Abstract
To determine the incidence of otogenic complications of Chronic suppurative otitis media (CSOM) and its management. The study was conducted at the tertiary referral centre and teaching hospital. An analysis was made about the clinical and operative findings, surgical techniques and approaches, the overall management and recovery of the patient. The data were then compared with the relevant and available literature. Over the study period of 12 years, a total 45 cases of CSOM with complications were reviewed. Out of these 45 cases, 20 cases had extracranial (EC) while 25 cases had intracranial (IC) complications. The prevalence of each complication was 0.17 and 0.13 %, IC and EC respectively. The commonly encountered IC complications were brain abscess, meningitis and lateral sinus thrombophlebitis. Among the EC complications, mastoid abscess followed by labyrinthitis and facial nerve palsy were encountered. The reliable warning signs and symptoms of IC complications were fever, headache, earache vestibular symptoms, meningeal signs and impairment of consciousness. Proteus mirabilis, Pseudomonas aeruginosa, Staphylococcus epidermidis were the common organism isolated. Cholesteatoma and granulation in the middle ear were the major findings in both groups of cases. Surgery was main modality of management of these conditions. We observed that two patients fail to regain full facial nerve function despite of surgery. Mortality rate was zero but morbidity was seen in 15 % (3) and 28 % (7) of cases in EC and IC group respectively. The epidemiological presentation, clinical features and results of treatment are discussed. CSOM complications, despite its reduced incidence still pose a great challenge in developing countries, as the disease present in the advanced stage leading to difficulty in management and consequently higher morbidity. In this study we emphasize the importance of the accurate and early diagnosis followed by adequate surgical therapy with multidisciplinary approach.
Keywords: Chronic suppurative otitis media (CSOM), Extracranial complications, Intracranial complications, Cerebellar abscess, Meningitis, Lateral sinus thrombophlebitis
Introduction
Otitis media is common in developing countries among population of low socioeconomic strata. The advent of antibiotics has clearly changed the management of otitis media. Chronic otitis media are potentially serious disease because of their complications. In chronic cases complications are usually caused by progressive erosion of the bone thus increasing the risk of damage to facial nerve, labyrinth and the dura. Prior to antibiotic era, intracranial (IC) complication occurred in 2.3–4 % cases. With antibiotic and new surgical techniques, the complication have been greatly reduced to 0.15–0.04 %. Mortality decreased from 25 to 8 %.
Despite of an overall decline in the incidence of complications of otitis media, life threatening complications still exists. The suggested reasons are decrease in the physician’s experience, changing of virulence and susceptibility of bacteria and the state of individual patient.
The purpose of this study is to show the prevalence of overall complications of Chronic suppurative otitis media (CSOM), warning signs and symptoms, some aspects of causative bacteria and results of treatment. The objective of the study is to determine various types of otogenic complications affecting both the paediatric and adult population in our institution and efficacy of various clinical measures such as CT scan and culture and sensitivity tests, involved in their diagnosis and management.
Material and Method
From 1999 to 2010, overall 14,510 patients with suppurative otitis media were treated in the Department of ENT and Head Neck Surgery, J.L.N. Hospital and Research centre, Bhilai, Chhattisgarh. The study includes 45 cases of CSOM with complications. The charts of these patients were reviewed as to their history, clinical finding and investigations, audiological and radiological studies as well as culture and sensitivity tests. The complications of CSOM in our study were classified into two major categories; Extracranial (EC) and IC complications. The EC group includes subperiosteal abscess, labyrinthitis, mastoiditis and facial paralysis whereas the IC group included brain abscess, meningitis, lateral sinus thrombosis, extradural and subdural abscess.
