Abstract
Objective
To determine the rate of adoption of electronic medical records (EMRs) by physicians across Canada, provincial incentives, and perceived benefits of and barriers to EMR adoption.
Data sources
Data on EMR adoption in Canada were collected from CINAHL, MEDLINE, PubMed, EMBASE, the Cochrane Library, the Health Council of Canada, Canada Health Infoway, government websites, regional EMR associations, and health professional association websites.
Study selection
After removal of duplicate articles, 236 documents were found matching the original search. After using the filter Canada, 12 documents remained. Additional documents were obtained from each province’s EMR website and from the Canada Health Infoway website.
Synthesis
Since 2006, Canadian EMR adoption rates have increased from about 20% of practitioners to an estimated 62% of practitioners in 2013, with substantial regional disparities ranging from roughly 40% of physicians in New Brunswick and Quebec to more than 75% of physicians in Alberta. Provincial incentives vary widely but appear to have only a weak relationship with the rate of adoption. Many adopters use only a fraction of their software’s available functions. User-cited benefits to adoption include time savings, improved record keeping, heightened patient safety, and confidence in retrieved data when EMRs are used efficiently. Barriers to adoption include financial and time constraints, lack of knowledgeable support personnel, and lack of interoperability with hospital and pharmacy systems.
Conclusion
Canadian physicians remain at the stage of EMR adoption. Progression in EMR use requires experienced, knowledgeable technical support during implementation, and financial support for the transcription of patient data from paper to electronic media. The interoperability of EMR offerings for hospitals, pharmacies, and clinics is the rate-limiting factor in achieving a unified EMR solution for Canada.
Abstract
Objectif
Déterminer le taux d’adoption par les médecins canadiens du dossier médical électronique (DME), les mesures incitatives provinciales, mais aussi les avantages perçus au DME et les obstacles qui ralentissent son adoption.
Sources des données
Les données concernant l’adoption du DME au Canada proviennent des bases de données CINAHL, MEDLINE, PubMed, Embase, Cochrane Library, du Conseil canadien de la santé, de l’Inforoute Santé du Canada, de sites Web du gouvernement, d’associations régionales pour le DME et de sites Web d’associations de professionnels de la santé.
Choix des études
Après avoir éliminé les duplicatas d’articles, on a retenu 236 documents qui correspondaient à la recherche initiale. Après utilisation du filtre Canada, il en restait 12. Des documents additionnels ont été tirés des sites Web traitant du DME de chacune des provinces et de celui de l’Inforoute Santé du Canada.
Synthèse
Depuis 2006, le taux d’adoption du DME par les médecins canadiens a augmenté, passant d’environ 20 % à environ 62 % en 2013, avec toutefois des disparités régionales importantes, les taux variant entre environ 40 % au Nouveau-Brunswick et au Québec, et plus de 75 % en Alberta. Les mesures incitatives provinciales varient considérablement, mais semblent n’avoir qu’une faible relation avec le taux d’adoption. Plusieurs de ceux qui adoptent le DME n’utilisent qu’une fraction des fonctions disponibles de leur logiciel. Parmi les avantages du DME que mentionnent les utilisateurs, citons les gains de temps, une meilleure conservation des dossiers, une sécurité améliorée pour le patient et une meilleure confiance dans les données lorsque le DME est utilisé correctement. Les facteurs qui ralentissent l’adoption du DME incluent les contraintes de temps et de financement, le peu d’appui d’un personnel compétent et le manque d’interopérabilité avec les systèmes existant dans les hôpitaux et les pharmacies.
Conclusion
Au Canada, les médecins en sont encore au stade de l’adoption du DME. La progression dans l’utilisation du DME requiert un soutien technique expérimenté et compétent durant la période d’adoption et un soutien financier pour la transcription des données du papier au support électronique. Enfin, l’interopérabilité du DME avec les hôpitaux, les pharmacies et les cliniques est le facteur principal qui limite l’atteinte d’une solution uniforme pour l’ensemble du Canada.
Health information technology (HIT)—the hardware, software, and infrastructure required to collect, store, and exchange electronic patient information in clinical practice—is transforming health care in Canada and around the world.1 Commonly used HIT software includes electronic health records, which are person-centric records; electronic medical records (EMRs), which are provider-centric records; clinical decision support systems; computerized provider order entry; and patient reminder and scheduling software.2,3 The usual foundation for HIT in community-based ambulatory practices is the EMR,4 which works harmoniously with computerized provider order entry, electronic prescribing (e-prescribing), and clinical decision support systems, enabling community practitioner access to patient information from a central repository.5 The EMR is a portal for the adoption of other HIT in clinical practice. Despite subtle distinctions between EMRs and electronic health records, the terms are generally used interchangeably6; we use EMR in this review.
In Canada, a patchwork of EMR systems, lacking interoperability, has developed as a result of the decentralized administration of health care from the federal government to individual provinces, and from the provinces to the local level. The multidisciplinary Canada Health Infoway (CHI) was created in 2001 to establish a national infrastructure, meant to enable the exchange of health information throughout Canada.7 Its 2015 mandate sought to improve patient safety through the establishment of a baseline EMR for each Canadian that is seamlessly accessible for all health care workers in hospitals, physicians’ offices, pharmacies, and community care facilities.
