Abstract
Study Objectives:
To compare the efficacy of guided online and individual face-to-face cognitive behavioral treatment for insomnia (CBT-I) to a wait-list condition.
Methods:
A randomized controlled trial comparing three conditions: guided online; face-to-face; wait-list. Posttest measurements were administered to all conditions, along with 3- and 6-mo follow-up assessments to the online and face-to-face conditions. Ninety media-recruited participants meeting the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) criteria for insomnia were randomly allocated to either guided online CBT-I (n = 30), individual face-to-face CBT-I (n = 30), or wait-list (n = 30).
Results:
At post-assessment, the online (Cohen d = 1.2) and face-to-face (Cohen d = 2.3) intervention groups showed significantly larger treatment effects than the wait-list group on insomnia severity (insomnia severity index). Large treatment effects were also found for the sleep diary estimates (except for total sleep time), and anxiety and depression measures (for depression only in the face-to-face condition). Face-to-face treatment yielded a statistically larger treatment effect (Cohen d = 0.9) on insomnia severity than the online condition at all time points. In addition, a moderate differential effect size favoring face-to-face treatment emerged at the 3- and 6-mo follow-up on all sleep diary estimates. Face-to-face treatment further outperformed online treatment on depression and anxiety outcomes.
Conclusions:
These data show superior performance of face-to-face treatment relative to online treatment. Yet, our results also suggest that online treatment may offer a potentially cost-effective alternative to and complement face-to-face treatment.
Clinical Trial Registration:
Clinicaltrials.gov, NCT01955850.
Commentary:
A commentary on this article appears in this issue on page 13.
Citation:
Lancee J, van Straten A, Morina N, Kaldo V, Kamphuis JH. Guided online or face-to-face cognitive behavioral treatment for insomnia: a randomized wait-list controlled trial. SLEEP 2016;39(1):183–191.
Keywords: CBT-I, face-to-face, insomnia, internet
Significance.
This is the first published study to compare guided online and individual face-to-face cognitive behavioral treatment for insomnia (CBT-I) to a wait-list condition. Whereas both treatments were significantly more effective than the wait-list condition, face-to-face treatment outperformed online treatment. These findings may guide clinicians in choosing the right treatment format for patients with insomnia if both treatments are available to the patient. Yet, if access to face-to-face treatment is limited, online treatment may be considered as it can significantly reduce insomnia complaints. However, our results need to be seen as preliminary until replicated in future clinical trials.
INTRODUCTION
Insomnia is a common disorder with a prevalence of about 10% in the general population.1 Individuals suffering from insomnia have difficulty initiating and/or staying asleep, have these complaints for at least 3 mo, and suffer from negative daytime consequences.2–5 Furthermore, insomnia is associated with an increased risk of anxiety and depression,6–8 suicidality,9 and cardiovascular diseases.10
Sleep medication is the most widely used treatment option for insomnia. Although sleep medication is effective in the short term, it is also associated with side effects,11 and the long-term efficacy of sleep medication has not been established.12 An alternative treatment option is cognitive behavioral treatment for insomnia (CBT-I); this psychological treatment has equal short-term effects12,13 and superior long-term effects12 as medication. Recently it was demonstrated that the acute phase of sleep restriction in CBT-I is also associated with side effects such as daytime sleepiness and objective performance impairment. However, these side effects are not maintained at 3-mo follow-up.14
Another issue with CBT-I is that it requires considerable time investment of trained psychologists that may not always be readily available.15 A possible solution to cut costs (i.e., time investment) and increase accessibility is to provide the CBT-I via the internet.15 In recent years several trials were published on online CBT-I. Overall the results were encouraging with recent meta-analyses identifying moderate to large effects sizes for these online treatments.16,17 Furthermore, it was established that such online interventions should best be delivered in a guided format (i.e., with some form of Email support)18 and that this guidance is possible with a low level of clinical training.19 For insomnia, several online treatment studies observed treatment effects comparable to face-to-face treatment.20–23 In other clinical domains there has been a surge in research on the comparison between face-to-face and online psychological interventions. Recent meta-analyses on somatic and psychiatric disorders have concluded that face-to-face and online treatments were equally effective.24,25 If these findings would also hold for insomnia, online treatments could be a major advancement in terms of accessibility and cost-effectiveness of interventions.
To our knowledge, only one published study directly compared online CBT-I and face-to-face group treatments for insomnia, utilizing a noninferiority trial design.26 In line with the studies on somatic and psychiatric disorders, online CBT-I was found to be non-inferior to group-administered CBT-I. No published studies have reported on the comparison between online CBT-I and individual face-to-face treatment. In this article, we report the results of a randomized wait-list controlled trial comparing online CBT-I to individual face-to-face CBT-I. We hypothesized that: (1) online and face-to-face treatment ameliorate insomnia complaints compared to a wait-list condition, and (2) online and face-to-face delivery methods do not differ considerably in treatment effect.
METHOD
Participants
Participants were recruited from April 2013 to January 2014 via a popular scientific website and a Facebook campaign. Enrollment took place in October 2013 and January 2014. Inclusion criteria were: (1) insomnia disorder according to Diagnostic and Statistical Manual of Mental Disorders (DSM-5)2; (2) insomnia severity index (ISI) score of 10 or higher,27 (3) being awake subjectively for at least 30 min a night at least 3 nights a week, and (4) being 18 y or older. Exclusion criteria were: (1) possible sleep apnea (determined with a subscale of the SLEEP-50, cutoff > 1528), (2) shift work, (3) pregnancy, (4) earlier CBT-I, (5) start of psychotherapy in the past 6 mo, (6) current major depressive disorder based on the Structured Clinical Interview for DSM-IV disorders (SCID-I; administered during the telephone screening), (7) alcohol abuse (more than three glasses of alcohol a day for at least 21 d/mo), (8) marijuana abuse (use more than once a week), (9) self-reported diagnosis of schizophrenia or psychosis, (10) or current suicidal plans. An initial group of 183 interested individuals completed an informed consent form and started the online questionnaire.