Result
Prevalence
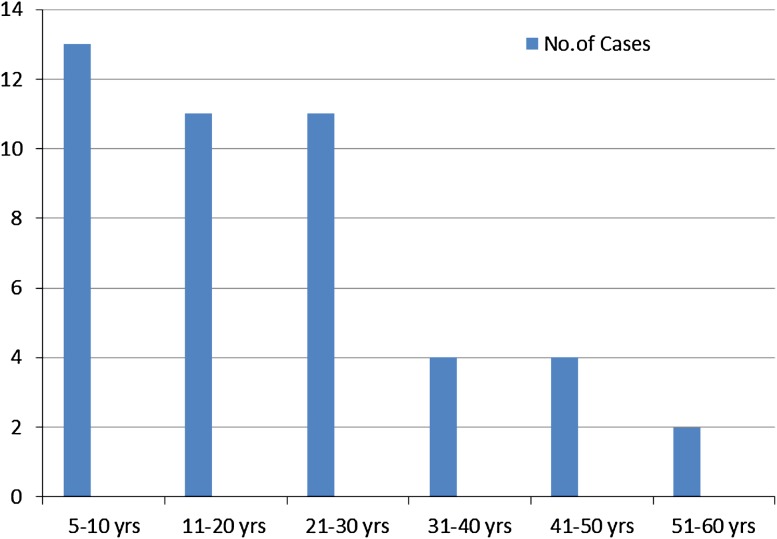
The prevalence of the EC group was 0.13 % and for the IC group was 0.17 %. The male to female ratio was found to be 3:2. The otitis media with complications usually occurred between the ages of 5–55 years. The youngest patient was 5 years old whereas the oldest one was of 55 years of age. The majority of patients were in the age group of 5–10 years (Graph 1).
Graph 1.
Age group distribution
Occupation
The patients included students and housewives. About 73.33 % (33) of patients were students. All patients were of low socioeconomic status and presented with a long standing neglected ear discharge.
Complication
A total 45 cases of CSOM were identified with complications out of which 20 patients had EC while 25 patients had IC complications. We found that 20 % (4) cases of EC group and 12 % (3) cases of IC group had more than one complication. The common complications in EC group were subperiosteal abscess, labyrinthitis and facial palsy. The subperiosteal abscess was the major co-disease. Brain abscess and meningitis were the two common complications in IC group. Out of 13 cases of Brain abscess, in nine cases it was seen in temporal lobe while in four cases it occurred in cerebellum. The other complications of the IC group were not uncommon and included lateral sinus thrombophlebitis and perisinus abscess, extradural and subdural abscess (Table 1).
Table 1.
Types of complications
| Sr. no. | Complication | No. of cases | Types | No. of cases |
|---|---|---|---|---|
| 1 | Extracranial | 20 | Subperiosteal abscess | 9 |
| Labyrinthitis | 8 | |||
| Facial nerve palsy | 7 | |||
| 2 | Intracranial | 25 | Brain abscess | 13 |
| Temporal lobe | 9 | |||
| Cerebellar | 4 | |||
| Meningitis | 6 | |||
| Lateral sinus thrombophlebitis and Perisinus abscess | 5 | |||
| Extradural abscess | 2 | |||
| Subdural empyema | 2 |
Clinical Signs and Symptoms
Out of 45 cases, the duration of otorrhoea was <5 years in 40 % of cases, 5–10 years in 30 % of cases and >10 years in 30 % of cases. Common clinical signs and symptoms in both groups are demonstrated in Table 2.
Table 2.
Common clinical signs and symptoms
| Sr. no. | Signs and symptoms | IC group (no. of cases) | EC group (no. of cases) |
|---|---|---|---|
| 1 | Fever | 10 | 9 |
| 2 | Headache | 18 | 13 |
| 3 | Meningeal signs | 9 | – |
| 4 | Altered sensorium | 9 | – |
| 5 | Otalgia | 16 | 10 |
| 6 | Nausea and vomiting | 9 | 8 |
| 7 | Localization signs | 23 | – |
| 8 | Post aural swelling/fistula | – | 9 |
| 9 | Papilloedema | 20 | – |
| 10 | Facial nerve palsy | – | 7 |
| 11 | Dizziness | 22 | 16 |
| 12 | Nystagmus | 21 | 8 |
Hearing loss assessment showed a conductive hearing loss in 11 cases whereas Sensorineural hearing loss in 28 cases while mixed type hearing loss in 12 cases.
