Abstract
Background
Plain packaging (PP) for tobacco products was fully implemented in Australia on 1 December 2012 along with larger graphic health warnings. Using longitudinal data from the Australian arm of the ITC Four Country Survey, we examined attitudes to the new packs before and after implementation, predictors of attitudinal change, and the relationship between support and quitting activity.
Methods
A population-based cohort study design, with some cross-sectional analyses. Surveys of Australian smokers assessed attitudes to PP at four time points prior to implementation (from 2007 to 2012) and one post-implementation wave collected (early/mid-2013).
Results
Trend analysis showed a slight rise in opposition to PP among smokers in the waves leading up to their implementation, but no change in support. Support for PP increased significantly after implementation (28.2% pre vs 49% post), such that post-PP more smokers were supportive than opposed (49% vs 34.7%). Multivariate analysis showed support either before or after implementation was predicted by belief in greater adverse health impacts of smoking, desire to quit and lower addiction. Among those not supportive before implementation, having no clear opinion about PP (versus being opposed) prior to the changes also predicted support post-implementation. Support for PP was prospectively associated with higher levels of quitting activity.
Conclusions
Since implementation of PP along with larger warnings, support among Australian smokers has increased. Support is related to lower addiction, stronger beliefs in the negative health impacts of smoking, and higher levels of quitting activity.
Introduction
The world's first legislation mandating plain packaging (PP) of tobacco products was announced in April 2010, and passed by the Australian Parliament in late 2011. Full implementation was delayed due to legal challenges until 1 December 2012. Regulations to increase the size of health warnings were also gazetted around this time with an introduction date coincident with the introduction of PP. Cigarettes in the new packaging began appearing at retailers in early October 2012, and gradually increased throughout November, with a majority of smokers using plain packs by the last few weeks before implementation.1 From full implementation on December 1, it was illegal to sell tobacco without regulated PP. It is important to document the impact of this pioneering legislation, both to assess its effect and to inform other countries considering adopting similar strategies.
The Australian measure combines the ‘Plain Packaging’ law with regulations mandating larger graphic warnings, which we describe in total as ‘standardised packaging’, as when the warnings are considered it is anything but plain. The new PP law required the removal of branding and trademarks on packs except for allowing the brand name in a standard font on any or all of the front and top and bottom surfaces. All non-warning areas except the barcode are coloured in a drab olive brown colour with the text in a light grey. The stipulated pack shape is rectangular with a flip-top lid and specified minimum and maximum sizes for pack height (85– 125 mm), width (55–82 mm) and depth (20– 42 mm). The legislation also restricts the colouring and embossing of cigarette sticks to a white or faux-cork tip and an optional α-numeric code (for industry use, and not meaningful to consumers), requiring the remainder to be plain white. In parallel, regulations under other legislation mandated an increase in graphic warning labels to 75% of the front of the pack (from 30%), 90% of the back of the pack and most of one side (see figure 1). This paper aims to explore how the new packs have been received among smokers, and whether they are associated with correlates of addiction and attitudes to quitting.
Figure 1.
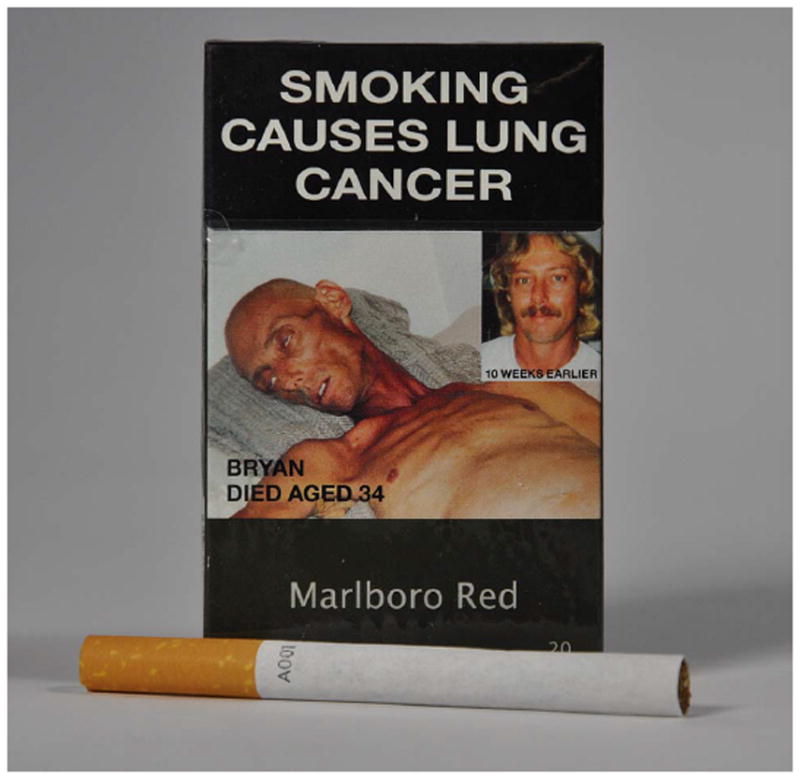
Pack with new plain packaging and stick.