Of these, 47 potential participants were excluded based on the online assessment. Next, a psychologist conducted a telephone screening interview that included an assessment on DSM-5 insomnia and the SCID-I for current depression. Figure 1 presents a flowchart of the recruitment, and details the reasons for exclusion. The final 90 participants were randomly assigned to online treatment (n = 30), face-to-face treatment (n = 30), or a wait-list condition (n = 30). Baseline characteristics and descriptive statistics of the sample are displayed in Tables 1 and 2.
Figure 1.
Flowchart.
Table 1.
Demographic and clinical characteristics at baseline.
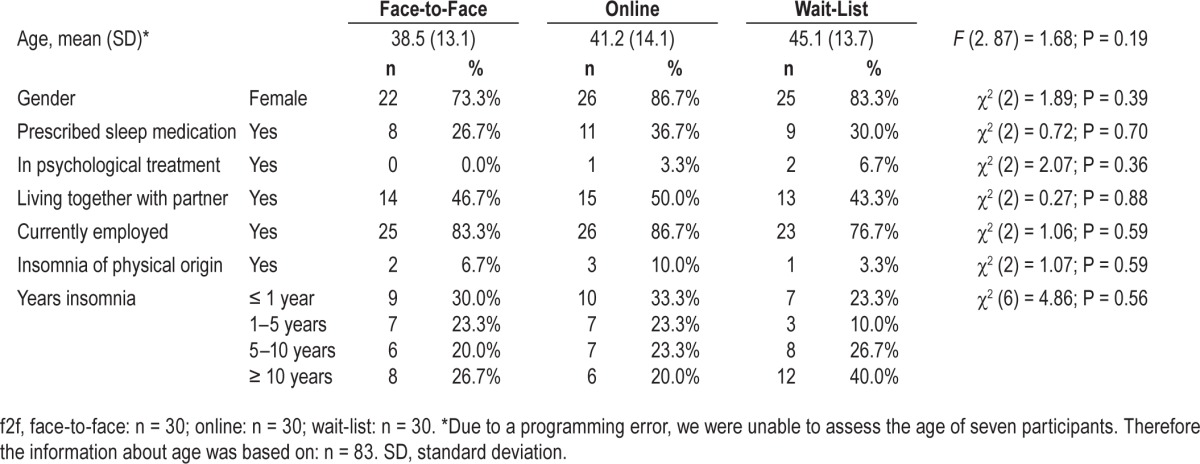
Table 2.
Pretest-and posttest means with corresponding Cohen d scores for the online, face-to-face (f2f), and wait-list (wl) condition.

Power
This study was powered for the detection of a within-between interaction effect size of f2 = 0.20. Based on an alpha of 0.05 and a power of 0.8, detecting this effect size requires a cell size of n = 22. In consideration of an expected attrition rate, we included 30 participants per group.
Materials
Online questionnaires
Demographic characteristics were assessed at baseline (Table 1). We also assessed treatment preference at baseline and treatment satisfaction at post-assessment.
Insomnia complaints were measured with a Dutch translation of the seven-item ISI. The ISI is a widely used measure to index changes in insomnia severity, and favorable psycho-metric properties have been documented.29,30 The total score ranges from 0 (no insomnia) to 28 (severe insomnia). A cutoff of 10 was determined as optimal to indicate clinical levels of insomnia27 and was therefore used in this study. Surprisingly, in the current study the internal consistency (Cronbach alpha) of the ISI was 0.22. After deleting the first item (regarding difficulty falling asleep), the Cronbach alpha rose to 0.57 (which is comparable to the α = 0.61 that was found in a validation study of the online version of the original ISI.31 For comparability with other publications, we decided to report on the full ISI score. We also performed all the analyses without the first item of the ISI and these results were highly similar to the full seven-item ISI (see Tables S1 and S2, supplemental material).
Depressive symptoms were measured using a Dutch translation of the 20-item Centre of Epidemiological Studies Depression scale (CES-D, range = 0, no depressive symptoms, to 60, high depressive symptoms).32,33 The original scale has shown strong reliability, and the psychometric properties of the Dutch scale are comparable to that of the original version (α = 0.79– 0.92).32,33 In the current study, the Cronbach alpha was 0.88.
Anxiety symptoms were assessed with the Dutch version of the seven anxiety items of the Hospital Anxiety and Depression Scale (HADS).34,35 The total score ranges from 0 (no symptoms of anxiety) to 21 (severe symptoms of anxiety). The internal consistency of the HADS is good (α = 0.84 in the Dutch version34). In the current study, the Cronbach alpha was 0.84.
A subscale of the SLEEP-5028 was used to exclude patients with possible apnea. The apnea subscale has eight items (α = 0.51), and the total scale ranges from 8 (no apnea indication) to 32 (severe apnea indication).
Online sleep diary
We used the Dutch translation of the consensus sleep diary.36 Participants kept a sleep diary for 7 d and recorded time to bed, time they tried to go to sleep, time of final awakening, time out of bed, sleep onset latency (SOL), wake after sleep onset (WASO), terminal wakefulness (TWAK), number of nocturnal awakenings (NWAK), sleep quality (1 = “very bad” to 5 = “very good”), and use of sleep medication. From these variables, the time in bed (TIB = final arising time − time to bed), total sleep time (TST = TIB − SOL – WASO – TWAK), sleep efficiency (SE = [TST / TIB] × 100), and total wake time (TWT = SOL + WASO + TWAK) were calculated.
Interventions
The online and face-to-face CBT-I treatments had equal content and included the following modules of standard multicomponent treatment for insomnia: (1) psychoeducation; (2) progressive muscle relaxation; (3) sleep hygiene; (4) sleep restriction (i.e., restricting time in bed to actual sleeping time; the sleep restriction parameters37 are reported in Table S3, supplemental material); and (5) cognitive exercises (i.e., challenging the misconceptions about sleep).38 The modules were offered in the same order in both treatment conditions.