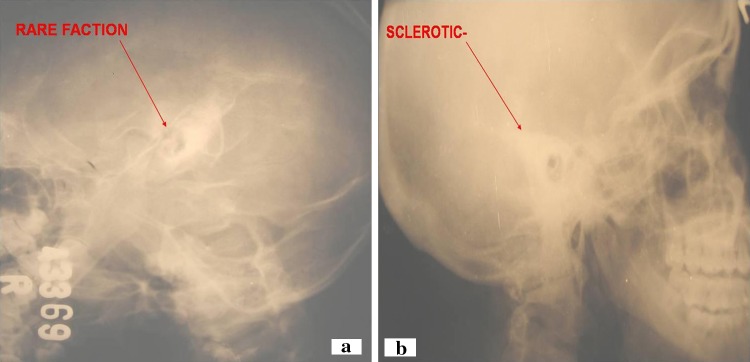
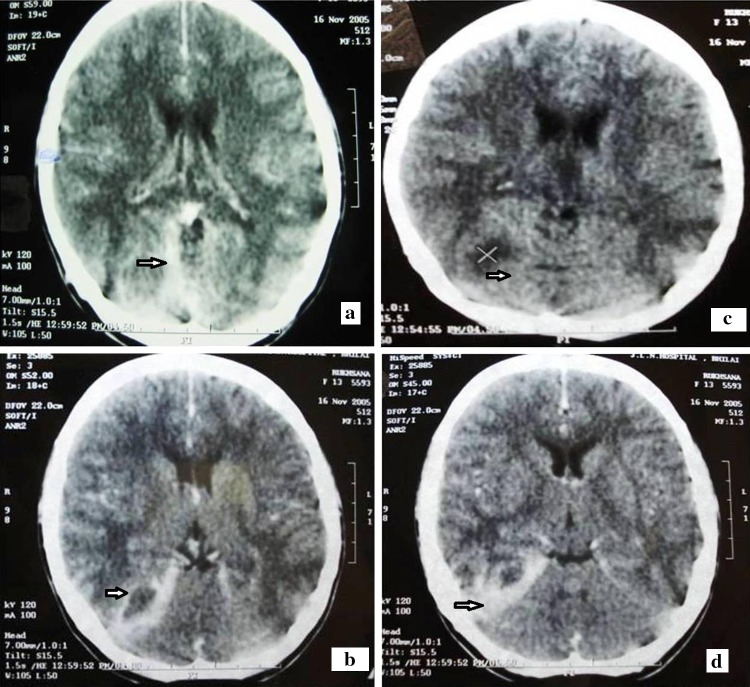
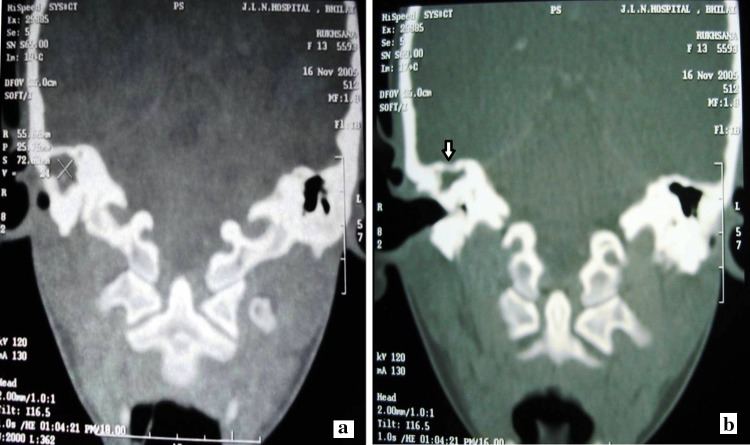
Radiological assessment included X-ray mastoid schuller’s view (Fig. 1a, b) showing Rarefaction in 16 cases, sclerotic in 12 cases and cloudy in three cases whereas CT scan Head (Fig. 2a, b, c, d) and Temporal bone (Fig. 3a, b) was made available in seven cases of which three cases showed posterior fossa collection while four cases revealed temporal collection.
Fig. 1.
X-ray Mastoid Schuller’s view showing a rarefaction in right mastoid and b sclerotic left mastoid
Fig. 2.
Computed tomography (CT) scan of Head, Axial view showing a meningeal enhancement b hypodense area c hypodense area with cerebral oedema and d sigmoid sinus enhancement
Fig. 3.
Computed tomography (CT) scan Temporal bone, coronal view showing a soft tissue density in right middle ear cavity b erosion of the Tegmen plate
Bacterial Organisms
In the IC group only nine cases showed result, out of which six cases were sterile because patients already received IV antibiotics while rest three patients showed growth of Proteus mirabilis on culture. In the EC group seven cases showed Staph aureus, Pseudomonas in four cases, E coli in two cases while seven cases were sterile (Table 3).
Table 3.