On May 21, 2013, the Canadian Pharmacists Association and the Canadian Medical Association (CMA) issued a joint statement to announce their goal of having all patient prescriptions created, signed, and transmitted electronically in patients’ EMRs by 2015, and to outline a 5-point plan to ensure that this challenging target would be met.8 A prime objective is that provinces and territories work alongside CHI to increase the adoption of EMRs at the point of care, and to implement and connect drug information systems (DISs) to ensure comprehensive communications. An overview of the status of HIT adoption across Canada in support of future seamless electronic information sharing between hospitals, care facilities, pharmacies, physicians, and patients would be helpful in tracking the advancement of this initiative.
The aims of this study were to present current EMR adoption rates across Canada, characterize interprovincial differences, and identify perceived benefits of and barriers to EMR adoption that would affect the realization of 100% compliance in DISs by 2015.
DATA SOURCES
CINAHL, MEDLINE, PubMed, EMBASE, and the Cochrane Library were searched for peer-reviewed articles concerning EMRs, using the following search terms: electronic health record, medical records system, attitude of health personnel, human, health information systems, and practice management, filtered by Canada. Additionally, each province’s EMR website was reviewed for pertinent policy, programs, and practices for adoption of EMRs. Sources of gray literature such as the Health Council of Canada, CHI, CanadianEMR, Canadian Healthcare Technology, the National Physician Survey (NPS), the Commonwealth Fund International Health Policy Survey, and websites concerned with health informatics were investigated for information pertinent to the objectives of this study.
The extent of adoption of EMRs in each province of Canada was determined from these sources, and the barriers, benefits, and factors contributing to the current state were reviewed.
Study selection
After removal of duplicate articles, 236 documents were found matching the original search string. After using the filter Canada, 12 documents remained.9–20 Additional documents were obtained from each province’s EMR websites and from the CHI website.1,3,21–30
SYNTHESIS
Adoption rates by province
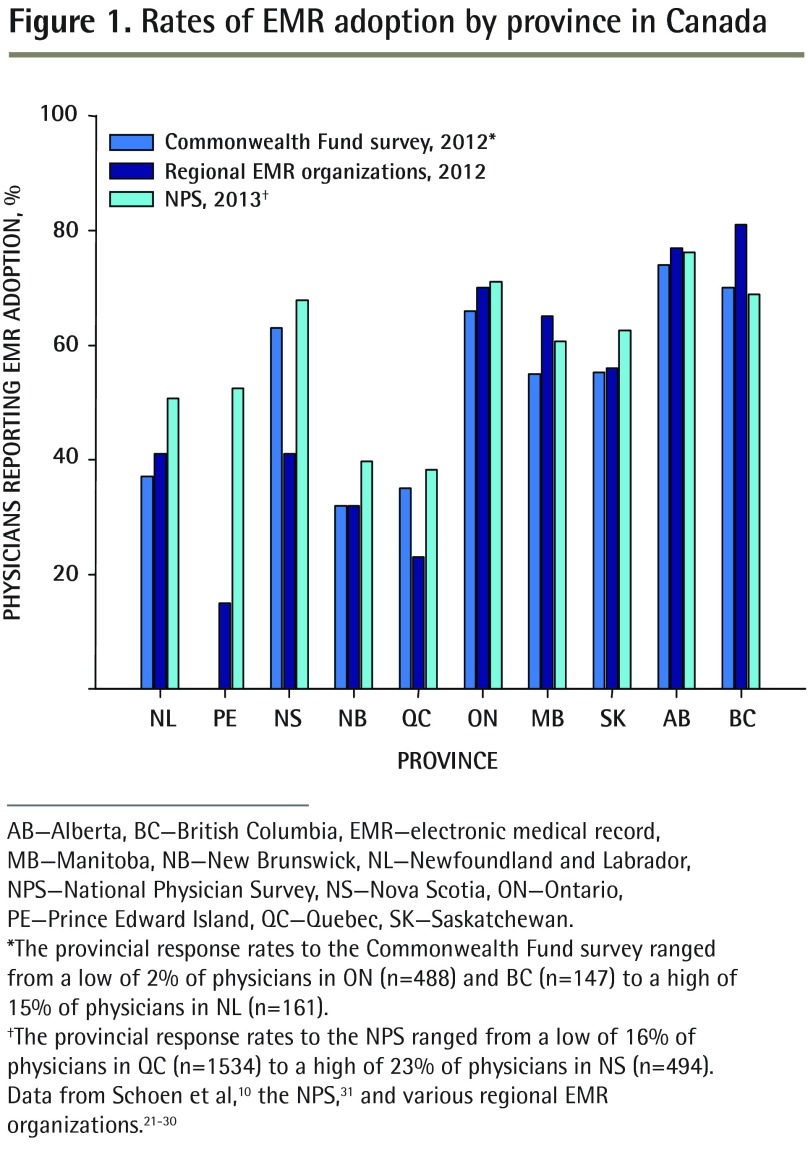
The rates of adoption of EMRs by province in Canada as reported by the NPS, the Commonwealth Fund International Health Policy Survey, and regional EMR adoption authorities are shown in Figure 1.10,21–31
Figure 1.
Rates of EMR adoption by province in Canada
AB—Alberta, BC—British Columbia, EMR—electronic medical record, MB—Manitoba, NB—New Brunswick, NL—Newfoundland and Labrador, NPS—National Physician Survey, NS—Nova Scotia, ON—Ontario, PE—Prince Edward Island, QC—Quebec, SK—Saskatchewan.
*The provincial response rates to the Commonwealth Fund survey ranged from a low of 2% of physicians in ON (n=488) and BC (n=147) to a high of 15% of physicians in NL (n=161).