One study on smokers' attitudes during the period of implementation showed that smokers already smoking from the new plain packs prior to full policy implementation were more likely to be supportive of the policy and were more interested in quitting.1 However, given the cross-sectional nature of this study, it is difficult to know whether the implementation of standardised packaging led to increased support for PP and greater interest in quitting, or whether pre-existing beliefs and/or greater interest in quitting led smokers to be more likely to choose or accept either or both aspects of the new standardised packs.
To the best of our knowledge, the only published national figures on support for PP among Australian smokers come from our ongoing ITC Australia Survey. The first time the survey asked smokers about whether they supported PP was in late 2007/early 2008, more than 2 years before the policy was announced.2 We found that 35.6% of smokers supported the policy in Australia, higher than in the USA (24.4%) and UK (27.6), but marginally lower than in Canada (37.7%). A 1992 unpublished survey found 37% of Australian smokers supporting a proposal similar to this,3 and a study in Western Australia in late 2010, about 6 months after the policy was announced but 2 years before the policy was implemented, found that 34% of smokers supported PP: only slightly lower than the percentage of smokers who opposed it (38%).4 The similarity of the level of support among smokers across these three studies suggests that support for PP among Australian smokers was fairly stable prior to implementation. What research there is shows that smokers are less supportive than non-smokers who tend to be overall net supportive.5
On the basis of research on the introduction of other tobacco control policies, we hypothesised that support for PP among smokers would increase following implementation. This pattern has been observed with smoke-free workplace policies,6 comprehensive indoor smoke-free laws, including hospitality venues such as restaurants and bars,7 across a number of countries,8 as well as for graphic health warnings9 and point-of-sale display bans on tobacco products.10 Such postimplementation support is thought to relate to the extent to which smokers can adapt to the changed circumstances,11 and also to the fact that experiences often reveal strong concerns held prior to implementation to be unfounded, or to the realisation that these new policies are actually helpful for quitting.
The current study took advantage of the longitudinal design of the ITC Survey conducted in Australia to examine how levels of support for PP among Australian smokers prior to the implementation of PP changed after its implementation. We conducted longitudinal analyses to explore factors associated with support post-PP and with changes in support. Finally, we explored whether a supportive attitude post-PP was associated with increased interest in quitting.
Method
Sample
The study used Australian data from the five most recent waves of the ITC Four Country Survey (2007–2013). Minimum eligibility criteria for trend analyses required participants to be currently smoking at least once a month, with a valid response to the question on support of plain packaging. The four pre-PP surveys were conducted from September 2007–February 2008 (n=1778), October 2008–March 2009 (n=1346), July 2010–May 2011 (n=1097) and September 2011–February 2012 (n=1093), with the post-PP survey from February 2013–May 2013 (n=1070). Additional predictive analyses required participants to have valid responses on all included variables, with exclusions made on a case-by-case basis (online supplementary table S1). Finally, the predictive analyses involving the post-PP wave also included smokers who had quit since the last pre-PP survey (n=112). Characteristics of the last pre-PP and post-PP samples are presented in table 1.
Table 1. Participant characteristics preimplementation and postimplementation of plain packaging (PP).
| Pre-PP (smokers only) | Present at pre-PP and post-PP (figures are pre-PP)* | Post-PP (smokers and recent ex-smokers) | |
|---|---|---|---|
| N | 1093 | 773 | 1182 |
| Per cent female | 54.4 | 54.0 | 53.6 |
| Age (% years) | |||
| 18–24 | 2.8 | 2.7 | 1.9 |
| 25–39 | 19.3 | 17.3 | 16.1 |
| 40–54 | 42.5 | 43.1 | 39.5 |
| 55 or older | 35.4 | 36.9 | 42.6 |
| Socioeconomic status (%) | |||
| Low | 42.5 | 44.8 | 46.3 |
| Moderate | 29.3 | 28.7 | 27.6 |
| High | 28.1 | 26.4 | 26.1 |
| Per cent ex-smokers | |||
| Pre-PP | 0.0 | 0.0 | 3.6 |
| Post-PP* | — | 14.5 | 9.5 |
| Mode Pre-PP | |||
| Web | 38.3 | 43.9 | — |
| Phone | 61.7 | 56.2 | — |
| Mode Post-PP | |||
| Web | — | 56.7 | 50.9 |
| Phone | — | 43.3 | 49.2 |
| Time in sample | |||
| Recontacted | 75.5 | 70.0 | 67.9 |
| New recruit | 24.5 | 20.1 | 32.2 |
The pre-PP survey occurred between September 2011 and February 2012, whereas the post-PP survey occurred between February 2013 and May 2013.
