Abstract
Anticoagulants, such as heparin and warfarin, are commonly used in the treatment and prevention of thromboembolic events. The risk of developing warfarin-induced skin necrosis (WISN) with warfarin is reported to be <1%. However, the risk of WISN may be increased with the initiation of warfarin in the setting of heparin-induced thrombocytopenia and thrombosis syndrome (HITT). WISN can lead to catastrophic tissue necrosis requiring amputations and mass debridement. This report describes a case of WISN following HITT and discusses the appropriate medical management of patients with HITT to avoid secondary WISN.
Warfarin is considered essential in the treatment of various hypercoagulable conditions (1). However, it is known to paradoxically cause hypercoagulable conditions, including warfarin-induced skin necrosis (WISN) and venous limb gangrene (1). These complications rarely occur in the setting of warfarin therapy, but the risk of developing them may be increased following heparin-induced thrombocytopenia and thrombosis syndrome (HITT) (1). We report the case of a 64-year-old woman who developed WISN 4 days following her diagnosis of HITT.
CASE REPORT
A 64-year-old Hispanic woman with a past medical history of myocardial infarction, hypertension, and diabetes mellitus was admitted to the hospital due to a non–ST elevation myocardial infarction. The patient underwent cardiac catheterization and received several medications, including heparin. Her platelet count on admission was 184,000/mm3. After 10 days of heparin therapy, she developed bilateral lower extremity cyanosis and a decrease in platelet count to 121,000/mm3. HITT was suspected, and both a heparin PF4 antibody test and 14C-serotonin release assay were positive, confirming the diagnosis. Heparin was discontinued, and the patient was started on argatroban and warfarin.
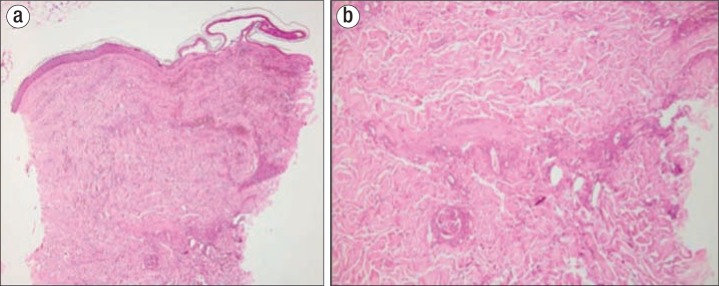
Four days after initiation of therapy, and while the patient was still on both agents, she developed ecchymosis of the right breast along with multiple hemorrhagic bullae. Her platelet count at the time was 132,000/mm3. Examination revealed a well-demarcated ecchymotic patch with overlying hemorrhagic blisters and areas of retiform purpura on the right breast (Figure 1a). Pronounced tenderness upon palpation of the right breast was also present. Bilateral lower extremities showed violaceous livedoid patches and retiform purpura on the plantar and dorsal feet and ankles, in addition to cyanosis involving all digits (Figure 1b). Laboratory evaluation demonstrated a hemoglobin of 10.8 g/dL, a hematocrit of 31.8%, a prothrombin time of 37 seconds, and an international normalized ratio of 3.5. Histopathologically, a biopsy of the right breast demonstrated widespread epidermal necrosis, thrombosed vessels containing fibrin deposits throughout the dermis, and extravasation of erythrocytes (Figure 2).
Figure 1.
(a) Right breast showing an erythematous ecchymotic patch with overlying hemorrhagic bullae. (b) Lower extremities showing violaceous livedoid patches and retiform purpura on the plantar and dorsal feet, in addition to cyanosis involving all digits.
Figure 2.
Punch biopsy from the right breast demonstrating widespread epidermal necrosis, thrombosed vessels containing fibrin deposits throughout the dermis, and extravasation of erythrocytes.
The clinical picture, along with the physical examination and the histopathologic findings, was consistent with the diagnosis of WISN. Warfarin was thus immediately discontinued, and the patient remained on monotherapy with argatroban. A right mastectomy was performed one day after the onset of the skin necrosis.
DISCUSSION
Heparin-induced thrombocytopenia (HIT) occurs in about 1% to 5% of patients receiving heparin, and only a third of patients progress to develop arterial or venous thrombosis (2). Two distinct forms of HIT exist: type I and type II (2). Type I HIT is a nonimmunologic response in which heparin induces platelet aggregation and sequestration, thus causing transient thrombocytopenia (2). Type II HIT is caused by the formation of antibodies that activate platelets, leading to a hypercoagulable state. The diagnosis is made largely based on clinical findings (2). It is confirmed by laboratory testing that demonstrates either >50% reduction in platelet count or thrombocytopenia in the setting of HIT antibody seroconversion (2). HITT is diagnosed when the criteria for HIT are met along with evidence of vascular thrombosis (2).
As for WISN, it is estimated to occur in approximately 0.01% to 0.1% of patients receiving warfarin (1). This rare adverse effect is characterized by the acute onset of paresthesia and swelling of the affected areas, followed by petechiae, ecchymosis, and eventually hemorrhagic bullae (3). Histopathologically, dermal microthrombi are found in the venules, veins, and capillaries, in addition to ischemic skin necrosis and erythrocyte extravasation (4).
Warfarin can induce a paradoxical hypercoagulable state in the early stages of treatment, usually within 3 to 10 days of therapy initiation, associated with inadequate overlap with heparin (3). The mechanism is thought to be due to a disturbance in the balance between the anticoagulant and procoagulant pathways (5). The anticoagulants protein C and protein S have a shorter half-life than other vitamin K–dependent factors, such as factors II, IX, and X (6). The net result is a deficiency in both proteins early in the treatment, which increases the chance of thrombosis and subsequent skin necrosis (5).
