Abstract
Kaposi sarcoma (KS) is a low-grade angioproliferative tumor associated with infection with human herpes virus 8 (HHV-8). The disease was named after Moritz Kaposi, a Hungarian dermatologist who first described it in 1872 as ‘idiopathic multiple pigmented sarcoma of the skin.’ HHV-8 infection is required for the development of KS, but not all infected persons develop the disease. KS is also considered an acquired immune deficiency syndrome (AIDS)-defining illness by the Centers for Disease Control and Prevention guidelines. According to data from the United States AIDS and cancer registries, both KS and non-Hodgkin lymphoma are the most common malignancies associated with human immunodeficiency virus (HIV) infection. However, the incidence of both malignancies has decreased dramatically since 1996 following the widespread utilization of highly active antiretroviral therapies. HIV-associated KS can involve virtually any site in the body including lymph nodes, gastrointestinal tract, respiratory system, heart, pericardium, bone marrow, and other visceral organs. However, cutaneous disease is the most common and is the usual initial presentation for KS. KS-related pericardial effusion can be a life-threatening emergency and should be considered in HIV/AIDS patients who present with signs and symptoms of pericardial effusion. The importance of diagnosing and differentiating KS-related pericardial effusion from other causes of pericardial effusion lies in the differences in the treatment and management in comparison to other etiologies of pericardial effusion. We report a case of a 54-year old man who presented to our hospital with a large pericardial effusion and was subsequently diagnosed to have HIV-related KS pericardial effusion. A brief review of the literature on the diagnosis and management is also presented.
Keywords: Kaposi sarcoma, malignancy, acquired immune deficiency syndrome, human immunodeficiency virus, pericardial effusion
A 54-year-old Hispanic male who was diagnosed with human immunodeficiency virus (HIV) infection, acquired immune deficiency syndrome (AIDS), and AIDS-related cutaneous Kaposi sarcoma (KS; affecting his nose, back, and left leg) 1 year earlier was seen by his primary care physician (PCP) with cough and exertional dyspnea. He was empirically treated with amoxicillin, but failed to show clinical improvement. During a follow-up visit to his PCP, he was noted to be hypoxemic on room air and was sent to our hospital emergency department for further evaluation.
At the time of his initial HIV diagnosis 9 months earlier, he was found to have a CD4 count of <20 (500–1,600) with 2% (25–65%) CD4 cells. Following the diagnosis, he was started on appropriate prophylactic therapy for opportunistic infections as well as highly active antiretroviral therapy (HAART). Unfortunately, he consistently demonstrated a lack of adherence to his medications. One month after the initial HIV diagnosis, he was noted to have systemic KS involving the pulmonary tree and bone marrow following presentation with hemoptysis and pancytopenia. Both processes were biopsy-proven. His HAART regimen was adjusted, and his symptoms and cell counts subsequently improved. He also underwent multiple cycles of chemotherapy with doxorubicin for the visceral involvement of KS.
In the emergency department, he was found to be hemodynamically stable with a low-grade fever and an oxygen saturation of 94% on room air. A computed tomography (CT) scan of his chest revealed a large pericardial effusion, but did not show any focal pulmonary infiltrates or evidence of pulmonary embolism. In light of these findings, he was admitted to the intensive care unit for closer monitoring. Concerns regarding poor adherence to his medications were again raised.
