Abstract
Wegener’s granulomatosis, Sarcoidosis, Sjögren’s Syndrome, Behçet disease, Systemic lupus erythematosus, relapsing polychondritis, Churg–Strauss syndrome and Cogan syndromes are rheumatic diseases commonly encountered by otolaryngologists. The present study was designed to assess the understanding and practice about various ENT problems of rheumatic diseases amongst otolaryngologists. A group of 29 otolaryngologists was asked to fill questionnaire which was based on knowledge and practice of otolaryngologists about various otolaryngologic manifestations of rheumatic diseases. Chronic sinusitis was most frequently seen followed by recurrent oral ulcers while spontaneous septal perforation was most infrequently seen symptom by participants. Otolaryngologists showed high index of suspicion and confidence for Wegener’s granulomatosis in comparison to other rheumatic diseases. There was no difference noted in practice of otolaryngologists of tertiary care centers and other practitioners. Eighty two percent of participants felt, they were not adequately trained about these diseases. Most of them (93 %) felt that knowledge of such diseases is also necessary for post graduate training in Otolaryngology. Though otolaryngologists are aware of otolaryngologic manifestations of Rheumatic diseases but their index of suspicion, practical implication of knowledge and confidence for evaluation of such diseases is low. Educational sector should define a better medical curriculum for training in Otorhinolaryngology, head and neck surgery.
Keywords: Rheumatic diseases, Otolaryngologic manifestations, Practice, Awareness, Wegener’s granulomatosis, Sarcoidosis
Introduction
Rheumatic diseases are systemic problems and involve almost all organs at various stages of the disease. Wegener’s granulomatosis now known as granulomatosis with polyangiitis (GPA), Sarcoidosis, Sjögren’s Syndrome, Behçet disease, Systemic lupus erythematosus (SLE), Relapsing polychondritis (RP), Churg–Strauss syndrome (Eosinophilic granulomatosis with polyangiitis) and Cogan syndromes are rheumatic diseases observed in clinical practice. These rheumatological disorders can have varied systemic and head and neck related manifestations. Common ear, nose, throat (ENT) manifestations of these disorders include bilateral parotid enlargement, excessive dryness of oral cavity, inflammation of cartilage of pinna & nose, recurrent sinusitis, sensorineural hearing loss, recurrent oral ulcers, spontaneous septal and palatal perforations. Rheumatologic patients often visit an otolaryngologist even before any specialist because of various ENT related problems. ENT symptoms may represent an early sign of an undiagnosed autoimmune disorder that often requires an immediate and aggressive immunosuppressive treatment [1]. An Otolaryngologist should maintain a high index of suspicion to identify the underlying disease as these may be the only manifestations of the systemic disease in early stages. Although otolaryngologic manifestations of various rheumatic diseases have been well described, awareness among otolaryngologists regarding these manifestations is negligible. [2–9] Early and accurate diagnosis with prompt treatment or referral to specialists may prevent morbidity and mortality related to these diseases. The present study was designed to assess the understanding and practice about various ENT problems of rheumatic diseases amongst otolaryngologists.
Materials and Methods
A descriptive cross sectional study was conducted among otolaryngologists practicing in North India. Otolaryngologists working in private clinics as well as teaching institutions were included. The otolaryngologists were contacted personally by the authors or via email. A questionnaire based on knowledge and practice of otolaryngologists about various rheumatic diseases was used to obtain information. Demographic data such as age, gender, education, place and duration of practice was also recorded. The questionnaire was based on seven diseases namely Wegener’s granulomatosis (GPA), Sarcoidosis, Sjögren’s syndrome, Relapsing polychondritis, SLE, Behçet disease, and Cogan syndrome. The questions related to otolaryngologist’s awareness about these diseases, the ENT manifestations and their approach toward these diseases. Their knowledge, practice and confidence in evaluation and investigation of these diseases were recorded and analyzed. Descriptive statistics was used to analyze the responses.
Results
A total of 36 otolaryngologists of North India were asked to fill this questionnaire. A total of 29 otolaryngologists agreed and returned the completed questionnaires, representing a response rate of 82 %. Mean age was 41 ± 9 years. Half of the participants were working in tertiary care facilities (medical colleges). The demographic characteristics of the participants are presented in Table 1.
Table 1.
