Abstract
Most of the implants used for total knee arthroplasty (TKA) in Asian patients have been produced based on anthropometry of Western people. Since anatomic features and life styles are different between Western and Eastern people, there would be ethnic differences in terms of conformity of implants to the patient's anatomy or clinical results after TKA. Therefore, surgeons in Asia are particularly interested in related surgical techniques and implant designs used in TKA for improved clinical results and patient satisfaction. In this review, we investigated the anthropometric differences of Koreans from Westerners. Koreans are of shorter stature, less weight, and smaller skeletal structure and have a higher incidence of constitutional varus alignment of the lower extremity. Moreover, compared to Westerner TKA populations, the proportion of female patients was large and primary osteoarthritis was prevalent in preoperative diagnosis in Korean TKA patients. Culturally, Koreans have life styles that demand high flexion positions of the knee such as squatting, kneeling, and cross-legged sitting. Although there were no notable differences in the complication and revision rates following TKA between Westerners and Koreans, the incidence of postoperative deep vein thrombosis and pulmonary thromboembolism was lower in Koreans than Westerners. We hope that further research on implant designs and more interest in TKA will improve outcomes in Korean patients.
Keywords: Knee, Arthroplasty, Korean, Ethnic difference
Introduction
In total knee arthroplasty (TKA), it has been the norm for orthopedic surgeons in Asia to utilize in their patients the same knee implants and surgical techniques designed for Western populations. Recently, however, there are increasing interests in the development of new implant designs and surgical approaches that can better accommodate Asian patients with lifestyles and anthropometric characteristics different from Western patients for, at least theoretically, more favorable clinical outcomes and higher satisfaction1,2,3,4,5). In this review, we will summarize physical characteristics of Korean patients such as relatively small stature/bone structure and high prevalence of varus deformity compared to Westerners4,5,6), and clinical studies concerning knee implants that allow for high flexion activities of squatting and kneeling. Furthermore, we will discuss modes of failure after TKA and revision rates reported in Korean and Western research.
1. Demographic Differences
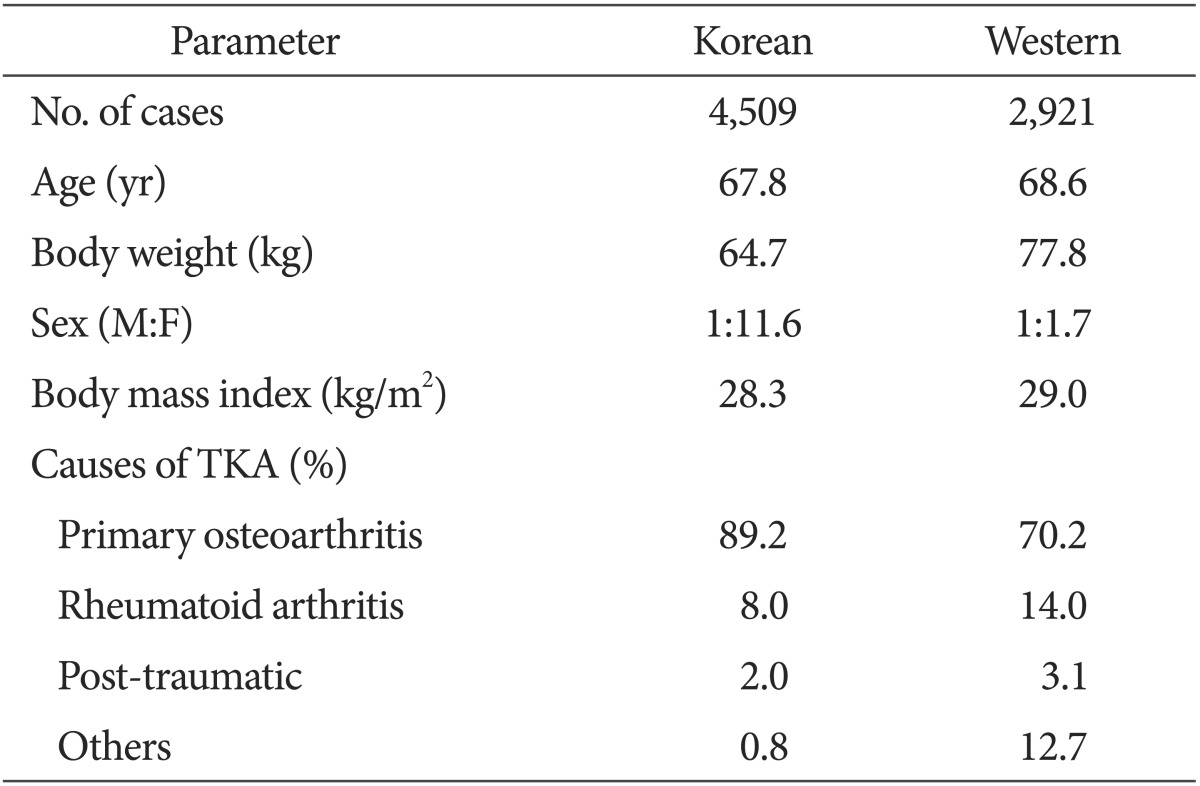
Compared to other races, especially Westerners, Korean patients with TKA have two distinctive demographic characteristics: considerably high female proportion and relatively light weight7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22,23). On the other hand, no significant difference was found in body mass index due to the proportionately short stature of Koreans (Table 1). The comparatively high female proportion has led to substantial interest in gender-specific knee implant designs in Korea as supported by various studies24,25). In a met-analysis, Cheng et al.24) observed no statistically significant difference between the standard unisex prostheses and gender-specific prostheses with regard to range of motion (ROM), clinical knee scores, satisfaction, and pain. In particular, gender-specific prostheses were found to have less overall femoral component coverage. In the knees with unisex prostheses, the femoral component closely matched the resected bone surface in 56%, was overhung in 13%, and undercovered the bone surface in 31%. The female-specific prostheses had a close fit in 25% and undercoverage in 75%. In a more recent study, Kim et al.25) reported that there was no significant difference between the traditional implant and the gender-specific implant in terms of the postoperative flexion contracture (0.4° vs. 0.3°), maximal flexion (130.6° vs. 129.6°), ROM (130.2° vs. 129.3°), and Hospital for Special Surgery score (90.8 points vs. 91.0 points); however, the overhang incidence was remarkably low in the knees with a gender-specific prosthesis compared to those with a traditional prosthesis (25.0% vs. 59.6%). In summary, studies have failed to demonstrate significant differences between traditional knee implants and gender-specific implants in female patients who comprise most of the TKA population in Korea. Although it is too early to draw definitive conclusions, these studies may indicate the surgeon's experience or capability is a more important determinant of TKA outcomes. On the indications for surgery, TKA was required in Western patients due to primary degenerative arthritis in 70.2%, rheumatoid arthritis in 14.0%, and others in 12.7%, whereas Korean TKA patients had primary degenerative arthritis in 89.2%, rheumatoid arthritis in 8.0%, and traumatic arthritis in 2.0%, indicating primary degenerative arthritis is more common in Korean TKA patients (Table 1).