The risk of WISN may be increased in the setting of HIT (5). Numerous case reports have described an association between the two conditions (7–11). The generation of procoagulant, platelet-derived microparticles observed in HIT is postulated to accelerate the rate of protein C consumption, thus contributing to the early warfarin-induced protein C deficiency and an increased state of hypercoagulability (7, 12, 13). These microparticles, along with the procoagulant HIT antibodies, may also contribute to an increase in thrombin, which predisposes the patient to the development of microvascular thrombosis during warfarin treatment (7, 14). The combination of these factors can lead to catastrophic hypercoagulable consequences, as noted in our patient. Patients with HIT should thus immediately discontinue heparin. Those who require anticoagulation should be initiated on a thrombin inhibitor, such as lepirudin or argatroban, and warfarin should be avoided until complete platelet recovery is achieved (5, 15). Once the thrombocytopenia has resolved, modest doses of warfarin should be used during the transition from the direct thrombin inhibitor (5).
References
- 1.Howard-Thompson A, Usery JB, Lobo BL, Finch CK. Heparin-induced thrombocytopenia complicated by warfarin-induced skin necrosis. Am J Health Syst Pharm. 2008;65(12):1144–1147. doi: 10.2146/ajhp070352. [DOI] [PubMed] [Google Scholar]
- 2.Ahmed I, Majeed A, Powell R. Heparin induced thrombocytopenia: diagnosis and management update. Postgrad Med J. 2007;83(983):575–582. doi: 10.1136/pgmj.2007.059188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Nazarian RM, Van Cott EM, Zembowicz A, Duncan LM. Warfarin-induced skin necrosis. J Am Acad Dermatol. 2009;61(2):325–332. doi: 10.1016/j.jaad.2008.12.039. [DOI] [PubMed] [Google Scholar]
- 4.Miura Y, Ardenghy M, Ramasastry S, Kovach R, Hochberg J. Coumadin necrosis of the skin: report of four patients. Ann Plast Surg. 1996;37(3):332–337. doi: 10.1097/00000637-199609000-00017. [DOI] [PubMed] [Google Scholar]
- 5.Srinivasan AF, Rice L, Bartholomew JR, Rangaswamy C, La Perna L, Thompson JE, Murphy S, Baker KR. Warfarin-induced skin necrosis and venous limb gangrene in the setting of heparin-induced thrombocytopenia. Arch Intern Med. 2004;164(1):66–70. doi: 10.1001/archinte.164.1.66. [DOI] [PubMed] [Google Scholar]
- 6.Lewandowski K, Zawilska K. Protein C concentrate in the treatment of warfarin-induced skin necrosis in the protein C deficiency. Thromb Haemost. 1994;71(3):395–399. [PubMed] [Google Scholar]
- 7.Warkentin TE, Sikov WM, Lillicrap DP. Multicentric warfarin-induced skin necrosis complicating heparin-induced thrombocytopenia. Am J Hematol. 1999;62(1):44–48. doi: 10.1002/(sici)1096-8652(199909)62:1<44::aid-ajh7>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- 8.Celoria GM, Steingart RH, Banson B, Friedmann P, Rhee SW, Berman JA. Coumarin skin necrosis in a patient with heparin-induced thrombocytopenia—a case report. Angiology. 1988;39(10):915–920. doi: 10.1177/000331978803901009. [DOI] [PubMed] [Google Scholar]
- 9.Drakos P, Uziely B, Nagler A, Gillis S, Eldor A. Successful administration of low molecular weight heparin in a patient with heparin-induced thrombocytopenia and coumarin-induced skin necrosis. Haemostasis. 1993;23(5):259–262. doi: 10.1159/000216884. [DOI] [PubMed] [Google Scholar]
- 10.Shahak A, Pósán E, Szücs G, Rigó J, Boda Z. Coumarin-induced skin necrosis following heparin-induced thrombocytopenia and thrombosis. A case report. Angiology. 1996;47(7):725–727. doi: 10.1177/000331979604700715. [DOI] [PubMed] [Google Scholar]
- 11.White CA, Chung DA, Thomas M, Marrinan MT. Warfarin-induced skin necrosis and heparin-induced thrombocytopenia following mitral valve replacement for marantic endocarditis. J Heart Valve Dis. 2006;15(5):716–718. [PubMed] [Google Scholar]
- 12.Warkentin TE, Hayward CP, Boshkov LK, Santos AV, Sheppard JA, Bode AP, Kelton JG. Sera from patients with heparin-induced thrombocytopenia generate platelet-derived microparticles with procoagulant activity: an explanation for the thrombotic complications of heparin-induced thrombocytopenia. Blood. 1994;84(11):3691–3699. [PubMed] [Google Scholar]
- 13.Tans G, Rosing J, Thomassen MC, Heeb MJ, Zwaal RF, Griffin JH. Comparison of anticoagulant and procoagulant activities of stimulated platelets and platelet-derived microparticles. Blood. 1991;77(12):2641–2648. [PubMed] [Google Scholar]
- 14.Visentin GP, Ford SE, Scott JP, Aster RH. Antibodies from patients with heparin-induced thrombocytopenia/thrombosis are specific for platelet factor 4 complexed with heparin or bound to endothelial cells. J Clin Invest. 1994;93(1):81–88. doi: 10.1172/JCI116987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Pravinkumar E, Webster NR. HIT/HITT and alternative anticoagulation: current concepts. Br J Anaesth. 2003;90(5):676–685. doi: 10.1093/bja/aeg063. [DOI] [PubMed] [Google Scholar]