Abstract
Since the advent of anti-retroviral therapy, patients with HIV are living longer, and in the year 2015, over half of those infected with the virus will be older than age 50. Moreover, as the general aging population continues to grow, more elderly individuals will become newly infected with HIV. Older patients with HIV contribute to high numbers of initial and rehospitalizations, have longer lengths of hospital day stays, and are at increased risk of death compared to younger patients with HIV and those without HIV. Age-related comorbidities can be exaggerated in HIV-positive patients on and off therapy. Furthermore, signs and symptoms of HIV and AIDS may mimic features seen in the normal aging process of older adults. Internists caring for patients in inpatient settings will be expected to care for and diagnose increasing numbers of older patients with HIV. This will be critical for improving quality of patient care, reducing morbidity and mortality, and managing newly diagnosed patients earlier in the disease course while reducing spread of the virus. Internists should be central leaders in the development of targeted and non-targeted HIV screening efforts in inpatient general medicine wards.
Keywords: HIV, vulnerable populations, aging, inpatients, healthcare utilization, screening
In the early 1980s, a diagnosis of HIV generally meant death from AIDS-related opportunistic infections or malignancies. Without effective treatment, life expectancy for most was about a year from the time of presentation of full-blown AIDS. Highly active antiretroviral therapy (ART), available by the late 1990s, dramatically changed the face of this illness (1). Individuals over age 55 made up more than a quarter (26%, 313,200) of patients with HIV in the United States in 2011 (2). The Centers for Disease Control and Prevention (CDC) projects that in 2015 more than 50% of patients with HIV will be older than age 50 (3). By 2020, 70% of people with HIV will be in this age range (4). The increasing prevalence of HIV is due in part to the increasing incidence in older adults, many of whom do not perceive themselves to be at risk (5). In addition, individuals infected with HIV are living longer (1). HIV is now considered a chronic illness, and patients are more likely to suffer and succumb to non-AIDS-related ailments similar to their HIV-free counterparts (6). These non-HIV conditions, such as hepatitis, coronary artery disease (CAD), chronic obstructive pulmonary disease, renal disease, and certain malignancies, progress more rapidly in HIV-infected individuals than in those without HIV infection (6). Hospital medicine doctors can play a key role in managing patients with HIV who are living longer and are more susceptible to poorer outcomes from common age-related comorbidities.
Being aware of this age shift is important for several reasons: 1) older adults with HIV are at increased risk for readmission and prolonged hospitalizations (7), 2) HIV is underdiagnosed (5, 8), and hospital admissions are often an opportunity for routine HIV screening, and 3) age-related comorbidities are exaggerated in HIV-positive patients even on ART (9). This article seeks to heighten physicians’ awareness of this paradigm shift and of the newly emerging face of HIV encountered in hospital settings.
Higher hospital utilization in older adults with HIV
Since the advent of ART, inpatient healthcare utilization by HIV patients has greatly decreased; however, for HIV-positive patients aged 50 or older, inpatient utilization has actually increased (7). Furthermore, Bachhuber et al. found that hospitalization rates among people living with HIV in the United States were higher than previously estimated (10). Older HIV-infected patients have longer lengths of stay and more frequent hospitalizations compared to their younger counterparts (7). Indeed, older HIV-infected patients contribute to growing numbers of overall inpatient admissions (7). Patients receiving treatment late in the HIV disease course have substantially higher direct medical expenditures compared to those managed earlier (11). Inpatient providers should aim to diagnose HIV infection early in order to decrease morbidity and mortality and curb healthcare utilization.
Routine screening for HIV in the hospital setting
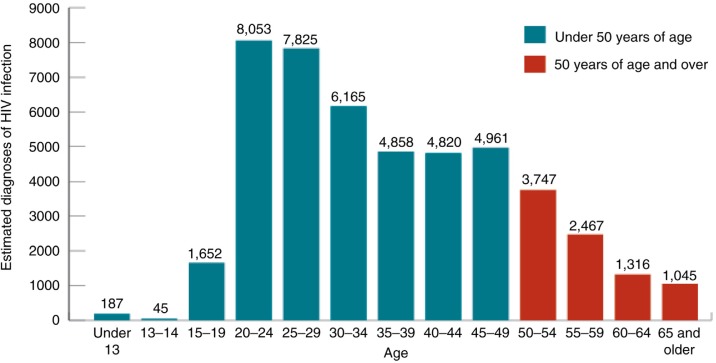
In 2013, the CDC estimated that 8,575 new HIV diagnoses in the United States were in patients aged 50 or older (Fig. 1) (2). These individuals are usually diagnosed and treated later in the disease course, portending poorer prognoses (2). According to the CDC, half of the patients older than age 50 diagnosed with HIV are concurrently diagnosed with AIDS (4). Older patients symptomatic with HIV or AIDS are often misdiagnosed as having signs or symptoms associated with aging, such as weight loss, fatigue, and memory loss (8). Missed opportunities for an earlier diagnosis of HIV may arise because healthcare providers and older patients do not typically discuss sexual practices or drug use (5). Furthermore, this patient population is not usually considered at risk for HIV (2, 12).