Table 1. Summary of Demographic Factors.
TKA: total knee arthroplasty.
2. Anatomical Differences
Anthropometric features are important factors that should be taken into consideration in the improvement of implant designs and surgical techniques. Selection of a proper implant that matches the patient's anthropometric features is essential to successful outcome of TKA; gap balance, patellofemoral kinematics, implant fixation, and soft tissue tension are all influenced by implant selection, which is also associated with the risk of complication and implant stability and longevity26,27,28). Most of the contemporary knee implants available in Korea are optimized for anthropometrical features of Western patients, hence the increased risk of overhang/underhang, unstable implant fixation, physical irritation, and ROM restriction. Therefore, a clear understanding of anthropometric features of the knee joint of Koreans is of utmost importance for the development of knee prostheses and advancement of surgical techniques.
1) Anthropometric features of the femur
Anthropometric features of the femur are crucial factors for the improvement of implant designs and surgical techniques. In a Korean study, Chung et al.29) described the mean condylar anteroposterior height as 67.2 mm for males and 61.1 mm for females, the mean condylar mediolateral width as 76.1 mm for males and 67.9 mm for females, and the mean trochlear width as 51.0 mm for males and 46.4 mm for females. The mean ratios of the condylar width and trochlear width to the condylar anteroposterior height (aspect ratio: mediolateral/anteroposterior ratio) were reported as 1.13 and 0.76, respectively, in males and 1.11 and 0.76, respectively, in females. Lonner et al.26) collected femoral anthropometric features from American patients undergoing TKA: the mean condylar anteroposterior height was 70.0 mm in males and 63.3 mm in females; the mean condylar mediolateral width was 77.0 in males and 67.5 in females; the mean trochlear width was 56.3 mm in males and 48.9 mm in females; and the mean condylar aspect ratio was 1.23 in males and 1.20 in females. These studies show that the overall size of the femur and the femoral aspect ratio are smaller in Koreans than in Westerners.
2) Anthropometric features of the proximal tibia
Proper tibial component sizing is closely associated with implant stability and survival rate of TKA30). Kwak et al.31) reported that the middle anteroposterior length of the proximal tibia was an average of 48.2 mm for males and 43.2 mm for females, and the mediolateral length of the proximal tibia averaged 76.1 mm for males and 67.6 mm for females in Korean cadaveric knees. Mensch and Amstutz32) measured mediolateral length of the proximal tibia on American cadaveric knees, which was an average of 89.3 mm for males and 70.1 mm for females. Westrich et al.30) reported that the mean anteroposterior length of the proximal tibia in American patients was 42.9 mm. According to these studies, Koreans appear to have relatively small anteroposterior and mediolateral lengths of the proximal tibia compared to Westerners.
3) Anthropometric features of the patella
The size and thickness of the patella, height/width ratio, and relative position of the median ridge have implications for selection of the patellar component size, patellofemoral contact stress, and patellar tracking33). In a Korean study by Kim et al.34), the mean thickness at central ridge of the patella was 23.1 mm in males and 21.2 mm in females and the mean mediolateral width was 45.6 mm in males and 41.0 mm in females; and the mean superoinferior height was 36.2 mm in males and 33.1 mm in females. In an American study by Baldwin and House35), the mean thickness at central ridge was 23.9 mm in males and 21.8 mm in females; the mean mediolateral width was 49.5 mm in males and 42.7 mm in females; and the mean superoinferior height was 39.4 mm in males and 35.0 mm in females. Chmell et al.36) documented English and American patient data on the patella: the mean thickness at central ridge was 26.1 mm for males and 22.6 mm for females. These studies show that Koreans have thinner and smaller patellae than Westerners.
