together theoretical and empirical research on marriage and health with innovative measures of sleep outcomes to highlight the importance of partnership status and relationship quality for older adults’ sleep. We found that relational status was strongly associated with older adults’ actigraphic sleep patterns in spite of the fact that we see no significant differences in their self-reported sleep outcomes. Among the partnered, relationship quality mattered but affected perceptions of sleep and actigraph-measured sleep characteristics differently. Thus, this study makes important contributions to research on marriage and health at old ages by extending the ideas to sleep outcomes. Since none of the proposed mechanisms fully mediated the relationship between partnership status and sleep, we leave unanswered the questions posed about the processes through which partnership promotes better sleep. Furthermore, the findings suggest that older adults’ sleep is amenable to social interventions. Interventions that aim to promote marital quality may have additional benefits on sleep among the elderly. As sleep is a complicated behavior with health implications, future studies and data collection are warranted to fully understand the social nature of human sleep at older ages.
Footnotes
We acknowledge that the relationship between physical and emotional health and sleep is quite likely bi-directional, with chronic sleep problems increasing chances of anxiety, irritability, depressive symptoms and leading to or exacerbating chronic conditions or other health problems (Dinges et al. 1997; Neckelman, Mykletun, and Dahl 2007). Those who are not well rested may also have more trouble than others in keeping their home neat and clean. Nevertheless, from the theoretical perspective, we consider it is critical to explicitly lay out the pathways through which marriage may affect sleep and point out the potential causal directions in our conceptual model. When interpreting our results, we stressed the coefficients as associational instead of causal.
There has been relatively little methodological work about how to ask about sleep duration in a survey. Single survey questions about sleep duration do not generally have a high correlation with measured sleep duration, and instruments developed by sleep researchers often ask respondents to think about bedtimes and wake times to yield more accurate data; asking about weekdays and weekends separately may also yield more accurate data (Girschik et al. 2012; Lauderdale 2013; Wolfson et al. 2003).
Prior studies have suggested that because women exhibit greater physiological arousal in response to relational conflicts than men, their health is more vulnerable to poor marital quality (Robles and Kiecolt-Glaser 2003; Umberson and Williams 2005). This motivated us to perform an additional test for gender variations in the association between marital status, relationship quality, and sleep characteristics. There was only one significant interaction term. Results (not shown) indicate that marital status was associated with longer actigraph-estimated sleep duration in men but not in women. Specifically, marital status was associated with an increase of approximately 45 minutes in men’s actigraph-estimated total sleep time but had no impact on women’s. None of the other interaction terms, however, were statistically significant, suggesting with the one exception noted marital status and relationship quality had similar effects on men and women’s sleep quality. A full treatment of the relationship between marriage, gender, and sleep at old ages is beyond the scope of this paper. We simply reported results from our post hoc analysis and we left detailed exploration of the issue for future studies.
The U shape relationship between sleep duration and health outcomes appears to imply an optimal sleep duration in the intermedia. However, a recent review article suggests that the curvilinear relationship is not universal and may depend on how sleep is measured (Kurina et al. 2013). As such, the sensitivity analysis was explorative purpose. We did not take a priori that there is an optimal amount of sleep duration of older adults.