Fig. 1.
Estimated diagnoses of HIV infection by age, 2013, United States.
Inpatient providers should include HIV/AIDS in the differential diagnosis when managing older patients and they should know HIV screening guidelines. The CDC recommends that all individuals aged between 13 and 64 be offered HIV testing as part of routine medical care regardless of risk factors (13). Individuals with risk factors should be tested more frequently (at least annually) (13). Signed consent and pretest counseling are not required. Screening should occur during any contact with healthcare systems, including inpatient settings (14). Given increasing infection rates in older individuals, screening individuals older than age 64 is reasonable. Hospitalization provides unique opportunities for routine screening. For persons without primary care providers, hospitalizations may be their only opportunity for such testing (15).
At our hospital, routine HIV testing has been successfully implemented in our emergency department, and we are currently upscaling the practice to our inpatient medicine wards. Collaborative work involving leaders from the departments of Hospital/Internal Medicine, Infectious Diseases, Psychiatry, Pathology, Case Management, Nursing, Adolescent Medicine, Emergency Medicine, and Addiction Medicine has proven critical in the initiation, expansion, and sustainability of our HIV screening program. Patients that test positive are evaluated and educated by inpatient infectious disease specialists and are linked to appropriate outpatient care for ongoing monitoring and management.
As suggested in a recent publication by the JACQUES Initiative, a six-step process to systematic organizational change consisting of 1) stake-holder buy-in, 2) identification of an interdisciplinary leadership team, 3) infrastructure development, 4) staff education, 5) implementation, and 6) continuous quality improvement will be essential for a successful hospital HIV testing program (16). All six steps may be led or facilitated by general internists.
Compounding comorbidities in HIV-positive patients
Age-related comorbidities can be exaggerated in HIV-positive patients on and off ART. Although many factors come into play, it is recognized that compared to younger patients, older patients with HIV have weaker immune systems (9) and are more likely to progress to AIDS if not on ART (17). Persistent inflammation from HIV itself, even in patients on ART, is believed to contribute to increased morbidity, potentially exacerbating age-related illnesses (18). Specific examples of such comorbidities are cardiovascular disease, and acute and chronic kidney disease. Polypharmacy and falls are also common in older patients.
Chest pain is one of the most common presentations hospitalists and inpatient providers encounter. Patients with HIV have a 50% increased risk of CAD (19, 20) and high risk of sudden cardiac death (21). Even individuals on ART, with undetectable viral loads, have a heightened risk for CAD compared to those without HIV (19). Yet, research has shown that less than a quarter of patients with HIV received aspirin when clinically indicated for prevention of CAD (21, 22). Additionally, interventions recommended after myocardial infarction were carried out less often in patients with HIV (23). Inpatient general internists aware of this disparity can intervene by initiating indicated treatment and preventative measures.
In considering cardiovascular risk factors, one recent study showed that patients with HIV are more likely to smoke and less likely to quit when compared to the general population (24). Hospitalists can intervene by carrying out smoking cessation counseling and providing prescription nicotine replacement (15). Obesity in HIV-positive patients is also increasing in frequency in the era of ART (25), and studies show that hospitalized obese patients welcome inpatient providers to initiate weight loss counselling and teach interventions that can continue after discharge (26). According to the HIV and Aging Consensus Project from 2012, providers should counsel patients at every visit to stop smoking and encourage patients on ART to avoid excess weight gain (27). Thus, hospital providers can play a crucial role in initiating behavioral modification to help reduce cardiovascular risks in inpatient settings.