The online program, first described in the study of Lancee and colleagues,18 features an integrated diary that gives visual feedback on participants' SE and total time spent awake. It enables the provision of feedback on treatment progress and assigned exercises. The participants first read information regarding the module, then do their homework, and then fill out online forms based on their exercises. Access to the next module is gained only if the previous one is completed. Feedback is provided by Email based on these exercises, forms, and on the sleep diary. In the current study, personal feedback was provided by Master level students of psychology, and supervised by the first author.
The online treatment comprised six weekly sessions and participants received feedback up to 8 w. In the first session, participants started with psychoeducation and a sleep diary, which was continued throughout treatment. In the second session, sleep hygiene and progressive muscle relaxation were covered. After reading the sleep hygiene section, participants wrote down their intentions for the following week; the coach used this for his/her feedback. Progressive muscle relaxation exercises were provided in mp3 downloads and participants reported their intended frequency. In the third session, participants started with sleep restriction. They used the guidelines to form their sleep window for the consecutive week. The coach assessed this sleep window and gave feedback based on the form and the sleep diary (e.g., “you are planning to spent 7 h in bed the following week but based on your diary it may be better to spent 6 h a night in bed.”). For the remainder of the program the coach and participants discussed sleep windows every week (up to 8 w). Cognitive exercises started in the fourth session. In these exercises common misconceptions were discussed and participants were asked to fill out a thought form with their original and challenged misconception (e.g., “I must sleep 8 h a night for full functioning next day” into “even if I sleep only 6 h tonight I will be able to work quite well tomorrow”). In the fifth session, again sleep restriction and cognitive exercises were covered. In the sixth and final session, sleep restriction was covered for the last time and a plan for the future was made.
In the face-to-face condition, all six individual treatment sessions were administered by a psychologist specialized in insomnia treatment. In total, six treatment sessions of 45 min were offered over a maximum time span of 12 w. The sessions followed the same order as the online treatment, with the only exception that in the face-to-face condition sleep hygiene was started in the first week. Furthermore, stimulus control was covered more elaborately in session two.
Procedure
Participants who met study criteria completed questionnaires, and an online sleep diary on 7 consecutive days. Participants were then randomized to either (1) guided online treatment; (2) individual face-to-face treatment; or (3) the wait-list condition. We used a block randomization procedure with blocks of 30. Randomization results were not blinded to the investigators and participants. Twelve weeks after the randomization, participants in all conditions were invited to complete post-assessment questionnaires and again the 7-night sleep diary. After completing the post-assessment sleep diary, participants in the wait-list condition received the online CBT-I treatment. The people participating in the online and face-to-face condition also received 3- and 6-mo follow-up measurements. The study was approved by the internal Ethical Review Board of the University of Amsterdam and was registered at Clinicaltrials.gov (NCT01955850).
Statistical Analysis
The effects of the intervention were tested using multilevel regression analysis, which lends itself well for intention-to-treat analyses, and enables the inclusion of participants with one measurement only.39
Analyses of variance detected baseline differences in depressive symptoms, F (2, 80) = 4.25; P = 0.02. A post hoc test identified that participants in the wait-list group (mean = 21.5; standard deviation [SD] = 8.0) had higher scores on depressive symptoms than people in the face-to-face condition (mean = 15.7; SD = 7.6; P = 0.02). Furthermore, participants in the online condition who completed the post-assessment questionnaire had lower depressive symptoms at baseline (mean = 16.0; SD = 6.5) than those who did not complete the questionnaire (mean = 27.3; SD = 9.3), F (1. 28) = 9.29; P = 0.005. This was also observed at the 6-month follow-up (mean = 22.0; SD = 9.8 versus mean = 15.6; SD = 6.0), F (1. 28) = 4.86; P = 0.04. Therefore, baseline depressive symptoms were added as a covariate in the multilevel regression analyses.
We also used multiple imputations based on the missing at random assumption to insert missing cases on the questionnaire and diary data.40 Using a predictive mean matching procedure we generated 10 separate datasets. The values in Tables 2 and 3 are based on these imputed datasets. Between-group Cohen ds were calculated on the difference in change scores divided by the pooled standard deviation of the change. A Cohen d of 0.20 indicates a small, 0.50 a moderate, and 0.80 a large effect.43 To enhance comparability with other studies we also included the Cohen d based on the pooled baseline standard deviation in Table S4 (supplemental material). A significance level of P < 0.05 (two-sided) was used throughout the study.
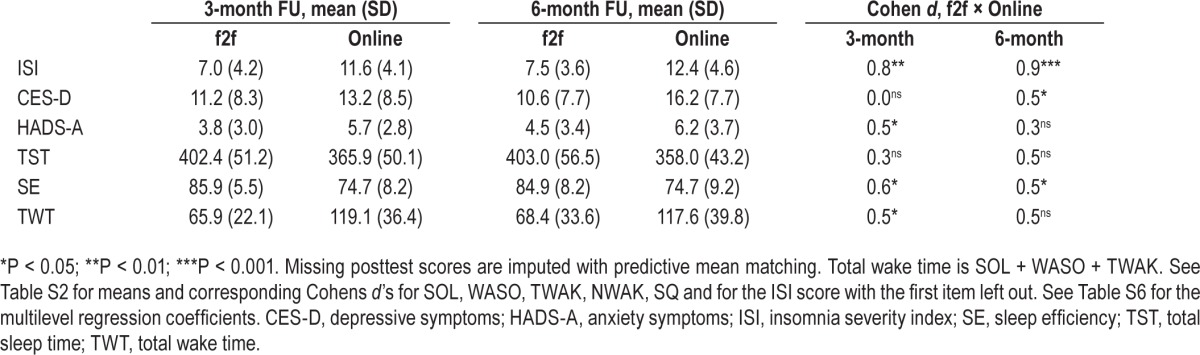
Table 3.
Three- and 6-month follow-up means with corresponding Cohen d scores for the online and face-to-face (f2f) condition.
