Abstract
Objective
To describe the smoking patterns of patients receiving elective surgery and their knowledge about the benefits of smoking cessation to inform and strengthen support for patients to quit smoking in order to optimize surgical outcomes.
Design
Patients who had elective surgery were screened for smoking status, and eligible patients completed a telephone survey.
Setting
Two regional hospitals in northern British Columbia.
Participants
Of 1722 patients screened, 373 reported smoking before surgery. Of these, 161 (59.0% women) completed a telephone survey.
Main outcome measures
Patient smoking cessation, knowledge of the perioperative risks of smoking, use of resources, and health care provider advice and assistance.
Results
Participants included 66 men and 95 women (mean [SD] age of 51.9 [14.0] years). In total, 7.5% of these patients quit smoking in the 8 weeks before their surgeries, although an additional 38.8% reduced their smoking. Only about half of the patients surveyed were aware that continuing to smoke increased their surgical risks. Further, only half of the patients surveyed reported being advised to quit before their surgeries by a health care professional. Few were using the provincial resources available to support smoking cessation (eg, QuitNow), and 39.6% were unaware of the provincial program to cover the cost of smoking cessation aids (eg, nicotine gum or patches), yet 62.7% of respondents were thinking about quitting smoking.
Conclusion
Many surgical patients in northern British Columbia who smoked were unaware of the perioperative risks of smoking and the cessation support available to them. An opportunity exists for all health care professionals to encourage more patients to quit in order to optimize their surgical outcomes.
Abstract
Objectif
Décrire les habitudes de tabagisme de patients en attente d’une chirurgie élective et déterminer ce qu’ils savent des avantages d’arrêter de fumer, les renseigner sur les méthodes favorisant l’arrêt du tabac et ainsi optimiser les résultats des chirurgies.
Type d’étude
On a évalué les habitudes de tabagisme chez des patients en attente d’une chirurgie élective; on a demandé aux patients admissibles de répondre à une enquête téléphonique.
Contexte
Deux hôpitaux régionaux du nord de la Colombie-Britannique.
Participants
Sur les 1722 patients qui ont été évalués, 373 ont déclaré qu’ils fumaient avant d’être opérés. Parmi ces derniers, 161 (dont 59,0 % de femmes) ont répondu à l’enquête téléphonique.
Principaux paramètres à l’étude
L’abandon du tagabisme par les patients, leur connaissance des risques péri-opératoires associés au tabac, leur utilisation des ressources disponibles, et les conseils et l’assistance fournis par les professionnels de la santé.
Résultats
Les participants comprenaient 66 hommes et 95 femmes (âge moyen [DS] : 51,9 [14,0]). Dans l’ensemble, 7,5 % de ces patients ont cessé de fumer au cours des 8 semaines précédant l’opération, et 38,8 % de plus ont réduit leur consommation de tabac. Seulement la moitié environ des participants savaient que le fait de continuer de fumer augmente les risques péri-opératoires. En outre, la moitié seulement a rapporté qu’un professionnel de la santé leur avait conseillé de cesser de fumer avant l’opération. Peu de répondants avaient recours aux mesures provinciales disponibles favorisant l’arrêt du tabagisme (p. ex. QuitNow), et 39,6 % d’entre eux n’étaient pas au courant du programme provincial qui couvre le coût des mesures favorisant l’arrêt du tabagisme (p. ex. la gomme ou les timbres à la nicotine), et pourtant 62,7 % des répondants envisageaient déjà d’arrêter de fumer.
Conclusion
Plusieurs fumeurs du nord de la Colombie-Britannique en attente de chirurgie ne connaissaient pas les risques péri-opératoires associés au tabac et ignoraient les mesures existantes pour les aider à arrêter. Les professionnels de la santé ont donc là une excellente occasion d’inciter davantage de patients à cesser de fumer pour optimiser leurs résultats chirurgicaux.