Contributor Information
Jen-Hao Chen, Department of Health Sciences, University of Missouri
Linda J. Waite, Department of Sociology, University of Chicago
Diane S. Lauderdale, Department of Public Health Sciences, University of Chicago
REFERENCES
- Ailshire Jennifer A, Burgard Sarah A. Family Relationships and Troubled Sleep among U.S. Adults: Examining the Influence of Contact Frequency and Relationship Quality. Journal of Health and Social Behavior. 2012;53(2):248–262. doi: 10.1177/0022146512446642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allison Paul. Missing Data. Thousand Oaks, CA: Sage Publications; 2001. [Google Scholar]
- Ancoli-Israel Sonia. Sleep and Its Disorders in Aging Populations. Sleep Medicine. 2009;10(1):S7–S11. doi: 10.1016/j.sleep.2009.07.004. [DOI] [PubMed] [Google Scholar]
- Ancoli-Israel Sonia, Cole Roger, Alessi Cathy, Chambers Mark, Willia Moorcroft, Oillak Charles P. The Role of Actigraphy in the Study of Sleep and Circadian Rhythms. Sleep. 2003;26(3):342–392. doi: 10.1093/sleep/26.3.342. [DOI] [PubMed] [Google Scholar]
- Arber Sara, Bote Marcos, Meadows Robert. Gender and Socioeconomic Patterning of Self-Reported Sleep Problems in Britain. Social Science & Medicine. 2009;68(2):281–289. doi: 10.1016/j.socscimed.2008.10.016. [DOI] [PubMed] [Google Scholar]
- Blackwell Terri, Redline Susan, Ancoli-Israel Sonia, Schneider Jennifer L, Surovec Susan, Johnson Nathan L, Cauley Jane A, Stone Katie L and Study of Osteoporotic Fractures Research Group. Comparison of Sleep Parameters from Actigraphy and Polysomnography in Older Women: the SOF Study. Sleep. 2008;31:283. doi: 10.1093/sleep/31.2.283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bookwala Jamila. Marital Quality as a Moderator of the Effects of Poor Vision on Quality of Life among Older Adults. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2011;66(5):605–616. doi: 10.1093/geronb/gbr091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bookwala Jamila, Franks Melissa M. Moderating Role of Marital Quality in Older Adults’ Depressed Affect: Beyond the Main-Effect Model. Journal of Gerontology Series B Psychological and Social Sciences. 2005;60(6):P338–P441. doi: 10.1093/geronb/60.6.p338. [DOI] [PubMed] [Google Scholar]
- Brassington GS, King AC, Bliwise DL. Sleep Problems as a Risk Factor for Falls in a Sample of Community-Dwelling Adults Aged 64–99 Years. Journal of the American Geriatrics Society. 2000;48(1):1234–1240. doi: 10.1111/j.1532-5415.2000.tb02596.x. [DOI] [PubMed] [Google Scholar]
- Brown Susan L. The Effect of Union Type on Psychological Well-Being: Depression among Cohabitors Versus Married. Journal of Health and Social behavior. 2000 Sep;41:241–255. [PubMed] [Google Scholar]
- Burgard Sarah A. The Needs of Others: Gender and Sleep Interruptions for Caregiving. Social Forces. 2011;89:1189–1215. [Google Scholar]
- Burgard Sarah A, Ailshire Jennifer A. Putting Work to Bed: Stressful Experiences on the Job and Sleep Quality. Journal of Health and Social Behavior. 2009;50:476–492. doi: 10.1177/002214650905000407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burgard Sarah A, Ailshire Jennifer A. Gender and Time for Sleep among US Adults. American Sociological Review. 2013;78:51–69. doi: 10.1177/0003122412472048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cacioppo John T, Hawkley Louise C, Berntson Gary C, Ernst John M, Gibbs Amber C, Stickgold Robert, Hobson JAllan. Do Lonely Days Invade the Nights? Potential Social Modulation of Sleep Efficiency. Psychological Science. 2002;13(4):384–387. doi: 10.1111/1467-9280.00469. [DOI] [PubMed] [Google Scholar]