The middle column presents pre-PP data for those participants who were smoking pre-PP and were also present at follow-up, post-PP. A proportion of these smokers had quit post-PP, and this is reflected in the row % ex-smokers post-PP
Procedures
The ITC Four Country Survey is a longitudinal survey of a nationally representative cohort of smokers in the USA, Canada, the UK and Australia. This paper only reports data from Australia. Samples are recruited through random digit dialling (RDD) procedures, and replenished via the same procedure at each wave to replace those lost at follow-up. All participants are current smokers (at least monthly; factory made or roll-your-own cigarettes) at recruitment, but are retained in the cohort if they subsequently quit. A detailed description of the ITC methodology can be found elsewhere.12 13 This means that the sample of ex-smokers only includes relatively recent quitters (up to 10 years) and over-represents those who have quit more recently. From 2010, participants could complete the survey either online or through computer-assisted telephone interviewing, although they were all recruited via the same RDD telephone sampling methods.
Measures
For the primary outcome, participants were asked to give an opinion (strongly agree/agree, neither agree nor disagree, or disagree/ strongly disagree) to a statement on plain packs. In the pre-PP waves, this was ‘Tobacco companies should be required to sell cigarettes in plain packages—that is, in packs without the usual brand colours and symbols, but keeping the warning labels’, while in the 2013 post-PP wave ‘Tobacco companies should continue to be required to sell cigarettes in plain packages, as they are now’.
Other measures included gender, age group (18–24, 25–39, 40–54, 55+), socioeconomic status (SES: low, medium or high; based on a combination of income and education, or where income was not disclosed, education alone). Smoking-related variables used for predictive analyses and all measured in the last pre-PP wave included: the Heaviness of Smoking Index (HSI)14; current smoking status at each wave (smoker/ex-smoker); desire to quit (‘how much do you want to quit?’ :not at all, a little, somewhat, a lot); quitting history (none versus at least one quit attempt: since the last survey/in the last year for new recruits), with being currently quit at the time of the interview constituting a quit attempt; quitting self-efficacy (‘If you decided to give up smoking completely in the next 6 months, how sure are you that you would succeed?’ :not at all sure, slightly sure, moderately sure, very sure, extremely sure); and proximity of intention to quit (no intention or beyond 6 months/within the next 6 months). Three measures of health were also included: overall health (described as poor, fair, good, very good, excellent); perceived risk of disease (‘if you continue to smoke as much as you do now, what are the chances that you will get a smoking-related disease, such as lung cancer, heart disease, or emphysema?’ :very high, somewhat high, neither high or low, somewhat low, very low); and realised health damage (‘To what extent, if at all, has smoking damaged your health?’ :not at all, just a little, a fair amount, a great deal). We also controlled for survey mode (telephone or web) and time in sample (followed-up cohort or new recruit).
For our categorical variables, we combined subcategories for any variables where response rates were small (under 10%), with the proviso that combined categories be contiguous and logically appropriate. For example, responses to the question ‘to what extent, if at all, has smoking damaged your health?’ were: not at all 14.4%, just a little 49.6%, a fair amount 28.6% and a great deal 7.4%, so we combined a fair amount and a great deal into one category (35.9%). The specific combinations are detailed within our tables of results.
For our analyses using pre-PP support to predict subsequent quitting activity, we calculated the recency of participants' last quit attempt (whether failed or still current) based on the question ‘When did your most recent (or current) quit attempt start?’ We stratified responses to within the past 6 months versus over 6 months ago.