Demographic data (n = 29)
| Sex distribution n (%) | |
| Male | 27 (93 %) |
| Female | 2 (7 %) |
| Duration of practice | |
| 0–5 years | 8 (28 %) |
| 6–10 years | 6 (20 %) |
| 10–20 years | 11 (38 %) |
| 21> | 4 (14 %) |
| Place of work | |
| Private clinic & nursing home | 8 (28 %) |
| Primary health care facility | 3 (10 %) |
| Secondary care facility | 3 (10 %) |
| Tertiary care facility | 15 (52 %) |
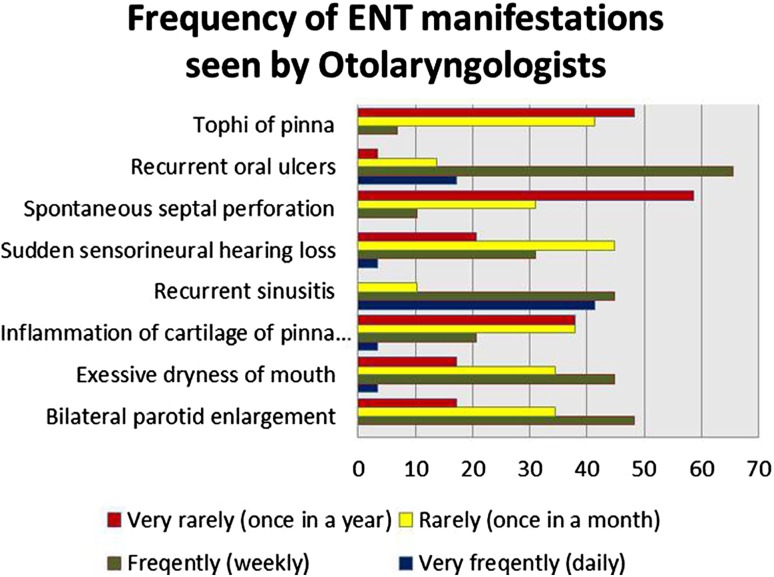
The frequency of visits to an ENT clinic with rheumatic disease related manifestations is displayed in Fig. 1. Chronic sinusitis was most frequently seen followed by recurrent oral ulcers while spontaneous septal perforation was most infrequently seen symptom by participants. All of them except one were familiar with Sjögren’s syndrome and Wegener’s granulomatosis/GPA. Few of them were unfamiliar to Relapsing polychondritis, Cogan and Behçet (Table 2). More than 85 % of them answered correctly regarding characteristic clinical feature of Wegener’s granulomatosis/GPA, Sjögren’s syndrome and Relapsing polychondritis while significant incorrect responses were noted about other diseases (Table 2). Index of suspicion was seen maximum (59 %) for Wegener’s granulomatosis/GPA and minimum (17 %) for Cogan syndrome. Similar index of suspicion was noted among tertiary care and non-tertiary care practitioners (Table 3: p value range for various diseases 0.13–1.0). Many of them (55–83 %) were referring their patients to a specialist in case of suspicion. Highest confidence was seen for investigating Wegener’s granulomatosis/GPA whereas the least for SLE (Table 2).
Fig. 1.
Frequency of ENT manifestations seen by otolaryngologists
Table 2.
Positive responses regarding familiarity, clinical features, index of suspicion and level of confidence about rheumatic diseases
| Disease | Familiarity about Rheumatic diseases n (%) | Choose characteristic clinical feature (correct answer) n (%) | Rheumatic diseases suspected or diagnosed by participants (yes) n (%) | Confidence in evaluation (yes) n (%) |
|---|---|---|---|---|
| Wegeners granulomatosis/GPA | 28 (100) | 25 (86) | 17 (59) | 13 (45) |
| Sarcoidosis | 29 (100) | 16(55) | 16 (55) | 08 (28) |
| Sjogrens | 28 (96) | 25 (86) | 12 (41) | 09 (31) |
| Relapsing polychondritis | 24 (82) | 25 (86) | 15 (52) | 11 (38) |
| Systemic lupus erythmatosus | 29 (100) | 19 (65) | 13 (45) | 05 (17) |
| Bechet’s disease | 23 (79) | 17 (59) | 07 (24) | 06 (21) |
| Cogan’s syndrome | 22 (75) | 19 (65) | 5 (17) | 07 (24) |
Table 3.