- Cappuccio Francesco P, D’Elia Lanfranco, Strazzullo Pasquale, Miller Michelle A. Quantity and Quality of Sleep and Incidence of Type 2 Diabetes: A Systematic Review and Meta-Analysis. Diabetes Care. 2009;33:414–420. doi: 10.2337/dc09-1124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cascardi Michele, Langhinrichsen Jennifer, Vivian Dian. Marital Aggression: Impact, Injury, and Health Correlates for Husbands and Wives. JAMA Internal Medicine. 1992;152(6):1178–1184. doi: 10.1001/archinte.152.6.1178. [DOI] [PubMed] [Google Scholar]
- Charlson Mary E, Pompei Peter, Ales Kathy L, MacKenzie CRonald. A New Method of Classifying Prognostic Comorbidity in Longitudinal Studies: Development and Validation. Journal of Chronic Diseases. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- Chen Jen-Hao, Waite Linda, Kurina Lianne M, Thisted Ronald A, McClintock Martha, Lauderdale Diane S. Insomnia Symptoms and Actigraph-estimated Sleep Characteristics in a Nationally Representative Sample of Older Adults. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences. 2015;70(2):185–192. doi: 10.1093/gerona/glu144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke Philippa, Wheaton Blair. Addressing Data Sparseness in Contextual Population Research Using Cluster Analysis to Create Synthetic Neighborhoods. Sociological Methods & Research. 2007;35(3):311–351. [Google Scholar]
- Clarke P. When Can Group Level Clustering Be Ignored? Multilevel Models versus Single-Level Models with Sparse Data. Journal of Epidemiology and Community Health. 2008;62(8):752–758. doi: 10.1136/jech.2007.060798. [DOI] [PubMed] [Google Scholar]
- Cornwell Benjamin, Laumann Edward O, Schumm LPhilip. The Social Connectedness of Older Adults: A National Profile. American Sociological Review. 2008;73(2):185–203. doi: 10.1177/000312240807300201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coyne James C, Delongis Anita. Going Beyond Social Support: The Role of Social Relationships in Adaptation. Journal of Consulting and Clinical Psychology. 1986;54(4):454–460. doi: 10.1037//0022-006x.54.4.454. [DOI] [PubMed] [Google Scholar]
- Choi Heejeong, Marks Nadine F. Marital Conflict, Depressive Symptoms, and Functional Impairment. Journal of Marriage and Family. 2008;70(2):377–390. doi: 10.1111/j.1741-3737.2008.00488.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornwell York. Social Resources and Disordered Living Conditions: Evidence from a National Sample of Community-Residing Older Adults. Research on Aging. 2014 doi: 10.1177/0164027513497369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornwell Erin York, Waite Linda. Social Network Resources and Management of Hypertension. Journal of Health and Social Behavior. 2012;53(2):215–231. doi: 10.1177/0022146512446832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crimmins Eileen M, Kim Jung Ki, Langa Kenneth M, Weir David R. Assessment of Cognition Using Surveys and Neuropsychological Assessment: The Health and Retirement Study and the Aging, Demographics, and Memory Study. Journal of Gerontology Series B: Psychological Sciences & Social Sciences. 2011;66B:i162–i171. doi: 10.1093/geronb/gbr048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curran Srar R, McLanahan Sara, Knab Jean. Does Remarriage Expand Perceptions of Kinship Support among the Elderly? Social Science Research. 2003;32(2):171–190. doi: 10.1016/S0049-089X(02)00046-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dinges David F, Pack Frances, Williams Katherine, Gillen Kelly A, Powell John W, Ott Geoffrey E, Aptowicz Caitlin, Pack Allan I. Cumulative sleepiness, mood disturbance and psychomotor vigilance performance decrements during aweek of sleep restricted to 4–5 hours per night. Sleep. 1997;20(4):267–277. [PubMed] [Google Scholar]