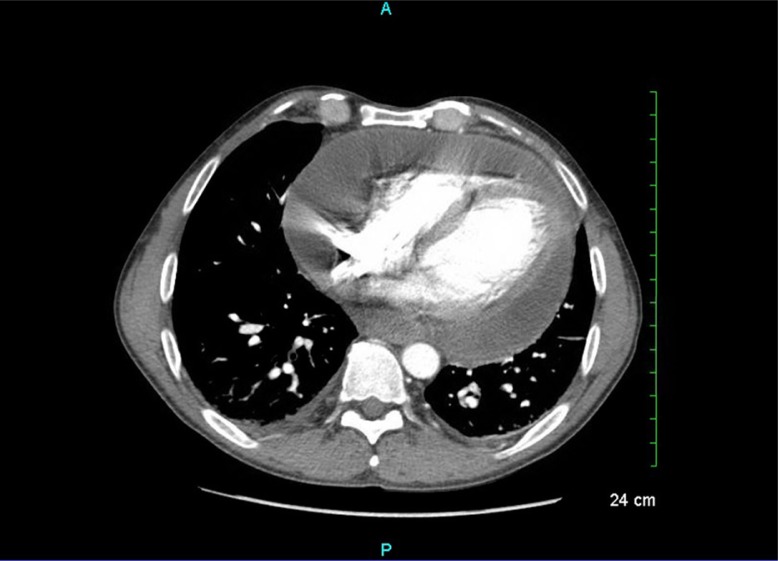
On the second day of his hospitalization, a transthoracic echocardiogram was done and revealed a large anterior and moderate posterior pericardial effusion with evidence of early pericardial tamponade. A CT scan of the chest also showed the pericardial effusion (Fig. 1). He underwent a pericardiocentesis, and 900 cc of bloody fluid was aspirated. A pericardial tube was placed, and this drained an additional 300 cc of bloody fluid. Laboratory examinations including serologic tests for acute EBV and CMV viral infections were negative. Pericardial fluid bacterial, fungal, and acid fast cultures were negative. Pericardial fluid cytology was also negative. However, the pericardial fluid cell count was compatible with hemopericardium. At that time, he had a viral load of 1,395 copies/ml, with a CD4 count of 113 (500–1,600). Multiple follow-up echocardiograms performed during the hospitalization showed stable small residual pericardial effusion, prompting removal of the pericardial tube on the fifth day of hospitalization. Given his stable disease and absence of recurrence of the effusion, treatment