3. Body Feature Differences
1) Constitutional varus alignment of the lower limb
Constitutional varus alignment can be defined as the hip-knee-ankle angle of -3° or less after attainment of skeletal maturity37). Bellemans et al.37) investigated the incidence of constitutional varus knees in Caucasians who were between 20 to 27 years of age and had reached skeletal maturity. In the study, constitutional varus alignment was observed in 24.6% of the total subjects (32% in males and 17.2% in females). The mean hip-knee-ankle angle was measured as -1.87°±2.42° for males and -0.79°±2.13° for females. In a study by Shetty et al.38), the incidence of constitutional varus alignment was documented as 35% in Koreans, 34% in Indians, and 24.5% in Caucasians. Therefore, when compared to Westerners, varus knee alignment is relatively prevalent among Koreans. In TKA, restoration of neutral mechanical alignment where the weight-bearing axis passes through the center of the knee has been considered as a key determinant of long-term implant survival9,21,22). In order to obtain neutral mechanical alignment in patients with constitutional varus knees (≤3° varus alignment29)), a great extent of medial soft tissue release has been considered unavoidable4,37). However, Magnussen et al.39) described that residual varus deformity after TKA had no adverse effect on the 10-year survival rate and the International Knee Society score at a mean of 4.7 years after TKA in 553 patients. Parratte et al.40) compared the revision rate at 15 years after TKA between a group with a postoperative limb alignment of 0°±3° and an outlier group, which showed know no significant intergroup difference. Based on the review of these studies, it would be reasonable to assume that the extent of correction can be adjusted during TKA according to the patient's inherent anatomical characteristics in knees with constitutional varus alignment. However, it is practically impossible to estimate the extent of inherent varus alignment at the time of TKA in patients with deformity; therefore, we think that the surgeon's experience will play a key role in such cases.
2) Femoral lateral bowing, varus condylar orientation, and varus tibia plateau inclination
Coronal alignment has been considered closely related to the implant function and survival rate after TKA5,40). In Asian TKA candidates, it is not difficult to encounter anatomical variations that can affect the coronal alignment, such as severe lateral bowing of the femur, varus femoral condylar orientation, and varus inclination of the tibial plateau5,41), which often requires additional surgical procedures during TKA. These anatomical variations appear to be common in Korean female TKA patients according to Lasam et al.5): lateral bowing of the femur was present in 88% in the TKA group and in 77% in the control group; the mean femoral condylar orientation angle was varus 2.6° in the TKA group and valgus 1.1° in the control group; and the mean inclination of the tibial plateau was varus 8.3° in the TKA group and varus 5.4° in the control group. It can be conjectured that the prevalence of such anatomical variations is expected to be lower in Western populations; however, it is difficult to make quantitative comparison due to the lack of measurement data on femoral bowing angle and femoral condylar orientation in Western patients5).
4. Lifestyle Differences
Most of the contemporary TKA prostheses and surgical techniques are designed to facilitate 120°-130° knee flexion. In Korea where squatting, kneeling, and cross-legged sitting are activities of daily living due to cultural and religious reasons, the desirable range of flexion is 111°-165°42). Therefore, compared to Western countries, restoration of the ability to perform a greater range of flexion should be taken into consideration in TKA in Korea.
1) High-flexion TKA
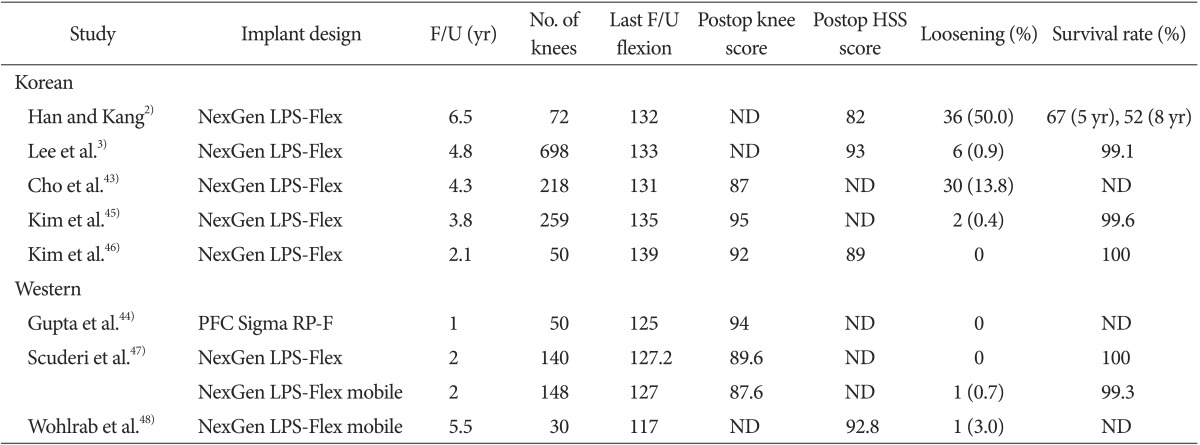
The long-term survivorship of TKA in Korean patients is relatively superior3). However, from the patient's perspective, the success of TKA is determined by the ability to perform and maintain preoperative level of high-flexion activities. Maximum flexion after TKA is dependent on a variety of factors including preoperative ROM, surgical technique, implant design, and postoperative rehabilitation42). The recent introduction of high-flexion implants designed to reduce friction and damage while maintaining the contact surfaces and to delay impingement has enabled up to 155° of knee flexion and high-flexion activities3,42). Still, a consensus has yet to be reached on the efficacy of high-flexion TKA. According to Cho et al.43), in spite of satisfactory improvement in the ROM (from 9°-117° preoperatively to 2°-131° postoperatively), the incidence of early loosening of the femoral component was found to be relatively high between 3 to 6 years after NexGen LPS-Flex (Zimmer Inc., Warsaw, IN, USA) TKA. Han and Kang2) reported that the survivorship of NexGen LPS-Flex TKA was lower than that of conventional and other high-flexion designs at a mean of 5 years after surgery in a Korean population. In addition, the prevalence of early loosening of the femoral component was relatively high in the knees with the NexGen LPS-Flex design, which they attributed to the engagement in high-flexion activities after surgery because there was no case of early loosening when squatting and kneeling were discouraged. In another NexGen LPS-Flex TKA study3), 52% of the patients achieved more than 135° maximum flexion and the incidence of aseptic loosening was as low as 0.9% at a mean of 4.8 years after TKA. In the study, the 5-year survivor rate was 99.1%, indicating favorable mid-term survivorship of high-flexion TKA. In summary, high-flexion TKA in Korean patients are advantageous for obtaining excellent ROM and knee scores that are comparable to those in Western patients; however, the incidence of component loosening was relatively high and the implant survival rate was low in Korean patients, which may be attributable to hyperflexion activities after surgery that frequently result in early loosening of the femoral component2,3,43,44,45,46,47,48) (Table 2).