RESULTS
Treatment Preference
When asked about treatment preference before randomization, 47 participants (52.2%) named online treatment, 70 (77.8%) face-to-face treatment, 39 (43.3%) treatment by the general practitioner, and 14 (15.6%) sleep medication as feasible options (checking more than one option was possible). Significantly more participants were interested in receiving face-to-face treatment than in online treatment (P = 0.003).
Completion Rates, Satisfaction and Nonresponse
In the online condition, 15 completed all six sessions, four completed five sessions, three completed four sessions, one completed three sessions, five completed two sessions, and two completed zero sessions. Accordingly, 22 (73.3%) participants completed at least four sessions (which has previously been described as an adequate dose of this intervention18), and 15 participants (50.0%) completed all six sessions. On average, the students spent 90.7 min (SD = 47.9) on giving feedback per participant for the full online treatment (i.e., all six lessons).
In the face-to-face condition, 21 followed all six sessions, five followed five sessions, two followed four sessions, one followed two sessions, and one followed zero sessions. Accordingly, 28 participants (93.3%) attended at least four sessions, with 21 (70.0%) attending all six sessions. This resulted in an average treatment time of 241.5 min (SD = 60.8). The completion rates did not significantly differ between the online and face-to-face conditions, four session: χ2 (1) = 4.32; P = 0.08; all sessions: χ2 (1) = 2.50; P = 0.19. At post-assessment, mean satisfaction ratings were statistically different, F (1. 50) = 17.71; P < 0.001 (range was 1, not satisfied at all, to 10, very satisfied), with a mean score of 6.8 (SD = 2.3) in the online condition, and of 8.8 (SD = 1.0) in the face-to-face condition.
The post-measure was completed by 87% to 97% of the participants. Figure 1 presents the percentages among groups and the completion rates for the diary and the follow-ups. As mentioned in the statistical analysis section of this article, participants in the online condition were less likely to fill out post-assessment questionnaires if they had high depressive symptoms at baseline.
Efficacy: Online and Face-to-Face Versus Wait-List
Both the online (Cohen d = 1.0; P < 0.001) and face-to-face (Cohen d = 2.3; P < 0.001) conditions showed stronger reductions at post-assessment on insomnia severity (ISI) than the wait-list condition (Figure 2). The same pattern was observed for anxiety (Cohen d = 0.8 / 1.2; P < 0.01), SE (Cohen d = 0.6 / 0.8; P < 0.05) and TWT (Cohen d = 0.8 / 0.9; P < 0.01). With regard to depressive symptoms, face-to-face treatment was associated with significantly lower scores at post-assessment (Cohen d = 1.2; P < 0.001) than the wait-list condition, whereas no significant difference was found between online treatment and wait-list at post-assessment. Finally, the active conditions did not significantly differ from the wait-list condition at post-assessment regarding TST (Cohen d = 0.4, P = 0.17 and Cohen d = 0.3, P = 0.21 for online and face-to-face treatment, respectively). See Table 2 for all means, corresponding Cohen ds, and significance levels as well as Table S5 (supplemental material) for all regression analyses. The data on the treatment completers sample showed highly similar effects to the intent-to-treat sample (Table S6, supplemental material). Other sleep diary measures are reported in the supplemental material (SOL, WASO, TWAK, NWAK and SQ; Table S1).
Figure 2.

Insomnia severity index scores on all time points for face-to-face, online and wait-list groups. The figure is based on the multiple imputation data. Error bars represent SEM.
Efficacy: Online Versus Face-to-Face
As compared to patients in the online condition, those in the face-to-face condition reported significantly lower ISI scores at post-assessment (Cohen d = 0.9), 3-mo (Cohen d = 0.8), and 6-mo follow-up assessments (Cohen d = 0.9 all Ps < 0.01), respectively (see Tables 2 and 3, Figure 2). Further, face-to-face treatment was significantly more effective in reducing comorbid depressive symptoms at post-assessment (Cohen d = 0.7; P < 0.05), and at the 6-mo follow-up assessment (Cohen d = 0.5; P < 0.05); for anxiety differences were marginally significant at the post-assessment (Cohen d = 0.4; P = 0.06), and significant at the 3-mo follow-up (Cohen d = 0.5; P < 0.05). At post-assessment, no difference was observed for the sleep diary, but the face-to-face intervention was more effective at the 3-mo (SE: Cohen d = 0.6; TWT: Cohen d = 0.5; P < 0.05), and 6-mo follow-up assessments (SE: Cohen d = 0.5; P < 0.05; Tables 2, 3, S1, S2, S7, and S8, supplemental material).
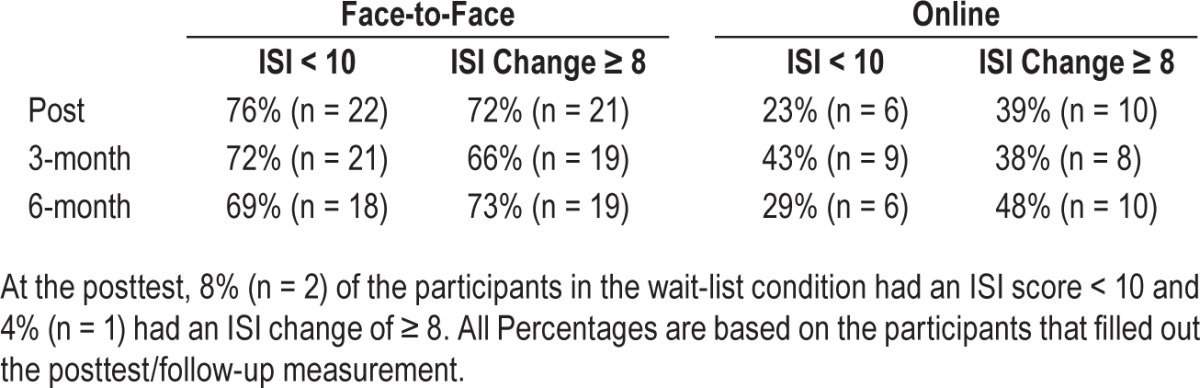
Clinical Change
Table 4 displays the insomnia cutoff scores (ISI < 10) and ISI clinical change scores (ISI change ≥ 8) for all time points and conditions.