with anti-inflammatory agents was deferred. He was discharged on the sixth day with instructions for close follow-up visits with transthoracic echocardiogram and positron emission tomography/computed tomography (PET/CT) scan.
Fig. 1.
CT scan of the chest on the second day of hospitalization showing large pericardial effusion.
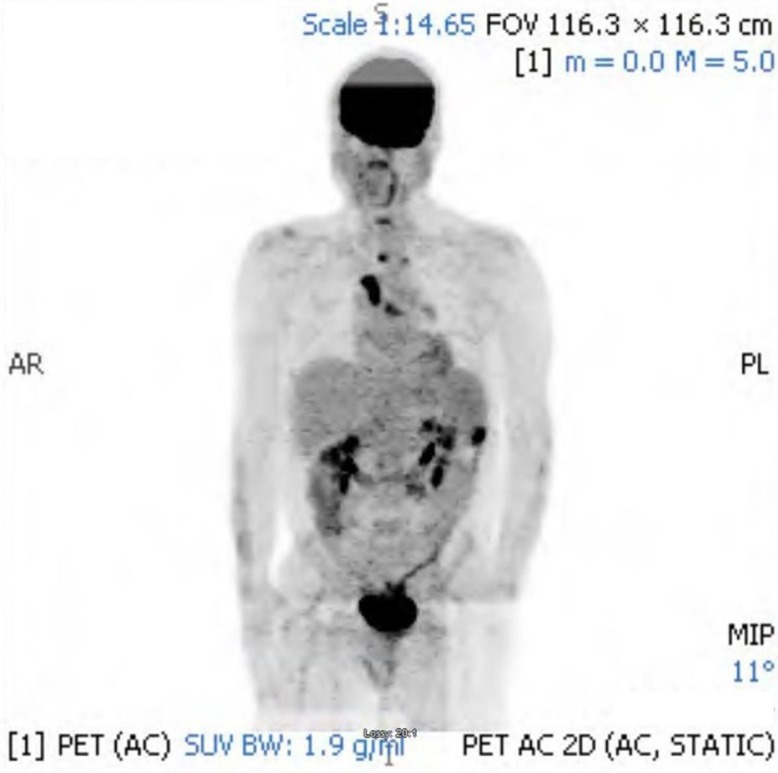
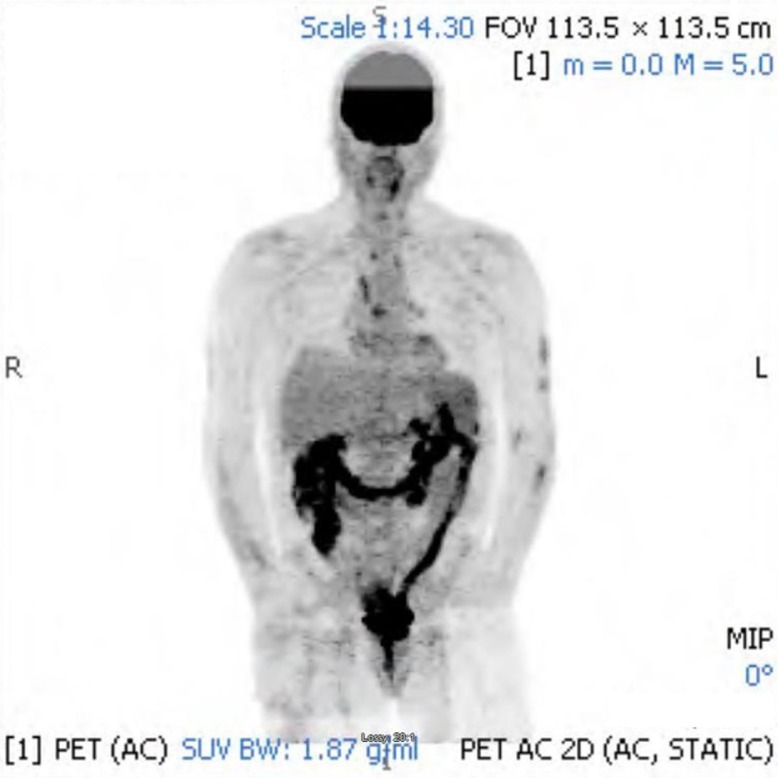
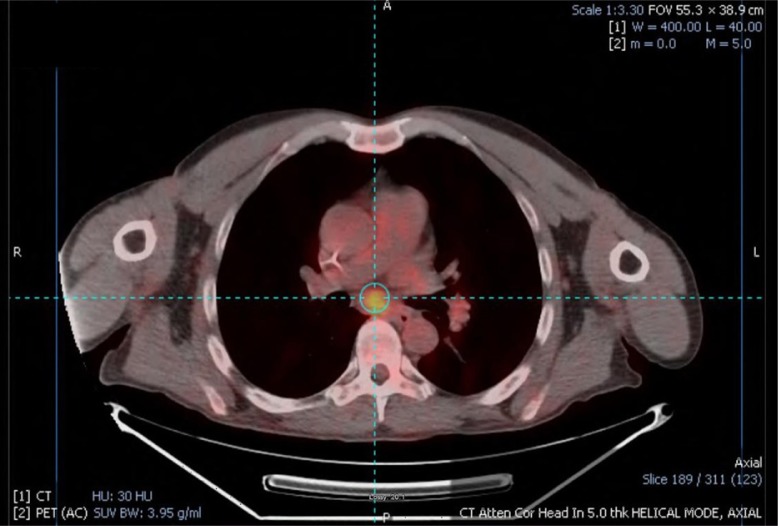
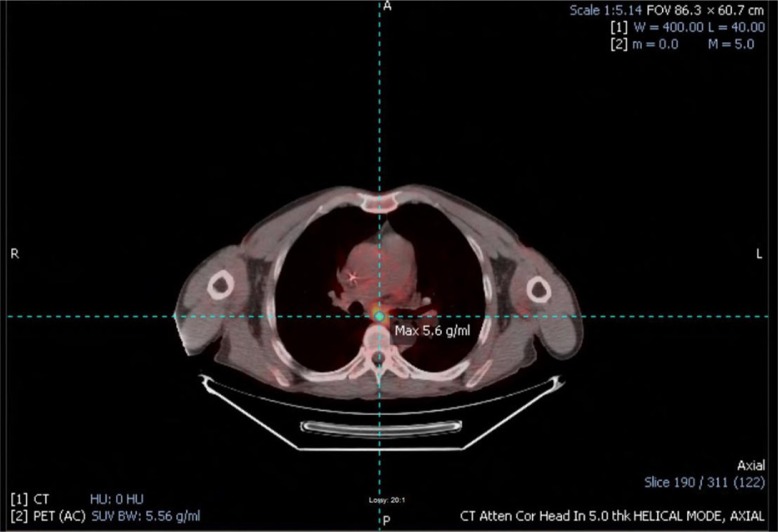
The follow-up PET/CT (Figs. 2–4) scan done after 2 months of discharge showed FDG avid areas in the right paratracheal (SUV of 9.8) and subcarinal (SUV 5.6) tissues representing pericardial involvement of KS. The scan also showed FDG avid areas in the left upper abdominal quadrant. It, however, failed to show any pulmonary tree or bone marrow involvement. A repeat PET/CT (Figs. 5, 6) done after 3 months to monitor the progression of the disease showed diminished metabolic activity in the previously seen right paratracheal and subcarinal regions with SUV up to 3.9 compared to 9.8 on the previous scan. There was also no subdiaphragmatic involvement.
Fig. 2.
