Abstract
Angiogenesis is an essential process for tumor growth and metastasis, and remains a promising therapeutic target process in cancer treatment for several cancer types. Bevacizumab, a monoclonal antibody that targets vascular endothelial growth factor (VEGF), was the first antiangiogenic agent approved for cancer therapy. Novel antiangiogenic agents, such as sunitinib, sorafenib, pazopanib, or vandetanib that target additional proangiogenic signaling pathways beyond VEGF, have also been approved for the treatment of various malignant diseases. While most of these agents are approved in combination with cytotoxic chemotherapy for indications including metastatic colorectal cancer, non-small-cell lung cancer, breast cancer, renal cell carcinoma (RCC), and gastric cancer, some are used as approved monotherapy for advanced RCC, hepatocellular carcinoma and medullary thyroid cancer. Major challenges to the success of antiangiogenic therapy include associated toxicity risks, limitation of efficacy through the possible development of resistance and induction or promotion of metastatic progression. Nintedanib (formally known as BIBF 1120) is a triple angiokinase inhibitor of VEGF, fibroblast growth factor, platelet-derived growth factor signaling with lesser activity against RET, Flt-3, and Src. Through this unique targeting profile nintedanib has demonstrated significant antitumor activity in several tumor types in preclinical studies. Nintedanib has also shown promising clinical efficacy in combination with docetaxel and has been approved for treating patients with locally advanced and metastatic non-small-cell lung cancer in Europe. Nintedanib has also been found to be clinically promising in terms of efficacy and safety in several other solid tumors including ovarian cancer (Phase III), RCC (Phase II), and prostate cancer (Phase II). This review article provides a comprehensive summary of the preclinical and clinical efficacy of nintedanib in the treatment of solid tumors.
Keywords: nintedanib, BIBF 1120, angiogenesis, VEGF, tyrosine kinase inhibitors
Introduction
Angiogenesis, the process of new blood vessel development from existing vasculature, is a hallmark of cancer progression and metastasis that has long been considered an attractive therapeutic target.1 Tumor angiogenesis is a complex process that represents a highly regulated yet disturbed balance between proangiogenic and antiangiogenic mechanisms.2 Among several proangiogenic signaling molecules, vascular endothelial growth factor (VEGF) is considered to be one of the most important factors involved in tumor angiogenesis.3 VEGF is frequently highly expressed in human solid cancers and plays a fundamental role in tumor-mediated blood vessel growth by mediating vasculogenesis, angiogenic remodeling, angiogenic sprouting, and vascular permeability.3–5 Thus, initial antiangiogenic therapy attempts have largely focused on inhibiting VEGF signaling. Bevacizumab, a monoclonal antibody that blocks angiogenesis by binding VEGF-A (a ligand for VEGFR1 and VEGFR2), was the first antiangiogenic agent approved in 2004 that showed clinical efficacy in combination with chemotherapy in some solid tumors including metastatic colorectal cancer (CRC),6 non-small-cell lung cancer (NSCLC),7 breast cancer,8 and renal cell carcinoma (RCC).9 Since then, several antiangiogenic agents, such as sunitinib,10 sorafenib,11 pazopanib,12 vandetanib,13 axitinib,14 regorafenib,15 aflibercept,16 cabozantinib,17 and ramucirumab18 that target VEGF signaling and/or some additional proangiogenic signaling activity have been approved for the treatment of various malignant diseases. These anti-angiogenic agents, either as monotherapy or in combination with chemotherapy, generally have only provided limited clinical benefits in some tumor types. Furthermore, in certain advanced metastatic cancers, VEGF inhibition alone was insufficient to prevent progression, induced resistance and in some cases may have contributed to increased invasion and metastasis.19,20 One of the main reasons for the limited and transient response of the anti-VEGF therapies is that tumor angiogenesis is regulated by multiple pathways that are able to compensate for each other when single pathways are inhibited. The fibroblast growth factor (FGF) and its receptors (FGFR1/2/3),21 platelet-derived growth factor (PDGF), and its receptors (PDGFRα and PDGFRβ),22 epidermal growth factor and its receptor,23 angiopoietin-2,24 placenta-derived growth factor,25 and neuropilin26 are key components within the main signaling pathways that provide potential escape mechanisms from anti-VEGF therapy leading to resistance development and facilitate resumption of tumor growth.27
The FGF/FGFR signaling axis plays an important role in tissue homeostasis, tissue repair, angiogenesis, and inflammation. Deregulation of FGF/FGFR signaling through genetic modification or over-expression of its ligands/receptors has been observed to promote cell proliferation, survival, and tumor angiogenesis in numerous tumor settings including pancreatic cancer, prostate cancer, and some squamous cell carcinomas.28,29 Several preclinical studies demonstrated that inhibition of FGF/FGFR signaling has antiproliferative, proapoptotic, and antiangiogenic effects, supporting the validity of this signaling axis as a potential therapeutic target. PDGF is another important growth factor that can be crucial for tumor growth and progression. PDGF itself is a potent mitogen in both normal and tumor cells,30 but it also has significant angiogenic effects on endothelial cells. PDGF/PDGFR signaling has been shown to promote cell division,31,32 cell migration,33 and angiogenesis.34 In addition, recruitment of pericytes such as vascular smooth muscle cells by PDGF is essential for maintenance of tumor angiogenesis.35 The PDGF/PDGFR signaling has been overactive in several malignancies such as brain tumor, sarcomas, prostate cancer, liver cancer, NSCLC, breast cancer, and CRC36,37 and therapeutic targeting of this pathway reduced tumor growth in many tumor types.37–39
As multiple proangiogenic factors contribute to tumor angiogenesis, and the fact that inhibition of one angiogenic signaling pathway induces compensatory mechanisms leading to the development of resistance,40–42 more recent therapeutic strategies have focused on developing multi-targeted tyrosine kinase receptors (TKIs) that have the ability to block multiple signaling pathways simultaneously, but at the same time maintain some selectivity profile of kinases in terms of safety and tolerability. This review summarizes the antitumor profile of nintedanib, a triple angiokinase inhibitor, which targets proangiogenic signaling of VEGFR, FGFR, and PDGFR.