Bacterial organisms isolated on culture
| Sr. no. | Intracranial group | Extracranial group | ||
|---|---|---|---|---|
| Organism isolated | No. of cases | Organism isolated | No. of cases | |
| 1 | Proteus mirabilis | 3 | Staphylococcus aureus | 7 |
| 2 | Sterile | 6 | Pseudomonas aerugenosa | 2 |
| E.coli | 2 | |||
| Sterile | 7 | |||
Treatment
In all cases a treatment protocol was followed in our study. (Table 4) The treatment included multiple high dose parenteral antibiotics such as crystalline penicillin (10–20 lakh IU 6 h/day), aminoglycosides (40–80 mg 8 h/day) depending on the age of the patient including inj. chloramphenicol (500 mg 6 h/day) and inj. metronidazole (400 mg 8 h/day) before surgical intervention. The other antibiotics used were inj. Ceftriaxone depending on culture and sensitivity.
Table 4.
Treatment protocol in our study
| Sr. no. | Type of complication | Medical management | Surgical management |
|---|---|---|---|
| 1 | Extracranial complication | IV Antibiotics | Aural T/t − Radical mastoidectomy |
| 2 | Intracranial complication | IV Antibiotics | Intracranial T/t + Aural T/t |
The most common complication in EC group was subperiosteal abscess. Most of the cases were children with extensive cholesteatoma, prolonged ear discharge while three cases were with post aural fistula. These cases required premedicated incision and drainage of post aural abscess along with IV multiple dose antibiotics followed by Canal wall down mastoid surgery.
The 2nd most common EC complication was labyrinthitis. These patients required IV multiple dose antibiotics, labyrinthine sedatives, absolute bed rest with canal wall down tympanomastoidectomy with complete removal of the disease (cholesteatoma, granulation) from middle ear, attic aditus, antrum and mastoid air cell system. The removal of cholesteatoma from fistula site was performed and fistula was sealed.
In EC group patient with Facial nerve paresis, surgical intervention at the earliest possible was carried out. In 95 % (19) of patients radical mastoidectomy was done with removal of the cholesteatoma matrix over the exposed facial nerve. In 80 % (16) of cases horizontal segment of facial nerve was exposed with disease.
Treatment in IC group included multiple high dose parenteral antibiotics, IC drainage and treatment of ear lesion. The multiple dose IV antibiotic therapy was initially given for 48–72 h before IC drainage because IC infection might take place due to osteo-thrombophlebitis and extension along a preformed pathway. In this way the infection process always spreads widely and is very difficult to control if the temporal bone blood supply is cut by early surgical treatment.
IC drainage in temporal lobe and cerebellar abscess was scheduled as soon as the patient’s general condition improved to decrease the anaesthetist risks. The ear surgery i.e. radical mastoidectomy was performed at the time of IC drainage if the patient condition permits. Generally it is delayed for 10–14 days after the IC complication has been controlled.
Meningitis is the second most common complication in our series. The lumbar puncture was done carefully. To check the status of infection again multiple dose intravenous antibiotics were given before ear surgery until meningitis was under control (48–72 h). The radical mastoidectomy was performed in the presence of irreversible pathological changes such as cholesteatoma, granulation and polyp. Simple mastoidectomy was performed in presence of reversible pathological changes such as mild to moderate middle ear mucosa swelling and good aditus drainage.
In patients with perisinus abscess and possible lateral sinus thrombosis, aspiration through sinus wall was attempted. If there was no blood, the upper and lower parts of sigmoid sinus were packed tightly with a pack before the wall of the sinus was incised. These packs were removed on 4th/5th day after surgery.
In all cases with IC complication, patients were treated with radical mastoidectomy because patients follow up is very poor hence it was tried to give the patient disease free ear in a single setting.
Result of Treatment
For IC group no mortality seen in our series while morbidity occurred in 28 % of cases i.e. seven patients, all of them had sensorineural hearing loss. For EC group no mortality seen out of 20 patients, morbidity was seen in 15 % of cases (three patients), out of these two patients had total Facial nerve palsy in spite of surgery, while in one patient profound sensorineural loss was seen.
Otitic facial nerve palsy was encountered in seven cases and all of them underwent surgery. Out of seven cases, two had intact fallopian canal and recovered House brackmann grade 1 postoperatively, while two cases had erosion of horizontal segment of facial nerve with granulation and failed to recover post operatively whereas three patients intraoperatively showed exposed vertical segment of fallopian canal but recovered fully.