Table 2. Outcome of High-Flexion Total Knee Arthroplasty Design.
F/U: follow-up, Postop: postoperative, HSS: Hospital for Special Surgery, ND: no data or unclear.
5. Failures in TKA
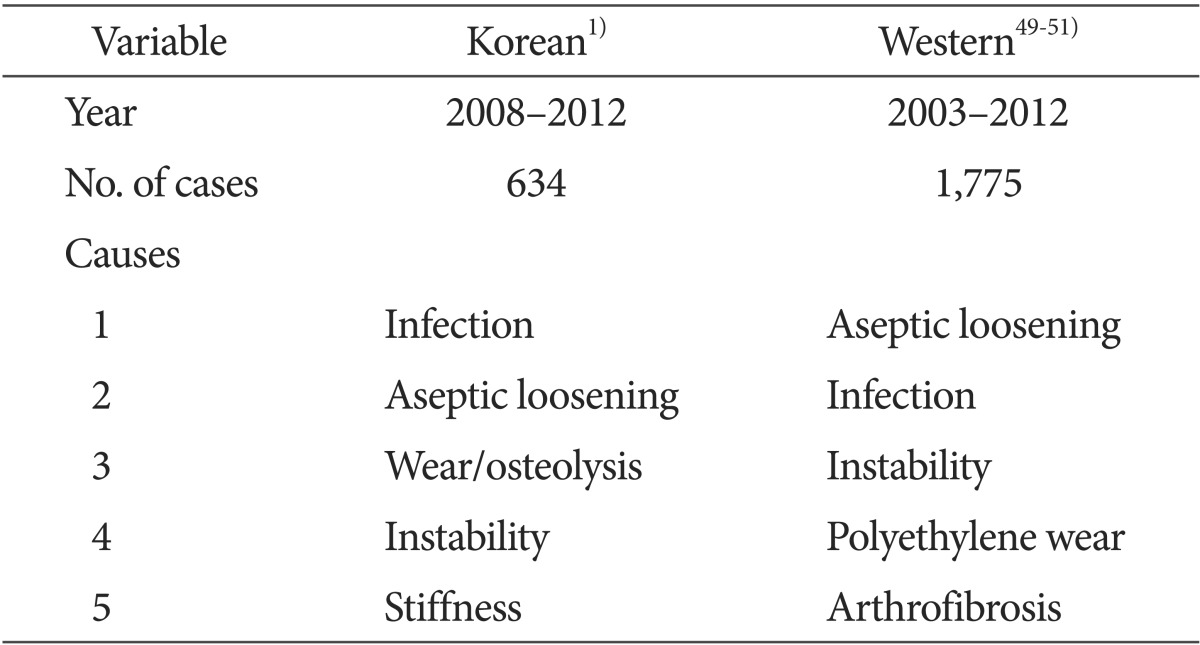
TKA is the most efficacious and successful treatment for advanced degenerative arthritis of the knee. Korea has seen a steady increase in the number of TKAs6), and thus the incidence of revision TKA is also expected to rise. In general, revision TKA is viewed as a costly and technically challenging procedure that delivers results not comparable to those of primary TKA1). Therefore, proper understanding of the mode of failure of primary TKA is crucial to improvement of surgical techniques and equipment and prevention of failure. In the past 5 years, the most common cause of revision TKA in Korean patients was infection followed by loosening and then component wear. More recently, the incidence of loosening appears to outnumber that of infection following TKA (Table 3), which is suspected to be associated with the growing cases of early loosening after high-flexion TKA, and accordingly with the engagement in high-flexion activities after primary TKA43). However, considering that these multicenter studies investigated the overall causes of revision TKA without differentiation of the early and late TKA failures, it is difficult to determine the number one cause of revision TKA between infection and component loosening. In general, infection is considered as the first major reason for early revision TKA both in the East and West1,49,50,51) whereas the late revisions were resulted from aseptic loosening, instability, and polyethylene wear52,53). In contrast, polyethylene wear, one of the classic failure mechanisms in TKA, showed marked decrease over time52,53).
Table 3. Failures after Total Knee Arthroplasty.
In Korea, aseptic loosening has surpassed infection in terms of prevalence in patients scheduled for revision TKA1). As we mentioned in the above, high-flexion positions after TKA and engagement of seniors in frequent social and leisure activities are thought to be linked with the growing incidence of aseptic loosening2,43). Cho et al.43) reported that early aseptic loosening of the femoral component did not occur in patients who had been prohibited from engaging in squatting and kneeling after high-flexion TKA.