Nintedanib: advantages and mechanism of action
The first commercially available antiangiogenic drug was bevacizumab, a monoclonal antibody against VEGF-A.43 Bevacizumab is currently approved in combination with standard chemotherapy for the treatment of several cancers including metastatic CRC,6 NSCLC,7 and RCC.6,7,19 While bevacizumab demonstrates some promising antitumor activity, its clinical use may also be limited by its side-effect profile that includes hypertension, proteinuria, bleeding, thrombotic events, and hemorrhage.44,45 Efforts beyond bevacizumab have focused on a second class of antiangiogenic agents, namely small molecules that are orally available and have the ability to target multiple TKIs. Most of these broad-spectrum TKIs such as sunitinib, sorafenib, pazopanib, vandetanib have complex efficacy data, but in many cases the use of these drugs is associated with a significant increase in the incidence and risk of side effects.46–48 Most of these TKIs that affect multiple kinases have lower specificity toward some of their therapeutic targets, particularly at the FGF/FGFR axis, requiring higher doses for efficacy.49 Therefore, these TKIs have increased risk for on-target toxicities (such as hypertension, skin toxicity, and diarrhea) and presumed off-target toxicities (such as cardiac impairment).49,50
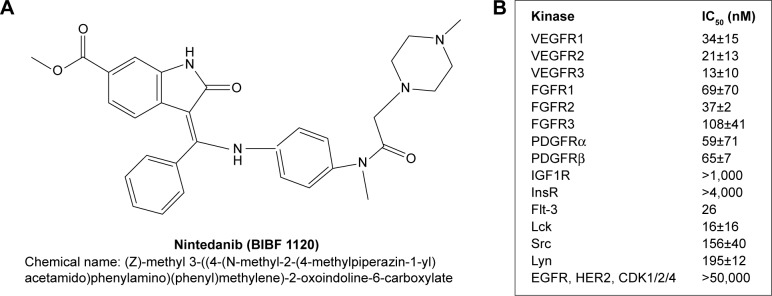
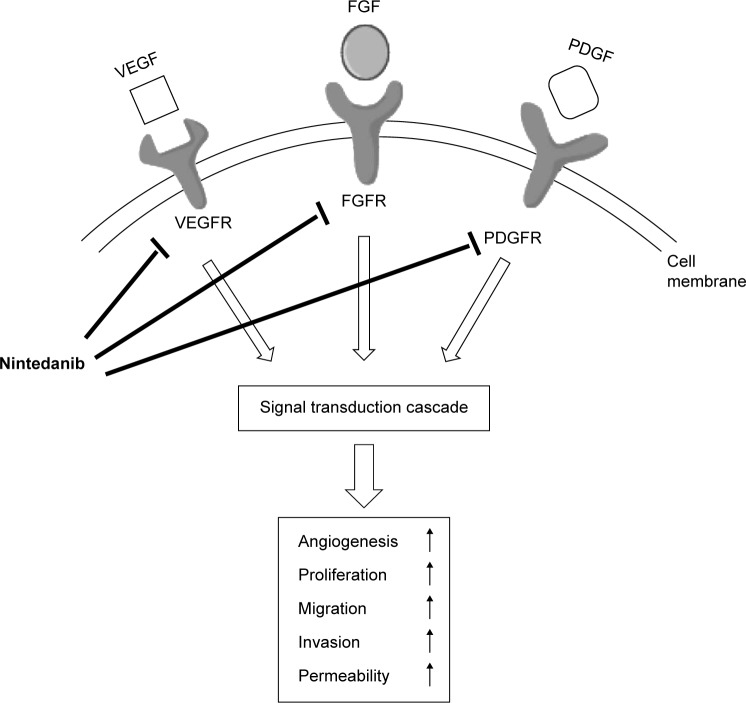
Nintedanib is a next generation, oral, and potent triple angiokinase inhibitor that inhibits the proangiogenic pathways mediated by VEGFR1/2/3 (IC50 13–34 nmol/L), FGFR1/2/3 (IC50 37–108 nmol/L), and PDGFRα/β (IC50 59–65 nmol/L) to a high degree of specificity (Figure 1). Nintedanib competitively binds to the ATP binding-pocket of these receptors, resulting in interference with receptor dimerization and blocking intracellular signaling critical for the proliferation and survival of angiogenesis-related endothelial cells, pericytes, and vascular smooth muscle cells (Figure 2). Nintedanib also inhibits some non-receptor kinases such as Fms-like tyrosine protein kinase (Flt-3, IC50 26 nmol/L), proto-oncogene ret (Ret, IC50 35 nmol/L), lymphocyte-specific tyrosine kinase (Lck, IC50 16 nmol/L), tyrosine-protein kinase lyn (Lyn IC50 195 nmol/L), and proto-oncogene tyrosine protein kinase src (Src, IC50 156 nmol/L)51,52 (Figure 1). In addition, nintedanib has recently been approved for the treatment of idiopathic pulmonary fibrosis based on results from the replicate Phase III trials involving 1,066 patients from 24 countries.53 Nintedanib is thus the first targeted treatment for idiopathic pulmonary fibrosis, indicating the therapeutic potential of TKIs in non-malignant diseases.
Figure 1.
Summary of nintedanib.
Notes: (A) Molecular structure of nintedanib. (B) In vitro kinase inhibition profile of nintedanib (IC50). Data presented as mean ± standard error of at least three determinations.
Abbreviations: VEGFR, vascular endothelial growth factor receptor; FGFR, fibroblast growth factor receptor; PDGFR, platelet-derived growth factor receptor; IGF1R, insulin-like growth factor 1 receptor; InsR, insulin receptor; Flt-3, fms-like tyrosine protein kinase 3; Lck, lymphocyte-specific tyrosine kinase; Src, proto-oncogene tyrosine protein kinase src; Lyn, tyrosine-protein kinase lyn; EGFR, epidermal growth factor receptor; HER2, human epidermal growth factor receptor 2; CDK, cyclin-dependent kinase.
Figure 2.
Triple angiokinase inhibition mechanism of nintedanib targeting tumor angiogenesis.
Abbreviations: VEGF, vascular endothelial growth factor; FGF, fibroblast growth factor; PDGF, platelet-derived growth factor.
A major challenge in the success of VEGF signaling blocking antiangiogenic therapy is the development of resistance in the primary tumor, probably due to induction of tumor escape mechanisms through upregulated FGFR and PDGFR signaling.54–56 This mechanism of the development of antiangiogenic drug resistance provides a potential rationale for efficacy of nintedanib, which can prevent tumor growth and metastasis via its triple inhibition of VEGFR, FGFR and PDGFR, and also provide a therapeutic alternative for patients with intrinsic and acquired resistance to single or dual target antiangiogenic drugs.
Nintedanib: preclinical studies to date
In vitro studies demonstrated that nintedanib treatment inhibited the proliferation of VEGF-stimulated human umbilical vein endothelial cells and human skin microvascular endothelial cells. Nintedanib also inhibited the proliferation of PDGF-stimulated smooth muscle cells and pericytes.52 Although Kutluk Cenik et al57 showed that nintedanib has no antiproliferative activity on selected lung and pancreatic cancer cell lines, recent reports suggest that nintedanib effects are not generally limited to stromal cells as it also differentially inhibited the proliferation of hepatocellular carcinoma (HCC) cells58 and pancreatic ductal adenocarcinoma (PDAC) cells.59 Tai et al58 demonstrated that nintedanib treatment caused a significant antiproliferative effect in a panel of four HCC cell lines (PLC5, Hep3B, SK-Hep1, and HuH7) and one hepatoblastoma cell line (Hepg2). Awasthi et al59 demonstrated that nintedanib not only inhibited the proliferation of human umbilical vein endothelial cells, fibroblast WI-38 cells and pancreatic cancer stromal cells, but it also inhibited the proliferation of human PDAC cells (AsPC-1, BxPC-3, MIA PaCa-2, and Panc-1) and murine PDAC cells PanO2.
In vivo, nintedanib demonstrated potent antitumor effects in all human tumor xenografts reported to date, including NSCLC, RCC, CRC, ovarian cancer, prostate cancer, and PDAC.52,57,59 More importantly, nintedanib treatment augmented the antitumor response of standard cytotoxic agents. In NSCLC xenografts (H460 cells), nintedanib treatment caused synergistic antitumor effects in combination with cytotoxic agents docetaxel or pemetrexed.60 Kutluk Cenik et al57 demonstrated significant antitumor activity of nintedanib monotherapy and in combination with standard cytotoxic chemotherapy in several xenograft models of lung and pancreatic cancer.57 Recently, Awasthi et al59 demonstrated that nintedanib significantly enhanced gemcitabine response in pancreatic cancer: net local tumor growth compared to controls (100%) was 60.8%±10.5% in the gemcitabine group, −2.1%±9.9% after nintedanib monotherapy and −12.4%±16% after gemcitabine plus nintedanib combination therapy. In addition, this study demonstrated that compared with controls, the increase in median animal survival was 56% with gemcitabine (P=0.036), 94% for nintedanib (P=0.004) and 138% after gemcitabine + nintedanib (P=0.001).59 In human tumor xenografts, intratumoral antitumor mechanism of nintedanib involves reduced microvessel density, pericyte coverage, vessel permeability, tumor perfusion, and induced hypoxia, as well as inhibition of phosphatidylinositol 3-kinase (PI3K)-AKT and mitogen-activated protein kinase (MAPK) signaling pathways.52,57,59
Nintedanib: clinical studies to date
The clinical pharmacokinetic profile studies of nintedanib demonstrated that it is rapidly absorbed as its maximum plasma concentrations occur within 1–3 hours after oral administration.61,62 The terminal half-life of nintedanib was observed to be ~13–19 hours.61,62 The first Phase I dose-escalation study with single agent nintedanib therapy was reported in 61 patients with different advanced solid tumors.62 Twenty-five patients received nintedanib 50–450 mg once daily (od) and 36 patients received nintedanib 150–300 mg twice daily (bid) in 4-week cycles with a week off. The most common drug-related adverse events (AEs) were mild to moderate; grade 3 or more AEs for nintedanib od vs bid occurring in >5% patients were reversible hepatic enzyme elevation (12% grade 3 and 4% grade 4 vs 0% grade 3 and 2.8% grade 4), increase in aspartate aminotransferase (AST; grade 3, 8% vs 2.8%), increase in alanine aminotransferase (ALT; grade 3, 0% vs 5.6%), increase in γ-glutamyl transpeptidase (grade 3, 4% vs 5.6%), decrease in CD-4 lymphocyte (grade 3, 16% vs 5.6%), hypertension (grade 3, 4% vs 0%), diarrhea (grade 3, 0% vs 2.8%), nausea (grade 3, 0% vs 5.6%), and vomiting (grade 3, 0% vs 2.8%). The maximum tolerable dose (MTD) of nintedanib was defined as 250 mg for both od and bid dosing.62 In another Phase I dose-escalation study, 21 Japanese patients with advanced refractory solid tumors were treated with bid nintedanib doses of 150 mg (n=3), 200 mg (n=12), or 250 mg (n=6).63 This study reported that the dose-limiting grade 3 or 4 toxicity elevation of liver enzymes occurred in 3 of 12 patients at 200 mg bid and 3 of 6 patients at 250 mg bid dose. Stable disease (SD) was reported in 76.2% of patients (n=16). The MTD of nintedanib in this study was determined to be 200 mg bid.