The challenges inherent in meeting the need for surgical services in northern and rural regions of Canada have been addressed through various practice models involving resident specialist surgeons and general practitioner surgeons, as well as family physicians and other health professionals.1 Accordingly, in low-volume centres, ensuring the quality and convenience of care for patients before and after surgery is a responsibility that is shared by a range of health care providers, including family physicians in remote communities served by these centres, where surgical patients might reside.
In regions where smoking rates are high, one important way to optimize surgical outcomes is to support smoking cessation. Surgical patients who smoke have greater risk of poor intraoperative and postoperative outcomes, including general morbidity, wound complications (eg, surgical site infections, slower healing, dehiscence, delayed healing), general infections, pulmonary complications (eg, unplanned intubation, reduced pulmonary function, and mucus accumulation with immobilization during and after surgery), neurologic complications, and admission to intensive care units.2–5 It is important, therefore, to ensure that surgical patients who smoke are aware of their increased surgical risks. A recent survey of surgical patient smokers in Australia revealed that less than half were aware of the perioperative risks of smoking.6
Although an upcoming surgery has been described as a “teachable moment” for cessation,7 in Canada efforts to encourage patients to quit before surgery are relatively recent, sporadic, and lacking a systematic approach. Notably, some work has taken place in western Canada, and the most formalized examples are in Ontario.8 Nevertheless, there are unique challenges in providing smoking cessation support to surgical patients in rural and remote communities, where there is often a low volume of surgeries (relative to large urban centres). The integration of tobacco use interventions into routine care in multiple heterogeneous centres competes with other priorities, and ongoing training and support for health care professionals who are geographically dispersed can be difficult. Despite this, the absence of consistent identification and education of this patient population presents an opportunity for improved patient care.9
In Canada, nearly half of all smokers report that they attempted to quit in the past year, and two-thirds were planning to quit within the next 6 months.10 The smoking rate in northern British Columbia (BC) in 2012 was 24%, substantially higher than the provincial average of 11%.10,11 The region also has the highest rate of lung cancer in the province. Consequently, implementing new approaches to support smoking cessation is a priority for strengthening cancer prevention in northern BC. Although patients who smoke benefit from smoking cessation support before surgery,12 up-to-date information is lacking from northern and rural regions about smoking cessation rates among surgical patients and the information and support they receive for cessation. This information is needed to guide future efforts to enhance health care services in these regions.
The objectives of this study were to survey a sample of northern BC surgical patients who smoked in order to investigate their level of knowledge about the perioperative risks of smoking, the proportion of patients who quit smoking before surgery, whether health care provider advice was received, and patients’ knowledge and use of resources to support smoking cessation.
METHODS
Study design
This research was approved by the University of British Columbia Behavioural Research Ethics Board and the Northern Health Research Review Committee. This cross-sectional study involved surveying surgical patients recruited from 2 regional hospitals serving northern BC residents. One hospital, a 200-bed facility near the centre of BC, carries out approximately 5700 surgeries annually. The second, a 25-bed facility located in the northwest that performs approximately 1600 surgeries annually, was chosen to represent other northern regional hospitals offering a full range of services. A provincewide effort and a tobacco reduction policy in the health authority were in place to encourage health care providers to advise and assist with cessation.
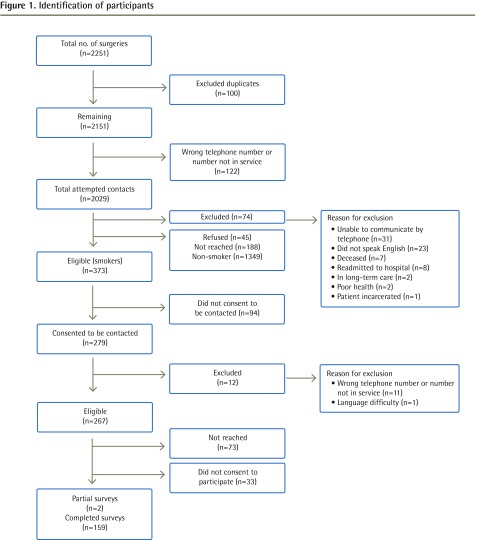
Sample and procedure
To recruit participants, patients (n = 2251) who underwent elective surgery at the 2 hospitals between December 1, 2012, and March 31, 2013, were contacted and screened. Of the 1722 patients contacted, 373 (21.7%) reported smoking at least 1 cigarette in the 6 months before their surgeries. Of these, 279 patients provided consent to have their contact information released and were forwarded a letter about the study before receiving a telephone call inviting them to participate in a telephone survey. Figure 1 outlines participant inclusion and exclusion. Patients who participated in the telephone survey were mailed a $5 gift card.