†The provincial response rates to the NPS ranged from a low of 16% of physicians in QC (n=1534) to a high of 23% of physicians in NS (n=494). Data from Schoen et al,10 the NPS,31 and various regional EMR organizations.21–30
The NPS, a collaborative effort of the CMA, the College of Family Physicians of Canada, and the Royal College of Physicians and Surgeons of Canada with support from the Canadian Institute for Health Information and Health Canada, sends surveys electronically or by mail to all Canadian physicians.31 In 2013, the response rate was 17.5%, with 10 487 responses to the 60 044 surveys sent. Roughly 40% of respondents from New Brunswick (NB) and Quebec (QC); 50% of respondents from Newfoundland and Labrador (NL) and Prince Edward Island (PE); 60% of respondents from Manitoba (MB) and Saskatchewan (SK); 70% of respondents from Nova Scotia (NS), British Columbia (BC), and Ontario (ON); and more than 75% of respondents from Alberta (AB) reported using EMRs in their practices. Overall, 62% of Canadian physicians reported using EMRs.31
The Commonwealth Fund, a private American organization founded in 1918 to promote an accessible, efficient, high-quality health care system in the United States, commissioned an international survey of primary care doctors in 10 countries from March to July 2012.10 In Canada, 2124 physicians responded to the survey; the physician sample sizes ranged between 500 and 1025 physicians in other countries (United Kingdom, Norway, Germany, the Netherlands, France, Switzerland, Australia, New Zealand, and the United States). The margin of error was 2% to 4% at the 95% confidence level. The uniqueness of the data stems from the partnership of the Commonwealth Fund, which provided core support, and the Health Council of Canada, Health Quality Ontario, the Quebec Health Commission, the Health Quality Council of Alberta, and CHI to obtain a larger sample size. This survey identified EMR adoption rates below 40% in NB, QC, and NL, and above 60% in NS, ON, AB, and BC; the province of PE was not represented.
Finally, EMR adoption rates were also obtained from each province’s EMR support organizations.21–30 The rates reported by these groups were similar to those reported by the NPS and the Commonwealth Fund in the western provinces (MB, SK, AB, and BC), NB, NL, and ON but were lower than NPS estimates in PE, NS, and QC.
Interprovincial differences in EMR adoption
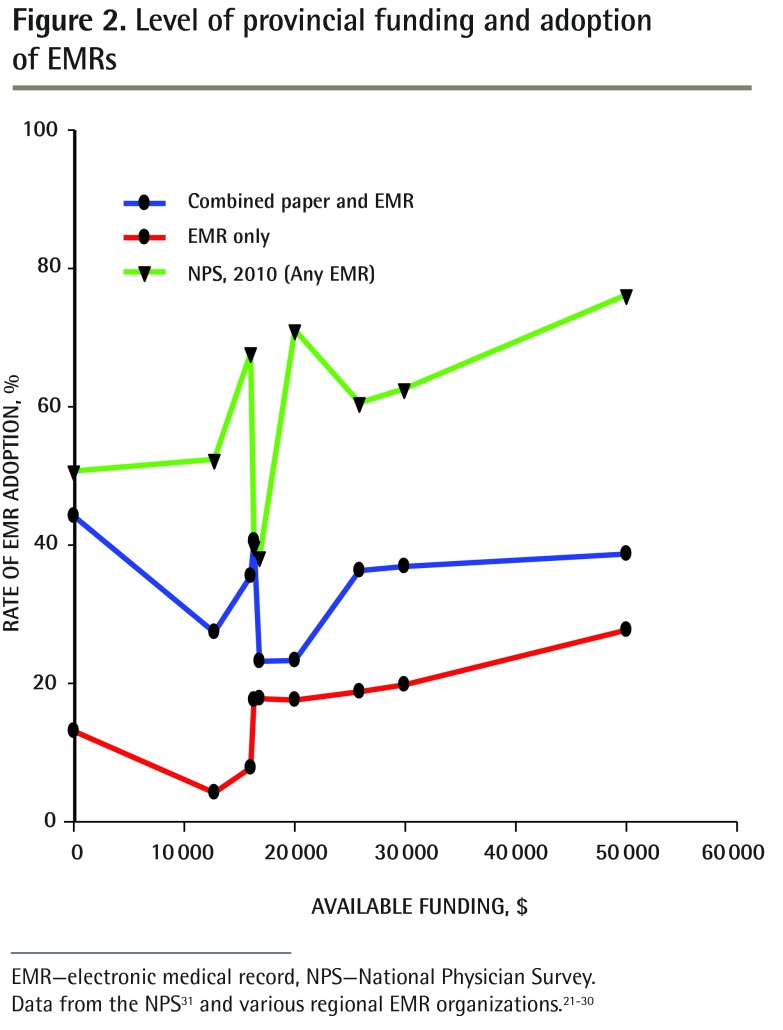
As summarized in Table 1, each province except NL has a specialized organization to promote implementation of EMRs in physicians’ offices. Support funding for individual physicians varied from none (NL, PE) to a maximum compensation of $50 000 (AB). Of the provinces offering financial incentives, 67% to 70% of eligible costs was the most common compensation rate. Nova Scotia, NB, QC, and SK did not stipulate a time limit on funding, but ON, MB, AB, and BC limited funding to 3, 2, 4.5, and 3 years, respectively. However, the level of available funding had a weak relationship with the rate of adoption of EMRs in Canada (Figure 2),21–31 suggesting that funding is not the main barrier to implementation of this technology. Indeed, according to the 2010 NPS survey,31 about half of the responding physicians from provinces with no support funding used EMRs, either alone or in combination with paper (Figure 2).21–31
Table 1.