Table 4.
Insomnia severity index cutoff (< 10) and clinical change scores (≥ 8) on the posttest, 3- and 6-month follow-up.
Medication and Use of Other Treatment during the Trial
Of the participants who completed the post-assessment, the following numbers used prescribed sleep medication: online, n = 6 (23.1%), face-to-face, n = 6 (20.7%), wait-list, n = 10 (38.5%). The proportions did not significantly differ from each other, χ2 (2) = 2.51; P = 0.29.
The following participants sought other treatment during the trial: online, n = 4 (13.3%; one fitness, one a psychologist, and two sleep medication), face-to-face, n = 1 (3.3%; psychologist), wait-list, n = 8 (26.7%; four sleep medication, two a general practitioner, one a psychologist, and one mindfulness).
Deterioration at Post-Assessment
At post-assessment, two participants (6.7%) in the online condition and six participants (20.0%) in the wait-list condition reported higher ISI scores at posttreatment than at pretreatment. None of the deteriorations were clinically meaningful (change ISI ≥ 8) and no participant in the face-to-face condition reported higher ISI scores at post-assessment. No adverse events were reported by any participant.
DISCUSSION
In this study we investigated the efficacy of a guided online treatment and a face-to-face treatment for insomnia. As expected, both interventions were more effective than the wait-list group at post-assessment on insomnia severity (ISI), TWT, SE, and anxiety. Face-to-face treatment (but not online treatment) was further effective in reducing comorbid depressive symptoms as compared to the wait-list. No differences were observed between the active conditions and the wait-list on TST.
Contrary to our expectation, face-to-face treatment yielded a much stronger effect on insomnia severity (ISI) than the online treatment. Effect size differences between the two interventions were large at all three measurement points following treatment (Cohen d = 0.9). Face-to-face treatment was also superior in terms of clinical change, with about 70% of the participants achieving clinically meaningful changes compared to about 40% of the participants in the online treatment. The same pattern held for the remission rates. About 70% of the participants remitted in the face-to-face treatment, whereas 20% to 40% did (depending on which measurement) in the online treatment.
The effects on the sleep diary measures were less pronounced. No differences emerged between the two intervention conditions at post-assessment. However, follow-up results revealed that participants in the face-to-face treatment reported more favorable scores in SE (both 3 mo and 6 mo following treatment) and TWT (3 mo following treatment only) than participants in the online intervention. To illustrate, these effect sizes translate to an 11% SE improvement at 6-mo follow-up in the online condition and an 18% improvement in the face-to face condition.
The superiority of face-to-face treatment was also observed with regard to comorbid anxiety and depressive symptoms. A direct comparison of the active conditions revealed that face-to-face treatment was more effective in reducing depressive symptoms as measured at the end of treatment and 6 mo afterward (with no difference found 3 mo following treatment). Face-to-face treatment was found to be more effective than online treatment in addressing comorbid anxiety only at the 3-mo follow-up.
Taken together, the results of this trial suggest that face-to-face treatment was substantially more effective than the online counterpart. Accordingly, our findings are not in line with previous clinical trials on online treatment for somatic and other psychiatric disorders.24,25 Furthermore, they are at odds with several studies showing that online treatment effects for insomnia are up to par with face-to-face delivery,20–22 and a study26 comparing online and group treatment for insomnia directly. However, in the latter study,26 group treatment instead of face-to-face treatment was investigated, and whether group treatment is equivalent to face-to-face treatment remains unanswered.42 A comparison of within-group effects indicated that the online intervention in the study by Blom and colleagues26 was somewhat more effective than in the current study (Cohen d = 1.8 compared to Cohen d = 1.5 in the current study), whereas the opposite was true for the face-to-face intervention (Cohen d = 2.1 compared to Cohen d = 2.8 in the current study).
To appraise the implications of these findings, several aspects of the current comparative trial warrant discussion. Conceivably, the difference in efficacy between the online and face-to-face treatments in our study may be explained by the large difference in time investment associated with both versions of treatment (242 min face-to-face treatment versus 91 min for online treatment). Another explanation may be that, prior to treatment, fewer participants were motivated for online than for face-to-face treatment (52% and 78%, respectively). Moreover, the face-to-face treatment was delivered by an insomnia expert, whereas the online treatment was provided by (supervised) graduate students with limited experience in psychotherapy.
Accordingly, the current study should not be mistaken for a true test of whether it is possible to achieve similar treatment effects with different delivery formats. However, we selected this design to examine the extent to which online treatment can produce significant treatment effects at low costs (i.e., limited time investment and low level of clinical training). Moreover, had we increased the time investment or used insomnia experts, we believe the ecological validity of the comparison would have suffered. Furthermore, our design was in line with previous online CBT-I trials, including our own, that found large treatment effects with feedback provided by students22 or even fully automated feedback.20,21 Apart from the feedback delivery, available online treatments are rather similar with regard to the content (albeit not with the same level of design and usage of media possibilities such as videos and animations). However, it should be noted that for insomnia self-help, provision of support seems essential to reaching large effects,18 and the effect of support appears to be mediated by an increased use of the most important treatment methods such as sleep restriction.43 In sum, the quality and intensity of the provided feedback may substantially affect outcome.