- Donoho Carrie J, Crimmins Eileen M, Seeman Teresa E. Marital Quality, Gender, and Markers of Inflammation in the MIDUS Cohort. Journal of Marriage and the Family. 2013;75(1):127–141. doi: 10.1111/j.1741-3737.2012.01023.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duncan JGreg, Wilkerson Bessie, England Paula. Cleaning Up Their Act: The Effects of Marriage and Cohabitation on Licit and Illicit Drug Use. Demography. 2006;43(4):691–710. doi: 10.1353/dem.2006.0032. [DOI] [PubMed] [Google Scholar]
- Espiritu, Joseph Roland D. Aging-Related Sleep Changes. Clinics in Geriatric Medicine. 2008;24(1):1–14. doi: 10.1016/j.cger.2007.08.007. [DOI] [PubMed] [Google Scholar]
- Faubel R, Lopez-Garcia E, Guallar-Castillon P, Graciani A, Banegas JR, Rodriguez-Artalejo F. Usual Sleep Duration and Cognitive Function in Older Adults in Spain. Journal of Sleep Research. 2009;18:427–435. doi: 10.1111/j.1365-2869.2009.00759.x. [DOI] [PubMed] [Google Scholar]
- Fleming Charles B, White Helene R, Catalano Richard F. Romantic Relationships and Substance Use in Early Adulthood: An Examination of the Influence of Relationship Type, Partner Substance Use, and Relationship Quality. Journal of Health and Social Behavior. 2010;51(2):153–167. doi: 10.1177/0022146510368930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foley DJ, Ancoli-Israel S, Britz P, Walsh J. Sleep Disturbances and Chronic Disease in Older Adults: Results of the 2003 National Sleep Foundation Sleep in America Survey. Journal of Psychosomatic Research. 2004;56(5):497–502. doi: 10.1016/j.jpsychores.2004.02.010. [DOI] [PubMed] [Google Scholar]
- Foley DJ, Monjan AA, Brown SL, Simonsick EM. Sleep Complaints among Elderly Persons: An Epidemiologic Study of Three Communities. Sleep. 1995;18(6):425–432. doi: 10.1093/sleep/18.6.425. [DOI] [PubMed] [Google Scholar]
- Galinsky Adena M, Waite Linda J. Sexual Activity and Psychological Health As Mediators of the Relationship Between Physical Health and Marital Quality. Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2014 doi: 10.1093/geronb/gbt165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Girschik Jennifer, Fritschi Lin, Heyworth Jane, Waters Flavie. Validation of Self-Reported Sleep Against Actigraphy. Journal of Epidemiology. 2012;22(5):462–468. doi: 10.2188/jea.JE20120012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grandner Michael A, Patel Nirav P, Gehrman Philip R, Xie Dawei, Sha Daohang, Weaver Terri, Gooneratne Nalaka. Who Gets the Best Sleep? Ethnic and Socioeconomic Factors Related to Sleep Complaints. Sleep Medicine. 2010;11:470–478. doi: 10.1016/j.sleep.2009.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gove Water R, Hughes Michael and Carolyn Briggs Style. Does Marriage Have Positive Effects on the Psychological Well-Being of the Individual? Journal of Health and Social Behavior. 1983 Jun;24:122–131. [PubMed] [Google Scholar]
- Hale Lauren. Who Has Time to Sleep? Journal of Public Health. 2005;27:205–211. doi: 10.1093/pubmed/fdi004. [DOI] [PubMed] [Google Scholar]
- Harvey AG. Insomnia: Symptom or Diagnosis? Clinical Psychology Review. 2001;21(7):1037–1059. doi: 10.1016/s0272-7358(00)00083-0. [DOI] [PubMed] [Google Scholar]
- Hawkley Louise C, Kocherginsky M, Wong J, Kim J, Cagney KA. Missing Data in Wave 2 of NSHAP: Prevalence, Predictors, and Recommended Treatment. Journal of Gerontology Series B: Psychological and Social Sciences. 2014 doi: 10.1093/geronb/gbu044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hawkley Louise C, Hughes Linda J, Waite CM, Masi Ronald A, Thisted, Cacioppo John T. From Social Structural Factors to Perceptions of Relationship Quality and Loneliness: The Chicago Health, Aging, and Social Relations Study. Journal of Gerontology Series B: Psychological and Social Sciences. 2008;63B(6):S375–S384. doi: 10.1093/geronb/63.6.s375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill Terrence D, Burdette Amy M, Hale Lauren. Neighborhood Disorder, Sleep Quality, and Psychological Distress: Testing a Model of Structural Amplification. Health and Place. 2009;15(4):1006–1013. doi: 10.1016/j.healthplace.2009.04.001. [DOI] [PubMed] [Google Scholar]