Summary of incentives and funding for implementation of EMRs in Canadian provinces
| PROVINCE, Y | ORGANIZATION | SYSTEMS IN PLACE | FUNDED SYSTEMS | PHYSICIAN COMPENSATION |
|---|---|---|---|---|
| NL,21 1996 | Department of Health and Community Services | • PACS • DIS |
• Wolf EMR • Nightingale Informatix |
No current policy |
| PE,22 2008 | One Island Health System | • CIS • CPOE • DIS • PACS • RIS |
• Cerner Millennium | Physicians on salary contract (70% of physicians) access this as part of their contract but they are not individually compensated |
| NS,23 2005 | Primary Healthcare Information Management Program | • PACS | • Dymaxion (Practimax) • Nightingale Informatix |
• $11 000 for licence and training • $5300 implementation grant • $9600 for annual participation |
| NB,24 2012 | Velante | • None | • Intrahealth | • Maximum $16 000 • 67% of cost of setup, installation, integration, and running |
| QC,25 1996 | Quebec EMR adoption program | • RIS • PACS |
• Info-Data • Soft Informatique • Omnimed • Purkinje • KinLogix |
• Maximum $12 710 • 70% of setup costs (up to $3710) • Annual Internet (up to $2400) • $1400 for operating costs • 70% of equipment cost (up to $3500 over 4 y) |
| ON,26 2004 | OntarioMD | • CPOE • PACS |
• ABELSoft • Alpha Global IT • Canadian Health Systems • Jonoke • Med Access • MD Financial Management • Nightingale Informatix • QHR Accuro • OSCAR • P & P Data Systems • York-Med Systems |
• Maximum $29 899 • $3500 readiness grant • $2000 performance grant • $675/mo for 36 mo |
| MB,27 2007 | Manitoba Health, Manitoba eHealth, and Canada Health Infoway | • RIS • PACS |
• Clinicare • QHR Accuro • Med Access • Jonoke |
• Maximum $20 000 for new clients • Maximum $10 000 before 2009 • 70% of EMR implementation costs • 70% of operating costs for 2 y |
| SK,28 2008 | Saskatchewan EMR Program | • iEHR • PIP • RIS • PACS |
• Med Access • QHR Accuro |
• Maximum $7200 • $300/mo if 50% of encounters are captured in the EMR in the first y • 95% of encounters must be captured in the EMR to obtain continued support after first y |
| AB,29 2001 | Physician Office System Program | • PIN • DI |
• Med Access • MD Financial Management • Wolf EMR |
• Maximum of $50 000 • 52% of setup cost (up to $10 400) • $389/mo for 54 mo for maintenance |
| BC,30 2006 | Physician Information Technology Office | • PLIS | • Intrahealth • Med Access • Wolf EMR • Osler Systems |
• Maximum of $25 840 • 70% of implementation costs • 70% of equipment costs • 70% of operating costs for 3 y |
AB—Alberta, BC—British Columbia, CIS—clinical information system, CPOE—computerized physician order entry, DI—diagnostic imaging, DIS—drug information system, EMR—electronic medical record, iEHR—interoperable electronic health record, MB—Manitoba, NB—New Brunswick, NL—Newfoundland and Labrador, NS—Nova Scotia, ON—Ontario, PACS—picture archive and communication system, PE—Prince Edward Island, PIN—pharmaceutical information network, PIP—pharmaceutical information program, PLIS—Provincial Laboratory Information Solution, QC—Quebec, RIS—radiology information system, SK—Saskatchewan.
Figure 2.
Level of provincial funding and adoption of EMRs
EMR—electronic medical record, NPS—National Physician Survey.
Data from the NPS31 and various regional EMR organizations.21–30
All provincial organizations except OntarioMD have attempted to encourage interoperability by limiting the number of systems to 1 (PE, NB), 2 (NL, NS, SK), 3 (AB), 4 (MB, BC), or 5 (QC). There was considerable variation in the systems supported by each province, with picture archive and communication systems or radiology information systems most likely to be in place. Only NL and PE reported having incorporated DISs into their systems, but AB had incorporated a pharmaceutical information network and SK had a pharmaceutical information program.
Benefits and barriers to adoption of EMRs
Issues that were identified as barriers to the adoption of EMRs in Canada are summarized in Table 2.9,11–14,17–20 These studies identified the greatest barriers to adoption to be a lack of computer literacy,6,12,20 a lack of appreciation for the capacity of EMRs,11,12,17 and a lack of compatibility with other systems.6,13,17 Examples include requirements to fax prescriptions to pharmacies, prepare paper referrals to specialists whose software does not correspond with that of the ordering physician, and scan paper copies of hospital and laboratory results that could not be accessed electronically in appropriate files. Factors that contributed to the success of establishing an EMR system included the presence of a clinic “superuser” or champion11,12,19 and flexible regional leadership and support.13,19
Table 2.