A further candidate explanation for the difference in treatment effect may be that our online treatment was not up to par with previous reported studies. However, this seems unlikely, as the current online treatment was tested in a previous trial18 and yielded treatment effects on insomnia severity that were large (Cohen d = 1.0), as compared to the wait-list condition, and commensurate with those reported in a meta-analysis concerning online treatment for insomnia (Cohen d = 0.9).16 Moreover, we found effect sizes for the sleep diary that were also in line with the effects reported in two meta-analyses.16,17 However, larger effects have been reported in other single trial studies.20,21,26 Additionally, the effects sizes regarding anxiety (Cohen d = 0.8) and depressive outcomes (Cohen d = 0.4) were similar or better than in previous studies.22,44–46
A final potential explanation for the differential effects might be that the observed effects in the face-to-face treatment are exceptional. Indeed, the current face-to-face treatment was delivered by an experienced insomnia expert under optimal conditions. The current treatment effects on insomnia severity (ISI) were superior to the already large effect in the group treatment in the study by Blom et al.26 and much larger than what we found in a recent meta-analysis concerning all CBT-I studies (between group Cohen d = 2.3 versus Cohen d = 1.2).47 However, treatment effects on insomnia severity similar to those observed in the current study have been reported previously48,49 and effects on the sleep diary were in line with the effects found in meta-analyses.13,47 Notwithstanding, the use of only one therapist reduces the external validity and calls for a replication study in which the psychologists are not insomnia experts (but receive standard CBT-I training before the trial).
The following limitations of the study need to be addressed. First, the ISI scale suffered from low internal consistency in our sample. However, the analyses with one item left out produced a similar internal consistency result as the data on the original ISI. Second, as a result of the modest sample size, the presented study had limited power to detect differences, which may be particularly relevant to the sleep diary outcomes. Third, a wait-list is not the optimal control condition. An online placebo treatment such as employed in the study of Espie and colleagues21 or a face-to-face placebo control (e.g., sleep hygiene) would have been very informative. Fourth, objective sleep measurements such as polysomnography would have enhanced our findings, but this measurement would have required some degree of additional interaction which could have compromised the online nature of the treatment. As the comparison of online versus face-to-face treatment was the primary purpose of this study, we chose to refrain from these measurements. Fifth, because restless legs syndrome is associated with insomnia,50 it could have been assessed in the screening. Sixth and finally, the study was conducted on a self-selected sample.
Notwithstanding these limitations, our current study shows that face-to-face treatment outperformed the online treatment. It cannot be ruled out that face-to-face treatment is more effective by mainly increasing the completion rates, although this explanation seems unlikely as the data on the treatment completers sample show highly similar effects to the intent-to-treat sample (Table S7 and S8, supplemental material). The first and most important step is now to replicate these results. We therefore encourage future studies with similar designs (preferably with an active control condition) to examine whether individual face-to-face treatment is indeed more effective that online treatment for insomnia.
In conclusion, our results indicate that face-to-face treatment for insomnia is more effective than online treatment. Yet, as online treatment also resulted in large effect sizes, our findings suggest that online treatment may offer a potentially cost-effective51 alternative and complement to face-to-face treatment. Indeed, large effect sizes were achieved by the online treatment and these gains were achieved by low-cost labor in about 38% of the time investment associated with the face-to-face treatment. Presumably, this means that the cost of online treatment is lower. Furthermore, specifically trained face-to-face treatment providers may not be generally or sufficiently available (e.g., in remote areas). Accordingly, if face-to-face treatment for individuals with insomnia is (perceived of as) not readily accessible, or if is not the client-preferred treatment format, online treatment offers an effective alternative. An interesting question for future research is to identify which individuals benefit from online treatment versus those who do not, and who may require face-to-face treatment, but such research would require (much) larger samples. Alternatively, one might envision a stepped care approach, in which individuals first receive online treatment and only if indicated subsequent face-to-face treatment.15
DISCLOSURE STATEMENT
The online and face-to-face treatments were made possible by financial support from VGZ insurance company. The authors have indicated no financial conflicts of interest.
ACKNOWLEDGMENTS
The authors thank Jorn Leistra from VGZ and Taco Bos from Slaapmakend for arranging the financial support and their valuable input on the design. We thank Barbara Mulder from Slaapmakend for carrying out the face-to-face treatment. We thank Rachel Renet, Marlene Stone, Britt van Hest, Noraly Dekkers, and Kristopher van Zanten for providing the feedback in the online condition. The intervention protocol in this study was offered by means of an advanced content management system (CMS) for intervention through the internet developed by Professor M.J. Sorbi with former support of the Health Insurers Innovation Foundation (1222).
REFERENCES
- 1.Ohayon MM. Epidemiology of insomnia: what we know and what we still need to learn. Sleep Med Rev. 2002;6:97–111. doi: 10.1053/smrv.2002.0186. [DOI] [PubMed] [Google Scholar]