Analyses
Predictive analyses focus on the last two waves, with responses at the 2011/2012 wave (pre-PP wave) used to predict attitudes both pre-PP and post-PP, as well as changes in attitudes among those originally not supportive. Associations were measured using multivariate regression with plain packaging support as a continuous outcome, compared across demographics and smoking-related variables. Preliminary analyses showed demographic and outcome differences across survey mode; therefore, we control for survey mode where relevant. We also control for time in sample where relevant. All our trend analyses were weighted for population percentages according to our sampling frame. The within-wave analyses were restricted to current smokers, but in the longitudinal predictive analyses between the pre-PP and post-PP waves follow-up cases were included regardless of smoking status to provide a broader picture of the change in support among smokers initially opposed. Our baseline samples for predictive analyses were always restricted to current smokers because many of our key predictors (eg, desire to quit, quitting self-efficacy and HSI) were not applicable to and therefore not asked of ex-smokers. Finally, predictors of change to increased support post-PP from those not supportive pre-PP were analysed using multivariate regression, including demographics, smoking and health-related variables from thelast pre-PP wave.
We examined the response profile of our missing sample (any participants excluded from multivariate analyses due to data missing on one or more variables) on all variables for which they had data, and observed that all were missing at random, with the exception of the desire to quit variable. For this variable, excluded participants were more likely to express no opinion and less likely to express support for plain packs pre-PP than those included in the final multivariate analyses χ2(4)=15.4, p<0.005. We therefore conducted analyses including these participants as a ‘missing’ dummy category on the desire to quit variable to assess their impact on our outcome. There were no significant effects of this category OR=1.33, 95% CI 0.87 to 2.03, p=0.18 on support, and none of the effects reported below were altered due to its inclusion, so we only report the analyses where these participants were excluded.
Results
Demographic characteristics of the samples from the last pre-PP and post-PP waves are presented in table 1. At both waves, smokers who responded online were less likely to be in the oldest age group (pre-PP χ2(3)=18.2, p<0.001; post-PP χ2(3)=21.3, p<0.001), reported higher SES (pre-PP χ2(2)=21.2, p<0.001; post-PP χ2(2)=54.9, p<0.001), and were more likely to be from the recontact sample (pre-PP χ2(1)=220.7, p<0.001; post-PP χ2(1)=27.5, p<0.001). No gender or HIS differences were found across mode at either wave.
Support for the new packaging
Figure 2 shows trends in support and opposition to plain packaging over time. Both support and opposition are reported as they changed differently due to changes in the percentages of smokers who gave neutral or no opinions. Analyses revealed a survey mode effect, with telephone responders showing greater support at both waves (pre-PP OR=1.24, 95% CI 1.07 to 1.43, p<0.01; post-PP OR=1.49, 95% CI 1.30 to 1.72, p<0.001), largely because the web-respondents were more likely to choose the neutral category.
Figure 2.
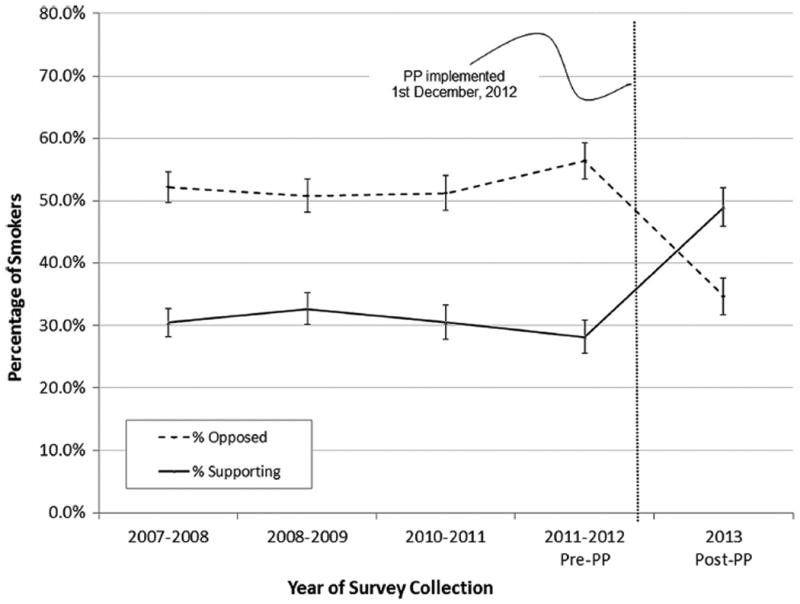
Trends in current smokers' support and opposition to plain packaging. Data are weighted for sampling frame, and represent means adjusted for survey mode through generalised estimating equations modelling.
Controlling for survey mode and time in sample, the support for PP increased markedly from a period of around a year prior to implementation to a period of 3–7 months post full implementation. Preimplementation, 28.2% of smokers supported PP (strongly agree or agree) and 56.4% were opposed (strongly disagree or disagree), while post-PP support rose to 49% and only 34.7% were opposed. Among those who participated in both waves, 47.7% increased their support, while only 19.9% showed lower levels of support, the remainder being stable.