Figure 1.
Identification of participants
Measures
Items assessing tobacco use were derived from measures used in national surveys and developed by experts in the field. The survey was pilot-tested with a subsample of participants (n = 10). Patients were asked about their smoking before and after their surgery (eg, Did you smoke cigarettes in any amount in the 2 months before your surgery? In the 2 months before your surgery, how many days in total did you not smoke any cigarettes [not even a puff]? During the 2-month period before your surgery, did you reduce your smoking?). Also included were questions about advice and support received from health providers (eg, Did your doctor or another health provider advise you to quit smoking at any time in the 2 months before your surgery? When you were in hospital for your surgery, did anyone ask you about your smoking?). Finally, patients were asked about any smoking cessation resources they used before surgery (eg, QuitNow) and whether they were aware of the BC Ministry of Health program to cover the cost of smoking cessation aids (eg, nicotine gum or patches).
Two measures with established reliability and validity were also included to describe the patient sample: the smoking stages of change scale (short form) based on the transtheoretical model of behaviour change13 and the Fagerstrom Test for Nicotine Dependence14 (Cronbach α = .65). Finally, a measure developed by Webb and colleagues was included to assess awareness of smoking-related perioperative complications.6 Using a Likert response scale (very likely = 3; somewhat likely = 2; somewhat unlikely = 1; very unlikely = 0; do not know = 0), patients were asked, “As far as you know, does smoking make any of the following likely?” for each of slower healing of wounds after surgery, increased risk of infection after surgery, increased pain after surgery, increased complications with the anesthesia, and increased risk of future heart or lung problems. Responses to the first 4 items were averaged to create a scale for awareness of smoking-related perioperative complications, with scores ranging from 0 to 3 (Cronbach α = .75). The last item assessed future health problems related to smoking and was scored separately.
Data analysis
Categorical variables were summarized using frequencies and percentages, and continuous variables were summarized using means and standard deviations. Data analyses were completed using SPSS, version 21.0.
RESULTS
In total 161 patients (66 men, 95 women), ranging in age from 20 to 78 years, participated in the survey. This represents a response rate of 60.3% of eligible participants. Demographic and smoking-related characteristics are displayed in Tables 1 and 2, respectively. In total, 105 (65.6%) patients reported that they quit smoking for at least 24 hours in the 2 months before their surgery. Presurgical quit durations were predominately short (Table 3), yet 12 (7.5%) patients abstained from smoking for the entire 8 weeks before their surgery, and an additional 62 (38.8%) reported that they reduced their smoking. Independent-samples t tests and χ2 analyses revealed that the samples from the 2 hospitals did not differ on any demographic or smoking-related variables.
Table 1.
Demographic characteristics of the patient sample: N = 161; not all participants answered all questions.