- Holt-Lunstad Julianne, Birmingham Wendy, Jones Brandon Q. Is There Something Unique about Marriage? The Relative Impact of Marital Status, Relationship Quality, and Network Social Support on Ambulatory Blood Pressure and Mental Health. Annals of Behavioral Medicine. 2008;35(2):239–244. doi: 10.1007/s12160-008-9018-y. [DOI] [PubMed] [Google Scholar]
- Hughes Mary Elizabeth, Waite Linda J. Health in Household Context: Living Arrangements and Health in Late Middle Age. Journal of Health and Social Behavior. 2002;43(1):1–21. [PMC free article] [PubMed] [Google Scholar]
- Hughes Mary Elizabeth, Waite Linda J. Marital Biography and Health at Mid-Life. Journal of health and Social Behavior. 2009;50(3):344–358. doi: 10.1177/002214650905000307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes Mary Elizabeth, Waite Linda J, Hawkley Louise C, Cacioppo John T. A Short Scale for Measuring Loneliness in Large Surveys. Research on Aging. 2004;26(6):655–672. doi: 10.1177/0164027504268574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huisingh-Scheetz M, Kocherginsky M, Schumm P, Engelman M, McClintock M, Dale W, Magett E, Rush P, Waite L. Measuring Functional Status in the National Social Life, Health, and Aging Project: Rationale, Measurement, and Preliminary Findings. Journal of Gerontology Series B: Psychological and Social Sciences. 2014 doi: 10.1093/geronb/gbu091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irwin Michael, Artim Kamal Haydari, Oxman Michael N. Screening for Depression in the Older Adult: Criterion Validity of the 10-item Center for Epidemiological Studies Depression Scale (CES-D) Archives of Internal Medicine. 1999;159(15):1701–1704. doi: 10.1001/archinte.159.15.1701. [DOI] [PubMed] [Google Scholar]
- Katz Jeffrey N, Chang Lily C, Sangha Oliver, Fossel Anne H, Bates David W. Can comorbidity be measured by questionnaire rather than medical record review? Medical Care. 1996;34(1):73–84. doi: 10.1097/00005650-199601000-00006. [DOI] [PubMed] [Google Scholar]
- Kawachi Ichiro, Berkman Lisa F. Social ties and mental health. Journal of Urban health. 2001;78(3):458–467. doi: 10.1093/jurban/78.3.458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim Hyoun K, McKenry Patrick C. The Relationship Between Marriage and Psychological Well-Being. Journal of Family Issues. 2002;23(8):885–911. [Google Scholar]
- Kim Juyeon, Waite Linda J. Relationship Quality and Shared Activity in Marital and Cohabiting Dyads in the National Social Life, Health and Aging Project, Wave 2. Journals of Gerontology Series B: Psychological and Social Sciences. 2014 doi: 10.1093/geronb/gbu038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knudsen Hannah K, Ducharme Lori J, Roman Paul M. Job Stress and Poor Sleep Quality: Data from an American Sample of Full-Time Workers. Social Science & Medicine. 2007;64(10):1997–2007. doi: 10.1016/j.socscimed.2007.02.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knutson Kristen L, Ryden Armand M, Mander Bryce A, Cauter Eve Van. Role of Sleep Duration and Quality in the Risk and Severity of Type 2 Diabetes Mellitus. JAMA Internal Medicine. 2006;166(16):1768–1774. doi: 10.1001/archinte.166.16.1768. [DOI] [PubMed] [Google Scholar]
- Kurina Lianne M, Knutson Kristen, Hawkley Louise C, Cacioppo John T, Lauderdale Diane S, Ober Carole. Loneliness Is Associated with Sleep Fragmentation in a Communal Society. Sleep. 2011;34(11):1519–1526. doi: 10.5665/sleep.1390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lauderdale Daine S. Survey Questions About Sleep Duration: Does Asking Separately About Weekdays and Weekends Matter? Behavioral Sleep Medicine. 2013;12(2):158–168. doi: 10.1080/15402002.2013.778201. [DOI] [PubMed] [Google Scholar]