Deep vein thrombosis (DVT) and pulmonary embolism (PE) after TKA are not common in Asian patients unlike in their Western counterparts in whom DVT and PE are two major complications after TKA54,55). In a meta-analysis of Asian populations, Kanchanabat et al.54) reported that the overall incidence of DVT, proximal DVT, symptomatic DVT, and symptomatic PE after TKA was 42.5%, 8.7%, 2.7%, and 0.5%, respectively. Regarding the incidence according to nations, postoperative DVT occurred in 11.8% in Southeast Asian countries, in 11.0% in Japan, in 7.5% in Korea, in 5.6% in China. Lee et al.55) documented the incidence of overall DVT after TKA as 40.8%, proximal DVT as 5.8%, distal DVT as 26.6%, symptomatic DVT as 1.9%, and symptomatic PE as 0.01%. Even without chemoprophylaxis, symptomatic PE and proximal DVT after TKA are not as common in Asians as in the Western populations54,55). Therefore, considering the significantly low risk of symptomatic DVT and the increased risk of drug-induced bleeding, chemoprophylaxis after TKA may need to be prescribed to high-risk patients only unlike in Western countries where chemoprophylaxis is the standard of care after TKA in all patients.
6. Revision Rate and Survivorship
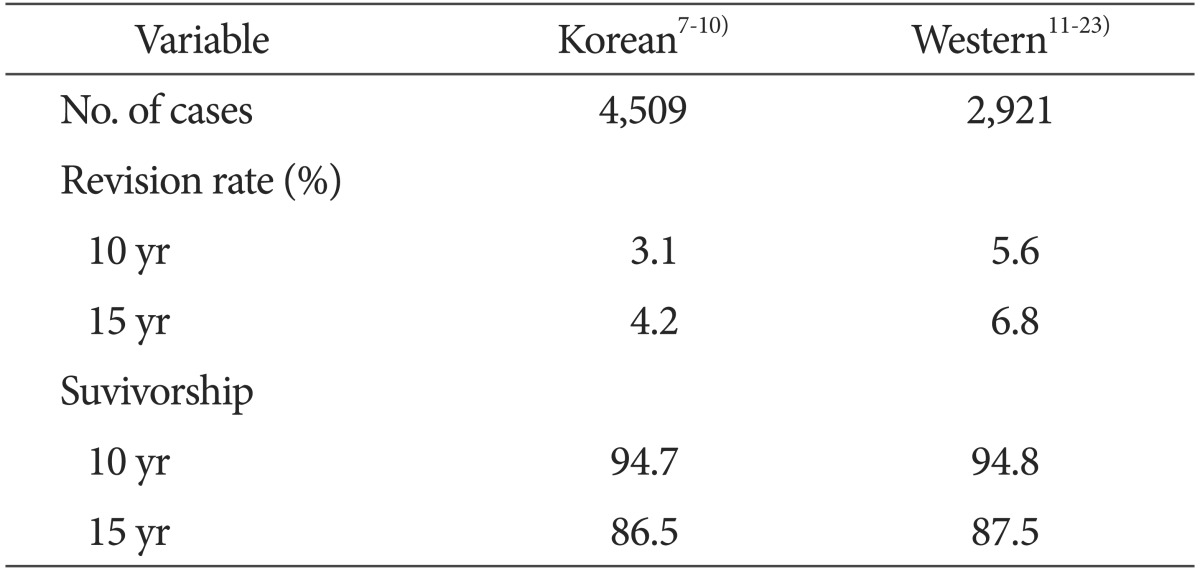
Based on a review of more than 10-year follow-up studies published since 2000, the revision rate after primary TKA was relatively low in Korean patients than in Western patients: 3.1% vs. 5.6% at 10 years after surgery and 4.2% vs. 6.8% at 15 years after surgery. However, there was no notable difference with regard to survivorship between Korean and Western patients: the 10-year and 15-year survivorships were 94.7% and 86.5%, respectively, among Koreans and 94.8% and 87.5%, respectively, among Westerners (Table 4).
Table 4. Revision Rate and Suvivorship of Total Knee Arthroplasty.
Conclusions
Our review of studies shows clinical outcomes of TKA in Korean patients are comparable to those in Western counterparts: there was no remarkable difference between races at least with respect to clinical results. However, most of the contemporary knee prostheses implanted in Korean patients are designed to accommodate Western patients' anatomical characteristics, which may result in component overhang or underhang, eventually compromising implant stability and clinical results. In addition, the introduction of high-flexion knee designs for improved patient satisfaction in Korea where high-flexion positions are frequently unavoidable during daily activities may be associated with component loosening. Considering that Koreans have smaller stature/bone structure and condylar aspect ratio than Westerners and most TKA patients are female, it may be advisable to utilize gender-specific knee designs. With regard to the postoperative complication and revision rates, no significant difference was found between Koreans and Westerners, but DVT and PE were remarkably less common in Koreans. In light of this review, we suggest further research and interest in physical characteristics of Korean TKA patients are necessary.
Footnotes
Conflict of Interest: No potential conflict of interest relevant to this article was re-ported.