Summary of barriers and success factors for implementation of EMRs in clinicians’ offices
| ARTICLE | STUDY DETAILS | SUCCESS FACTORS | BARRIERS |
|---|---|---|---|
| Boonstra and Broekhuis,6 2010 | Review of 22 articles concerning barriers to EMRs as perceived by physicians (17 American, 2 Canadian, 1 Israeli, 1 Irish, and 1 Norwegian study) | • Treat EMR implementation as a change project led by quality change managers | • Financial • Technical • Time • Psychological • Social • Legal • Organizational • Change process |
| Terry et al,12 2009 | 30 new users in southwestern Ontario | • Assess computer skills before implementing the system • Retain a full-time “superuser” for consultation |
• Poor staff computer literacy • Frustration with navigating the system |
| Denomme et al,11 2011 | Follow-up of 19 of 30 users from a previous study | • Training to ensure consistent use by all staff • Retaining a full-time “superuser” • Improved internal communication |
• Need for consistent input into EMR • Lack of enthusiasm for efficient use |
| Paterson et al,13 2010 | Interviews in 20 clinics encoded 3749 physician comments and assigned 20 themes (2 clinics per province, except 4 in ON, 3 in QC, and 1 each in the Maritime provinces) | • Personal leadership and commitment • Funding • Management change • Payment model • Collaborative culture • Integrated business and clinical aspects • Consistent, reliable data • Improved quality of care • Legibility of notes |
• Lack of interoperability with other systems • Need to scan documents from non-EMR systems into patient EMRs |
| Ludwick and Doucette,9 2009 | Semistructured interviews at AB clinics | NA | • Time constraints • Insufficient computer skills • Complex HIT user interfaces • Fee-for-service remuneration model • Poor vendor support |
| Gagnon et al,19 2010 | 15 semistructured interviews of family medicine groups in QC | • A “champion” combining roles of clinical technology and knowledge • Supportive organization open to change • Locally adapted implementation strategy |
NA |
| Rozenblum et al,18 2011 | Interviews with 29 stakeholders: national, AB (most advanced), BC (moderately advanced), and ON (least advanced) | • Funding • National standards • Patient registries • Digital imaging |
• Lack of electronic health policy • Inadequate clinician involvement • Lack of a business case to use EMRs • Focus on national not regional interoperability |
| Lau et al,14 2012 | Systematic review of EMR use and effect on practice worldwide | • Micro: user support aids adoption • Meso: better productivity and work flow • Macro: funding incentive to change |
NA |
| Price et al,17 2013 | 57 interviews in clinics using EMRs > 6 mo in MB |
NA | • Ceiling effect of current technology • Underuse owing to lack of awareness of EMR functionality |
| Kuhn and Lau,20 2014 | Study in 1 Canadian jurisdiction 4 y after EMR implementation; 46 surveys on EMR use, benefits, system, and service; paired with extraction of actual system log data on EMR use | • Relevant, accurate, complete information • Perceived enhanced efficiency • Perceived improvement in continuity of care |
• Training limitations • Security of information concerns |
AB—Alberta, BC—British Columbia, EMR—electronic medical record, HIT—health information technology, MB—Manitoba, NA—not applicable, ON—Ontario, QC—Quebec.
As summarized in Table 3,1,20,28–32 the immediate benefits of adoption of EMRs are reported to be efficiencies in staff time (no filing of or searching for records)1,14 and patient tests (fewer duplicate or unnecessary tests),1,20 and more rapid access to results or updates from other providers.1,20 Longer-term benefits include improved patient care coordination and improved patient monitoring and safety.1,20,32
Table 3.
Recognized benefits of EMR adoption
| OFFICE BENEFITS | PATIENT BENEFITS | REVENUE | USES |
|---|---|---|---|
| • Improved access to patient records20,29–31 • Improved security of patient records29,31 • Improved record and report preparation29,30 • Reduced repeated tests and tasks1,20,30,31 • Track and share prescriptions, tests, procedures20,29,32 |
• Improved patient care1,20,28–31 • Improved practice efficiency1,20,30,31 • Improved patient safety1,28,30,32 • Improved continuity of care for chronic conditions and reduced delays1,20,29,31 • Improved drug safety1,29,32 |
• Improved billing accuracy30 • Paperless or reduced paper28,30 • Improved or same revenue28,32 |
• Write prescriptions28,29,32 • Access laboratory reports20,28,30,31 • Record patient encounters28 • Drug interaction checking1,29,31,32 • Referrals1 |
EMR—electronic medical record.
DISCUSSION
Current state of EMRs in Canada
Canadian EMR adoption rates are increasing annually. In the 2010 NPS, 16% of Canadian physicians reported using EMRs exclusively and another 34% reported using a combination of EMRs and paper charts.31 Overall adoption rates have increased from about 20% of practitioners in 20061 to an estimated 62% of practitioners in 2013.31 The most commonly reported uses of EMRs were to look up patient notes (39%), electronic reminders for patient care (20%), and electronic drug interaction checking software (20%).33 Clerical and medical staff who have adopted EMRs appreciate that the long-term advantages outweigh the short-term pain in establishment. A lack of leadership and direction in the earlier years hindered many physicians from adopting a system. Of the many clinicians who have not yet adopted EMRs, a lack of computer literacy appears to be the greatest barrier to implementation, but the hours of staff time needed to learn a new system, to input current patient records into EMR files, to maintain new files, and to learn scheduling, billing, prescription, and test retrieval systems are contributing factors. Thus, the services of provincially funded and trained superusers to transform systems and to train current staff in their efficient use are likely a necessary incentive for late-stage adopters.
Why do we see interprovincial variability in EMR adoption?