| CHARACTERISTIC | VALUE |
|---|---|
| Mean (SD) age, y | 51.9 (14.0) |
| Female, n (%) | 95 (59.0) |
| Ethnicity, n (%)* | |
| • White | 122 (76.7) |
| • First Nations or Metis | 32 (20.1) |
| • Asian | 2 (1.3) |
| • Other | 3 (1.9) |
| Marital status, n (%)* | |
| • Single | 28 (17.6) |
| • Married or common-law | 93 (58.5) |
| • Separated or divorced | 28 (17.6) |
| • Widowed | 10 (6.3) |
| Education level, n (%)* | |
| • Some high school or less | 41 (25.8) |
| • High school | 40 (25.2) |
| • Trade certification or some college | 46 (28.9) |
| • Community college degree | 11 (6.9) |
| • Some university | 8 (5.0) |
| • University undergraduate degree | 11 (6.9) |
| • University postgraduate degree | 2 (1.3) |
| Employment status, n (%)* | |
| • Full-time | 74 (46.5) |
| • Part-time | 17 (10.7) |
| • Not employed | 34 (21.4) |
| • Retired | 34 (21.4) |
| Annual household income, n (%)† | |
| • < $20 000 | 28 (18.4) |
| • $20 000–$39 999 | 36 (23.7) |
| • $40 000–$59 999 | 20 (13.2) |
| • $60 000–$79 999 | 24 (15.8) |
| • $80 000–$99 999 | 20 (13.2) |
| • ≥ $100 000 | 24 (15.8) |
| Type of surgery, n (%) | |
| • Abdominal | 46 (28.6) |
| • Orthopedic | 39 (24.2) |
| • Gynecologic | 23 (14.3) |
| • Urologic | 10 (6.2) |
| • Eye | 11 (6.8) |
| • Vascular | 7 (4.3) |
| • Cardiac | 3 (1.9) |
| • Other | 22 (13.7) |
N = 159.
N = 152.
Table 2.
Smoking-related characteristics of the patient sample: N = 161.
| CHARACTERISTIC | VALUE |
|---|---|
| Mean (SD) age of initiation, y | 14.7 (5.2) |
| Mean (SD) age daily smoking began, y | 18.2 (7.0) |
| Mean (SD) cigarettes per day for current smokers | 15.5 (10.4) |
| Mean (SD) cigarettes per day before quitting | 16.5 (12.6) |
| Mean (SD) nicotine dependence score* | 3.5 (2.4) |
| Stage of change for considering smoking cessation, n (%) | |
| • Precontemplation | 30 (18.6) |
| • Contemplation | 60 (37.3) |
| • Preparation | 41 (25.5) |
| • Action | 29 (18.0) |
Possible scores range from 1 to 10, with scores of 8 or higher indicating high nicotine dependence.
Table 3.
Number of days in the 2 months before surgery on which patients did not smoke at all: N = 161.
| DURATION OF ABSTINENCE | N (%) |
|---|---|
| 1 day | 37 (23.0) |
| 2–5 days | 21 (13.0) |
| 6–9 days | 16 (9.9) |
| 10–20 days | 12 (7.5) |
| 4 weeks | 7 (4.3) |
| 8 weeks | 12 (7.5) |
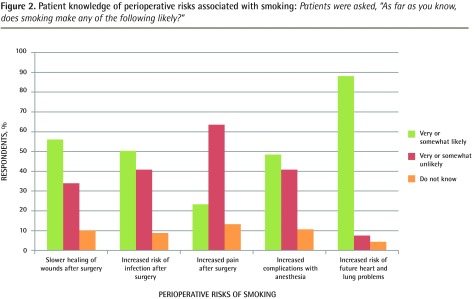
Although most patients correctly identified future heart and lung problems as a smoking-related risk, the mean (SD) score on the awareness of smoking-related perioperative complications scale was low (1.22 [0.83], range 0 to 3). Slightly more than half identified slower healing as being “very likely or somewhat likely”; however, less than half were aware of the association between smoking and postsurgical infection, pain after surgery, or complications with anesthesia (Figure 2). Patients who quit or reduced their smoking before surgery did not have a higher mean (SD) awareness score (1.20 [0.88]) than those who continued to smoke the same amount (1.23 [0.79]; F1,156 = 0.05, P = .83).
Figure 2.
Patient knowledge of perioperative risks associated with smoking: Patients were asked, “As far as you know, does smoking make any of the following likely?”