Nintedanib in NSCLC
In NSCLC patients, two Phase I dose-escalation studies have been conducted investigating nintedanib in combination with a standard chemotherapy regimen. The first study investigated the MTD of continuous nintedanib oral treatment in combination with standard-dose pemetrexed (500 mg/m2) in patients who had been previously treated with one platinum-based chemotherapy regimen.64 In this study, one patient achieved a complete response after 44 days for more than 3 years; otherwise, the best overall response was SD in 50% patients (n=13). The second trial investigated the safety, tolerability, and MTD of nintedanib in combination with carboplatin and paclitaxel in patients with advanced NSCLC who were previously untreated.65 In these two Phase I studies, the recommended dose of nintedanib was determined as 200 mg bid when used in combination with the mentioned standard chemotherapy regimens of NSCLC. The most frequent AEs in these studies were comparable to the nintedanib monotherapy trials.
A Phase II double-blind trial evaluated the efficacy of nintedanib monotherapy (150 mg bid, n=36 or 250 mg bid, n=37) in patients with relapsed, advanced NSCLC (any histology) with an Eastern Cooperative Oncology Group performance status 0–2. This study reported a median progression free survival (PFS) of 6.9 weeks, the median overall survival (OS) was 21.9 weeks, and SD was observed in 46% of the patients (Table 1). In 56 patients with Eastern Cooperative Oncology Group performance status 0–1, median PFS was 11.6 weeks with a median OS of 37.7 weeks. Most commonly reported drug-related AEs included nausea, diarrhea, vomiting, anorexia, and abdominal pain.66
Table 1.
Summary of key efficacy and safety results from Phase II and III studies with nintedanib in patients with NSCLC
| Study | Setting | Regimen | Median PFS | Median OS | Most common AEs |
|---|---|---|---|---|---|
| Phase II66 | Advanced NSCLC, previously treated | Nintedanib 150 mg (bid, n=36) or 250 mg (bid, n=37) | 6.9 weeks | 21.9 weeks | Nausea, diarrhea, vomiting, anorexia, abdominal pain |
| Phase III67 LUME-lung 1 | Advanced NSCLC, previously treated | Nintedanib (200 mg, bid, 2–21 days) + docetaxel (75 mg/m2, day 1), n=565 or placebo + docetaxel (75 mg/m2, day 1), n=569 | 3.4 months vs 2.7 months, P=0.0019 (nintedanib vs placebo) | 12.6 months vs 10.3 months, P=0.0359 (nintedanib vs placebo arm) | The more common AEs in the nintedanib vs placebo: diarrhea (42.3% vs 21.8%), increase in ALT (28.5% vs 8.4%), increase in AST (22.5% vs 6.6%), nausea (24.2% vs 18%), vomiting (16.9% vs 9.3%) |
| Phase III68 LUME-lung 2 | Advanced NSCLC or nonsquamous histology, after relapse or failure of first-line chemotherapy | Nintedanib (200 mg, bid, 2–21 days) + pemetrexed (500 mg/m2, day 1), n=353 or placebo + pemetrexed (500 mg/m2, day 1), n=360 | 4.4 months vs 3.6 months, P=0.0435 (nintedanib vs placebo) | 12.2 months vs 12.7 months, P=0.7921 (nintedanib arm vs placebo arm) | Nintedanib vs placebo: grade 3/4 AEs (increase in liver enzymes and gastrointestinal events; 58.5% vs 42.3%), serious AEs (30% vs 32.8%), grade 5 AEs (9.8% vs 12%) |
Abbreviations: AEs, adverse events; bid, twice daily; NSCLC, non-small cell lung cancer; OS, overall survival; PFS, progression free survival.
A Phase III, double-blind, randomized trial of nintedanib (200 mg, bid, n=565) or placebo (n=569) on days 2–21, in combination with docetaxel (75 mg/m2 on day 1) in patients with previously treated NSCLC (LUME-Lung 1 trial), reported that median PFS was significantly improved in the docetaxel plus nintedanib group compared with the docetaxel plus placebo group (3.4 months vs 2.7 months, hazard ratio (HR) 0.79, P=0.0019). The median OS was also significantly improved in the docetaxel plus nintedanib group compared with docetaxel alone group (12.6 months vs 10.3 months; HR 0.83, P=0.0359) for all patients with adenocarcinoma histology. In the total study population, median OS in the docetaxel plus nintedanib group and docetaxel alone group was 10.1 and 9.1 months (HR 0.94, P=0.2720), respectively. Nintedanib plus docetaxel had a manageable safety profile as AEs more common in the combination group than in the docetaxel alone group included diarrhea (42.3% vs 21.8%), increases in ALT (28.5% vs 8.4%), increase in AST (22.5% vs 6.6%), nausea (24.2% vs 18%), and vomiting (16.9% vs 9.3%) (Table 1). Most of these AEs were manageable by symptom management and/or dose reduction.67 Based on the positive results of this study of 1,300 patients in 27 countries, the European Union granted approval for nintedanib in combination with docetaxel for use in patients with locally advanced, metastatic, or locally recurrent NSCLC with adenocarcinoma histology and progression after first-line chemotherapy. Another Phase III study (LUME-Lung 2) trial investigated the efficacy and safety of nintedanib (200 mg, bid on 2–21 days) in combination with standard pem-etrexed (500 mg/m2 on day 1) compared with pemetrexed alone (500 mg/m2 on day 1) in patients with advanced or recurrent nonsquamous NSCLC after relapse or failure of first-line chemotherapy. In this study, patient enrollment was halted after 713 patients based on a pre-defined futility analysis of investigator-assessed PFS by an independent data monitoring committee. This decision was based on the likelihood that the primary endpoint of centrally assessed PFS would not be met, and was not safety related. Interestingly, a subsequent analysis of the 713 patients who were enrolled, demonstrated that the primary end-point of centrally reviewed PFS was met even though the study was stopped prematurely. This analysis showed that median PFS was significantly improved in the pemetrexed plus nintedanib group compared with pemetrexed alone (4.4 vs 3.6 months, HR 0.83, P=0.0435). There was no difference in OS between the two treatment groups (12.2 vs 12.7 months, HR 1.03, P=0.7921) and overall response rates were also comparable (9.1% vs 8.3%). There was a higher incidence of grade 3/4 AEs (increase in liver enzymes and gastrointestinal events, overall 58.5% vs 42.3%), serious AEs were 30% vs 32.8% and grade 5 AEs were 9.8% vs 12% in the nintedanib arm vs placebo (Table 1).68 A Phase II study (a biomarker-driven study: FGFR1 amplification as predictive of efficacy) of nintedanib in advanced squamous cell lung cancer patients who have failed up to two prior chemotherapy regimens is currently ongoing (NCT01948141). Another placebo-controlled, Phase III trial of nintedanib plus docetaxel in patients with stage IIIB/IV or recurrent adenocarcinoma NSCLC after failure of first line chemotherapy is also ongoing (LUME-Columbus, NCT02231164).