Hospital medicine providers should also be aware that acute and chronic kidney diseases are more common in older patients (28, 29) and that both are independently associated with HIV infection (30, 31). For the general population, rates of hospitalizations due to acute renal failure (ARF) increased 346% between 1997 and 2011 (32). The combination of older age and HIV are both associated with renal failure (33, 34). Hospitalized HIV-positive patients are three times more likely to suffer ARF than those without HIV (31). About 50% of ARF cases are iatrogenic and can result from radiocontrast, hypoperfusion (in the setting of hypotension or heart failure exacerbations), and medications, such as ACE inhibitors and non-steroidal anti-inflammatory drugs (35). Inpatient general internists are in key positions to interpret laboratory results (i.e., basic metabolic panels and urinalyses), understand treatment options (i.e., discontinue nephrotoxic medication), and consult nephrologists when indicated (36). Preemptive monitoring for decreases in renal function is important, especially for patients on multiple medications, some of which may require dose adjustment. Rises in serum creatinine, for instance, necessitate dose adjustment of the commonly used nucleoside analogue tenofovir to prevent further renal injury.
Polypharmacy is common in older adults, and medication regimens can change substantially during hospitalizations (37). Medication errors of ART are common early during hospitalizations and can potentially lead to treatment failure and viral resistance (38). Furthermore, older patients on ART are at an increased risk for adverse medication interactions (39, 40). Holtzman et al. found that those older than age 50 compared to those younger than 50 were more likely to be prescribed an antiviral and non-antiviral combination that was contraindicated (39). Since medication errors may occur before and during hospitalizations, hospitalists are in excellent position to intercept these mistakes. Ongoing monitoring of medication added or removed from treatment regimens is essential for averting adverse outcomes. Furthermore, optimal medication reconciliation upon discharge is essential, as medication errors in transitions of care are frequently implicated in readmissions (41).
Fall-related injuries in older adults lead to hospitalizations five times more than any other cause of injury in this population (42). In 2013, direct medical costs from falls were about 34 billion dollars, with fractures the most common and costly consequence (43). Patients with HIV have lower bone mineral densities compared to the general population and are at a greater risk for developing fractures (44). Both HIV and ART directly accelerate osteoporosis, and fracture risk increases over age 50 (44). However, inpatient management of osteoporosis and fractures is often suboptimal. In one study, rates of in-hospital osteoporosis diagnoses in patients that presented with hip fracture were low (45). Only 2% of these patients were started on calcium, vitamin D, or bisphosphonates during their hospitalization (45). Managing inpatient general internists can also include screening for vitamin D deficiency and starting or optimizing medical care to reduce future fracture risks (27).
Conclusions
As the HIV-infected population ages, inpatient general internal medicine physicians are challenged to recognize and appropriately manage older HIV-infected patients in acute settings. A diagnosis of HIV may be missed when symptoms and signs mimic common conditions associated with aging. Obtaining a thorough social history, including information about sexual practices and other risk factors, is crucial. Because history may not be reliable, routine HIV screening is recommended. This screening should include older patients.
Inpatient healthcare utilization is higher among older than younger HIV-infected individuals. Factors responsible for longer hospitalizations and more frequent readmissions appear to be the increased severity of comorbidities, such as cardiac and renal disease, and the high rates of polypharmacy.
With 5,686 hospitals in the United States, the 8,575 HIV cases diagnosed in those older than age 50 in the year 2013 seem relatively small. Hence, it may be tempting to diminish the importance of this issue. However, increased coverage of our population by the Affordable Care Act is expected to increase the number of individuals seeking healthcare. Also, of particular importance, recently released results from the large, randomized Strategic Timing of Antiretroviral Therapy trials demonstrated benefit from treatment of HIV for those with high CD4 counts (46). These findings strengthen recommendations by the Department of Human Health Services to treat everyone diagnosed with HIV (47). Because treatment can lead to prevention of spread of the disease, diagnosing and treating HIV infection is important for the individual patient and society.
Conflict of interest and funding
Ché Matthew Harris received grant funding from the Gilead Bayview Project.
References
- 1.Samji H, Cescon A, Hogg RS, Modur SP, Althoff KN, Buchacz K, et al. Closing the gap: Increases in life expectancy among treated HIV-positive individuals in the United States and Canada. PLoS One. 2013;8(12):e81355. doi: 10.1371/journal.pone.0081355. doi: http://dx.doi.org/10.1371/journal.pone.0081355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Available from: http://www.cdc.gov/hiv/risk/age/olderamericans/ [cited 14 September 2015].
- 3.National Institute on Aging. Available from: http://www.nia.nih.gov/newsroom/features/aging-hiv-responding-emerging-challenge [cited 14 September 2015].
- 4.Diverse Elders Coalition. Issue brief-eight policy recommendations for improving the health and wellness of older adults with HIV. Available from: http://napca.org/wp-content/uploads/2014/07/DEC-HIV-and-Aging-Policy-Report_web.pdf [cited 14 September 2015].