References
- 1.Koh IJ, Cho WS, Choi NY, Kim TK Kleos Korea Research Group. Causes, risk factors, and trends in failures after TKA in Korea over the past 5 years: a multicenter study. Clin Orthop Relat Res. 2014;472:316–326. doi: 10.1007/s11999-013-3252-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Han HS, Kang SB. Brief followup report: does high-flexion total knee arthroplasty allow deep flexion safely in Asian patients? Clin Orthop Relat Res. 2013;471:1492–1497. doi: 10.1007/s11999-012-2628-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lee BS, Chung JW, Kim JM, Kim KA, Bin SI. High-flexion prosthesis improves function of TKA in Asian patients without decreasing early survivorship. Clin Orthop Relat Res. 2013;471:1504–1511. doi: 10.1007/s11999-012-2661-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Song MH, Yoo SH, Kang SW, Kim YJ, Park GT, Pyeun YS. Coronal alignment of the lower limb and the incidence of constitutional varus knee in korean females. Knee Surg Relat Res. 2015;27:49–55. doi: 10.5792/ksrr.2015.27.1.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lasam MP, Lee KJ, Chang CB, Kang YG, Kim TK. Femoral lateral bowing and varus condylar orientation are prevalent and affect axial alignment of TKA in Koreans. Clin Orthop Relat Res. 2013;471:1472–1483. doi: 10.1007/s11999-012-2618-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Koh IJ, Kim MW, Kim JH, Han SY, In Y. Trends in high tibial osteotomy and knee arthroplasty utilizations and demographics in Korea from 2009 to 2013. J Arthroplasty. 2015;30:939–944. doi: 10.1016/j.arth.2015.01.002. [DOI] [PubMed] [Google Scholar]
- 7.Kim YH, Yoon SH, Kim JS. The long-term results of simultaneous fixed-bearing and mobile-bearing total knee replacements performed in the same patient. J Bone Joint Surg Br. 2007;89:1317–1323. doi: 10.1302/0301-620X.89B10.19223. [DOI] [PubMed] [Google Scholar]
- 8.Kim YH, Park JW, Kim JS, Kulkarni SS, Kim YH. Long-term clinical outcomes and survivorship of press-fit condylar sigma fixed-bearing and mobile-bearing total knee prostheses in the same patients. J Bone Joint Surg Am. 2014;96:e168. doi: 10.2106/JBJS.M.01130. [DOI] [PubMed] [Google Scholar]
- 9.Bae DK, Song SJ, Park MJ, Eoh JH, Song JH, Park CH. Twenty-year survival analysis in total knee arthroplasty by a single surgeon. J Arthroplasty. 2012;27:1297–1304. doi: 10.1016/j.arth.2011.10.027. [DOI] [PubMed] [Google Scholar]
- 10.Yang JH, Yoon JR, Oh CH, Kim TS. Hybrid component fixation in total knee arthroplasty: minimum of 10-year follow-up study. J Arthroplasty. 2012;27:1111–1118. doi: 10.1016/j.arth.2011.09.019. [DOI] [PubMed] [Google Scholar]
- 11.Arthur CH, Wood AM, Keenan AC, Clayton RA, Walmsley P, Brenkel I. Ten-year results of the Press Fit Condylar Sigma total knee replacement. Bone Joint J. 2013;95:177–180. doi: 10.1302/0301-620X.95B2.29695. [DOI] [PubMed] [Google Scholar]
- 12.Ritter MA, Meneghini RM. Twenty-year survivorship of cementless anatomic graduated component total knee arthroplasty. J Arthroplasty. 2010;25:507–513. doi: 10.1016/j.arth.2009.04.018. [DOI] [PubMed] [Google Scholar]
- 13.Duffy GP, Murray BE, Trousdale RR. Hybrid total knee arthroplasty analysis of component failures at an average of 15 years. J Arthroplasty. 2007;22:1112–1115. doi: 10.1016/j.arth.2007.04.007. [DOI] [PubMed] [Google Scholar]
- 14.Huizinga MR, Brouwer RW, Bisschop R, van der Veen HC, van den Akker-Scheek I, van Raay JJ. Long-term follow-up of anatomic graduated component total knee arthroplasty: a 15- to 20-year survival analysis. J Arthroplasty. 2012;27:1190–1195. doi: 10.1016/j.arth.2011.11.020. [DOI] [PubMed] [Google Scholar]
- 15.Petursson G, Fenstad AM, Havelin LI, Gothesen O, Lygre SH, Rohrl SM, Furnes O. Better survival of hybrid total knee arthroplasty compared to cemented arthroplasty: a report from the Norwegian Arthroplasty Register 1999-2012. Acta Orthop. 2015 Jul 16; doi: 10.3109/17453674.2015.1073539. [Epub] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schroder HM, Berthelsen A, Hassani G, Hansen EB, Solgaard S. Cementless porous-coated total knee arthroplasty: 10-year results in a consecutive series. J Arthroplasty. 2001;16:559–567. doi: 10.1054/arth.2001.23565. [DOI] [PubMed] [Google Scholar]
- 17.Melton JT, Mayahi R, Baxter SE, Facek M, Glezos C. Long-term outcome in an uncemented, hydroxyapatite-coated total knee replacement: a 15- to 18-year survivorship analysis. J Bone Joint Surg Br. 2012;94:1067–1070. doi: 10.1302/0301-620X.94B8.28350. [DOI] [PubMed] [Google Scholar]
- 18.Dixon MC, Brown RR, Parsch D, Scott RD. Modular fixed-bearing total knee arthroplasty with retention of the posterior cruciate ligament: a study of patients followed for a minimum of fifteen years. J Bone Joint Surg Am. 2005;87:598–603. doi: 10.2106/JBJS.C.00591. [DOI] [PubMed] [Google Scholar]