Nintedanib in ovarian cancer
In a Phase II double-blind, randomized trial of 83 patients who had just completed chemotherapy for relapsed ovarian cancer with evidence of response but at high risk of further early recurrence, patients were randomized to receive either nintedanib 250 mg (n=43) or placebo (n=40), bid, continuously for 36 weeks. The PFS rates at 36 weeks were 16.3% and 5% in the nintedanib and placebo groups, respectively (HR 0.65, 95% CI: 0.42–1.02, P=0.06). Grade 3 or 4 AEs were similar between the nintedanib group and placebo (34.9% vs 27.5%, P=0.49) (Table 2). This study concluded that nintedanib is well tolerated and it is associated with a potential improvement in survival.69
Table 2.
Summary of key efficacy and safety results from Phase II and III studies with nintedanib in solid tumors other than NSCLC
| Study | Setting | Regimen | Median PFS/PFS rate | Median OS | Most common AEs |
|---|---|---|---|---|---|
| Phase II69 | Ovarian cancer, previously treated | Nintedanib 250 mg (bid, n=43) or placebo (n=40) continuous for 36 weeks | PFS rate at 36 weeks: 16.3% vs 5%, P=0.06 (nintedanib vs placebo) | NR | Nintedanib vs placebo: grade 3/4 AEs were similar (34.9% vs 27.5%, P=0.49) |
| Phase III70 LUME-ovar 1 | Advanced epithelial ovarian cancer, previously untreated | Standard first-line chemotherapy (carboplatin and paclitaxel) followed by nintedanib (200 mg, bid) up to 120 weeks, or placebo plus chemotherapy | PFS: 17.3 months vs 16.6 months, P=0.0239 (nintedanib vs placebo arm) | NR | Nintedanib vs placebo: major AEs: gastrointestinal symptoms, hematologic symptoms |
| Phase II71 | Advanced clear cell renal cell carcinoma (RCC), previously untreated | Nintedanib (200 mg, bid, 4 week cycle; n=64) or sunitinib (50 mg od, 4 weeks on 2 weeks off cycle; n=32) | PFS: 8.44 months vs 8.38 months, P=0.56 (nintedanib vs sunitinib) | 20.37 months vs 21.22 months, P=0.63 (nintedanib vs sunitinib) | Nintedanib and sunitinib: diarrhea (61% vs 50%), nausea (38% vs 34%), fatigue (both 25%), vomiting (16% vs 22%), dermatologic events (8% vs 47%), hypertension (3.1% vs 15.6%), hand–foot syndrome (0% vs 31.3%), stomatitis (0% vs 31.3%) |
| Phase II72 | Advanced and unresectable hepatocellular carcinoma (HCC), pooled analysis of two randomized trials | Nintedanib (200 mg, bid; n=125) or sorafenib (400 mg, bid; n=63) continuously in 28-day cycle | PFS: 3.7 months vs 3.9 months (nintedanib vs sorafenib groups) | 11.4 months vs 11 months (nintedanib vs sorafenib group) | Nintedanib vs sorafenib: diarrhea (10% vs 6%), fatigue (7% vs 2%), anemia (7% vs 6%), increased AST (8% vs 13%), increased ALT (6% vs 8%), thrombocytopenia (5% vs 8%), skin reaction (1% vs 6%), rate of grade ≥3 AEs (62% vs 87%), AEs leading to dose-reduction (19% vs 51%) |
| Phase II73 | Metastatic castration-resistant prostate cancer (CRPC); primary endpoint ≥20% decline in the PSA | Nintedanib 150 mg, bid or nintedanib 250 mg, bid | PFS: 73.5 days vs 76 days; decline in PSA: 0% vs 11.1% (nintedanib 150 mg vs 250 mg) | NR | Gastrointestinal disorders, asthenia, hypertension, and reversible transaminase. Serious AEs were 20% vs 24.4% in nintedanib 150 mg vs 250 mg |
| Phase II74 | Advanced castration-resistant prostate cancer (CRPC) | Nintedanib (250 mg, bid) or afatinib (40 mg, od) or alternating sequential 7-day nintedanib and afatinib (70 mg, od, Combi70, which was reduced to 40 mg od, Combi40) | PFS rate at 12 weeks: 26% nintedanib group, 0% afatinib, and Combi40 groups | NR | Diarrhea, nausea, vomiting, and lethargy |
| Phase II75 | Advanced colorectal cancer (CRC), previously treated | Repeated courses of alternating 7-day treatment periods. First with nintedanib (250 mg, bid) then afatinib (50 mg, od), n=46 | PFS: 1.9 months; stable disease: 43.5% (20 patients) | 5.5 months | Diarrhea (80.4%), asthenia (47.8%), nausea (43.5%), rash (41.3%) |
| Phase I/II76,77 | Metastatic colorectal cancer, previously untreated | Phase I: Nintedanib (200 mg or 150 mg, bid) + mFOLFOX6 q2w; n=15 Phase II: Nintedanib (200 mg, bid) + mFOLFOX6 (q2w), n=85 or bevacizumab (5 mg/kg, q2w) + mFOLFOX6 (q2w), n=41 | PFS: 10.5 months vs 15.4 months in nintedanib vs bevacizumab groups | NR | Nintedanib vs bevacizumab: diarrhea (77.6% vs 68.3%), nausea (70.6% vs 58.5%), asthenia (55.3% vs 61%), neutropenia (47.1% vs 36.6%), vomiting (45.9% vs 34.1%), decreased appetite (31.8% vs 41.5%), constipation (18.8% vs 46.3%), serious AEs: (37.6% vs 53.7%) |
Abbreviations: AE, adverse events; bid, twice daily; NSCLC, non-small-cell lung cancer; OS, overall survival; PFS, progression free survival; od, once daily; NR, not reported; q2w, once every two weeks.
In a Phase III study (LUME-Ovar 1 or AGO-OVAR 12), nintedanib 200 mg bid was added to standard first-line chemotherapy (carboplatin and paclitaxel) followed by nintedanib maintenance therapy for a maximum of 120 weeks as first-line treatment in patients with advanced epithelial ovarian cancer. This study demonstrated a significant improvement in median PFS in the nintedanib plus chemotherapy group compared with placebo/chemotherapy alone (17.3 vs 16.6 months, HR 0.84, 95% CI: 0.72–0.98, P=0.0239) (Table 2). In a subgroup analysis, a more pronounced PFS benefit was observed with nintedanib compared with the placebo arm in patients with <1 cm postsurgical residual tumor deposits (27.1 vs 20.8 months, HR 0.75, 95% CI: 0.61–0.92, P=0.005). This study is still ongoing.70 Three Phase II trials of nintedanib are currently ongoing: one with and without metronomic dose of cyclophosphamide in advanced ovarian cancer (NCT01610869), one in combination with first line chemotherapy with interval debulking surgery in patients with ovarian cancer (NCT01583322), and another in bevacizumab resistant, persistent, or recurrent epithelial ovarian cancer (NCT01669798).