The initial follow-up PET scan, 2 months after hospital discharge, showing FDG avid areas in the right paratracheal and subcarinal tissue representing pericardial involvement of Kaposi sarcoma. It also shows FDG avid areas in the abdominal left upper quadrant, but it failed to show any pulmonary tree or bone marrow involvement.
Fig. 4.
The initial follow-up PET/CT scan, 2 months after hospital discharge, showing FDG avid areas in the right paratracheal (SUV of 9.8) tissue representing pericardial involvement of Kaposi sarcoma.
Fig. 5.
The repeat PET scan done 3 months after the initial PET scan showing diminished metabolic activity in previously seen right paratracheal and subcarinal region with SUV up to 3.9 compared to 9.8 on the previous scan. There was also no subdiaphragmatic involvement.
Fig. 6.
The repeat PET/CT scan done 3 months after the initial PET/CT scan showing diminished metabolic activity in previously seen right subcarinal region with SUV up to 3.9 compared to 5.6 on the previous scan.
Fig. 3.
The initial follow-up PET/CT scan, 2 months after hospital discharge, showing FDG avid areas in the subcarinal (SUV 5.6) tissue representing pericardial involvement of Kaposi sarcoma.
In light of the improved appearance of the lesions, resolution of the pericardial effusion, and improved medication adherence, the patient was continued on the same HAART regimen with close monitoring, and the lesions were attributed to KS.
Discussion
HIV-associated cutaneous KS is characterized by the appearance of purplish, reddish blue, or dark brown/black macules, plaques, and nodules on the skin. Cutaneous KS can be one of the first manifestations of HIV infection and AIDS, as in our patient, and can give a clue for possible visceral involvement as the cause of an appropriate patient's symptoms. HHV-8 infection is required for the development of KS (1–4). The incidence of KS has decreased dramatically since 1996 following the widespread utilization of highly active antiretroviral therapies (5).
HIV-associated KS involvement has been observed in almost all visceral sites including the lymph nodes, gastrointestinal (GI) tract, respiratory system, liver, pancreas, heart, pericardium, testes, bone marrow, bone, and skeletal muscles (6, 7), but involvement of these sites is rarely diagnosed.
The most frequent sites of non-cutaneous disease are the oral cavity, GI tract, and respiratory system. Visceral involvement as the initial manifestation of KS is relatively uncommon. Furthermore, visceral disease now appears to be much less frequent with the use of antiretroviral therapy (ART) as well as other treatment options (8).
In most cases, KS has an indolent course and has a good prognosis.
Asymptomatic patients with HIV-associated KS usuallydo not require radiographic evaluation of the affected area due to the chronic indolent course of disease. Also, screening for distant organ involvement is not needed, given the low frequency of radiographically evident metastatic disease.
When suspected, fluorine-18-fluorodeoxyglucose PET/CT is a useful tool in detecting and monitoring the extent and progression of visceral KS (9–13); however, no study has been conducted so far comparing the effectiveness of the multiple imaging modalities available for tumor staging. Bronchoscopy and upper and lower endoscopy are frequently used tools for the diagnosis of pulmonary and GI KS, respectively, when involvement of these organs is suspected.
Pericardial effusion is a known complication of HIV infection. However, the incidence has declined dramatically since the application of ART and it is currently considered a rare complication of HIV infection (14, 15). Some studies suggest that KS is responsible for 5–7% of HIV-associated pericardial effusions (16, 17). Other causes of pericardial effusion in HIV patients include mycobacterial, bacterial, fungal, and viral infections, and lymphoma (16, 17).
There are multiple cases in the literature of biopsy-proven KS-related pericardial effusions with the diagnoses established either at autopsy or in symptomatic patients (18–21). Other cases of KS-related pericardial effusions were reported based on the course of the disease (22).
The major goals of therapy are to prevent progression of disease, to reduce tumor size thereby reducing organ compromise and edema, and to reduce psychological stress (8).
Systemic treatment with potent combination ART is the main method of treatment. Further treatment beyond ART depends on the extent of disease, location, the rapidity of tumor growth, HIV viral load, CD4 cell count, and the patient's overall condition and preference. Options include intralesional chemotherapy, systemic chemotherapy, and radiation therapy (8, 22–26).
Conclusions
KS-related pericardial effusion can be a life-threatening emergency and should be in the differential diagnosis in HIV-positive patients who present with signs and symptoms of pericardial effusion.
The importance of differentiating KS-related pericardial effusion from other causes of pericardial effusion lies in the differences in treatment in comparison to other causes of pericardial effusion.