- 19.Wright RJ, Sledge CB, Poss R, Ewald FC, Walsh ME, Lingard EA. Patient-reported outcome and survivorship after Kinemax total knee arthroplasty. J Bone Joint Surg Am. 2004;86:2464–2470. doi: 10.2106/00004623-200411000-00016. [DOI] [PubMed] [Google Scholar]
- 20.Baker PN, Khaw FM, Kirk LM, Esler CN, Gregg PJ. A randomised controlled trial of cemented versus cementless press-fit condylar total knee replacement: 15-year survival analysis. J Bone Joint Surg Br. 2007;89:1608–1614. doi: 10.1302/0301-620X.89B12.19363. [DOI] [PubMed] [Google Scholar]
- 21.Gothesen O, Espehaug B, Havelin L, Petursson G, Lygre S, Ellison P, Hallan G, Furnes O. Survival rates and causes of revision in cemented primary total knee replacement: a report from the Norwegian Arthroplasty Register 1994-2009. Bone Joint J. 2013;95:636–642. doi: 10.1302/0301-620X.95B5.30271. [DOI] [PubMed] [Google Scholar]
- 22.Attar FG, Khaw FM, Kirk LM, Gregg PJ. Survivorship analysis at 15 years of cemented press-fit condylar total knee arthroplasty. J Arthroplasty. 2008;23:344–349. doi: 10.1016/j.arth.2007.02.012. [DOI] [PubMed] [Google Scholar]
- 23.Schai PA, Thornhill TS, Scott RD. Total knee arthroplasty with the PFC system: results at a minimum of ten years and survivorship analysis. J Bone Joint Surg Br. 1998;80:850–858. doi: 10.1302/0301-620x.80b5.8368. [DOI] [PubMed] [Google Scholar]
- 24.Cheng T, Zhu C, Wang J, Cheng M, Peng X, Wang Q, Zhang X. No clinical benefit of gender-specific total knee arthroplasty. Acta Orthop. 2014;85:415–421. doi: 10.3109/17453674.2014.931194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kim JM, Kim SB, Kim JM, Lee DH, Lee BS, Bin SI. Results of gender-specific total knee arthroplasty: comparative study with traditional implant in female patients. Knee Surg Relat Res. 2015;27:17–23. doi: 10.5792/ksrr.2015.27.1.17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lonner JH, Jasko JG, Thomas BS. Anthropomorphic differences between the distal femora of men and women. Clin Orthop Relat Res. 2008;466:2724–2729. doi: 10.1007/s11999-008-0415-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bonnin MP, Schmidt A, Basiglini L, Bossard N, Dantony E. Mediolateral oversizing influences pain, function, and flexion after TKA. Knee Surg Sports Traumatol Arthrosc. 2013;21:2314–2324. doi: 10.1007/s00167-013-2443-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hitt K, Shurman JR, 2nd, Greene K, McCarthy J, Moskal J, Hoeman T, Mont MA. Anthropometric measurements of the human knee: correlation to the sizing of current knee arthroplasty systems. J Bone Joint Surg Am. 2003;85(Suppl 4):115–122. [PubMed] [Google Scholar]
- 29.Chung BJ, Kang JY, Kang YG, Kim SJ, Kim TK. Clinical implications of femoral anthropometrical features for total knee arthroplasty in Koreans. J Arthroplasty. 2015;30:1220–1227. doi: 10.1016/j.arth.2015.02.014. [DOI] [PubMed] [Google Scholar]
- 30.Westrich GH, Haas SB, Insall JN, Frachie A. Resection specimen analysis of proximal tibial anatomy based on 100 total knee arthroplasty specimens. J Arthroplasty. 1995;10:47–51. doi: 10.1016/s0883-5403(05)80100-7. [DOI] [PubMed] [Google Scholar]
- 31.Kwak DS, Surendran S, Pengatteeri YH, Park SE, Choi KN, Gopinathan P, Han SH, Han CW. Morphometry of the proximal tibia to design the tibial component of total knee arthroplasty for the Korean population. Knee. 2007;14:295–300. doi: 10.1016/j.knee.2007.05.004. [DOI] [PubMed] [Google Scholar]
- 32.Mensch JS, Amstutz HC. Knee morphology as a guide to knee replacement. Clin Orthop Relat Res. 1975;(112):231–241. [PubMed] [Google Scholar]
- 33.Hsu HC, Luo ZP, Rand JA, An KN. Influence of patellar thickness on patellar tracking and patellofemoral contact characteristics after total knee arthroplasty. J Arthroplasty. 1996;11:69–80. doi: 10.1016/s0883-5403(96)80163-x. [DOI] [PubMed] [Google Scholar]
- 34.Kim TK, Chung BJ, Kang YG, Chang CB, Seong SC. Clinical implications of anthropometric patellar dimensions for TKA in Asians. Clin Orthop Relat Res. 2009;467:1007–1014. doi: 10.1007/s11999-008-0557-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Baldwin JL, House CK. Anatomic dimensions of the patella measured during total knee arthroplasty. J Arthroplasty. 2005;20:250–257. doi: 10.1016/j.arth.2004.09.027. [DOI] [PubMed] [Google Scholar]
- 36.Chmell M, McManus J, Scott RD. Thickness of the patella in men and women with osteoarthritis. Knee. 1995;2:239–241. [Google Scholar]
- 37.Bellemans J, Colyn W, Vandenneucker H, Victor J. The Chitranjan Ranawat award: is neutral mechanical alignment normal for all patients? The concept of constitutional varus. Clin Orthop Relat Res. 2012;470:45–53. doi: 10.1007/s11999-011-1936-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Shetty GM, Mullaji A, Bhayde S, Nha KW, Oh HK. Factors contributing to inherent varus alignment of lower limb in normal Asian adults: role of tibial plateau inclination. Knee. 2014;21:544–548. doi: 10.1016/j.knee.2013.09.008. [DOI] [PubMed] [Google Scholar]