Multivariate analysis of predictors of support for PP, both pre-PP and post-PP, among respondents who were smokers pre-PP are shown in table 2; these analyses control for mode of survey and cohort. The pattern of findings for predictors of support was similar at the two waves. Gender, SES and age group were not clearly related to PP support at either wave.
Table 2. Factors pre-PP predicting plain packaging support preimplementation and postimplementation, plus predictors of support post-PP among those not originally supportive.
| Predictors of level of support, pre-PP OR (95% CI) | Pre-PP predictors of post-PP level of support OR (95% CI) | Predictors of change in support from non-support, for those in pre-PP wave OR (95% PI) | |
|---|---|---|---|
| N | 1037 | 732 | 535 |
| Gender | |||
| Female | REF | REF | REF |
| Male | 1.20* (1.04 to 1.39) | 0.95 (0.80 to 1.12) | 0.69 (0.46 to 1.05) |
| Age in years | |||
| 18-24 | 0.73 (0.46 to 1.14) | 0.66 (0.39 to 1.13) | 0.69 (0.19 to 2.55) |
| 25-39 | 0.91 (0.73 to 1.13) | 0.81 (0.63 to 1.04) | 0.60 (0.33 to 1.11) |
| 40-54 | 0.92 (0.78 to 1.09) | 1.00 (0.83 to 1.21) | 0.75 (0.47 to 1.20) |
| 55+ | REF | REF | REF |
| SES | |||
| Low | REF | REF | REF |
| Medium | 0.78** (0.65 to 0.93) | 0.89 (0.72 to 1.09) | 0.88 (0.53 to 1.45) |
| High | 0.89 (0.74 to 1.08) | 0.90 (0.72 to 1.11) | 1.06 (0.62 to 1.81) |
| Pre-PP want to quit? | |||
| Not at all | REF | REF | REF |
| A little | 1.03 (0.77 to 1.37) | 1.27 (0.91 to 1.75) | 1.60 (0.70 to 3.64) |
| Somewhat | 1.52** (1.19 to 1.95) | 1.32* (1.004 to 1.75) | 2.05 (0.997 to 4.21) |
| A lot | 1.71*** (1.32 to 2.20) | 1.56** (1.17 to 2.08) | 2.20* (1.05 to 4.59) |
| Recent QA at outcome wave | |||
| No | REF | REF | REF |
| Yes | 1.07 (0.91 to 1.26) | 1.04 (0.86 to 1.28) | 1.20 (0.74 to 1.94) |
| Self-rated health pre-PP | |||
| Poor | REF | REF | REF |
| Fair | 1.09 (0.80 to 1.48) | 0.90 (0.61 to 1.31) | 0.58 (0.23 to 1.46) |
| Good | 1.10 (0.81 to 1.50) | 1.03 (0.71 to 1.50) | 0.80 (0.32 to 1.95) |
| Very good/excellent | 1.18 (0.85 to 1.64) | 1.06 (0.71 to 1.57) | 0.81 (0.31 to 2.11) |
| Disease risk if keep smoking | |||
| Very high | REF | REF | REF |
| Somewhat high | 0.84 (0.70 to 1.02) | 0.82 (0.65 to 1.03) | 0.84 (0.48 to 1.45) |
| Neither | 0.73* (0.58 to 0.94) | 0.60*** (0.46 to 0.79) | 0.43* (0.22 to 0.84) |
| Somewhat/very low | 0.77 (0.56 to 1.07) | 0.63* (0.42 to 0.93) | 0.89 (0.33 to 2.41) |
| Smoking has damaged your health | |||
| Not at all | REF | REF | REF |
| Just a little | 0.93 (0.73 to 1.18) | 0.98 (0.75 to 1.27) | 1.19 (0.59 to 2.39) |
| A fair amount/a great deal | 1.06 (0.81 to 1.39) | 1.13 (0.83 to 1.53) | 1.69 (0.77 to 3.71) |
| Pre-PP self-efficacy | |||
| Not at all sure | REF | REF | REF |
| Slightly sure | 1.19 (0.96 to 1.46) | 1.07 (0.85 to 1.36) | 0.89 (0.49 to 1.62) |
| Moderately sure | 0.96 (0.80 to 1.15) | 1.07 (0.87 to 1.31) | 0.98 (0.60 to 1.62) |
| Very/extremely sure | 0.84 (0.66 to 1.07) | 0.82 (0.61 to 1.09) | 1.04 (0.52 to 2.09) |
| Pre-PP HIS | |||
| Low | REF | REF | REF |
| Medium | 0.78** (0.65 to 0.94) | 0.78* (0.63 to 0.96) | 0.81 (0.49 to 1.36) |
| High | 0.67*** (0.54 to 0.82) | 0.65*** (0.51 to 0.82) | 0.54* (0.30 to 0.97) |
| Post-PP Smoking Status | |||
| Ex-smoker | REF | REF | |
| Smoker | 0.84 (0.64 to 1.10) | 0.70 (0.37 to 1.32) | |
| Pre-PP Opinion | |||
| Opposed | REF | ||
| Neutral | 1.90** (1.19 to 3.01) |
p<0.05;
p<0.01;
p<0.001
The pre-PP survey occurred between September 2011 and February 2012, whereas the post-PP survey occurred between February 2013 and May 2013.