- 5.National Institute on Aging. Available from: http://www.nia.nih.gov/health/publication/hiv-aids-and-older-people [cited 14 September 2015].
- 6.AIDS.gov. Available from: https://www.aids.gov/hiv-aids-basics/staying-healthy-with-hiv-aids/taking-care-of-yourself/aging-with-hiv-aids/ [ cited 14 September 2015].
- 7.Yehia BR, Fleishman JA, Hicks PL, Ridore M, Moore RD, Gebo KA, et al. Inpatient health services utilization among HIV-infected adult patients in care 2002–2007. J Acquir Immune Defic Syndr. 2010;53(3):397–404. doi: 10.1097/QAI.0b013e3181bcdc16. doi: http://dx.doi.org/10.1097/QAI.0b013e3181bcdc16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.The Aging of HIV. Available from: http://www.naswdc.org/practice/hiv_aids/AgingOfHIVFactSheet.pdf [cited 14 September 2015].
- 9.Gras L, Kesselring AM, Griffin JT, van Sighem AI, Fraser C, Ghani AC, et al. CD4 cell counts of 800 cells/mm3 or greater after 7 years of highly active antiretroviral therapy are feasible in most patients starting with 350 cells/mm3 or greater. J Acquir Immune Defic Syndr. 2007;45:183–9. doi: 10.1097/QAI.0b013e31804d685b. [DOI] [PubMed] [Google Scholar]
- 10.Bachhuber MA, Southern WN. Hospitalization rates of people living with HIV in the United States, 2009. Public Health Rep. 2014;129:178–86. doi: 10.1177/003335491412900212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Fleishman JA, Yehia BR, Moore RD, Gebo KA. The economic burden of late entry into medical care for patients with HIV infection. Med Care. 2010;48:1071–9. doi: 10.1097/MLR.0b013e3181f81c4a. doi: http://dx.doi.org/10.1097/MLR.0b013e3181f81c4a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Links N. HIV and the elderly. Fam Soc. 1994;75(6):362–72. [Google Scholar]
- 13.Centers for Disease Control and Prevention. Available from: http://www.cdc.gov/hiv/testing/clinical/ [cited 14 September 2015].
- 14.Centers for Disease Control and Prevention. Available from: http://www.cdc.gov/mmwr/preview/mmwrhtml/rr5514a1.htm [cited 14 September 2015].
- 15.Kisuule F, Necochea A, Howe EE, Wright S. Utilizing audit and feedback to improve hospitalists’ performance in tobacco dependence counseling. Nicotine Tob Res. 2010;12:797–800. doi: 10.1093/ntr/ntq093. doi: http://dx.doi.org/10.1093/ntr/ntq093. [DOI] [PubMed] [Google Scholar]
- 16.Mignano JL, Miner L, Cafeo C, Spencer DE, Gulati M, Brown T, et al. Routinization of HIV testing in an inpatient setting: a systematic process for organizational change. J Healthc Qual. 2015 doi: 10.1097/01.JHQ.0000462676.94393.ee. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 17.Phillips A, Pezzotti P, CASCADE Collaboration Short-term risk of AIDS according to current CD4 cell count and viral load in antiretroviral drug-naive individuals and those treated in the monotherapy era. AIDS. 2004;18(1):51–8. doi: 10.1097/00002030-200401020-00006. [DOI] [PubMed] [Google Scholar]
- 18.Lederman MM, Funderburg NT, Sekaly RP, Klatt NR, Hunt PW. Residual immune dysregulation syndrome in treated HIV infection. Adv Immunol. 2013;119:51–83. doi: 10.1016/B978-0-12-407707-2.00002-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Freiberg MS, Chang CC, Kuller LH, Skanderson M, Lowy E, Kraemer KL, et al. HIV infection and the risk of acute myocardial infarction. JAMA Intern Med. 2013;173(8):614–22. doi: 10.1001/jamainternmed.2013.3728. doi: http://dx.doi.org/10.1001/jamainternmed.2013.3728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tseng ZH, Secemsky EA, Dowdy D, Vittinghoff E, Moyers B, Wong JK, et al. Sudden cardiac death in patients with human immunodeficiency virus infection. J Am Coll Cardiol. 2012;59(21):1891–6. doi: 10.1016/j.jacc.2012.02.024. doi: http://dx.doi.org/10.1016/j.jacc.2012.02.