- Lauderdale Diane S, Schumm LPhilip, Kurina Lianne M, McClintock Martha, Thisted Ronald A, Chen Jen-Hao, Waite Linda. Assessment of Sleep in the National Social Life, Health, and Aging Project. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2014;69:S125–S133. doi: 10.1093/geronb/gbu092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leonard Kenneth E, Rothbard Julie C. Alcohol and the Marriage Effect. Journal of Studies on Alcohol and Drugs. 1999;13:139–146. doi: 10.15288/jsas.1999.s13.139. [DOI] [PubMed] [Google Scholar]
- Levenson Robert W, Gottman John M. Physiological and Affective Predictors of Change in Relationship Satisfaction. Journal of Personality and Social Psychology. 1985;49(1):85–94. doi: 10.1037//0022-3514.49.1.85. [DOI] [PubMed] [Google Scholar]
- Liu Hui, Waite Linda. Bad Marriage, Broken Heart? Age and Gender Differences in the Link between Marital Quality and Cardiovascular Risks among Older Adults. Journal of Health and Social Behavior. 2014;55(4):403–423. doi: 10.1177/0022146514556893. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lombardo P, Formicola G, Gori S, Gneri C, Massetani R, Murri L, Fagioli I, Salzarulo P. Slow Wave Sleep (SWS) Distribution across Night Sleep Episode in the Elderly. Aging Clinical and Experimental Research. 1998;10:445–448. doi: 10.1007/BF03340157. [DOI] [PubMed] [Google Scholar]
- Lopresti Adrian L, Hood Sean D, Drummond Peter D. A Review of Lifestyle Factors that Contribute to Important Pathways Associated with Major Depression: Diet, Sleep and Exercise. Journal of Affective Disorders. 2013;148(1):12–27. doi: 10.1016/j.jad.2013.01.014. [DOI] [PubMed] [Google Scholar]
- Lund Rikke, Due Pernille, Modvig Jens, Holstein Bjorn Evald, Damsgaard Mogens Trab, Andersen Per Kragh. Cohabitation and Marital Status as Predictors of Morality— An Eight Year Follow-Up Study. Social Science & Medicine. 2002;55(4):673–679. doi: 10.1016/s0277-9536(01)00219-2. [DOI] [PubMed] [Google Scholar]
- Mallon L, Broman JE, Hetta J. Sleep Complaints Predict Coronary Artery Disease Mortality in Males: A 12-Year Follow-Up Study of a Middle-Aged Swedish Population. Journal of Internal Medicine. 2002;251:207–216. doi: 10.1046/j.1365-2796.2002.00941.x. [DOI] [PubMed] [Google Scholar]
- McPherson J Miller, Smith-Lovin Lynn, Brashears Matthew E. Social Isolation in America: Changes in Core Discussion Networks over Two Decades. American Sociological Review. 2006;71:353–375. [Google Scholar]
- Michael L Yvonne, Berkman Lisa F, Colditz Graham A, Kawachi Ichiro. Living Arrangements, Social Integration, and Change in Functional Health Status. American Journal of Epidemiology. 2001;153(2):123–131. doi: 10.1093/aje/153.2.123. [DOI] [PubMed] [Google Scholar]
- Neckelmann Dag, Mykletun Amstein, Dahl Alv A. Chronic insomnia as a risk factor for developing anxiety and depression. Sleep. 2007;30(7):873–880. doi: 10.1093/sleep/30.7.873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neikrug Ariel B, Ancoli-Israel Sonia. Sleep Disorders in the Older Adult—A Mini-Review. Gerontology. 2010;56:181–189. doi: 10.1159/000236900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Muricheartaigh Colm, English Ned, Pedlow Steven, Kwok Peter K. Sample Design, Sample Augmentation, and Estimation ofr Wave 2 of the NSHAP. The Journal of Gerontology Series B: Psychological Sciences and Social Sciences. 2014;69(Suppl 2):S15–S26. doi: 10.1093/geronb/gbu053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Payne Carolyn, Hedberg EC, Kozloski Michael, Dale William, McClintock Martha K. Using and Interpreting Mental Health Measures in the National Social Life, Health, and Aging Project. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2014;69:S99–S116. doi: 10.1093/geronb/gbu100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pace-Schott Edward F, Spencer Rebecca MC. Age-Related Changes in the Cognitive Function of Sleep. Progress in Brain Research. 2011;191:75–89. doi: 10.1016/B978-0-444-53752-2.00012-6. [DOI] [PubMed] [Google Scholar]