Change in Canadian health care is confounded by provincial and regional variation in the driving forces behind the adoption of EMRs.33 The use of EMRs varies across Canada. Provincial survey results from western Canada and ON were generally consistent with NPS findings, while provincial survey results in eastern Canada and QC were generally lower than NPS findings. The greatest discrepancies were found in PE, NS, and QC. This might be in part attributed to differing sample sizes among reporting agencies, or to differences in the questions asked to determine the percentage of physicians using any form of electronic recording systems. The NPS, with more than 10 000 respondents, likely depicts the adoption of EMRs more accurately than the Commonwealth Fund survey, which based its results on 2000 responses. Further, the Commonwealth Fund surveys primary care physicians and the NPS surveys all physicians. The NPS tends to project the highest numbers in all provinces except MB and BC.
Interprovincial variability might be attributed to differences in funding support from provincial EMR authorities; the level of continued support (financial incentives and maintenance costs); the presence of peer-to-peer networks; the variety of EMR vendors eligible for funding; the age of physicians; and the length of time a program has been in place. For a physician contemplating adopting EMRs, a lack of support or a confusing array of possibilities might cause hesitation. An additional Canadian issue, particularly in QC and NB, is the need for information in both French and English, which reduces the number of suitable systems. While the level of funding provided by provinces differs widely, it appears to have a minimal effect on the rate of EMR adoption (Figure 2),21–31 suggesting that the rate of adoption is not primarily impeded by direct financial support.
A key factor in adoption of EMRs is the commitment of EMR organizations. In BC, officers of the Physician Information Technology Office reach out to community physicians to offer aid in implementing EMRs. Physicians who spoke to the Physician Information Technology Office were more likely to buy an EMR system and to connect with peer mentors, EMR user groups, and local EMR communities of practice.30 Other factors influencing adoption include recommendations about EMR products from fellow physicians; a product rated highly by a colleague encouraged purchase, while confusion over the large number of vendors and options caused hesitation.30
Future of EMRs
Despite numerous benefits of EMR systems, many outstanding issues require resolution. The diverse systems, priorities, and supports of the various provinces are not necessarily aligned, thereby limiting their usefulness. While EMRs from different vendors are not expected to communicate with each other, the EMR must be able to connect all physicians, and this interoperability should come from within the EMR solutions.18
Denmark is a world leader in EMR adoption.34 Each Danish citizen has a centralized electronic identifier that is used to track every contact with the health care system.35 In consultation with its physicians, Denmark mandated use of EMRs in 2004 and provided financial incentives, including technical support in the form of a team of data consultants, to individual practices. Like Canada and many of its provinces, Denmark does not support a national data system, but MedCom, a government-financed cooperative venture, similar to CHI, acts as a data integrator by setting national standards. More than 98% of Danish doctors use EMRs with advanced functions that permit inclusion of doctors’ notes, as well as information from other external providers such as specialists, hospitals, clinics, pharmacies, and laboratories, all of which is automatically entered into the EMR.35 Data-capture modules enable evaluation of treatment efficacy for chronic diseases such as diabetes or chronic obstructive pulmonary disease, which can help to determine best practices. In contrast, only 41% of Canadian primary care physicians could easily generate patient lists by diagnosis (diabetes, chronic obstructive pulmonary disease, etc), and 43% could create a list of any particular patient’s medications.36 Nonetheless, the Danish still struggle to access patient data across a number of systems and are focusing on strengthening national standards to attain convergence of local systems.34
Meeting the challenge for e-prescribing
Canada ranked seventh out of 10 countries in the use of e-prescribing in primary care, with 98% of physicians in the Netherlands and 77% of physicians in Germany using electronic forms to transmit prescriptions.10 Currently, 43% of primary care physicians in Canada report that they routinely use electronic systems to prescribe medication, with highest use in western Canada and NS and lowest use in the remaining eastern provinces.33,36 Randhawa et al report that physicians in BC use 75% of the features available on EMR software to prepare, check, and transmit prescriptions.16 However, only in QC do pharmacies fill these electronic prescriptions; elsewhere, they are entered electronically and printed out for the patient or faxed to the pharmacy.37 This is attributed to factors such as pharmacies not accepting e-prescriptions, EMR interoperability issues, and a lack of leadership or incentives. It is unlikely that the ambitious goal set by the Canadian Pharmacists Association and the CMA of having all patient prescriptions created, signed, and transmitted electronically into a patient’s EMR has been met within their timeline.
Limitations
This study was conducted to assess the current status of EMR adoption in Canada. Much of the data concerning implementation of EMRs into practice were based on survey information from a small percentage of the total physicians in Canada. It is possible that physicians responding to a survey on EMR use might not be representative of the total population of doctors, either overestimating EMR use or underestimating it. The information presented, up to date at the time of writing, reflect a rapidly changing field. Reliable information was not available from the territories, so these areas were not included in this study.
Conclusion
The early stages of EMR adoption persist in Canada, with substantial regional disparities in rates of adoption and funding support. The main obstacles to adoption of EMRs include financial and time constraints associated with the implementation of EMRs and availability of knowledgeable support personnel. The lack of interoperability of EMR offerings for hospitals, pharmacies, and clinics is the rate-limiting factor in achieving a unified EMR solution for Canada. The key outcome—realization of patient safety benefits—can only be achieved after users become familiar with record maintenance, billing, and test requisition software.
EDITOR’S KEY POINTS.
Canada is lagging in electronic health technology and is still at the stage of electronic medical record (EMR) adoption, with substantial regional disparities in rates of adoption and funding support.
Stumbling blocks to adoption of EMRs include the financial and time constraints associated with implementation, a lack of knowledgeable support personnel, and a lack of interoperability. A unified EMR solution for Canada cannot be achieved until the interoperability of EMR offerings for hospitals, pharmacies, and clinics is addressed.