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Burkholder GA, Tamhane AR, Salinas JL, Mugavero MJ, Raper JL, Westfall AO, et al. Underutilization of aspirin for primary prevention of cardiovascular disease among HIV-infected patients. Clin Infect Dis. 2012;55(11):1550–7. doi: 10.1093/cid/cis752. doi: http://dx.doi.org/10.1093/cid/cis752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Suchindran S, Regan S, Meigs JB, Grinspoon SK, Triant VA. Aspirin use for primary and secondary prevention in human immunodeficiency virus (HIV)-infected and HIV-uninfected patients. Open Forum Infect Dis. 2014;1(3) doi: 10.1093/ofid/ofu076. ofu076. doi: http://dx.doi.org/10.1093/ofid/ofu076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pearce D, Ani C, Espinosa-Silva Y, Clark R, Fatima K, Rahman M, et al. Comparison of in-hospital mortality from acute myocardial infarction in HIV sero-positive versus sero-negative individuals. Am J Cardiol. 2012;110(8):1078–84. doi: 10.1016/j.amjcard.2012.05.045. doi: http://dx.doi.org/10.1016/j.amjcard.2012.05.045. [DOI] [PubMed] [Google Scholar]
- 24.Mdodo R, Frazier EL, Dube SR, Mattson CL, Sutton MY, Brooks JT, et al. Cigarette smoking prevalence among adults with HIV compared with the general adult population in the United States: Cross-sectional surveys. Ann Intern Med. 2015;162(5):335–44. doi: 10.7326/M14-0954. doi: http://dx.doi.org/10.7326/M14-0954. [DOI] [PubMed] [Google Scholar]
- 25.Crum-Cianflone N, Tejidor R, Medina S, Barahona I, Ganesan A. Obesity among patients with HIV: The latest epidemic. AIDS Patient Care STDS. 2008;22(12):925–30. doi: 10.1089/apc.2008.0082. doi: http://dx.doi.org/10.1089/apc.2008.0082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Harris CM, Rios R, Landis R, Khaliq W, Wright S. Receptivity to weight management interventions among hospitalized obese patients: An untapped opportunity. South Med J. 2013;106(6):337–42. doi: 10.1097/SMJ.0b013e31829680ff. doi: http://dx.doi.org/10.1097/SMJ.0b013e31829680ff. [DOI] [PubMed] [Google Scholar]
- 27.Work Group for HIV and Aging Consensus Project. Summary report from the Human Immunodeficiency Virus and Aging Consensus Project: treatment strategies for clinicians managing older individuals with the human immunodeficiency virus. J Am Geriatr Soc. 2012;60(5):974–9. doi: 10.1111/j.1532-5415.2012.03948.x. doi: http://dx.doi.org/10.1111/j.1532-5415.2012.03948.x. Epub 2012 May 9. [DOI] [PubMed] [Google Scholar]
- 28.Grams ME, Juraschek SP, Selvin E, Foster MC, Inker LA, Eckfeldt JH, et al. Trends in the prevalence of reduced GFR in the United States: A comparison of creatinine- and cystatin C-based estimates. Am J Kidney Dis. 2013;62(2):253–60. doi: 10.1053/j.ajkd.2013.03.013. doi: http://dx.doi.org/10.1053/j.ajkd.2013.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ali T, Khan I, Simpson W, Prescott G, Townend J, Smith W, et al. Incidence and outcomes in acute kidney injury: A comprehensive population-based study. J Am Soc Nephrol. 2007;18:1292–8. doi: 10.1681/ASN.2006070756. [DOI] [PubMed] [Google Scholar]
- 30.Choi AI, Rodriguez RA, Bacchetti P, Bertenthal D, Volberding PA, O'Hare AM. Racial differences in end-stage renal disease rates in HIV infection versus diabetes. J Am Soc Nephrol. 2007;18:2968–74. doi: 10.1681/ASN.2007040402. [DOI] [PubMed] [Google Scholar]
- 31.Wyatt CM, Arons RR, Klotman PE, Klotman ME. Acute renal failure in hospitalized patients with HIV: Risk factors and impact on in-hospital mortality. AIDS. 2006;20:561–5. doi: 10.1097/01.aids.0000210610.52836.07. [DOI] [PubMed] [Google Scholar]
- 32.Pfuntner A, Wier LM. Most frequent conditions in U.S. hospitals, 2011. Statistical Brief #162. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. Available from: http://www.hcup-us.ahrq.gov/reports/statbriefs/sb162.pdf [cited 13 September 2015]