- Pearlin Leonard I, Johnson Joyce S. Marital Status, Life-Strains and Depression. American Sociological Review. 1977;42(5):704–715. [PubMed] [Google Scholar]
- Phillips Barbara, Mannino David M. Do Insomnia Complaints Cause Hypertension or Cardiovascular Disease? Journal of Clinical Sleep Medicine” JCSM: Official Publication of the American Academy of Sleep Medicine. 2007;3:489–493. [PMC free article] [PubMed] [Google Scholar]
- Phillips/Respironics. Andover, MA: Actiwatch Spectrum; 2010. [Google Scholar]
- Population Reference Bureau. America’s Aging Population. Population Bulletin. 2011;66(1) [Google Scholar]
- Robles Theodore F, Kiecolt-Glaser Janice K. The Physiology of Marriage: Pathways to Health. Physiology & Behavior. 2003;79(3):409–416. doi: 10.1016/s0031-9384(03)00160-4. [DOI] [PubMed] [Google Scholar]
- Roehrs Timothy, Roth Thomas. Sleep, Sleepiness, Sleep Disorders and Alcohol Use and Abuse. Sleep Medicine Reviews. 2001;5(4):287–297. doi: 10.1053/smrv.2001.0162. [DOI] [PubMed] [Google Scholar]
- Ross Catherine E, Mirowsky John. Neighborhood Disadvantage, Disorder, and Health. Journal of Health and Social Behavior. 2001 Sep;42:258–276. [PubMed] [Google Scholar]
- Rubin Donald B. Multiple Imputation for Nonresponse in Surveys. New York, NY: J. Wiley & Sons; 1987. [Google Scholar]
- Sarwari AR, Fredman L, Langenberg P, Magaziner J. Prospectives Study on the Relation between Living Arrangement and Change in Functional Health Status of Elderly Women. American Journal of Epidemiology. 1998;147(4):370–378. doi: 10.1093/oxfordjournals.aje.a009459. [DOI] [PubMed] [Google Scholar]
- Sbarra David A. Marriage Protects Men from Clinically Meaningful Elevations in C-Reactive Protein: Results from the National Social Life, Health, and Aging Project. Psychosomatic Medicine. 2009;71(8):828–835. doi: 10.1097/PSY.0b013e3181b4c4f2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schnittker Jason. Look (Closely) at All the Lonely People: Age and the Social Psychology of Social Support. Journal of Aging and Health. 2007;19:659–682. doi: 10.1177/0898264307301178. [DOI] [PubMed] [Google Scholar]
- Schwartz Skai W, Cornoni-Huntley Joan, Cole Stephen R, Hays Judith C, Blazer Dan G, Schocken Douglas D. Are Sleep Complaints and Independent Risk Factor for Myocardial Infarction? Annals of Epidemiology. 1998;8:384–392. doi: 10.1016/s1047-2797(97)00238-x. [DOI] [PubMed] [Google Scholar]
- Seeman Teresa E, Berkman Lisa F, Blazer Dan, Rowe John W. Social ties and support and neuroendocrine function: The MacArthur studies of successful aging. Annals of Behavioral Medicine. 1994;16(2):95–106. [Google Scholar]
- Seeman Teresa E. Health Promoting Effects of Friends and Family on Health Outcomes in Older Adults. American Journal of Health Promotion. 2000;14(3):362–370. doi: 10.4278/0890-1171-14.6.362. [DOI] [PubMed] [Google Scholar]
- StataCorp. Statistical Software (Release 13) College Station, TX: StataCorp LP; 2011. [Google Scholar]
- Thoits Peggy A. Mechanisms Linking Social Ties and Support to Physical and Mental Health. Journal of Health and Social Behavior. 2011;52(2):145–161. doi: 10.1177/0022146510395592. [DOI] [PubMed] [Google Scholar]
- Umberson Debra. Family Status and Health Behaviors: Social Control as a Dimension of Social Integration. Journal of health and social behavior. 1987:306–319. [PubMed] [Google Scholar]