HSI, Heaviness of Smoking Index; PP, plain packaging; SES, socioeconomic status.
Those with a stronger desire to quit were more likely to be supportive of PP, as were those with low scores on the HSI, and those who believed they were at high risk of future smoking-related harms. However, support for PP was unrelated to having already experienced smoking-related harm or to the smoker's overall health assessment.
Essentially the same factors were also related to changes in support for PP: the only hint of a difference was that those who held intermediate views on future risks were least likely to become more supportive. In addition, and unsurprisingly, those who were previously neutral were more likely to become supportive than those initially opposed (see table 2).
We now turn to the relationship between support and subsequent quit activity. At both the immediate pre-PP and post-PP waves, those who were supportive of PP were more likely to intend to quit in the future (OR=1.78, 95% CI 1.35 to 2.35, N=1056 and OR=1.68, 95% CI 1.28 to 2.20, N=955, respectively), and those at the pre-PP wave who were supportive were more likely to make quit attempts in the 6 months before the post-PP wave (OR=1.51, 95% CI 1.07 to 2.11, N=732), but there were insufficient cases to explore any impact on the duration of attempts.
Discussion
Support for PP increased significantly among Australian smokers after implementation of the law. We cannot tell whether this was just related to the PP rules or was also influenced by the changes to the warnings, that is, if it was a response to the total standardised packaging initiative. A substantially greater percentage of smokers now support PP than oppose it, whereas the opposite was true before PP was introduced. Moreover, smokers who support the policy were more interested in quitting and were more likely to make quit attempts in the months following implementation. The finding that around half of the smokers actively support the policy is evidence of its broad acceptability among smokers. It should be noted that support among nonsmokers is likely to be considerably higher.5
Current health status, in terms of both self-reported health and whether smoking had already damaged the smoker's health, was not related to PP support. However, strength of addiction and concern about future health harms from smoking both predicted post-PP support. It is notable that it is future concerns, rather than current health status, that were related to support for PP. Being opposed to restrictions on something for which you underestimate the harms is a rational response, making it plausible that this relationship is causal. The argument for a causal relationship is strengthened by the finding that future concerns are also related to increases in support.
The finding that support for PP was related to subsequent quitting attempts, and the similar-sized association of intentions pre-PP to post-PP, suggests that there may exist a small positive tendency for PP to encourage more cessation attempts, or that opposition to PP leads to a reduced interest in quitting. Alternatively, it could be that interest in quitting motivates greater support without contributing to attempts. A possible mechanism for a positive causal role comes from the experimental research indicating that PP enhances warning label effects,15 which means that it could enhance negative evaluations of smoking and thus more strongly motivate quitting activity. However, we should stress that it is beyond the capacity of this study, and potentially any reasonably sized study, to directly demonstrate a small increase in quitting activity, as PP is only one of a number of theorised influences. Further, if such an effect exists, it is more likely to be with less addicted smokers who are predominantly those young people who have not developed long-term dependence. Unfortunately, the ITC cohort under-represents this group, so we are not in a position to explore what is happening within this important subgroup of the smoking population.