The level of available funding support had a weak relationship with the rate of adoption of EMRs in Canada, suggesting that funding is not the main barrier to implementation of this technology.
POINTS DE REPÈRE DU RÉDACTEUR.
Dans le domaine de la santé, au Canada, la technologie électronique accumule du retard puisqu’elle est encore au stade de l’adoption du dossier médical électronique (DME), avec d’importantes disparités régionales dans les taux d’adoption et les sources de financement.
Les principaux facteurs qui ralentissent l’adoption du DME comprennent les contraintes de temps et de financement associées à sa mise en place, le peu de personnel de support compétent et le manque d’interopérabilité. On ne pourra pas trouver de solution pour l’ensemble du pays à moins de tenir compte de l’interopérabilité du DME avec les hôpitaux, les pharmacies et les cliniques médicales.
L’étude n’a trouvé qu’une faible relation entre le taux d’adoption des DME et le niveau du soutien financier disponible au Canada, ce qui donne à croire que le financement n’est pas le principal obstacle à l’adoption de cette technologie.
Footnotes
Contributors
Ms Gupta completed the data gathering. Dr Chang and Ms Gupta contributed to the concept and design of the study; analysis and interpretation; and preparing the manuscript for submission.
Competing interests
None declared
References
- 1.Canada Health Infoway The emerging benefits of electronic medical record use in community-based care. Toronto, ON: Health Canada Infoway; 2013. Available from: https://www.infoway-inforoute.ca/en/component/edocman/1225-the-emerging-benefits-of-electronic-medical-record-use-in-community-based-care-executive-summary/view-document?Itemid=101 Accessed 2015 Oct 27. [Google Scholar]
- 2.Häyrinen K, Saranto K, Nykanen P. Definition, structure, content, use and impacts of electronic health records: a review of the research literature. Int J Med Inform 2008;77(5):291–304. Epub 2007 Oct 22. [DOI] [PubMed] [Google Scholar]
- 3.Canada Health Infoway EMR, EHR, and PHR—why all the confusion? Toronto, ON: Health Canada Infoway; 2013. Available from: http://infowayconnects.infoway-inforoute.ca/2011/04/07/emr-ehr-and-phr-why-all-the-confusion Accessed 2015 Oct 27. [Google Scholar]
- 4.Buntin MB, Jain SH, Blumenthal D. Health information technology: laying the infrastructure for national health reform. Health Aff (Millwood) 2010;29(6):1214–9. [DOI] [PubMed] [Google Scholar]
- 5.Healthcare Information and Management Systems Society Defining and testing EMR usability: principles and proposed methods of EMR usability evaluation and rating. Chicago, IL: Healthcare Information and Management Systems Society; 2013. Available from: www.himss.org/ResourceLibrary/GenResourceDetail.aspx?ItemNumber=39192 Accessed 2015 Oct 27. [Google Scholar]
- 6.Boonstra A, Broekhuis M. Barriers to the acceptance of electronic medical records by physicians from systematic review to taxonomy and interventions. BMC Health Serv Res 2010;10:231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Catz M, Bayne J. Canada Health Infoway—a pan-Canadian approach. AMIA Annu Symp Proc 2003;2003:807. [PMC free article] [PubMed] [Google Scholar]
- 8.Canadian Pharmacists Association, Canadian Medical Association e-Prescribing: a joint statement. Ottawa, ON: Canadian Medical Association, Canadian Pharmacists Association; 2013. Available from: www.pharmacists.ca/cpha-ca/assets/File/ePrescribingStatementENG2013.pdf Accessed 2015 Oct 27. [Google Scholar]
- 9.Ludwick DA, Doucette J. Adopting electronic medical records in primary care: lessons learned from health information systems implementation experience in seven countries. Int J Med Inform 2009;78(1):22–31. Epub 2008 Jul 21. [DOI] [PubMed] [Google Scholar]
- 10.Schoen C, Osborn R, Squires D, Doty M, Rasmussen P, Pierson R, et al. A survey of primary care doctors in ten countries shows progress in use of health information technology, less in other areas. Health Aff (Millwood) 2012;31(12):2805–16. Epub 2012 Nov 15. [DOI] [PubMed] [Google Scholar]
- 11.Denomme LB, Terry AL, Brown JB, Thind A, Stewart M. Primary health care teams’ experience of electronic medical record use after adoption. Fam Med 2011;43(9):638–42. [PubMed] [Google Scholar]
- 12.Terry AL, Giles G, Brown JB, Thind A, Stewart M. Adoption of electronic medical records in family practice: the providers’ perspective. Fam Med 2009;41(7):508–12. [PubMed] [Google Scholar]
- 13.Paterson G, Shaw N, Grant A, Leonard K, Delisle E, Mitchell S, et al. A conceptual framework for analyzing how Canadian physicians are using electronic medical records in clinical care. Stud Health Technol Inform 2010;160(Pt 1):141–5. [PubMed] [Google Scholar]
- 14.Lau F, Price M, Boyd J, Partridge C, Bell H, Raworth R. Impact of electronic medical record on physician practice in office settings: a systematic review. BMC Med Inform Decis Mak 2012;12:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lau F, Partridge C, Randhawa G, Bowen M. Applying the clinical adoption framework to evaluate the impact of an ambulatory electronic medical record. Stud Health Technol Inform 2013;183:15–20. [PubMed] [Google Scholar]