Discussion
The prevalence of CSOM with complication in our series was 0.31 % in total, 0.13 % of EC and 0.17 % of IC group respectively. In Thailand, reports from some centres shows decline in prevalence of these complication. The decline could be explained in many ways such as increase in number of ENT surgeons, improvement in standard of living and quality of life of the people [1].
In our series, the common age group of patient with complication was between 5–10 years as compared to age group of 10–20 years seen in other reports [2] Males seem to have a higher preponderance for otogenic complications as compared with females [3, 4]. The probable reason why these complication are still encountered may be related to ignorance about the seriousness of persistent and sometimes offensive ear discharge [3].
The development of subperiosteal abscess with or without fistula leads to reduction of pressure of pus within the middle ear cleft which in turn reduces the chances of infection spreading intracranially. The mastoid antrum is shallower in younger people. It reaches adult thickness by the age of 16 years. Consequently we found younger patients frequently develop mastoid abscess and post aural fistula than IC complication. The facial nerve palsy in CSOM is associated with dehiscence or destruction of the bony facial canal by cholesteatoma or granulation.
Otitic meningitis is the most common IC complication [5, 6]. It is often associated with brain abscess in our series. Therefore CT scan is necessary to rule out IC complication.
Lateral sinus thrombosis in our series had zero mortality as compared to other series [3, 6–8]. The reason behind this is early arrival of the patients and adequate intravenous/oral antibiotics given by local practitioners. None of the patients in our series received any thrombolytics because of risk of dissemination of infected thrombus and its consequences.
Brain abscess is the most common IC complication in our series all are caused by extensive cholesteatoma. Out of these temporal abscess is most commonly found. Timely intervention along with support of neurosurgery department in our hospital and proper antibiotic support gave zero mortality as compared to other series [3, 6, 9]. We suggest that appropriate investigation and early treatment should be made in every patient who presents with fever headache and neck stiffness.
Organisms isolated from otorrhoea reasonably reflect the etiological agent of middle ear infection. Proteus mirabilis, Pseudomonas aerugenosa and Staphylococcus were the most common organisms in our series as in other reports [9, 10].
Multiple dose parenteral antibiotics and hydration therapy for 48–72 h before any surgical procedure are important to control the infective process and to improve general condition of the patient. The antibiotics which were based on culture sensitivity report of aural swab and after consultation with our physician played a vital role in good outcome.
Canal wall down mastoidectomy was done in all cases in our series because of extensive cholesteatoma and taking into consideration a possibility of lack of follow up after surgery as most of the patients were from near by village with a poor economic condition making them unable to bear second surgery.
IC drainage should be done first and aural surgery should be scheduled at the earliest safe time during convalescence which is usually several days to weeks [11]. In our series, Ear surgery was done as an interval procedure, about 48–72 h after medical treatment in life threatening complications and 7–10 days after medical treatment in non life threatening complications, to reduce surgical time and to avoid anaesthetic risks.
Management of lateral sinus thrombosis in our series depends on clinical feature of spiky temperature in preoperative period. We prefer to expose lateral sinus plate in anticipation of an infected thrombus in it. The various types of lateral sinus condition found intraoperatively in our series are as in Table 5.
Table 5.
Types of lateral sinus condition found intraoperatively
| Sr. no | Intraoperative type of lateral sinus wall | Status of blood flow and involvement | No. of cases in our series |
|---|---|---|---|
| 1 | Normal blue sinus wall | Blood flow in sinus verified by needle aspiration | 2 |
| 2 | Dull lustreless sinus wall | Blood could not be aspirated. Soft infected thrombus found in the sinus lumen after opening it. Sinus blood flow encountered after removal of clot | 1 |
| 3 | Thick sinus wall with perisinus granulation | Sinus outline was apparent proximally and distally with/without scanty intrasinus pus, no intrasinus blood flow | 2 |
| 4 | Extensive perisinus granulation with perisinus abscess | Osteitic bone all around the sinus. Sinus outline, indistinguishable. Involvement of transverse sinus proximally and internal jugular vein distally creates difficulty in establishing proximal blood flow | Nil |
Morbidity in our series is mainly sensorineural hearing loss in 17.77 % of cases (eight cases). The mortality in our series is zero as compared to other series [1, 3, 4, 6].