In our patient, a high index of suspicion for the possible involvement of KS led to the correct diagnosis and thus the successful management.
Conflict of interest and funding
The authors have not received any funding or benefits from industry or elsewhere to conduct this study.
References
- 1.Chang Y, Cesarman E, Pessin MS, Lee F, Culpepper J, Knowles DM, et al. Identification of herpesvirus-like DNA sequences in AIDS-associated Kaposi's sarcoma. Science. 1994;266(5192):1865. doi: 10.1126/science.7997879. [DOI] [PubMed] [Google Scholar]
- 2.Moore PS, Chang Y. Detection of herpesvirus-like DNA sequences in Kaposi's sarcoma in patients with and without HIV infection. N Engl J Med. 1995;332(18):1181. doi: 10.1056/NEJM199505043321801. [DOI] [PubMed] [Google Scholar]
- 3.Sitas F, Carrara H, Beral V, Newton R, Reeves G, Bull D, et al. Antibodies against human herpesvirus 8 in black South African patients with cancer. N Engl J Med. 1999;340(24):1863. doi: 10.1056/NEJM199906173402403. [DOI] [PubMed] [Google Scholar]
- 4.Gao SJ, Kingsley L, Hoover DR, Spira TJ, Rinaldo CR, Saah A, et al. Seroconversion to antibodies against Kaposi's sarcoma-associated herpesvirus-related latent nuclear antigens before the development of Kaposi's sarcoma. N Engl J Med. 1996;335(4):233. doi: 10.1056/NEJM199607253350403. [DOI] [PubMed] [Google Scholar]
- 5.Biggar RJ, Chaturvedi AK, Goedert JJ, Engels EA. HIV/AIDS Cancer Match Study. AIDS-related cancer and severity of immunosuppression in persons with AIDS. J Natl Cancer Inst. 2007;99(12):962. doi: 10.1093/jnci/djm010. [DOI] [PubMed] [Google Scholar]
- 6.Ioachim HL, Adsay V, Giancotti FR, Dorsett B, Melamed J. Kaposi's sarcoma of internal organs. A multiparameter study of 86 cases. Cancer. 1995;75(6):1376. doi: 10.1002/1097-0142(19950315)75:6<1376::aid-cncr2820750621>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 7.Caponetti G, Dezube BJ, Restrepo CS, Pantanowitz L. Kaposi sarcoma of the musculoskeletal system: A review of 66 patients. Cancer. 2007;109(6):1040. doi: 10.1002/cncr.22500. [DOI] [PubMed] [Google Scholar]
- 8.Bower M, Dalla Pria A, Coyle C, Andrews E, Tittle V, Dhoot S, et al. Prospective stage-stratified approach to AIDS-related Kaposi's sarcoma. J Clin Oncol. 2014;32(5):409. doi: 10.1200/JCO.2013.51.6757. [DOI] [PubMed] [Google Scholar]
- 9.Sathekge M, Maes A, Van de Wiele C. FDG-PET imaging in HIV infection and tuberculosis. Semin Nucl Med. 2013;43(5):349–66. doi: 10.1053/j.semnuclmed.2013.04.008. [DOI] [PubMed] [Google Scholar]
- 10.Morooka M, Ito K, Kubota K, Yanagisawa K, Teruya K, Hasuo K, et al. Usefulness of F-18 FDG PET/CT in a case of Kaposi sarcoma with an unexpected bone lesion. Clin Nucl Med. 2011;36(3):231–4. doi: 10.1097/RLU.0b013e318208f4ea. [DOI] [PubMed] [Google Scholar]
- 11.Mankia SK, Miller RF, Edwards SG, Ramsay A, Lee SM. The response of HIV-associated lymphadenopathic Kaposi sarcoma to highly active antiretroviral therapy evaluated by 18F-FDG PET/CT. Clin Nucl Med. 2012;37(7):692–3. doi: 10.1097/RLU.0b013e3182485261. [DOI] [PubMed] [Google Scholar]
- 12.Reuter S, Vrachimis A, Huss S, Wardelmann E, Weckesser M, Pavenstädt H. A challenging case of rapid progressive Kaposi sarcoma after renal transplantation: Diagnostics by FDG PET/CT. Medicine (Baltimore) 2014;93(11):e67. doi: 10.1097/MD.0000000000000067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.van de Luijtgaarden A, van der Ven A, Leenders W, Kaal S, Flucke U, Oyen W, et al. Imaging of HIV-associated Kaposi sarcoma; F-18-FDG-PET/CT and In-111-bevacizumabscintigraphy. J Acquir Immune Defic Syndr. 2010;54(4):444–6. doi: 10.1097/QAI.0b013e3181cdf61f. [DOI] [PubMed] [Google Scholar]