- 16.Randhawa GK, Lau F, Price M. Evaluating the adoption of e-prescribing in primary care. Healthc Q 2012;16(4):55–60. [DOI] [PubMed] [Google Scholar]
- 17.Price M, Singer A, Kim J. Adopting electronic medical records. Are they just electronic paper records? Can Fam Physician 2013;59:e322–9. Available from: www.cfp.ca/content/59/7/e322.full.pdf+html Accessed 2015 Oct 26. [PMC free article] [PubMed] [Google Scholar]
- 18.Rozenblum R, Jang Y, Zimlichman E, Salzberg C, Tamblyn M, Buckeridge D, et al. A qualitative study of Canada’s experience with the implementation of electronic health information technology. CMAJ 2011;183(5):E281–8. Epub 2011 Feb 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gagnon MP, Desmartis M, Labrecque M, Légaré F, Lamothe L, Fortin JP, et al. Implementation of an electronic medical record in family practice: a case study. Inform Prim Care 2010;18(1):31–40. [DOI] [PubMed] [Google Scholar]
- 20.Kuhn K, Lau F. Evaluation of a shared electronic health record. Healthc Q 2014;17(1):30–5. [DOI] [PubMed] [Google Scholar]
- 21.Newfoundland and Labrador Centre for Health Information Annual report, part 3.7. St John’s, NL: Auditor General of Newfoundland and Labrador; 2013. Available from: www.ag.gov.nl.ca/ag/annualReports/2012AnnualReport/3.7%20%20NL%20Centre%20for%20Health%20Information.pdf Accessed 2015 Oct 27. [Google Scholar]
- 22.Health PEI [website] Electronic health records. Charlottetown, PE: Health PEI; 2013. Available from: www.healthpei.ca/ehr Accessed 2015 Jul 6. [Google Scholar]
- 23.Doctors Nova Scotia [website] Electronic medical records. Dartmouth, NS: Doctors Nova Scotia; 2013. Available from: www.doctorsns.com/en/home/practiceresources/electronicmedicalrecords/default.aspx Accessed 2015 Oct 27. [Google Scholar]
- 24.Velante [website] Who is choosing Velante? Fredericton, NB: Velante; 2015. Available from: http://velante.com/en/emr/why_emr Accessed 2015 Jul 6. [Google Scholar]
- 25.Société de gestion informatique [website] Technologies de l’information internet. Quebec city, QC: Santé et services sociaux; 2013. Available from: www.ti.msss.gouv.qc.caAccessed 2015 Jul 6. [Google Scholar]
- 26.OntarioMD [website] EMR funding overview. Toronto, ON: Ontario MD; 2013. Available at https://www.ontariomd.ca/portal/server.pt/community/emr_funding/new_emr_adopters Accessed 2015 Jul 6. [Google Scholar]
- 27.Manitoba eHealth [website] Electronic medical record (EMR) adoption program fact sheet. Winnipeg, MB: Manitoba eHealth; 2013. Available from: www.manitoba-ehealth.ca/files/pcis-emr-adopt-fs.pdf Accessed 2015 Jul 6. [Google Scholar]
- 28.Saskatchewan EMR program Program positioned well to reach its objective. SMA News Digest 2013; 53(1):7–9. Available from: www.sma.sk.ca/kaizen/content/files/SMA_News_Digest_Winter_2013.pdf Accessed 2015 Oct 27. [Google Scholar]
- 29.Physician Office System Program Performance measure definition. Physician’s use of electronic medical records (EMR). Edmonton, AB: Government of Alberta; 2013Available from: www.health.alberta.ca/documents/PMD-Physicians-Use-EMR.pdf. Accessed 2015 Jul 6. [Google Scholar]
- 30.Physician Information Technology Office Why use EMRs? Vancouver, BC: Physician Information Technology Office; 2013. [Google Scholar]
- 31.National Physician Survey National Physician Survey results. Mississauga, ON: College of Family Physicians of Canada; 2014. Available from: nationalphysiciansurvey.ca/surveys Accessed 2015 Oct 27. [Google Scholar]
- 32.Silversides A. Canadian physicians playing “catch-up” in adopting electronic medical records. CMAJ 2010;182(2):E103–4. Epub 2009 Dec 7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Biro SC, Barber DT, Kotecha JA. Trends in the use of electronic medical records [Fast Facts]. Can Fam Physician 2012;58:e21 Available from: www.cfp.ca/content/58/1/e21.full.pdf+html Accessed 2015 Oct 26. [PMC free article] [PubMed] [Google Scholar]
- 34.Kierkegaard P. E-prescription across Europe. Health Technol 2013;3:205–19. [Google Scholar]
- 35.Denmark: electronic patient records. MedTech Europe; 2012. Available from: www.reforminghealthcare.eu/economist-report/some-roads-ahead-innovative-approaches-in-five-west-european-countries/denmark-electronic-patient-records Accessed 2015 Oct 27. [Google Scholar]
- 36.Health Council of Canada How do Canadian primary care physicians rate the healthcare system? Health Care Matters Bulletin 2013;7:1–47. Available from: http://publications.gc.ca/collections/collection_2013/ccs-hcc/H173-1-7-2013-eng.pdf Accessed 2015 Oct 27. [Google Scholar]
- 37.Simpson C. E-prescribing—nothing to write home about yet. Ottawa, ON: Canadian Medical Association; 2014. Available from: https://www.cma.ca/En/Pages/E-prescribing-nothing-to-write-home-about-yet.aspx Accessed 2015 Oct 27. [Google Scholar]