Comparison of index of suspicion among tertiary care practitioners and other practitioners
| Disease | Tertiary care practitioner n: 15 (%) | Non tertiary care practitioner n: 14 (%) | P value |
|---|---|---|---|
| Wegeners granulomatosis/GPA | 73 | 46 | 0.28 |
| Sarcoidosis | 66 | 53 | 0.49 |
| Sjogrens | 46 | 35 | 0.55 |
| Relapsing polychondritis | 60 | 35 | 0.13 |
| Systemic lupus erythmatosus | 42 | 42 | 1.0 |
| Bechet’s disease | 35 | 14 | 0.45 |
| Cogan’s syndrome | 26 | 7.6 | 0.37 |
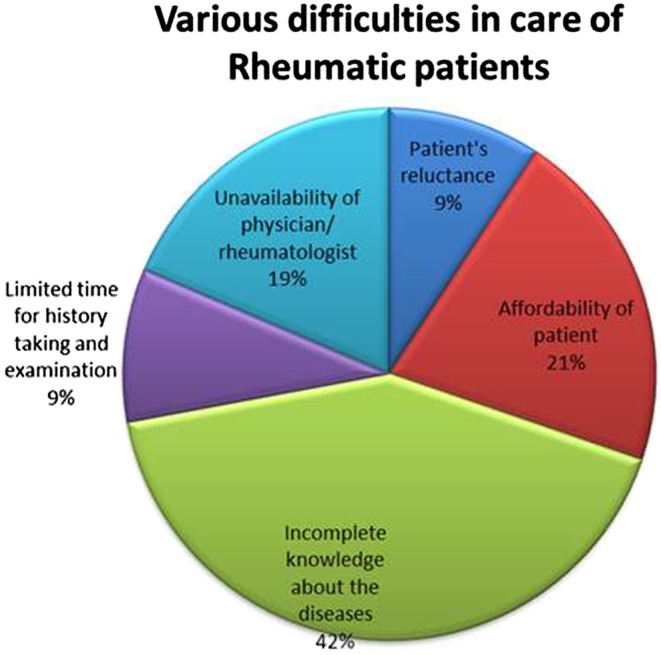
One participant did not answer, four opined that they were adequately taught and 24 (82 %) felt that their post graduate training was not adequate about rheumatic diseases. Otolaryngologists experienced various difficulties in care of rheumatic disease patients (Fig. 2). Most of them (93 %) felt that knowledge of such diseases is also necessary for post graduate training in Otolaryngology.
Fig. 2.
Various difficulties in care of rheumatic patients
Discussion
Patients suffering with rheumatic diseases need to visit various specialists apart from rheumatologists/physician because of multiple organs involved. Early recognition and best management of these patients depends on awareness of these diseases among other specialists. In present study we tried to assess knowledge and practice about ENT manifestations of rheumatic diseases among a group of otolaryngologists. Half of the otolaryngologists were working in tertiary care centers (medical colleges).Otolaryngologists were well aware about clinical features of Wegener’s granulomatosis/GPA and approximately 60 % had suspected and evaluated their patients for Wegener’s granulomatosis/GPA sometime in their practice. Otolaryngologists showed maximum confidence in investigating Wegener’s granulomatosis/GPA in comparison to other rheumatic diseases.
Dryness of oral cavity and salivary gland enlargement are two clinical features for which these Sjögren’s patients often visit to an otolaryngologist. Minor salivary gland biopsy is one of the criteria for diagnosing Sjögren’s syndrome and it is the domain of an Otolaryngologist [10]. Interestingly almost 80 % of the participants were seeing sicca symptoms every month but 60 % had never suspected this disease in their patients and only 30 % showed confidence in evaluation of Sjögren’s syndrome.
Relapsing polychondritis, a rare disorder with frequent delay in diagnosis [11] is another rheumatic disease with predominant ENT related manifestations. Though a large number (almost 80 %) in our study was familiar to this disease and chose correct answer regarding its clinical feature but only half of them had ever thought of this disease in clinical practice.
Other rheumatic diseases of Otolaryngologist’s interest are Behcets and Cogan’s syndrome. While defining feature of Behçet’s disease is recurrent oral ulceration, Cogan syndrome resembles Meniere’s disease [12, 13]. Though three fourth of them were familiar about these disease only one fifth had ever suspected and shown confidence in evaluation of these disease.
It shows though they are aware of Otolaryngologic manifestations of Rheumatic diseases but their index of suspicion, practical implication of knowledge and the confidence for evaluation of such diseases are not sufficient. One very interesting finding in our study was that there was no difference noted in practice of otolaryngologists of tertiary care centers and other practitioners.
A large number (82 %) felt that such diseases were not given adequate importance during their post graduate training. Amongst the various limiting factors for detail evaluation of such patients, 62 % rated incomplete knowledge about these diseases, one third said unaffordability of patients and 27 % felt unavailability of Physician or Rheumatologist as the major factors. Most of them (93 %) felt that incorporation of this aspect in the post graduate training in Otolaryngology is necessary.
Since lack of awareness may result in eligible patients with rheumatic diseases not being referred for appropriate evaluation and management, strategies to improve otolaryngologist’s awareness are critical to ensure proper evaluation and appropriate referral of patients. This study suggests that the educational sector should revamp the medical curriculum for training in Otorhinolaryngology, head and neck surgery. Based on this survey’s results, educational strategies to improve otolaryngologists awareness about rheumatic diseases is necessary for best management of patients suffering with these diseases. The two limitations of this study were the small sample size and the lack of enough responses in the questionnaire which would reflect the subject’s actual response. The result of the study may differ from actual practice since responding to a question is different from actual practice.