Nintedanib in renal cell carcinoma
The efficacy and safety of nintedanib (200 mg, bid, given in 4 week cycle, n=64) was assessed in a Phase II study of previously untreated advanced RCC patients and compared with the standard of care agent sunitinib (50 mg od, 4 weeks on, 2 weeks off schedule, n=32) as first-line systemic therapy. No significant difference in median PFS was observed between nintedanib and sunitinib treated groups (8.44 vs 8.38 months, HR 1.16, 95% CI: 0.71–1.89, P=0.56). Also, no significant difference was observed between the two therapy groups in terms of median OS (20.37 vs 21.22 months, HR 0.92, 95% CI: 0.54–0.156, P=0.63) or 9 month PFS (43% vs 45%, P=0.85). The overall incidence of AE (any grade) was similar between nintedanib and sunitinib groups (90.6% vs 93.8%). However, grade 3 or more AEs occurred in 47% of patients after nintedanib compared with 56% after sunitinib. Most common AEs of all grades after nintedanib compared to sunitinib included diarrhea (61% vs 50%), nausea (38% vs 34%), fatigue (both 25%), and vomiting (16% vs 22%). However, dermatologic AEs (8% vs 47%) and other common AEs associated with antiangiogenic agents such as hypertension (3.1% vs 15.6%), hand–foot syndrome (0% vs 31.3%), and stomatitis (0% vs 31.3%), were less common in nintedanib treated patients compared with sunitinib therapy (Table 2).71
Nintedanib in HCC
Two Phase II studies evaluated the efficacy and safety of nintedanib (200 mg, bid) in comparison with sorafenib (400 mg, bid) continuously in 28-day cycle, in patients with unresectable, advanced HCC in Europe (NCT0100434003) and Asia (NCT00987935). Pooled analysis of these two trials (180 patients) in Caucasian and Asian patients showed similar efficacy between nintedanib and sorafenib therapy groups in terms of median time to progression (TTP; 3.7 vs 3.9 months, HR 1.31, 95% CI: 0.89–1.91), median OS (11.4 vs 11 months, HR 0.91, 95% CI: 0.65–1.29), and overall response rates (4% vs 5%). The most frequent (>5% of patients in any group) grade ≥3 AEs after nintedanib compared to sorafenib included diarrhea (10% vs 6%), fatigue (7% vs 2%), anemia (7% vs 6%), increased AST (8% vs 13%) and ALT (6% vs 8%), thrombocytopenia (5% vs 8%), and skin reaction (1% vs 6%). However, the rates of grade ≥3 AEs (62% vs 87%) and AEs leading to dose reduction (19% vs 51%) were lower in the nintedanib group compared to sorafenib (Table 2).72
Nintedanib in prostate cancer
Two doses of nintedanib (150 and 250 mg, bid) were evaluated in a randomized Phase II study in metastatic castration-resistant prostate cancer patients after progression with docetaxel.73 The primary endpoint, prostate-specific antigen (PSA) response rate (≥20% decline in PSA from baseline), was 0% in the nintedanib 150 mg group and 11.1% in the nintedanib 250 mg group (P=0.12). However, nintedanib at 250 mg showed at least 50% PSA reduction in 5.6% patients and the rate of PSA increase in this group was significantly decelerated on treatment vs before treatment (P=0.002). The median PFS was similar between the two groups (73.5 vs 76 days, P=0.3). AEs included gastrointestinal disorders, asthenia, hypertension, and reversible transaminase elevation. The incidence of serious AEs for nintedanib 150 mg vs 250 mg, were 20% vs 24.4% (Table 2).73
Another Phase II study evaluated nintedanib and afatinib, an ErbB family blocker, in advanced castration-resistant prostate cancer patients; dosing included nintedanib (250 mg, bid, n=27), afatinib (40 mg od, n=13), or alternating sequential 7-day nintedanib (250 mg, bid) and afatinib (70 mg od; Combi70), which was later termed Combi40 (n=10) because the afatinib dose was reduced to 40 mg od due to AEs. The primary end-point of the study, the progression-free rate at 12 weeks was 26% for nintedanib and 0% for the afatinib and Combi40 groups (Table 2). However, the median TTP was 31 days (95% CI: 29–84) for nintedanib monotherapy, 29 days (95% CI: 29–54) for afatinib monotherapy, and 57 days (95% CI: 29–78) for Combi40. The median PFS results were the same as for median TTP. Two patients had a ≥50% decline in PSA, one each in the nintedanib and the Combi40 groups. The most common drug-related AEs were diarrhea, nausea, vomiting, and lethargy; the majority of patients (>90%) in each group had at least one therapy-related AE. Rash was more frequent with afatinib and elevation in transaminase was more frequent with nintedanib monotherapy. The frequency of therapy-related AEs did not increase in Combi40 compared with monotherapy.74
Nintedanib in CRC
In a Phase II study an alternating regimen of nintedanib (250 mg, bid) and then afatinib (50 mg, od) was evaluated in patients with advanced pretreated CRC. In this study, the best response was SD in 20 patients (43.5%) but no objective responses were observed. Seven patients (15.2%) remained progression-free for ≥16 weeks. Median PFS was 1.9 months; median OS was 5.5 months. The most common AEs were diarrhea (80.4%), asthenia (47.8%), nausea (43.5%), and rash (41.3%) (Table 2).75 In another Phase II study, nintedanib plus mFOLFOX6 compared to bevacizumab plus mFOLFOX6 were evaluated in 126 patients with previously untreated metastatic CRC. The primary endpoint of this study was the kaplan-meier (KM) estimate of PFS at 9 months, which was 62.1% for the nintedanib regimen and 70.2% for the bevacizumab regimen; a numerical difference in PFS between treatments was −8.1% (95% CI: −27.8 to 11.5). The results for best confirmed overall response were 63.5% (95% CI: 52.4–73.7) for the nintedanib and 56.1% (95% CI: 39.7–71.5) for the bevacizumab group. SD frequency was lower in the nintedanib than in the bevacizumab group (27.1% vs 36.6%). The final analysis of this study demonstrated that the median PFS was 10.5 months in the nintedanib group (95% CI: 9.4–12.4) and 15.4 months in the bevacizumab group (95% CI: 9.6–18.9), which contrasted with a median PFS at the time of the interim analysis (nintedanib: 10.6 months, bevacizumab: 9.2 months). The most frequent AEs (>40% in either group) in the nintedanib vs bevacizumab groups were diarrhea (77.6% vs 68.3%), nausea (70.6% vs 58.5%), asthenia (55.3% vs 61%), neutropenia (47.1% vs 36.6%), vomiting (45.9% vs 34.1%), decreased appetite (31.8% vs 41.5%), and constipation (18.8% vs 46.3%). Incidences of AEs leading to discontinuation of nintedanib or bevacizumab, with or without discontinuation of mFOLFOX, were 27.1% for nintedanib and 31.7% in the bevacizumab group. The overall incidence of serious AEs was lower for the nintedanib group than for the bevacizumab group (37.6% vs 53.7%) (Table 2).76,77 A double-blind, randomized, Phase III study of nintedanib vs placebo in refractory CRC is currently ongoing (NCT02149108). Another Phase I/II study of nintedanib in combination with capecitabine in treating patients with refractory metastatic CRC is currently ongoing (NCT02393755).
Nintedanib in breast cancer
In a Phase I study, the combination of nintedanib (150 mg, bid) with a standard preoperative treatment for breast cancer (weekly 80 mg/m2 paclitaxel, followed by adriamycin plus cyclophosphamide) was evaluated in HER-2-negative breast cancer patients.78 At this dose level, the observed toxicity was not different from that reported with paclitaxel alone therapy. The dose-limiting toxicity was transaminase elevation. The dose intensity of both initial drugs, nintedanib and paclitaxel, was 99.9% and 97.4%, respectively. Despite the low number of patients (n=8), the efficacy at this dose level was very promising with a pathological complete response of 50%. Based on these trial data, a randomized Phase II study of docetaxel with or without nintedanib in patients receiving a second-line of chemotherapy for neoadjuvant HER-2-negative breast cancer patients is ongoing (NCT01658462). Another Phase II study of nintedanib monotherapy for patients with metastatic HER2-negative inflammatory breast cancer is also ongoing (NCT02389764).
Based on promising efficacy and safety results of nintedanib in the above-mentioned solid tumors, nintedanib is currently under investigation in several other solid tumors including thyroid cancer (NCT01788982), neuroendocrine tumors (NCT02399215), cervix cancer (NCT02009579), endometrial cancer (NCT01225887), esophagogastric cancer (NCT02234596), urothelial carcinoma (NCT02278978), and glioblastoma (NCT01666600).