Approximately half of the patients (n = 84, 52.5%) recalled being advised to quit by a health care provider in the 2 months before their surgeries, and 52 (32.3%) were given specific help to quit smoking. When in the hospital, 77 (48.1%) reported being asked about their smoking and 26 (16.3%) were given help. Although 38 (45.2%) of the patients who were advised to quit by a health care provider reported that they reduced their smoking or quit, this was not significantly different from those who reduced their smoking or quit and were not advised (n = 36 [47%], , P = .84). Patients who were advised to quit also did not have a higher mean (SD) score on the awareness of smoking-related perioperative complications scale (1.23 [0.87]) than those not advised (1.22 [0.79]; F1,157 = 0.00, P = .98). In the 2 months before their surgery, 34 (21.3%) patients reported using nicotine patches, 24 (15.0%) used nicotine gum or lozenges, and 12 (7.5%) used a medication (eg, varenicline). QuitNow services were used infrequently: 8 (5.0%) reported accessing the website, 10 (6.3%) accessed the telephone service, and none reported using the text service. In total, 63 (39.6%) were unaware of the BC Ministry of Health program to cover the cost of pharmaceutical cessation aids, and 36 (22.4%) had received aids through this program.
DISCUSSION
Smoking cessation before surgery provides an important opportunity to optimize surgical outcomes. To our knowledge this is the first study to provide information about patterns of smoking cessation before surgery in a health authority serving a large rural area where multiple hospitals of varying size provide surgical procedures. The findings indicate that in a sample of surgical patients in northern BC, knowledge about the perioperative risks of smoking and use of smoking cessation resources were low. Further, few patients were completely smoke free before their surgeries, even though stage of change scores suggested most were interested in quitting. There were no differences between the patients having surgery in the low- and high-volume regional hospitals.
The fact that many patients were unaware of the association between smoking and postsurgical infection, slower healing, pain after surgery, or complications with anesthesia mirrors the findings of research conducted in Australia.6 Awareness of the association between smoking and heart and lung problems in this sample was similar to findings reported by Webb et al6 and might be attributable to public health campaigns and cigarette label warnings about these more general risks. The results suggest a need for systematic approaches to ensuring that all surgical patients who smoke are provided with information about the perioperative risks of smoking.
The 2 northern BC hospitals included in this study are regional hospitals serving residents from many surrounding communities. Patients were therefore likely to be in contact with their family physicians as well as their surgeons both before and following their elective surgeries. In addition, all patients were required to attend a preoperative assessment within 30 days of their surgery, providing another opportunity for a health care professional to address tobacco use. Nevertheless in our study, only half of the patients surveyed reported being advised to quit in the 2 months before their surgery by a health care professional. These findings are similar to a 2012 national survey of Canadian smokers that found that only half of those who had visited a health care provider in the previous 6 months had been advised to quit.10 Yet a recent survey of patients from Ontario family health teams indicates a promising trend to higher rates, with 74% having been advised to quit smoking in the previous 12 months.15 Our findings suggest that in regional and northern centres where smoking rates are higher, there is an opportunity for improving targeted cessation advice and support.
Perplexingly, we found that receiving advice from a health care professional was not related to whether or not patients quit or reduced their smoking. It seems possible that, even if advised to quit, many might not have been informed of the surgical risks associated with smoking, which could have provided further incentive to quit. Indeed, patients who received advice to quit were no more aware of the surgical risks of smoking than those who did not receive such advice. Further, many patients attempted to quit smoking, but quit durations were fairly short. Evidence suggests that telephone counseling and pharmacologic aids can support smoking cessation16–19; however, few patients reported using these resources. Consistent with a national survey of Canadian smokers in 2012, only about a third of the patients in this study were referred by a health care provider to resources to help them quit smoking.10
Physician advice and support has been shown in other research to increase patient smoking cessation,20 and experts agree that pending surgery can provide further incentive for patients to stop smoking.7,9 Given that most surgical patients were interested in quitting, and that presurgical services are provided by various health professionals, systems need to be designed to ensure that throughout the perioperative period all elective surgery patients are screened for smoking status and provided with information about the benefits of smoking cessation for surgery, assistance with quitting, and referral to cessation resources. As these health care professionals have numerous other roles and responsibilities, systems for addressing tobacco use with surgical patients in rural communities should be easy to use and flexible, and should enable information to be shared between community-based providers and hospital services. Family physicians have an important role in advocating for such systems and the resources to enable the provision of patient education and support for smoking cessation during the entire perioperative period.