Acknowledgments
We acknowledge Dr. Naveen kakkar, Dr. Jency koshy and Dr. Saurabh varshney for their valuable contribution.
References
- 1.Gusmão RJ, Fernandes FL, Guimarães AC, Scaramussa L, Sachetto Z, Pauna HF, de Carvalho GM. Otorhinolaryngological findings in a group of patients with rheumatic diseases. Rev Bras Reumatol. 2014;54(3):172–178. doi: 10.1016/j.rbr.2013.10.003. [DOI] [PubMed] [Google Scholar]
- 2.Papadimitraki ED, Kyrmizakis DE, Kritikos I, Boumpas DT. Ear-nose-throat manifestations of autoimmune rheumatic diseases. Clin Exp Rheumatol. 2004;22(4):485–494. [PubMed] [Google Scholar]
- 3.Parra-García GD, Callejas-Rubio JL, Ríos-Fernández R, Sainz-Quevedo M, Ortego-Centeno N. Otolaryngologic manifestations of systemic vasculitis. Acta Otorrinolaringol Esp. 2012;63(4):303–310. doi: 10.1016/j.otorri.2011.09.002. [DOI] [PubMed] [Google Scholar]
- 4.Nakamaru Y, Takagi D, Oridate N, Homma A, Fukuda S. Otolaryngologic manifestations of antineutrophil cytoplasmic antibody-associated vasculitis. Otolaryngol Head Neck Surg. 2012;146(1):119–121. doi: 10.1177/0194599811424044. [DOI] [PubMed] [Google Scholar]
- 5.PinoRivero V, González Palomino A, Pantoja Hernández CG, Trinidad Ruíz G, Pardo Romero G, Montero García C, Blasco Huelva A. Otolaryngologic manifestations of Churg-Strauss sindrome. Report of a case and review of the literature. An OtorrinolaringolIbero Am, 2006; 33(1): 1–7 [PubMed]
- 6.Freeman SR, Sheehan PZ, Thorpe MA, Rutka JA. Ear, nose, and throat manifestations of Sjögren’s syndrome: retrospective review of a multidisciplinary clinic. J Otolaryngol. 2005;34(1):20–24. doi: 10.2310/7070.2005.00020. [DOI] [PubMed] [Google Scholar]
- 7.Shah UK, White JA, Gooey JE, Hybels RL. Otolaryngologic manifestations of sarcoidosis: presentation and diagnosis. Laryngoscope. 1997;107(1):67–75. doi: 10.1097/00005537-199701000-00015. [DOI] [PubMed] [Google Scholar]
- 8.Kulahli I, Balci K, Koseoglu E, Yuce I, Cagli S, Senturk M. Audio-vestibular disturbances in Behcet’s patients: report of 62 cases. Hear Res. 2005;203(1–2):28–31. doi: 10.1016/j.heares.2004.11.020. [DOI] [PubMed] [Google Scholar]
- 9.Knopf A, Bas M, Chaker A, Strassen U, Pickhard A, Stark T, Lahmer T, Thürmel K. Rheumatic disorders affecting the head and neck: underestimated diseases. Rheumatology (Oxford) 2011;50(11):2029–2034. doi: 10.1093/rheumatology/ker213. [DOI] [PubMed] [Google Scholar]
- 10.Cornec D, Saraux A, Cochener B, Pers JO, Jousse-Joulin S, Renaudineau Y, Marhadour T, Devauchelle-Pensec V. Level of agreement between 2002 American-European Consensus Group and 2012 American College of Rheumatology classification criteria for Sjögren’s syndrome and reasons for discrepancies. Arthritis Res Ther. 2014;16(2):R74. doi: 10.1186/ar4514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Trentham DE, Le CH. Relapsing Polychondritis. Ann Intern Med. 1998;129(2):114–122. doi: 10.7326/0003-4819-129-2-199807150-00011. [DOI] [PubMed] [Google Scholar]
- 12.Kontogiannis V, Powell RJ. Behçet’s disease. Postgrad Med J. 2000;76(900):629–637. doi: 10.1136/pmj.76.900.629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Greco A, Gallo A, Fusconi M, Magliulo G, Turchetta R, Marinelli C, Macri GF, De Virgilio A, de Vincentiis M. Cogan’s syndrome: an autoimmune inner ear disease. Autoimmun Rev. 2013;12(3):396–400. doi: 10.1016/j.autrev.2012.07.012. [DOI] [PubMed] [Google Scholar]