Conclusion
Increased understanding of the complexity of tumor angiogenesis pathways indicated the importance of multitargeted antiangiogenic agents to increase tumor response and overcome or delay resistance development. By simultaneous targeting of VEGF, FGF, and PDGF signaling, nintedanib may offer a better approach for the treatment of several solid tumors. The clinical efficacy of nintedanib in combination with docetaxel in NSCLC was recognized by its approval in the European Union. Nintedanib also demonstrated rather encouraging clinical efficacy and tolerability data in patients with different solid tumors, and several additional clinical studies are currently ongoing. There is a good possibility that nintedanib will be approved for at least some of these tumor types in the near future. However, more understanding of nintedanib’s molecular mechanism of action and identifying molecular biomarkers to predict nintedanib response is highly desired to maximize clinical benefits.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Folkman J. Tumor angiogenesis: therapeutic implications. N Engl J Med. 1971;285(21):1182–1186. doi: 10.1056/NEJM197111182852108. [DOI] [PubMed] [Google Scholar]
- 2.Al-Husein B, Abdalla M, Trepte M, Deremer DL, Somanath PR. Antiangiogenic therapy for cancer: an update. Pharmacotherapy. 2012;32(12):1095–1111. doi: 10.1002/phar.1147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Moreira IS, Fernandes PA, Ramos MJ. Vascular endothelial growth factor (VEGF) inhibition – a critical review. Anticancer Agents Med Chem. 2007;7(2):223–245. doi: 10.2174/187152007780058687. [DOI] [PubMed] [Google Scholar]
- 4.Ferrara N. Vascular endothelial growth factor as a target for anticancer therapy. Oncologist. 2004;9(Suppl 1):2–10. doi: 10.1634/theoncologist.9-suppl_1-2. [DOI] [PubMed] [Google Scholar]
- 5.Shojaei F, Ferrara N. Antiangiogenic therapy for cancer: an update. Cancer J. 2007;13(6):345–348. doi: 10.1097/PPO.0b013e31815a7b69. [DOI] [PubMed] [Google Scholar]
- 6.Giantonio BJ, Catalano PJ, Meropol NJ, et al. Bevacizumab in combination with oxaliplatin, fluorouracil, and leucovorin (FOLFOX4) for previously treated metastatic colorectal cancer: results from the Eastern Cooperative Oncology Group Study E3200. J Clin Oncol. 2007;25(12):1539–1544. doi: 10.1200/JCO.2006.09.6305. [DOI] [PubMed] [Google Scholar]
- 7.Sandler A, Gray R, Perry MC, et al. Paclitaxel-carboplatin alone or with bevacizumab for non-small-cell lung cancer. N Engl J Med. 2006;355(24):2542–2550. doi: 10.1056/NEJMoa061884. [DOI] [PubMed] [Google Scholar]
- 8.Miller K, Wang M, Gralow J, et al. Paclitaxel plus bevacizumab versus paclitaxel alone for metastatic breast cancer. N Engl J Med. 2007;357(26):2666–2676. doi: 10.1056/NEJMoa072113. [DOI] [PubMed] [Google Scholar]
- 9.Rini BI, Halabi S, Rosenberg JE, et al. Phase III trial of bevacizumab plus interferon alfa versus interferon alfa monotherapy in patients with metastatic renal cell carcinoma: final results of CALGB 90206. J Clin Oncol. 2010;28(13):2137–2143. doi: 10.1200/JCO.2009.26.5561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Motzer RJ, Hutson TE, Tomczak P, et al. Sunitinib versus interferon alfa in metastatic renal-cell carcinoma. N Engl J Med. 2007;356(2):115–124. doi: 10.1056/NEJMoa065044. [DOI] [PubMed] [Google Scholar]
- 11.Escudier B, Eisen T, Stadler WM, et al. Sorafenib in advanced clear-cell renal-cell carcinoma. N Engl J Med. 2007;356(2):125–134. doi: 10.1056/NEJMoa060655. [DOI] [PubMed] [Google Scholar]
- 12.Sternberg CN, Davis ID, Mardiak J, et al. Pazopanib in locally advanced or metastatic renal cell carcinoma: results of a randomized phase III trial. J Clin Oncol. 2010;28(6):1061–1068. doi: 10.1200/JCO.2009.23.9764. [DOI] [PubMed] [Google Scholar]
- 13.Wells SA, Jr, Robinson BG, Gagel RF, et al. Vandetanib in patients with locally advanced or metastatic medullary thyroid cancer: a randomized, double-blind phase III trial. J Clin Oncol. 2012;30(2):134–141. doi: 10.1200/JCO.2011.35.5040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Motzer RJ, Escudier B, Tomczak P, et al. Axitinib versus sorafenib as second-line treatment for advanced renal cell carcinoma: overall survival analysis and updated results from a randomised phase 3 trial. Lancet Oncol. 2013;14(6):552–562. doi: 10.1016/S1470-2045(13)70093-7. [DOI] [PubMed] [Google Scholar]
- 15.Grothey A, Van Cutsem E, Sobrero A, et al. Regorafenib monotherapy for previously treated metastatic colorectal cancer (CORRECT): an international, multicentre, randomised, placebo-controlled, phase 3 trial. Lancet. 2013;381(9863):303–312. doi: 10.1016/S0140-6736(12)61900-X. [DOI] [PubMed] [Google Scholar]
- 16.Van Cutsem E, Tabernero J, Lakomy R, et al. Addition of aflibercept to fluorouracil, leucovorin, and irinotecan improves survival in a phase III randomized trial in patients with metastatic colorectal cancer previously treated with an oxaliplatin-based regimen. J Clin Oncol. 2012;30(28):3499–3506. doi: 10.1200/JCO.2012.42.8201. [DOI] [PubMed] [Google Scholar]
- 17.Elisei R, Schlumberger MJ, Muller SP, et al. Cabozantinib in progressive medullary thyroid cancer. J Clin Oncol. 2013;31(29):3639–3646. doi: 10.1200/JCO.2012.48.4659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fuchs CS, Tomasek J, Yong CJ, et al. Ramucirumab monotherapy for previously treated advanced gastric or gastro-oesophageal junction adenocarcinoma (REGARD): an international, randomised, multicentre, placebo-controlled, phase 3 trial. Lancet. 2014;383(9911):31–39. doi: 10.1016/S0140-6736(13)61719-5. [DOI] [PubMed] [Google Scholar]
- 19.Rini BI, Michaelson MD, Rosenberg JE, et al. Antitumor activity and biomarker analysis of sunitinib in patients with bevacizumab-refractory metastatic renal cell carcinoma. J Clin Oncol. 2008;26(22):3743–3748. doi: 10.1200/JCO.2007.15.5416. [DOI] [PubMed] [Google Scholar]
- 20.Ebos JM, Lee CR, Cruz-Munoz W, Bjarnason GA, Christensen JG, Kerbel RS. Accelerated metastasis after short-term treatment with a potent inhibitor of tumor angiogenesis. Cancer Cell. 2009;15(3):232–239. doi: 10.1016/j.ccr.2009.01.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Rusnati M, Presta M. Fibroblast growth factors/fibroblast growth factor receptors as targets for the development of anti-angiogenesis strategies. Curr Pharm Des. 2007;13(20):2025–2044. doi: 10.2174/138161207781039689. [DOI] [PubMed] [Google Scholar]
- 22.Wu E, Palmer N, Tian Z, et al. Comprehensive dissection of PDGF-PDGFR signaling pathways in PDGFR genetically defined cells. PLoS One. 2008;3(11):e3794. doi: 10.1371/journal.pone.0003794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cascone T, Herynk MH, Xu L, et al. Upregulated stromal EGFR and vascular remodeling in mouse xenograft models of angiogenesis inhibitor-resistant human lung adenocarcinoma. J Clin Invest. 2011;121(4):1313–1328. doi: 10.1172/JCI42405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rigamonti N, Kadioglu E, Keklikoglou I, Wyser Rmili C, Leow CC, De Palma M. Role of angiopoietin-2 in adaptive tumor resistance to VEGF signaling blockade. Cell Rep. 2014;8(3):696–706. doi: 10.1016/j.celrep.2014.06.059. [DOI] [PubMed] [Google Scholar]