Limitations
It should be noted that there are limits in terms of generalizability when describing the retrospective experiences of a regionally based sample of surgical patients. Participant responses might be subject to recall bias, and smoking patterns were based on self-report. In addition, we oriented our research to the 2 months before surgery. Although it is possible that some patients waiting for elective surgery might have received advice about smoking cessation before this time frame, the low rates of smoking cessation before surgery indicate that patients would benefit from additional support. The findings provide new information on patient smoking behaviour before surgery that can serve as a basis for measuring changes in policies and practice aimed at strengthening surgery-specific smoking cessation.
Conclusion
The results of this research indicate that there continues to be gaps in patient knowledge of the surgical risks of smoking. An opportunity exists for all health care professionals serving rural and northern communities to optimize surgical outcomes by informing patients about the benefits of quitting smoking before surgery and the resources available to support smoking cessation.
Acknowledgment
This research was supported by the Canadian Cancer Society Research Institute (Grant #701259-00).
EDITOR’S KEY POINTS.
There is a substantive body of evidence linking smoking before surgery to increased perioperative risks. This survey of surgical patients from northern British Columbia who smoked revealed that many of them were unaware of the perioperative risks of smoking, only half were advised to quit smoking before their surgery, and few used provincial cessation resources.
Increasing patient knowledge of the surgical risks of smoking and the availability of cessation resources might encourage more patients to quit before surgery and optimize surgical outcomes.
POINTS DE REPÈRE DU RÉDACTEUR.
De nombreuses données indiquent que le fait de fumer avant une opération augmente les risques péri-opératoires. Cette enquête chez des fumeurs du nord de la Colombie-Britannique en attente d’une chirurgie a révélé que plusieurs d’entre eux n’étaient pas conscients des risques péri-opératoires qu’ils encouraient en fumant; seulement la moitié avait eu le conseil de cesser de fumer avant l’opération et seuls quelques-uns avaient eu recours aux ressources provinciales favorisant l’arrêt du tabac.
En renseignant davantage les patients sur les risques chirurgicaux associés au tabagisme et sur les ressources existantes pour arrêter de fumer, on pourrait aider plus de patients à cesser de fumer avant leur intervention et ainsi optimiser les résultats des chirurgies.
Footnotes
Contributors
Dr Bottorff was involved in the study conception and design, data collection and interpretation, and drafting, revising, and approving the article. Dr Seaton was involved in the study design, data collection and analysis, interpretation of the data, and drafting the article. Ms Lamont was involved in the study conception and design, and drafting the article.
Competing interests
None declared
References
- 1.Kornelsen J, Iglesias S, Humber N, Caron N, Grzybowski S. The experience of GP surgeons in western Canada: the influence of interprofessional relationships in training and practice. J Res Interprof Pract Educ 2013; 3 (1):43–61. [Google Scholar]
- 2.Grønkjær M, Eliasen M, Skov-Ettrup LS, Tolstrup JS, Christiansen AH, Mikkelsen SS, et al. Preoperative smoking status and postoperative complications: a systematic review and meta-analysis. Ann Surg 2014; 259 (1):52–71. [DOI] [PubMed] [Google Scholar]