- 2.American Psychiatric Association. 5th ed. Arlington, VA: American Psychiatric Association; 2013. Diagnostic and Statistical Manual of Mental Disorders. [Google Scholar]
- 3.LeBlanc M, Beaulieu-Bonneau S, Merette C, Savard J, Ivers H, Morin CM. Psychological and health-related quality of life factors associated with insomnia in a population-based sample. J Psychosom Res. 2007;63:157–66. doi: 10.1016/j.jpsychores.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 4.Roth T, Drake C. Evolution of insomnia: current status and future direction. Sleep Med. 2004;5(Suppl 1):S23–30. doi: 10.1016/s1389-9457(04)90004-4. [DOI] [PubMed] [Google Scholar]
- 5.Kyle SD, Morgan K, Espie C. Insomnia and health-related quality of life. Sleep Med Rev. 2010;14:69–82. doi: 10.1016/j.smrv.2009.07.004. [DOI] [PubMed] [Google Scholar]
- 6.Baglioni C, Battagliese G, Feige B, et al. Insomnia as a predictor of depression: a meta-analytic evaluation of longitudinal epidemiological studies. J Affect Disord. 2011;135:10–9. doi: 10.1016/j.jad.2011.01.011. [DOI] [PubMed] [Google Scholar]
- 7.Taylor DJ, Lichstein KL, Durrence HH, Reidel BW, Bush AJ. Epidemiology of insomnia, depression, and anxiety. Sleep. 2005;28:1457–64. doi: 10.1093/sleep/28.11.1457. [DOI] [PubMed] [Google Scholar]
- 8.Espie CA, Kyle SD, Hames P, Cyhlarova E, Benzeval M. The daytime impact of DSM-5 insomnia disorder: comparative analysis of insomnia subtypes from the Great British Sleep Survey. J Clin Psychiatry. 2012;73:e1478–84. doi: 10.4088/JCP.12m07954. [DOI] [PubMed] [Google Scholar]
- 9.Wojnar M, Ilgen MA, Wojnar J, McCammon RJ, Valenstein M, Brower KJ. Sleep problems and suicidality in the National Comorbidity Survey Replication. J Psychiatr Res. 2009;43:526–31. doi: 10.1016/j.jpsychires.2008.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mallon L, Broman JE, Hetta J. Sleep complaints predict coronary artery disease mortality in males: a 12-year follow-up study of a middle-aged Swedish population. J Intern Med. 2002;251:207–16. doi: 10.1046/j.1365-2796.2002.00941.x. [DOI] [PubMed] [Google Scholar]
- 11.Glass J, Lanctot KL, Herrmann N, Sproule BA, Busto UE. Sedative hypnotics in older people with insomnia: meta-analysis of risks and benefits. Br Med J. 2005;331:1169–73. doi: 10.1136/bmj.38623.768588.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Riemann D, Perlis ML. The treatments of chronic insomnia: a review of benzodiazepine receptor agonists and psychological and behavioral therapies. Sleep Med Rev. 2009;13:205–14. doi: 10.1016/j.smrv.2008.06.001. [DOI] [PubMed] [Google Scholar]
- 13.Smith TS, Perlis ML, Park A, et al. Comparative meta-analysis of pharmacotherapy and behavior therapy for persistent insomnia. Am J Psychiat. 2002;159:5–11. doi: 10.1176/appi.ajp.159.1.5. [DOI] [PubMed] [Google Scholar]
- 14.Kyle SD, Miller CB, Rogers Z, Siriwardena AN, Macmahon KM, Espie CA. Sleep restriction therapy for insomnia is associated with reduced objective total sleep time, increased daytime somnolence, and objectively impaired vigilance: implications for the clinical management of insomnia disorder. Sleep. 2014;37:229–37. doi: 10.5665/sleep.3386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Espie CA. “Stepped Care”: a health technology solution for delivering cognitive behavioral therapy as a first line insomnia treatment. Sleep. 2009;32:1549–58. doi: 10.1093/sleep/32.12.1549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cheng SK, Dizon J. Computerised cognitive behavioural therapy for insomnia: a systematic review and meta-analysis. Psychother Psychosom. 2012;81:206–16. doi: 10.1159/000335379. [DOI] [PubMed] [Google Scholar]
- 17.Ho FY, Chung KF, Yeung WF, et al. Self-help cognitive-behavioral therapy for insomnia: a meta-analysis of randomized controlled trials. Sleep Med Rev. 2015;19:17–28. doi: 10.1016/j.smrv.2014.06.010. [DOI] [PubMed] [Google Scholar]
- 18.Lancee J, van den Bout J, Sorbi MJ, van Straten A. Email support improves the effectiveness of internet-delivered self-help treatment for insomnia: a randomized trial. Behav Res Ther. 2013;51:797–805. doi: 10.1016/j.brat.2013.09.004. [DOI] [PubMed] [Google Scholar]
- 19.Johnston L, Titov N, Andrews G, Spence J, Dear BF. A RCT of a transdiagnostic internet-delivered treatment for three anxiety disorders: examination of support roles and disorder-specific outcomes. PloS ONE. 2011;6:e28079. doi: 10.1371/journal.pone.0028079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ritterband LM, Thorndike FP, Gonder-Frederick LA, et al. Efficacy of an internet-based behavioral intervention for adults with insomnia. Arch Gen Psychiatry. 2009;66:692–8. doi: 10.1001/archgenpsychiatry.2009.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Espie CA, Kyle SD, Williams C, et al. A randomized, placebo-controlled trial of online cognitive behavioral therapy for chronic insomnia disorder delivered via an automated media-rich web application. Sleep. 2012;35:769–81. doi: 10.5665/sleep.1872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.van Straten A, Emmelkamp J, de Wit J, et al. Guided internet-delivered cognitive behavioral treatment for insomnia: a randomized trial. Psychol Med. 2014;44:1521–32. doi: 10.1017/S0033291713002249. [DOI] [PubMed] [Google Scholar]
- 23.Kaldo V, Jernelöv S, Blom K, et al. Guided internet cognitive behavioral therapy for insomnia compared to a control treatment - a randomized trial. Behav Res Ther. 2015;71:90–100. doi: 10.1016/j.brat.2015.06.001. [DOI] [PubMed] [Google Scholar]
- 24.Cuijpers P, Donker T, van Straten A, Li J, Andersson G. Is guided self-help as effective as face-to-face psychotherapy for depression and anxiety disorders? A systematic review and meta-analysis of comparative outcome studies. Psychol Med. 2010:40. doi: 10.1017/S0033291710000772. [DOI] [PubMed] [Google Scholar]