- 25.Fischer C, Jonckx B, Mazzone M, et al. Anti-PlGF inhibits growth of VEGF(R)-inhibitor-resistant tumors without affecting healthy vessels. Cell. 2007;131(3):46–475. doi: 10.1016/j.cell.2007.08.038. [DOI] [PubMed] [Google Scholar]
- 26.Ellis LM, Hicklin DJ. Pathways mediating resistance to vascular endothelial growth factor-targeted therapy. Clin Cancer Res. 2008;14(20):6371–6375. doi: 10.1158/1078-0432.CCR-07-5287. [DOI] [PubMed] [Google Scholar]
- 27.Abdullah SE, Perez-Soler R. Mechanisms of resistance to vascular endothelial growth factor blockade. Cancer. 2012;118(14):3455–3467. doi: 10.1002/cncr.26540. [DOI] [PubMed] [Google Scholar]
- 28.Beenken A, Mohammadi M. The FGF family: biology, pathophysiology and therapy. Nat Rev Drug Discov. 2009;8(3):235–253. doi: 10.1038/nrd2792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Presta M, Dell’Era P, Mitola S, Moroni E, Ronca R, Rusnati M. Fibroblast growth factor/fibroblast growth factor receptor system in angiogenesis. Cytokine Growth Factor Rev. 2005;16(2):159–178. doi: 10.1016/j.cytogfr.2005.01.004. [DOI] [PubMed] [Google Scholar]
- 30.Heldin CH, Westermark B. Mechanism of action and in vivo role of platelet-derived growth factor. Physiol Rev. 1999;79(4):1283–1316. doi: 10.1152/physrev.1999.79.4.1283. [DOI] [PubMed] [Google Scholar]
- 31.Xie J, Aszterbaum M, Zhang X, et al. A role of PDGFRalpha in basal cell carcinoma proliferation. Proc Natl Acad Sci U S A. 2001;98(16):9255–9259. doi: 10.1073/pnas.151173398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Funa K, Papanicolaou V, Juhlin C, et al. Expression of platelet-derived growth factor beta-receptors on stromal tissue cells in human carcinoid tumors. Cancer Res. 1990;50(3):748–753. [PubMed] [Google Scholar]
- 33.Bornfeldt KE, Raines EW, Nakano T, Graves LM, Krebs EG, Ross R. Insulin-like growth factor-I and platelet-derived growth factor-BB induce directed migration of human arterial smooth muscle cells via signaling pathways that are distinct from those of proliferation. J Clin Invest. 1994;93(3):1266–1274. doi: 10.1172/JCI117081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kerbel RS. Tumor angiogenesis. N Engl J Med. 2008;358(19):2039–2049. doi: 10.1056/NEJMra0706596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hellstrom M, Kalen M, Lindahl P, Abramsson A, Betsholtz C. Role of PDGF-B and PDGFR-beta in recruitment of vascular smooth muscle cells and pericytes during embryonic blood vessel formation in the mouse. Development. 1999;126(14):3047–3055. doi: 10.1242/dev.126.14.3047. [DOI] [PubMed] [Google Scholar]
- 36.Pietras K, Sjoblom T, Rubin K, Heldin CH, Ostman A. PDGF receptors as cancer drug targets. Cancer Cell. 2003;3(5):439–443. doi: 10.1016/s1535-6108(03)00089-8. [DOI] [PubMed] [Google Scholar]
- 37.Heldin CH. Targeting the PDGF signaling pathway in tumor treatment. Cell Commun Signal. 2013;11:97. doi: 10.1186/1478-811X-11-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Taeger J, Moser C, Hellerbrand C, et al. Targeting FGFR/PDGFR/VEGFR impairs tumor growth, angiogenesis, and metastasis by effects on tumor cells, endothelial cells, and pericytes in pancreatic cancer. Mol Cancer Ther. 2011;10(11):2157–2167. doi: 10.1158/1535-7163.MCT-11-0312. [DOI] [PubMed] [Google Scholar]
- 39.Kinoshita K, Nakagawa K, Hamada J, et al. Imatinib mesylate inhibits the proliferation-stimulating effect of human lung cancer-associated stromal fibroblasts on lung cancer cells. Int J Oncol. 2010;37(4):869–877. doi: 10.3892/ijo_00000738. [DOI] [PubMed] [Google Scholar]
- 40.Erber R, Thurnher A, Katsen AD, et al. Combined inhibition of VEGF and PDGF signaling enforces tumor vessel regression by interfering with pericyte-mediated endothelial cell survival mechanisms. FASEB J. 2004;18(2):338–340. doi: 10.1096/fj.03-0271fje. [DOI] [PubMed] [Google Scholar]
- 41.Bergers G, Song S, Meyer-Morse N, Bergsland E, Hanahan D. Benefits of targeting both pericytes and endothelial cells in the tumor vasculature with kinase inhibitors. J Clin Invest. 2003;111(9):1287–1295. doi: 10.1172/JCI17929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Casanovas O, Hicklin DJ, Bergers G, Hanahan D. Drug resistance by evasion of antiangiogenic targeting of VEGF signaling in late-stage pancreatic islet tumors. Cancer Cell. 2005;8(4):299–309. doi: 10.1016/j.ccr.2005.09.005. [DOI] [PubMed] [Google Scholar]
- 43.Ferrara N, Hillan KJ, Gerber HP, Novotny W. Discovery and development of bevacizumab, an anti-VEGF antibody for treating cancer. Nat Rev Drug Discov. 2004;3(5):391–400. doi: 10.1038/nrd1381. [DOI] [PubMed] [Google Scholar]
- 44.Afranie-Sakyi JA, Klement GL. The toxicity of anti-VEGF agents when coupled with standard chemotherapeutics. Cancer Lett. 2015;357(1):1–7. doi: 10.1016/j.canlet.2014.10.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Herbst RS. Toxicities of antiangiogenic therapy in non-small-cell lung cancer. Clin Lung Cancer. 2006;8(Suppl 1):S23–S30. doi: 10.3816/clc.2006.s.010. [DOI] [PubMed] [Google Scholar]
- 46.Iacovelli R, Palazzo A, Procopio G, et al. Incidence and relative risk of hepatic toxicity in patients treated with anti-angiogenic tyrosine kinase inhibitors for malignancy. Br J Clin Pharmacol. 2014;77(6):929–938. doi: 10.1111/bcp.12231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cabebe E, Fisher GA. Clinical trials of VEGF receptor tyrosine kinase inhibitors in pancreatic cancer. Expert Opin Investig Drugs. 2007;16(4):467–476. doi: 10.1517/13543784.16.4.467. [DOI] [PubMed] [Google Scholar]
- 48.Arora A, Scholar EM. Role of tyrosine kinase inhibitors in cancer therapy. J Pharmacol Exp Ther. 2005;315(3):971–979. doi: 10.1124/jpet.105.084145. [DOI] [PubMed] [Google Scholar]
- 49.Capdevila J, Carrato A, Tabernero J, Grande E. What could Nintedanib (BIBF 1120), a triple inhibitor of VEGFR, PDGFR, and FGFR, add to the current treatment options for patients with metastatic colorectal cancer? Crit Rev Oncol Hematol. 2014;92:83–106. doi: 10.1016/j.critrevonc.2014.05.004. [DOI] [PubMed] [Google Scholar]
- 50.Broekman F, Giovannetti E, Peters GJ. Tyrosine kinase inhibitors: multi-targeted or single-targeted? World J Clin Oncol. 2011;2(2):80–93. doi: 10.5306/wjco.v2.i2.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Roth GJ, Heckel A, Colbatzky F, et al. Design, synthesis, and evaluation of indolinones as triple angiokinase inhibitors and the discovery of a highly specific 6-methoxycarbonyl-substituted indolinone (BIBF 1120) J Med Chem. 2009;52(14):4466–4480. doi: 10.1021/jm900431g. [DOI] [PubMed] [Google Scholar]
- 52.Hilberg F, Roth GJ, Krssak M, et al. BIBF 1120: triple angiokinase inhibitor with sustained receptor blockade and good antitumor efficacy. Cancer Res. 2008;68(12):4774–4782. doi: 10.1158/0008-5472.CAN-07-6307. [DOI] [PubMed] [Google Scholar]
- 53.Richeldi L, du Bois RM, Raghu G, et al. Efficacy and safety of nintedanib in idiopathic pulmonary fibrosis. N Engl J Med. 2014;370(22):2071–2082. doi: 10.1056/NEJMoa1402584. [DOI] [PubMed] [Google Scholar]