- 3.Schmid M, Sood A, Campbell L, Kapoor V, Dalela D, Klett DE, et al. Impact of smoking on perioperative outcomes after major surgery. Am J Surg 2015; 210 (2):221–9. Epub 2015 Apr 23. [DOI] [PubMed] [Google Scholar]
- 4.Sørensen LT. Wound healing and infection in surgery. The clinical impact of smoking and smoking cessation: a systematic review and meta-analysis. Arch Surg 2012; 147 (4):373–83. [DOI] [PubMed] [Google Scholar]
- 5.Turan A, Mascha EJ, Roberman D, Turner PL, You J, Kurz A, et al. Smoking and perioperative outcomes. Anesthesiology 2011; 114 (4):837–46. [DOI] [PubMed] [Google Scholar]
- 6.Webb AR, Robertson N, Sparrow M. Smokers know little of their increased surgical risks and may quit on surgical advice. ANZ J Surg 2013; 83 (10):753–7. Epub 2013 Feb 17. [DOI] [PubMed] [Google Scholar]
- 7.Shi Y, Warner DO. Surgery as a teachable moment for smoking cessation. Anesthesiology 2010; 112 (1):102–7. [DOI] [PubMed] [Google Scholar]
- 8.Welcome to “Stop Smoking for Safer Surgery” [website] Toronto, ON: Ontario’s Anesthesiologists; 2014. Available from: www.ontarioanesthesiologists.com/what-we-do Accessed 2015 Jun 13. [Google Scholar]
- 9.Oyston J. The role of anesthesiologists in promoting smoking cessation. Can J Anaesth 2011; 58 (10):897–9 (Eng), 899–901 (Fr). Epub 2011 Jun 30. [DOI] [PubMed] [Google Scholar]
- 10.Reid JL, Hammond D, Rynard VL, Burkhalter R. Tobacco use in Canada: patterns and trends. 2014. ed. Waterloo, ON: Propel Centre for Population Health Impact, University of Waterloo; 2014. [Google Scholar]
- 11.Northern Health Position on tobacco reduction: an integrated population health report. Prince George, BC: Northern Health; 2012. [Google Scholar]
- 12.Zaki A, Abrishami A, Wong J, Chung FF. Interventions in the preoperative clinic for long term smoking cessation: a quantitative systematic review. Can J Anaesth 2008; 55 (1):11–21. [DOI] [PubMed] [Google Scholar]
- 13.Velicer WF, Fava JL, Prochaska JO, Abrams DB, Emmons KM, Pierce JP. Distribution of smokers by stage in three representative samples. Prev Med 1995; 24 (4):401–11. [DOI] [PubMed] [Google Scholar]
- 14.Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom KO. The Fagerstrom Test for Nicotine Dependence: a revision of the Fagerstrom Tolerance Questionnaire. Br J Addict 1991; 86 (9):1119–27. [DOI] [PubMed] [Google Scholar]
- 15.Papadakis S, Gharib M, Hambleton J, Reid RD, Assi R, Pipe AL. Delivering evidence-based smoking cessation treatment in primary care practice. Experience of Ontario family health teams. Can Fam Physician 2014; 60 :e362–71. Available from: www.cfp.ca/content/60/7/e362.full.pdf+html. Accessed 2015 Nov 9. [PMC free article] [PubMed] [Google Scholar]
- 16.Eisenberg MJ, Filion KB, Yavin D, Belisle P, Mottillo S, Joseph L, et al. Pharmacotherapies for smoking cessation: a meta-analysis of randomized controlled trials. CMAJ 2008; 179(2): 135–44. Erratum in: CMAJ 2008; 179 (8):802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Schmelzle J, Rosser WW, Birtwhistle R. Update on pharmacologic and nonpharmacologic therapies for smoking cessation. Can Fam Physician 2008; 54 :994–9. [PMC free article] [PubMed] [Google Scholar]
- 18.Fiore MC, Jaén CR, Baker TB, Baily WC, Benowitz NL, Curry SJ, et al. Treating tobacco use and dependence: 2008 update. Clinical practice guideline. Rockville, MD: US Department of Health and Human Services, Public Health Service; 2008. [Google Scholar]
- 19.Stead LF, Hartmann-Boyce J, Perera R, Lancaster T. Telephone counselling for smoking cessation. Cochrane Database Syst Rev 2013 ;(8):CD002850. [DOI] [PubMed] [Google Scholar]
- 20.Stead LF, Buitrago D, Preciado N, Sanchez G, Hartmann-Boyce J, Lancaster T. Physician advice for smoking cessation. Cochrane Database Syst Rev 2013 ;(5):CD000165. [DOI] [PMC free article] [PubMed] [Google Scholar]