- 14.Lind A, Reinsch N, Neuhaus K, Esser S, Brockmeyer N, Potthoff A, et al. Pericardial effusion of HIV-infected patients – Results of a prospective multicenter cohort study in the era of antiretroviral therapy. Eur J Med Res. 2011;16:480–3. doi: 10.1186/2047-783X-16-11-480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Heidenreich PA, Eisenberg MJ, Kee LL, Somelofski CA, Hollander H, Schiller NB, et al. Pericardial effusion in AIDS. Incidence and survival. Circulation. 1995;92:3229–34. doi: 10.1161/01.cir.92.11.3229. [DOI] [PubMed] [Google Scholar]
- 16.Gowda RM, Khan IA, Mehta NJ, Gowda MR, Sacchi TJ, Vasavada BC. Cardiac tamponade in patients with human immunodeficiency virus disease. Angiology. 2003;54(4):469–74. doi: 10.1177/000331970305400411. [DOI] [PubMed] [Google Scholar]
- 17.Chen Y, Brennessel D, Walters J, Johnson M, Rosner F, Raza M. Human immunodeficiency virus-associated pericardial effusion: Report of 40 cases and review of the literature. Am Heart J. 1999;137(3):516–21. doi: 10.1016/s0002-8703(99)70500-4. [DOI] [PubMed] [Google Scholar]
- 18.Stotka JL, Good CB, Downer WR, Kapoor WN. Pericardial effusion and tamponade due to Kaposi's sarcoma in acquired immunodeficiency syndrome. Chest. 1989;95(6):1359–61. doi: 10.1378/chest.95.6.1359. [DOI] [PubMed] [Google Scholar]
- 19.Kabangila R, Mahalu W, Masalu N, Jaka H, Peck RN. Recurrent, massive Kaposi's sarcoma pericardial effusion presenting without cutaneous lesions in an HIV infected adult: A case report. Tanzan J Health Res. 2011;13(1):82–5. doi: 10.4314/thrb.v13i1.59465. [DOI] [PubMed] [Google Scholar]
- 20.Chyu KY, Birnbaum Y, Naqvi T, Fishbein MC, Siegel RJ. Echocardiographic detection of Kaposi's sarcoma causing cardiac tamponade in a patient with acquired immunodeficiency syndrome. Clin Cardiol. 1998;21(2):131–3. doi: 10.1002/clc.4960210217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cammarosano C, Lewis W. Cardiac lesions in acquired immune deficiency syndrome (AIDS) J Am Coll Cardiol. 1985;5(3):703–6. doi: 10.1016/s0735-1097(85)80397-1. [DOI] [PubMed] [Google Scholar]
- 22.Maradona JA, Carton JA, Asensi V, Rodríguez-Guardado A. AIDS-related Kaposi's sarcoma with chylothorax and pericardial involvement satisfactorily treated with liposomal doxorubicin. AIDS. 2002;16(5):806. doi: 10.1097/00002030-200203290-00025. [DOI] [PubMed] [Google Scholar]
- 23.Bower M, Collins S, Cottrill C, Cwynarski K, Montoto S, Nelson M, et al. British HIV Association guidelines for HIV-associated malignancies 2008. HIV Med. 2008;9(6):336. doi: 10.1111/j.1468-1293.2008.00608.x. [DOI] [PubMed] [Google Scholar]
- 24.Krown SE. Highly active antiretroviral therapy in AIDS-associated Kaposi's sarcoma: Implications for the design of therapeutic trials in patients with advanced, symptomatic Kaposi's sarcoma. J Clin Oncol. 2004;22(3):399. doi: 10.1200/JCO.2004.08.064. [DOI] [PubMed] [Google Scholar]
- 25.Gbabe OF, Okwundu CI, Dedicoat M, Freeman EE. Treatment of severe or progressive Kaposi's sarcoma in HIV-infected adults. Cochrane Database Syst Rev. 2014;8 doi: 10.1002/14651858.CD003256.pub2. CD003256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Nichols CM, Flaitz CM, Hicks MJ. Treating Kaposi's lesions in the HIV-infected patient. J Am Dent Assoc. 1993;124(11):78. doi: 10.14219/jada.archive.1993.0231. [DOI] [PubMed] [Google Scholar]