- 25.Andersson G, Cuijpers P, Carlbring P, Riper H, Hedman E. Guided Internet-based vs. face-to-face cognitive behavior therapy for psychiatric and somatic disorders: a systematic review and meta-analysis. World Psychiatry. 2014;13:288–95. doi: 10.1002/wps.20151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Blom K, Tarkian Tillgren H, Wiklund T, et al. Internet- vs. group-delivered cognitive behavior therapy for insomnia: a randomized controlled non-inferiority trial. Behav Res Ther. 2015;70:47–55. doi: 10.1016/j.brat.2015.05.002. [DOI] [PubMed] [Google Scholar]
- 27.Morin CM, Belleville G, Belanger L, Ivers H. The insomnia severity index: psychometric indicators to detect insomnia cases and evaluate treatment response. Sleep. 2011;34:601–8. doi: 10.1093/sleep/34.5.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Spoormaker VI, Verbeek I, van den Bout J, Klip EC. Initial validation of the SLEEP-50 questionnaire. Behav Sleep Med. 2005;3:227–46. doi: 10.1207/s15402010bsm0304_4. [DOI] [PubMed] [Google Scholar]
- 29.Morin CM. New York: Guilford Press; 1993. Insomnia: psychological assessment and management. [Google Scholar]
- 30.Bastien CH, Vallières A, Morin CM. Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med. 2001;2:297–307. doi: 10.1016/s1389-9457(00)00065-4. [DOI] [PubMed] [Google Scholar]
- 31.Thorndike FP, Ritterband LM, Saylor DK, Magee JC, Gonder-Frederick LA, Morin CM. Validation of the insomnia severity index as a web-based measure. Behav Sleep Med. 2011;9:216–23. doi: 10.1080/15402002.2011.606766. [DOI] [PubMed] [Google Scholar]
- 32.Bouma J, Ranchor AV, Sanderman R, van Sonderen E. Groningen: Noordelijk Centrum voor Gezondheidsvraagstukken; 1995. Het meten van symptomen van depressie met de CES-D: een handleiding [Dutch translation of the Epidemiological Studies-Depression scale] [Google Scholar]
- 33.Radloff LS. The CES-D Scale: a self-report depression scale for research in the general population. Appl Psych Meas. 1977;1:385–401. [Google Scholar]
- 34.Spinhoven P, Ormel J, Sloekers PP, Kempen GI, Speckens AE, Van Hemert AM. A validation study of the Hospital Anxiety and Depression Scale (HADS) in different groups of Dutch subjects. Psychol Med. 1997;27:363–70. doi: 10.1017/s0033291796004382. [DOI] [PubMed] [Google Scholar]
- 35.Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand. 1983;67:361–70. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 36.Carney CE, Buysse DJ, Ancoli-Israel S, et al. The consensus sleep diary: standardizing prospective sleep self-monitoring. Sleep. 2012;35:287–302. doi: 10.5665/sleep.1642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kyle SD, Aquino MR, Miller CB, et al. Towards standardisation and improved understanding of sleep restriction therapy for insomnia disorder: a systematic examination of CBT-I trial content. Sleep Med Rev. 2015;23:83–8. doi: 10.1016/j.smrv.2015.02.003. [DOI] [PubMed] [Google Scholar]
- 38.Morin CM, Espie CA. New York: Springer; 2003. Insomnia. A clinical guide to assessment and treatment. [Google Scholar]
- 39.Hox JJ. Mahwah: Lawrence Erlbaum Associates; 2002. Multilevel analysis: techniques and applications. [Google Scholar]
- 40.Sterne JA, White IR, Carlin JB, et al. Multiple imputation for missing data in epidemiological and clinical research: potentials and pitfalls. Br Med J. 2009:338. doi: 10.1136/bmj.b2393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cohen J. 2nd ed. New York: Lawrence Erlbaum Associates; 1988. Statistical Power Analysis for the Behavioral Sciences. [Google Scholar]
- 42.Koffel EA, Koffel JB, Gehrman PR. A meta-analysis of group cognitive behavioral therapy for insomnia. Sleep Med Rev. 2015;19:6–16. doi: 10.1016/j.smrv.2014.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kaldo V, Ranmerö J, Jernelöv S. Involving clients in treatment methods - a neglected interaction in the therapeutic relationship. J Consult Clin Psychol. 2015 Jul 13; doi: 10.1037/ccp0000039. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 44.Lancee J, van den Bout J, van Straten A, Spoormaker VI. Internet-delivered or mailed self-help treatment for insomnia? A randomized waiting-list controlled trial. Behav Res Ther. 2012;50:22–9. doi: 10.1016/j.brat.2011.09.012. [DOI] [PubMed] [Google Scholar]
- 45.Espie CA, Kyle SD, Miller CB, Ong J, Hames P, Fleming L. Attribution, cognition and psychopathology in persistent insomnia disorder: outcome and mediation analysis from a randomized placebo-controlled trial of online cognitive behavioural therapy. Sleep Med. 2014;15:913–7. doi: 10.1016/j.sleep.2014.03.001. [DOI] [PubMed] [Google Scholar]
- 46.Ho FY, Chung KF, Yeung WF, Ng TH, Cheng SK. Weekly brief phone support in self-help cognitive behavioral therapy for insomnia disorder: relevance to adherence and efficacy. Behav Res Ther. 2014;63:147–56. doi: 10.1016/j.brat.2014.10.002. [DOI] [PubMed] [Google Scholar]
- 47.Geiger-Brown JM, Rogers VE, Liu W, Ludeman EM, Downton KD, Diaz-Abad M. Cognitive behavioral therapy in persons with comorbid insomnia: a meta-analysis. Sleep Med Rev. 2015;23:54–67. doi: 10.1016/j.smrv.2014.11.007. [DOI] [PubMed] [Google Scholar]
- 48.Harvey AG, Belanger L, Talbot L, et al. Comparative efficacy of behavior therapy, cognitive therapy, and cognitive behavior therapy for chronic insomnia: a randomized controlled trial. J Consult Clin Psychol. 2014;82:670–83. doi: 10.1037/a0036606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Morin CM, Vallieres A, Guay B, et al. Cognitive behavioral therapy, singly and combined with medication, for persistent insomnia: a randomized controlled trial. JAMA. 2009;301:2005–15. doi: 10.1001/jama.2009.682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Phillips B, Hening W, Britz P, Mannino D. Prevalence and correlates of restless legs syndrome: results from the 2005 National Sleep Foundation Poll. Chest. 2006;129:76–80. doi: 10.1378/chest.129.1.76. [DOI] [PubMed] [Google Scholar]
- 51.Warmerdam L, Smit F, van Straten A, Riper H, Cuijpers P. Cost-utility and cost-effectiveness of internet-based treatment for adults with depressive symptoms: randomized trial. J Med Internet Res. 2010;12:e53. doi: 10.2196/jmir.1436. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.