Conclusion
Otogenic complication of CSOM still occur in spite of modern antibiotics though have declining incidences (Table 6).
Table 6.
Master chart
| Sr. no | Pt name | Age/sex | Ear pathology | Extracranial complication | Intracranial complication |
|---|---|---|---|---|---|
| 1 | Nageshwar | 28 years/m | CSOM Rt | – | Rt Temporal lobe Abscess |
| 2 | Amit soni | 6 years/m | CSOM Lt | – | Lt Temporal lobe Abscess |
| 3 | Ajay | 10 years/m | CSOM Lt | – | Meningitis |
| 4 | Dolly | 10 years/F | CSOM Lt | Post aural abscess with fistula, 7th CN palsy | – |
| 5 | Tikaram | 27 years/m | CSOM Rt | – | Meningitis , subdural empyema |
| 6 | Ansuila | 37 years/F | CSOM Lt | Post aural abscess | – |
| 7 | Hemlata | 7 years/F | CSOM Rt | Post aural abscess | – |
| 8 | Sunil | 20 years/m | CSOM Lt | – | Meningitis , Temporal lobe abscess |
| 9 | yashoda | 50 years/F | CSOM Rt | Labyrinthitis | – |
| 10 | T. Bhagyani | 20 years/F | CSOM Rt | Labyrinthitis | – |
| 11 | Vandana | 9 years/F | CSOM Rt | – | Lateral sinus thrombophlebitis |
| 12 | Geeta | 15 years/F | CSOM Lt | Post aural Abscess with fistula | – |
| 13 | Gangaram | 45 years/m | CSOM Rt | Labyrinthitis, 7th CN palsy | – |
| 14 | Shatrughan | 26 years/m | CSOM Lt | Lateral sinus thrombosis | |
| 15 | Moman | 15 years/m | CSOM Lt | – | Temporal lobe abscess |
| 16 | Romesh | 7 years/m | CSOM Rt | Post aural Abscess | – |
| 17 | Bema | 10 years/F | CSOM Lt | Post aural Abscess with fistula | – |
| 18 | Mehaterin bai | 15 years/F | CSOM Rt | – | Lateral sinus thrombosis |
| 19 | Brijlal | 52 years/m | CSOM Rt | Labyrinthitis | – |
| 20 | Omprakash | 14 years/m | CSOM Lt | – | Cerebellar Abscess |
| 21 | Devendra kumar | 21 years/m | CSOM Rt | – | Meningitis |
| 22 | Rajesh | 5 years/m | CSOM Lt | – | Extradural abscess, meningitis |
| 23 | Yogesh | 23 years/m | CSOM Lt | – | Temporal lobe abscess |
| 24 | Leela | 36 years/F | CSOM Rt | – | Lateral sinus thrombophlebitis with perisinus collection |
| 25 | Gayatri | 21 years/F | CSOM Rt | Labyrinthitis | – |
| 26 | Shivcharan | 10 years/m | CSOM Lt | – | Temporal lobe abscess |
| 27 | Ahilyabai | 13 years/F | CSOM Lt | – | Cerebellar abscess |
| 28 | Goma | 26 years/m | CSOM Rt | – | Temporal lobe abscess |
| 29 | Manish | 19 years/m | CSOM Rt | Mastoid abscess, 7th CN palsy | – |
| 30 | Murth chandu | 55 years/m | CSOM Lt | – | Lateral sinus thrombophlebitis with perisinus collection |
| 31 | K. S. Thakur | 44 years/m | CSOM Rt | 7th CN Palsy | – |
| 32 | Jatin | 46 years/m | CSOM Lt | 7th CN Palsy | – |
| 33 | Baby P Monali | 9 years/F | CSOM Lt | 7th CN Palsy | – |
| 34 | Shaukat Ahmed | 30 years/m | CSOM Rt | Labyrinthitis | – |
| 35 | Narmada | 21 years/F | CSOM Lt | Post aural abscess, 7th CN Palsy | – |
| 36 | khemu | 9 years/m | CSOM Lt | – | Meningitis |
| 37 | P. Geeta | 5 years/F | CSOM Rt | – | Extradural collection |
| 38 | Rukhsana | 20 years/F | CSOM Lt | – | Temporal lobe abscess |
| 39 | Girdhar | 35 years/F | CSOMRt | – | Subdural collection |
| 40 | Suresh | 40 years/m | CSOM Lt | Labyrinthitis | – |
| 41 | Neelash | 10 years/m | CSOM Lt | Subperiosteal abscess | – |
| 42 | Rajkishore | 23 years/m | CSOM Lt | – | Temporal lobe abscess |
| 43 | Imran | 29 years/m | CSOM Lt | Labyrinthitis | – |
| 44 | Bhuneshwar | 28 years/m | CSOM Lt | – | Cerebellar abscess |
| 45 | K. P. Malti | 12 years/F | CSOM Lt | – | Cerebellar abscess |
The decreasing mortality in our institution is largely due to modern antibiotic therapy, early diagnosis based on clinical features, CT scan and culture sensitivity and early intervention as and when required.