The mode of survey effect requires some discussion since it was related to responses on the question about support for the law. The survey mode effects observed may be due in part to the characteristics of those choosing the internet over phone surveying, although we feel it is most likely also due to the survey mode itself. Online respondents were much more likely not to express an opinion (choosing the ‘neither agree nor disagree’ or ‘don't know’ category). This is a response pattern that has been reported in similar attitudinal questions in other ITC countries,16 and is most likely at least partly due to the ‘don't know’ option not being read out in phone interviews, but being an explicit option in the web version. We have controlled for the mode differences in the analyses of correlates of support and changes in support. The main limitation that remains with mode is the difficulty it creates in providing a simple overall estimate of the level of support. Internet administration may reflect a more accurate reflection of smokers' beliefs as there is evidence of less social desirability when not responding to a person.17 It is also possible that the difference to the wording of the question about support for PP from pre-implementation to post-implementation acknowledging that it was implemented post-PP may have impacted on the responses; however, we would expect any such effect to be small, as it really only more accurately contextualised the question, and are confident in attributing the changes in support to the implementation of the policy rather than the wording of the questions. Apart from this, the study is subject to many of the inevitable limitations of survey research. Even with the prospective analyses, caution should be exercised in attributing causation.
Since the Australian announcement of PP, there has been interest in other countries for similar laws. Our findings indicate that it is likely that the implementation of such a policy would come to be accepted by smokers in other countries, as where studied, attitudes have not differed markedly from Australia and, at least among smokers, have also been mildly negative.5 18 19 Youth have also been found to support PP and to believe that it would reduce youth uptake,20 21 and it is among the youth that PP is most likely to have a protective effect.
Conclusion
Support for PP has greatly increased among Australian smokers since the implementation of the policy, with now only a minority of smokers remaining opposed, although we cannot be sure as to what extent this is a response to the total standardised packaging initiative rather than just to the PP aspect. Opposition mainly comes from those who smoke heavily and those who underestimate the risks. Support is also associated with higher levels of quitting activity.
What this paper adds.
This paper is the first to report that support for the new standardised (plain) cigarette packs increased among a national sample of Australian smokers following their implementation in Australia on 1 December 2012. It shows that smokers increasingly come to accept plain packaging following its implementation.
Acknowledgments
The authors would like to thank members of the Data Management Core at the University of Waterloo for assistance in preparing the data for this analysis.
The ITC Four Country Survey is supported by multiple grants including R01 CA100362, P50 CA111236 (Roswell Park Transdisciplinary Tobacco Use Research Centre), P01 CA138389 (Medical University of South Carolina), P30 CA138313 (Hollings Cancer Center Support Grant, Medical University of South Carolina), all funded by the National Cancer Institute of the USA, Robert Wood Johnson Foundation (045734), Canadian Institutes of Health Research (57897, 79551), National Health and Medical Research Council of Australia (265903, 450110, APP1005922), Cancer Research UK (C312/A3726), Canadian Tobacco Control Research Initiative (014578); Centre for Behavioural Research and Program Evaluation, National Cancer Institute of Canada/Canadian Cancer Society. KMC has served in the past and continues to serve as a paid expert witness for plaintiffs in litigation against the tobacco industry. GTF and JFT have each served as a paid expert witness or consulting expert for governments in countries whose policies are being challenged by parties under trade agreements. DH has served as an expert witness on behalf of national governments in legal challenges to packaging regulations, as well as an advisor to regulatory agencies for tobacco packaging policies. RB was a member of an expert advisory committee that advised the Australian government on the research carried out to support the introduction of the plain packaging legislation.
Footnotes
Contributors: RB conceived the study design and drafted the manuscript. ES assisted with the study design, conducted statistical analyses and drafted the manuscript. KMC, GTF, JFT, AM and DH provided theoretical guidance and edited the manuscript. H-HY provided high-level statistical advice and edited the manuscript, and TRP conducted literature reviews, provided statistical analyses and edited the manuscript. All approved the final version.
Competing interests: All remaining authors declare that they have no conflicts of interest.
Ethics approval : All waves of the study have received ethical approval from the relevant institutional review board or research ethics committee at The Cancer Council Victoria (Australia), Roswell Park Cancer Institute (USA), University of Waterloo (Canada) and University of Strathclyde (UK).
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Wakefield MA, Hayes L, Durkin S, et al. Introduction effects of the Australian plain packaging policy on adult smokers: a cross-sectional study. BMJ Open. 2013;3:e003174. doi: 10.1136/bmjopen-2013-003175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Moore K, Borland R, Yong HH, et al. Support for tobacco control interventions: do country of origin and socioeconomic status make a difference? Int J Public Health. 2012;57:777–86. doi: 10.1007/s00038-012-0378-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.CBRC. Public approval of proposed tobacco pack labelling and other modifications. Centre for Behavioural Research in Cancer. [accessed Jul 2014];Supplement to: Health warnings and contents labelling of tobacco products (unpublished report) 1992 http://legacy.library.ucsf.edu/tid/cze1978e1900.