- 39.Magnussen RA, Weppe F, Demey G, Servien E, Lustig S. Residual varus alignment does not compromise results of TKAs in patients with preoperative varus. Clin Orthop Relat Res. 2011;469:3443–3450. doi: 10.1007/s11999-011-1988-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Parratte S, Pagnano MW, Trousdale RT, Berry DJ. Effect of postoperative mechanical axis alignment on the fifteen-year survival of modern, cemented total knee replacements. J Bone Joint Surg Am. 2010;92:2143–2149. doi: 10.2106/JBJS.I.01398. [DOI] [PubMed] [Google Scholar]
- 41.Mason JB, Fehring TK, Estok R, Banel D, Fahrbach K. Meta-analysis of alignment outcomes in computer-assisted total knee arthroplasty surgery. J Arthroplasty. 2007;22:1097–1106. doi: 10.1016/j.arth.2007.08.001. [DOI] [PubMed] [Google Scholar]
- 42.Kurosaka M, Yoshiya S, Mizuno K, Yamamoto T. Maximizing flexion after total knee arthroplasty: the need and the pitfalls. J Arthroplasty. 2002;17(4 Suppl 1):59–62. doi: 10.1054/arth.2002.32688. [DOI] [PubMed] [Google Scholar]
- 43.Cho SD, Youm YS, Park KB. Three- to six-year follow-up results after high-flexion total knee arthroplasty: can we allow passive deep knee bending? Knee Surg Sports Traumatol Arthrosc. 2011;19:899–903. doi: 10.1007/s00167-010-1218-x. [DOI] [PubMed] [Google Scholar]
- 44.Gupta SK, Ranawat AS, Shah V, Zikria BA, Zikria JF, Ranawat CS. The P.F.C. sigma RP-F TKA designed for improved performance: a matched-pair study. Orthopedics. 2006;29(9 Suppl):S49–S52. [PubMed] [Google Scholar]
- 45.Kim TH, Lee DH, Bin SI. The NexGen LPS-flex to the knee prosthesis at a minimum of three years. J Bone Joint Surg Br. 2008;90:1304–1310. doi: 10.1302/0301-620X.90B10.21050. [DOI] [PubMed] [Google Scholar]
- 46.Kim YH, Sohn KS, Kim JS. Range of motion of standard and high-flexion posterior stabilized total knee prostheses: a prospective, randomized study. J Bone Joint Surg Am. 2005;87:1470–1475. doi: 10.2106/JBJS.D.02707. [DOI] [PubMed] [Google Scholar]
- 47.Scuderi GR, Hedden DR, Maltry JA, Traina SM, Sheinkop MB, Hartzband MA. Early clinical results of a high-flexion, posterior-stabilized, mobile-bearing total knee arthroplasty: a US investigational device exemption trial. J Arthroplasty. 2012;27:421–429. doi: 10.1016/j.arth.2011.06.011. [DOI] [PubMed] [Google Scholar]
- 48.Wohlrab D, Hube R, Zeh A, Hein W. Clinical and radiological results of high flex total knee arthroplasty: a 5 year follow-up. Arch Orthop Trauma Surg. 2009;129:21–24. doi: 10.1007/s00402-008-0665-z. [DOI] [PubMed] [Google Scholar]
- 49.Schroer WC, Berend KR, Lombardi AV, Barnes CL, Bolognesi MP, Berend ME, Ritter MA, Nunley RM. Why are total knees failing today? Etiology of total knee revision in 2010 and 2011. J Arthroplasty. 2013;28(8 Suppl):116–119. doi: 10.1016/j.arth.2013.04.056. [DOI] [PubMed] [Google Scholar]
- 50.Sharkey PF, Lichstein PM, Shen C, Tokarski AT, Parvizi J. Why are total knee arthroplasties failing today: has anything changed after 10 years? J Arthroplasty. 2014;29:1774–1778. doi: 10.1016/j.arth.2013.07.024. [DOI] [PubMed] [Google Scholar]
- 51.van Kempen RW, Schimmel JJ, van Hellemondt GG, Vandenneucker H, Wymenga AB. Reason for revision TKA predicts clinical outcome: prospective evaluation of 150 consecutive patients with 2-years followup. Clin Orthop Relat Res. 2013;471:2296–2302. doi: 10.1007/s11999-013-2940-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Calliess T, Ettinger M, Hulsmann N, Ostermeier S, Windhagen H. Update on the etiology of revision TKA: evident trends in a retrospective survey of 1449 cases. Knee. 2015;22:174–179. doi: 10.1016/j.knee.2015.02.007. [DOI] [PubMed] [Google Scholar]
- 53.Thiele K, Perka C, Matziolis G, Mayr HO, Sostheim M, Hube R. Current failure mechanisms after knee arthroplasty have changed: polyethylene wear is less common in revision surgery. J Bone Joint Surg Am. 2015;97:715–720. doi: 10.2106/JBJS.M.01534. [DOI] [PubMed] [Google Scholar]
- 54.Kanchanabat B, Stapanavatr W, Meknavin S, Soorapanth C, Sumanasrethakul C, Kanchanasuttirak P. Systematic review and meta-analysis on the rate of postoperative venous thromboembolism in orthopaedic surgery in Asian patients without thromboprophylaxis. Br J Surg. 2011;98:1356–1364. doi: 10.1002/bjs.7589. [DOI] [PubMed] [Google Scholar]
- 55.Lee WS, Kim KI, Lee HJ, Kyung HS, Seo SS. The incidence of pulmonary embolism and deep vein thrombosis after knee arthroplasty in Asians remains low: a meta-analysis. Clin Orthop Relat Res. 2013;471:1523–1532. doi: 10.1007/s11999-012-2758-9. [DOI] [PMC free article] [PubMed] [Google Scholar]