It is hoped that this study might give some options and awareness to all otorhinolaryngologists that will result in early diagnosis, prompt treatment and further reduction of mortality.
Contributor Information
Neeta Sharma, Email: dr1neetasharma@gmail.com, Email: neetasharma@sail-bhilaisteel.com.
Ashwin Ashok Jaiswal, Email: ash1978jaiswal@gmail.com, Email: ash1978jaiswal@yahoo.com.
Praveer Kumar Banerjee, Email: drpraveer_31@yahoo.co.in.
Amrish Kumar Garg, Email: drakgarg19@yahoo.co.in.
References
- 1.Kangsanarak J, Fooanant S, Ruckphaopunt K, et al. Extracranial and intracranial complications of suppurative otitis media; report of 102 cases. J Laryngol Otol. 1993;107(11):999–1004. doi: 10.1017/S0022215100125095. [DOI] [PubMed] [Google Scholar]
- 2.Pennybacker J, Dixon JW, Fulton CJ, Dawes JD. Discussion on intracranial complications of otogenorigin. Proc R Soc Med. 1961;54:309–320. [PMC free article] [PubMed] [Google Scholar]
- 3.Dubey SP, Larawin V. Complications of chronic suppurative otitis media and their management. Laryngoscope. 2007;117(2):264–267. doi: 10.1097/01.mlg.0000249728.48588.22. [DOI] [PubMed] [Google Scholar]
- 4.Singh B, Maharaj TJ. Radical mastoidectomy—its place in otitic intracranial complications. J Laryngol Otol. 1993;107(12):1113–1118. doi: 10.1017/S0022215100125435. [DOI] [PubMed] [Google Scholar]
- 5.Osma U, Cureoglu S, Hosoglu S. The complications of chronic otitis media: report of 93 cases. J Laryngol Otol. 2000;114(02):97–100. doi: 10.1258/0022215001905012. [DOI] [PubMed] [Google Scholar]
- 6.Samuel J, Fernandes CM, Steinberg JL. Intracranial otogenic complications: a persisting problem. Laryngoscope. 1986;96(3):272–278. doi: 10.1288/00005537-198603000-00007. [DOI] [PubMed] [Google Scholar]
- 7.Syms MJ, Tsai PD, Holtel MR. Management of lateral sinus thrombosis. Laryngoscope. 1999;109(10):1616–1620. doi: 10.1097/00005537-199910000-00013. [DOI] [PubMed] [Google Scholar]
- 8.Kutluhan A, Kiriş M, Yurttaş V, Kiroğlu AF, Unal O. When can lateral sinus thrombosis be treated conservatively? J Otolaryngol. 2004;33(2):107–110. doi: 10.2310/7070.2004.02094. [DOI] [PubMed] [Google Scholar]
- 9.Kangsanarak J, Navacharoen N, Fooanant S, Ruckphaopunt K. Intracranial complications of suppurative otitis media: 13 years’ experience. Am J Otol. 1995;16(1):104–109. [PubMed] [Google Scholar]
- 10.Mathews TJ, Oliver SP. Bacteriology of mastoiditis, 5 year experience. J Laryngol Otol. 1988;102:397–398. doi: 10.1017/S0022215100105183. [DOI] [PubMed] [Google Scholar]
- 11.Myers EN, Ballantine HT. The management of otogenic brain abscess. Laryngoscope. 1965;75:273–288. doi: 10.1288/00005537-196502000-00007. [DOI] [PubMed] [Google Scholar]