Abstract
Background: Over the past decade over two-thirds of U.S. hospitals have established palliative care programs. National data on palliative care program staffing and its association with operational outcomes are limited.
Objective: The objective of this report is to examine the impact of palliative care program staffing on access to palliative care in U.S. hospitals.
Methods: Data from the National Palliative Care Registry™ for 2014 were used to calculate staffing levels, palliative care service penetration, and time to initial palliative care consultation for 398 palliative care programs operating across 482 U.S. hospitals.
Results: Hospital-based palliative care programs reported an average service penetration of 4.4%. Higher staffing levels were associated with higher service penetration; higher service penetration was associated with shorter time to initial palliative care consultation.
Discussion: This report demonstrates that operational effectiveness, as measured by staffing and palliative care service penetration, is associated with shorter time to palliative care consultation.
Introduction
Palliative care programs improve patient and family satisfaction, reduce symptom burden,1 and in a few studies, prolong life.2 Early palliative care consultation also reduces hospital costs.3
The National Palliative Care Registry™ is a repository for information on the nation's hospital palliative care programs. The registry tracks the development of palliative care programs and promotes standardization of palliative care to enhance quality. This study reports on the impact of staffing on palliative care service penetration and penetration on time to consultation in U.S. hospitals.
Methods
Hospital palliative care programs participating in the National Palliative Care Registry™ report on operational metrics including palliative care team staffing, service penetration (palliative care consultations as a percentage of total hospital admissions), and time to initial palliative care consultation. Palliative care program staffing was calculated as total funded full-time equivalent (FTE) per 10,000 admissions for physicians, advanced practice registered nurses, physician assistants, chaplains, social workers, psychologists, and registered nurses. Time to consultation is the average number of days from hospital admission to initial palliative care consultation. Programs were grouped by quartile for penetration and staffing, and mean penetration and time to consultation were calculated by quartile. Confidence intervals for means are reported.
Results
In 2014, 398 programs providing palliative care services to 482 hospitals participated in the registry, representing over one-quarter of all hospitals with more than 50 beds. Thirty-four percent (137/398) of registry participating programs were from hospitals with 300 beds or more.
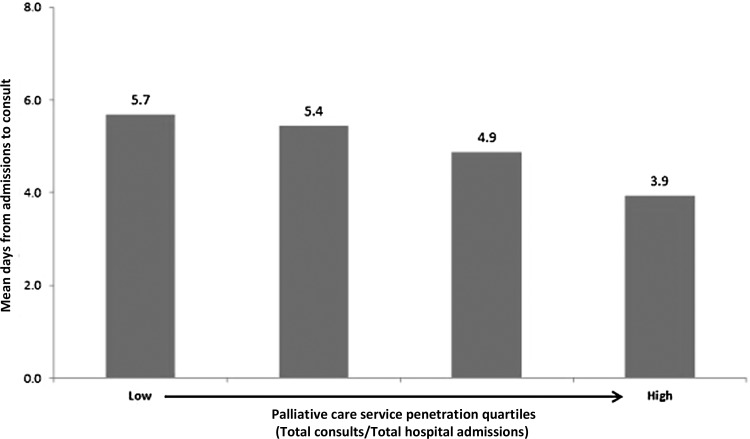
Programs reporting to the registry reported an average service penetration of 4.4% (CI = 4.1, 4.7) of annual hospital admissions. Programs in the highest quartile of service penetration reached an average of 8.5% (CI = 7.8, 9.1) of annual hospital admissions. Programs with the highest staffing levels (≥2.7 FTE per 10,000 admissions) reached 6.5% (CI = 5.6, 7.4) of admissions, while programs in the lowest staffing quartile (<1.2 FTE per 10,000 admissions) reached 2.9% (CI = 2.5, 3.3). Palliative care programs in the highest service penetration quartile (≥5.3%) also report shorter times to palliative care consult compared to programs in the lowest quartile (<2.4%), 3.9 (CI = 3.6, 4.3) versus 5.7 (CI = 5.2, 6.2) days, respectively (see Fig. 1).
FIG. 1.
Programs with higher palliative care service penetration report shorter time to initial consult.
Discussion
Over 66% of U.S. hospitals with more than 50 beds and over 90% of hospitals with 300 beds or more currently report palliative care programs, with higher prevalence among public, nonprofit and teaching hospitals.4 The past decade has shown a steady increase in palliative care service penetration, an estimate of how well these programs are reaching patients in need.
The findings reported here demonstrate that higher service penetration is associated with shorter time to consultation, helping to ensure that patients are reached early enough in their hospital stay to influence its subsequent course. However, insufficient staffing continues to present a barrier to reaching patients in need of palliative care services.
Additional research is needed to understand optimal composition and capacity of interdisciplinary palliative care teams; the role of triggers or checklists in improving timely access; and how accreditation and regulatory policy could improve access to high-quality palliative care.
Acknowledgments
The National Palliative Care Registry™ is a project of the Center to Advance Palliative Care and the National Palliative Care Research Center. This work was supported by grants from the National Institute on Aging (R24AG044300, P30AG028741). Dr. Morrison is the recipient of a Clinical Research Professor Award from the American Cancer Society.
Author Disclosure Statement
The authors have no competing financial interests. The sponsors had no role in the design, conduct, analyses, and preparation of the manuscript.
References
- 1.Kelley AS, Morrison RS: Palliative care for the seriously ill. N Engl J Med 2015;373:747–755 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bakitas M, Lyons KD, Hegel MT, et al. : Effects of a palliative care intervention on clinical outcomes in patients with advanced cancer: The Project Enable III randomized controlled trial. J Clin Oncol 2009;33:1438–1448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.May P, Garrido MM, Cassel JB, et al. : Prospective cohort study of hospital palliative care teams for inpatients with advanced cancer: Earlier consultation is associated with larger cost-saving effect. J Clin Oncol 2015;33:2745–2752 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Dumanovsky T, Augustin R, Rogers M, et al. : The growth of palliative care in U.S. hospitals: A status report. J Palliat Med 2015. [E-pub ahead of print.] [DOI] [PMC free article] [PubMed] [Google Scholar]