- 33.Edelman EJ, Gordon KS, Glover J, McNicholl IR, Fiellin DA, Justice AC. The next therapeutic challenge in HIV: Polypharmacy. Drugs Aging. 2013;30(8):613–28. doi: 10.1007/s40266-013-0093-9. doi: http://dx.doi.org/10.1007/s40266-013-0093-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zhan C, Sangl J, Bierman AS, Miller MR, Friedman B, Wickizer SW, et al. Potentially inappropriate medication use in the community-dwelling elderly: Findings from the 1996 Medical Expenditure Panel Survey. JAMA. 2001;286(22):2823–9. doi: 10.1001/jama.286.22.2823. [DOI] [PubMed] [Google Scholar]
- 35.Star RA. Treatment of acute renal failure. Kidney Int. 1998;54(6):1817–31. doi: 10.1046/j.1523-1755.1998.00210.x. [DOI] [PubMed] [Google Scholar]
- 36.Finn KM. Hospital-acquired acute renal failure-what hospitalists need to know. Case Study and Commentary. J Clin Outcomes Manage. 2003;10(4):214–223. [Google Scholar]
- 37.Harris CM, Sridharan A, Landis R, Howell E, Wright S. What happens to the medication regimens of older adults during and after an acute hospitalization? J Patient Saf. 2013;9(3):150–3. doi: 10.1097/PTS.0b013e318286f87d. doi: http://dx.doi.org/10.1097/PTS.0b013e318286f87d. [DOI] [PubMed] [Google Scholar]
- 38.Yehia BR, Mehta JM, Ciuffetelli D, Moore RD, Pham PA, Metlay JP, et al. Antiretroviral medication errors remain high but are quickly corrected among hospitalized HIV-infected adults. Clin Infect Dis. 2012;55(4):593–9. doi: 10.1093/cid/cis491. doi: http://dx.doi.org/10.1093/cid/cis491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Holtzman C, Armon C, Tedaldi E, Chmiel JS, Buchacz K, Wood K, et al. Polypharmacy and risk of antiretroviral drug interactions among the aging HIV-infected population. J Gen Intern Med. 2013;28(10):1302–10. doi: 10.1007/s11606-013-2449-6. doi: http://dx.doi.org/10.1007/s11606-013-2449-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Marzolini C, Back D, Weber R, Furrer H, Cavassini M, Calmy A, et al. Ageing with HIV: Medication use and risk for potential drug-drug interactions. J Antimicrob Chemother. 2011;66(9):2107–11. doi: 10.1093/jac/dkr248. doi: http://dx.doi.org/10.1093/jac/dkr248. [DOI] [PubMed] [Google Scholar]
- 41.Lu Y, Clifford P, Bjorneby A, Thompson B, VanNorman S, Won K, et al. Quality improvement through implementation of discharge order reconciliation. Am J Health Syst Pharm. 2013;70(9):815–20. doi: 10.2146/ajhp120050. doi: http://dx.doi.org/10.2146/ajhp120050. [DOI] [PubMed] [Google Scholar]
- 42.Alexander BH, Rivara FP, Wolf ME. The cost and frequency of hospitalization for fall-related injuries in older adults. Am J Public Health. 1992;82:1020–3. doi: 10.2105/ajph.82.7.1020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Stevens JA, Corso PS, Finkelstein EA, Miller TR. The costs of fatal and nonfatal falls among older adults. Inj Prev. 2006a;12:290–5. doi: 10.1136/ip.2005.011015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Mallon PW. Aging with HIV: Osteoporosis and fractures. Curr Opin HIV AIDS. 2014;9:428–35. doi: 10.1097/COH.0000000000000080. doi: http://dx.doi.org/10.1097/COH.0000000000000080. [DOI] [PubMed] [Google Scholar]
- 45.Jennings LA, Auerbach AD, Maselli J, Pekow PS, Lindenauer PK, Lee SJ. Missed opportunities for osteoporosis treatment in patients hospitalized for hip fracture. J Am Geriatr Soc. 2010;58:650–7. doi: 10.1111/j.1532-5415.2010.02769.x. doi: http://dx.doi.org/10.1111/j.1532-5415.2010.02769.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.INSIGHT START Study Group. Initiation of antiretroviral therapy in early asymptomatic HIV infection. N Engl J Med. 2015;373(9):795–807. doi: 10.1056/NEJMoa1506816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.AIDSinfo. Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents. Available from: http://aidsinfo.nih.gov/contentfiles/lvguidelines/AA_Recommendations.pdf [cited 14 September 2015].