- 54.Ebos JM, Kerbel RS. Antiangiogenic therapy: impact on invasion, disease progression, and metastasis. Nat Rev Clin Oncol. 2011;8(4):210–221. doi: 10.1038/nrclinonc.2011.21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Paez-Ribes M, Allen E, Hudock J, et al. Antiangiogenic therapy elicits malignant progression of tumors to increased local invasion and distant metastasis. Cancer Cell. 2009;15(3):220–231. doi: 10.1016/j.ccr.2009.01.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Sennino B, Ishiguro-Oonuma T, Wei Y, et al. Suppression of tumor invasion and metastasis by concurrent inhibition of c-Met and VEGF signaling in pancreatic neuroendocrine tumors. Cancer Discov. 2012;2(3):270–287. doi: 10.1158/2159-8290.CD-11-0240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Kutluk Cenik B, Ostapoff KT, Gerber DE, Brekken RA. BIBF 1120 (nintedanib), a triple angiokinase inhibitor, induces hypoxia but not EMT and blocks progression of preclinical models of lung and pancreatic cancer. Mol Cancer Ther. 2013;12(6):992–1001. doi: 10.1158/1535-7163.MCT-12-0995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Tai WT, Shiau CW, Li YS, et al. Nintedanib (BIBF-1120) inhibits hepatocellular carcinoma growth independent of angiokinase activity. J Hepatol. 2014;61(1):89–97. doi: 10.1016/j.jhep.2014.03.017. [DOI] [PubMed] [Google Scholar]
- 59.Awasthi N, Hinz S, Brekken RA, Schwarz MA, Schwarz RE. Nintedanib, a triple angiokinase inhibitor, enhances cytotoxic therapy response in pancreatic cancer. Cancer Lett. 2015;358(1):59–66. doi: 10.1016/j.canlet.2014.12.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hilberg F, Brandstetter I. Efficacy of BIBF 1120, a potent triple angiokinase inhibitor, in models of human non-small cell lung cancer is augmented by chemotherapy. Eur J Cancer. 2007;2:S380. [Google Scholar]
- 61.Stopfer P, Rathgen K, Bischoff D, et al. Pharmacokinetics and metabolism of BIBF 1120 after oral dosing to healthy male volunteers. Xenobiotica. 2011;41(4):297–311. doi: 10.3109/00498254.2010.545452. [DOI] [PubMed] [Google Scholar]
- 62.Mross K, Stefanic M, Gmehling D, et al. Phase I study of the angiogenesis inhibitor BIBF 1120 in patients with advanced solid tumors. Clin Cancer Res. 2010;16(1):311–319. doi: 10.1158/1078-0432.CCR-09-0694. [DOI] [PubMed] [Google Scholar]
- 63.Okamoto I, Kaneda H, Satoh T, et al. Phase I safety, pharmacokinetic, and biomarker study of BIBF 1120, an oral triple tyrosine kinase inhibitor in patients with advanced solid tumors. Mol Cancer Ther. 2010;9(10):2825–2833. doi: 10.1158/1535-7163.MCT-10-0379. [DOI] [PubMed] [Google Scholar]
- 64.Ellis PM, Kaiser R, Zhao Y, Stopfer P, Gyorffy S, Hanna N. Phase I open-label study of continuous treatment with BIBF 1120, a triple angiokinase inhibitor, and pemetrexed in pretreated non-small cell lung cancer patients. Clin Cancer Res. 2010;16(10):2881–2889. doi: 10.1158/1078-0432.CCR-09-2944. [DOI] [PubMed] [Google Scholar]
- 65.Doebele RC, Conkling P, Traynor AM, et al. A phase I, open-label dose-escalation study of continuous treatment with BIBF 1120 in combination with paclitaxel and carboplatin as first-line treatment in patients with advanced non-small-cell lung cancer. Ann Oncol. 2012;23(8):2094–2102. doi: 10.1093/annonc/mdr596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Reck M, Kaiser R, Eschbach C, et al. A phase II double-blind study to investigate efficacy and safety of two doses of the triple angiokinase inhibitor BIBF 1120 in patients with relapsed advanced non-small-cell lung cancer. Ann Oncol. 2011;22(6):1374–1381. doi: 10.1093/annonc/mdq618. [DOI] [PubMed] [Google Scholar]
- 67.Reck M, Kaiser R, Mellemgaard A, et al. Docetaxel plus nintedanib versus docetaxel plus placebo in patients with previously treated non-small-cell lung cancer (LUME-Lung 1): a phase 3, double-blind, randomised controlled trial. Lancet Oncol. 2014;15(2):143–155. doi: 10.1016/S1470-2045(13)70586-2. [DOI] [PubMed] [Google Scholar]
- 68.Hanna NK, Kaiser R, Sullivan RN, et al. Lume-lung 2: a multicenter, randomized, double-blind, phase III study of nintedanib plus pem- etrexed versus placebo plus pemetrexed in patients with advanced nonsquamous non-small cell lung cancer (NSCLC) after failure of first-line chemotherapy. J Clin Oncol. 2013;31(Suppl:8034) [Google Scholar]
- 69.Ledermann JA, Hackshaw A, Kaye S, et al. Randomized phase II placebo-controlled trial of maintenance therapy using the oral triple angiokinase inhibitor BIBF 1120 after chemotherapy for relapsed ovarian cancer. J Clin Oncol. 2011;29(28):3798–3804. doi: 10.1200/JCO.2010.33.5208. [DOI] [PubMed] [Google Scholar]
- 70.du Bois A, Kristensen G, Ray-Coquard I, et al. AGO-Ovar 12: a randomized placebo-controlled GCIG/ENGOT-intergroup phase III trial of standard frontline chemotherapy ± nintedanib for advanced ovarian cancer. Int J Gynecol Cancer. 2013;23:PL01. [Google Scholar]
- 71.Eisen T, Shparyk Y, Jones R, et al. Phase II efficacy and safety study of nintedanib versus sunitinib in previously untreated renal cell carcinoma (RCC) patients. J Clin Oncol. 2013;31(abstract 4506) [Google Scholar]
- 72.Meyer T, Palmer DH, Chao Y, et al. Efficacy and safety study of nintedanib (N) versus sorafenib (S) in Caucasian and Asian patients with advanced hepatocellular carcinoma (HCC): pooled analysis of two randomized phase II trials. J Clin Oncol. 2015;33(abstract 4074) [Google Scholar]
- 73.Droz JP, Medioni J, Chevreau C, et al. Randomized phase II study of nintedanib in metastatic castration-resistant prostate cancer postdocetaxel. Anticancer Drugs. 2014;25(9):1081–1088. doi: 10.1097/CAD.0000000000000131. [DOI] [PubMed] [Google Scholar]
- 74.Molife LR, Omlin A, Jones RJ, et al. Randomized Phase II trial of nintedanib, afatinib and sequential combination in castration-resistant prostate cancer. Future Oncol. 2014;10(2):219–231. doi: 10.2217/fon.13.250. [DOI] [PubMed] [Google Scholar]
- 75.Bouche O, Maindrault-Goebel F, Ducreux M, et al. Phase II trial of weekly alternating sequential BIBF 1120 and afatinib for advanced colorectal cancer. Anticancer Res. 2011;31(6):2271–2281. [PubMed] [Google Scholar]
- 76.Van Cutsem E, Prenen H, Guillen-Ponce C, et al. A phase I/II, open-label, randomised study of BIBF 1120* plus mFOLFOX6 compared to bevacizumab plus mFOLFOX6 in patients with metastatic colorectal cancer. Eur J Cancer. 2011;47:8–9. [Google Scholar]
- 77.Boehringer Ingelheim BTNFR A phase I-II study of BIBF 1120 and Folfox compared to Bevacizumab and Folfox in first line metastatic colorectal cancer patients. [Accessed June 3, 2013]. NLM identifier: 2008-005364-14. Available from: http://trials.boehringer-ingelheim.com/content/dam/internet/opu/clinicaltrial/com_EN/results/1199/1199.51_U12-2578-02_DR.pdf.
- 78.Quintela-Fandino M, Urruticoechea A, Guerra J, et al. Phase I clinical trial of nintedanib plus paclitaxel in early HER-2-negative breast cancer (CNIO-BR-01-2010/GEICAM-2010-10 study) Br J Cancer. 2014;111(6):1060–1064. doi: 10.1038/bjc.2014.397. [DOI] [PMC free article] [PubMed] [Google Scholar]