- Umberson Debra. Gender, Marital Status, and the Social Control of Health Behavior. Social Science & Medicine. 1992;34(8):907–917. doi: 10.1016/0277-9536(92)90259-s. [DOI] [PubMed] [Google Scholar]
- Umberson Debra, Williams Kristi. Marital Quality, Health, and Aging: Gender Equity? Journal of Gerontology Series B: Psychological and Social Sciences. 2005;60:S109–S113. doi: 10.1093/geronb/60.special_issue_2.s109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Umberson Debra, Williams Kristi, Powers Daniel A, Liu Hui, Needham Belinda. You Make Me Sick: Marital Quality and Health over the Life Course. Journal of Health and Social Behavior. 2006;47(1):1–16. doi: 10.1177/002214650604700101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vasilopoulos Terrie, Kotwal Ashwin, Huisingh-Scheetz Megan, Waite Linda, McClintock Martha and William Dale. Comorbidity and Chronic Conditions in the National Social Life, Health, and Aging Project Wave 2. Journal of Gerontology Series B: Psychological and Social Sciences. 2014 doi: 10.1093/geronb/gbu025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Venn Susan, Arber Sara, Meadows Robert, Hislop Jenny. The Fourth Shift: Exploring the Gendered Nature of Sleep Disruption among Couples with Children. British Journal of Sociology. 2008;59(1):79–97. doi: 10.1111/j.1468-4446.2007.00183.x. [DOI] [PubMed] [Google Scholar]
- Vitiello Michael V. Sleep in Normal Aging. Sleep Medicine Clinics. 2006;1:17–176. doi: 10.1016/j.jsmc.2017.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waite Linda. Does Marriage Matter? Demography. 1995;32(4):483–507. [PubMed] [Google Scholar]
- Waite Linda, Gallagher Maggie. The Case for Marriage: Why Married People are Happier, Healthier, and Better Off Financially. New York, NY: Broadway Books; 2001. [Google Scholar]
- Waite Linda, Laumann EO, Levinson W, Lindau ST, O'Muircheartaigh CA. National Social Life, Health, and Aging Project (NSHAP). ICPSR20541-v5. Ann Arbor, MI: Inter-university Consortium for Political and Social Research [distributor]; 2010. [Google Scholar]
- Warner David F, Kelley-Moore Jessica. The Social Context of Disablement among Older Adults: Does Marital Quality Matter for Loneliness? Journal of Health and Social Behavior. 2012;53(1):50–66. doi: 10.1177/0022146512439540. [DOI] [PubMed] [Google Scholar]
- Wilcox Sara, King Abby C. Sleep Complaints in Older Women Who Are Family Caregivers. Journal of Gerontology: Series B Psychological and Social Sciences. 1999;54B(3):P189–P198. doi: 10.1093/geronb/54b.3.p189. [DOI] [PubMed] [Google Scholar]
- Wilmoth J, Koso G. Does Marital History Matter? Marital Status and Wealth Outcomes among Preretirement Adults. Journal of Marriage and the Family. 2002;64(1):254–268. [Google Scholar]
- Wolfson Amy R, Carskadon Mary A, Acebo Christine, Seifer Ronald, Fallone Gahan, Labyak Susan E, Martin Jennifer L. Evidence for the Validity of a Sleep Habits Survey for Adolescents. Sleep. 2003;26(2):213–216. doi: 10.1093/sleep/26.2.213. [DOI] [PubMed] [Google Scholar]
- World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders: Cinical Descriptions and Diagnostic Guidelines. 2012 [Google Scholar]
- Zepelin Harold, McDonald Cathleen S, Zammit Gary K. Effects of Age on Auditory Awakening Thresholds. Journal of Gerontology. 1984;39(3):294–300. doi: 10.1093/geronj/39.3.294. [DOI] [PubMed] [Google Scholar]
- Zhang Lin, Samet Jonathan, Caffo Brian, Punjabi Naresh M. Cigarette Smoking and Nocturnal Sleep Architecture. American Journal of Epidemiology. 2006;164(6):529–537. doi: 10.1093/aje/kwj231. [DOI] [PubMed] [Google Scholar]
- Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatrica Scandinavica. 1983;67(6):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]