- 4.Rosenberg M, Pettigrew S, Wood L, et al. Public support for tobacco control policy extensions in Western Australia: a cross-sectional study. BMJ Open. 2012;2:e000784. doi: 10.1136/bmjopen-2011-000784. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Moodie C, Stead M, Bauld L, et al. Plain tobacco packaging: a systematic review Institute of Education. University of London; 2012. [Google Scholar]
- 6.Borland R, Chapman S, Owen N, et al. Effects of workplace smoking bans on cigarette consumption. Am J Public Health. 1990;80:178–80. doi: 10.2105/ajph.80.2.178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Fong GT, Hyland A, Borland R, et al. Reductions in tobacco smoke pollution and increases in support for smoke-free public places following the implementation of comprehensive smoke-free workplace legislation in the Republic of Ireland: findings from the ITC Ireland/UK survey. Tob Control. 2006;15(Suppl 3):iii51–8. doi: 10.1136/tc.2005.013649. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Thrasher JF, Abad-Vivero EN, Sebrie EM, et al. Tobacco smoke exposure in public places and workplaces after smoke-free policy implementation: a longitudinal analysis of smoker cohorts in Mexico and Uruguay. Health Policy Plan. 2013;28:789–98. doi: 10.1093/heapol/czs118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Shanahan P, Elliott D. Evaluation of the effectiveness of the graphic health warnings on tobacco product packaging 2008. Canberra: Australian Government Department of Health and Ageing; 2009. [Google Scholar]
- 10.McNeill A, Lewis S, Quinn C, et al. Evaluation of the removal of point-of-sale tobacco displays in Ireland. Tob Control. 2011;20:137–43. doi: 10.1136/tc.2010.038141. [DOI] [PubMed] [Google Scholar]
- 11.Borland R, Owen N, Hill D, et al. Regulatory innovations, behaviour and health: Implications of research on workplace smoking bans. In: Maes S, Leventhal H, Johnston M, editors. International review of health psychology. Chichester: John Wiley & Sons Ltd; 1994. pp. 167–85. [Google Scholar]
- 12.Fong GT, Cummings KM, Borland R, et al. The conceptual framework of the International Tobacco Control (ITC) policy evaluation project. Tob Control. 2006;15:iii3–11. doi: 10.1136/tc.2005.015438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thompson M, Fong GT, Hammond D, et al. Methods of the International Tobacco Control (ITC) Four Country Survey. Tob Control. 2006;15:iii12–18. doi: 10.1136/tc.2005.013870. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Heatherton TF, Kozlowski LT, Frecker RC, et al. Measuring the heaviness of smoking: using self-reported time to the first cigarette of the day and number of cigarettes smoked per day. Brit J Addict. 1989;84:791–800. doi: 10.1111/j.1360-0443.1989.tb03059.x. [DOI] [PubMed] [Google Scholar]
- 15.Gallopel-Morvan K, Moodie C, Hammond D, et al. Consumer perceptions of cigarette pack design in France: a comparison of regular, limited edition and plain packaging. Tob Control. 2012;21:502–6. doi: 10.1136/tobaccocontrol-2011-050079. [DOI] [PubMed] [Google Scholar]
- 16.Nagelhout GE, Willemsen MC, Thompson ME, et al. Is web interviewing a good alternative to telephone interviewing? Findings from the International Tobacco Control (ITC) Netherlands survey. BMC Public Health. 2010;10:351. doi: 10.1186/1471-2458-10-351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kreuter F, Presser S, Tourangeau R. Social desirability bias in CATI, IVR, and Web surveys: the effects of mode on question sensitivity. Public Opinion Q. 2008;72:847–65. [Google Scholar]
- 18.Arora M, Tewari A, Grills N, et al. Exploring perception of Indians about plain packaging of tobacco products: a mixed method research. Front Public Health. 2013;1:35. doi: 10.3389/fpubh.2013.00035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hoek J, Gendall P, Maubach N. Strong public support for plain packaging of tobacco products. Aust N Z J Public Health. 2012;36:405–7. doi: 10.1111/j.1753-6405.2012.00907.x. [DOI] [PubMed] [Google Scholar]
- 20.Hoek J, Healey B, Gendall P, et al. How do adolescents perceive plain packaging? N Z Med J. 2013;126:100–3. [PubMed] [Google Scholar]
- 21.Smith A, McCool J, Paynter J, et al. Youth opinions of tobacco control in New Zealand: support for specific measures and the relationship with smoking behaviors among 14–15-year-olds. Nicotine Tob Res. 2012;14:479–785. doi: 10.1093/ntr/ntr239. [DOI] [PubMed] [Google Scholar]


