Abstract
Background:
The intake of green tea has been increased recently due to its medicinal values. The antibacterial and antioxidant properties of green tea were found to be beneficial in the treatment of gingival and periodontal diseases. The aim of this comparative study was to compare the efficacy of the mouthwash containing green tea and chlorhexidine in the management of dental plaque-induced gingivitis.
Materials and Methods:
Thirty patients who participated in the study were divided randomly into two groups, each group of 15 patients was prescribed with either chlorhexidine or green tea mouthwash. Turesky modification of Quigley-Hein plaque index, Löe and Silness gingival index, Ainamo and Bay bleeding index, tooth stain, and tongue stain (TS) were recorded at baseline, 15 days, and 1 month. The subjects were asked to report any discomfort or alteration in taste.
Results:
There was a significant decrease in plaque index, gingival index, and bleeding index in both the groups. However, green tea mouthwash resulted in a statistically significant decrease in bleeding index compared to chlorhexidine group. There was no significant difference in tooth stain and TS in both the groups.
Conclusion:
The green tea-containing mouthwash is equally effective in reducing the gingival inflammation and plaque to chlorhexidine.
Keywords: Chlorhexidine, dental plaque, gingivitis, green tea, mouthwash, plaque control
Introduction
Dental plaque is the major etiologic agent for the initiation of gingivitis.[1] Gingival disease can progress to periodontitis which if left untreated may eventually compromise the entire periodontium.[2] Regular plaque control helps in controlling the progression of gingival diseases. Mechanical plaque control remains the gold standard of periodontal therapy. However, mechanical plaque control by means of tooth brushing and flossing is not always completely effective as it is based on the dexterity and motivational level of individual.[2] Moreover, bacteria present in the soft tissues can re-colonize the tooth surfaces even after mechanical plaque control.[3] Adjunctive use of chemical plaque control agents had shown better efficacy in the control of plaque and gingival inflammation.[4]
Chlorhexidine[5] still remains the gold standard against which the efficacy of newer antiplaque agents is compared because of its superior antiplaque effect and its substantivity for a period of 10–12 h. However, the side effects of chlorhexidine such as tooth and tongue staining, taste alterations, and mucosal erosions limit patient compliance.[5,6] There are a huge number of chemical plaque control agents emerging in the market focusing on the reduction of plaque and gingival inflammation.
India is a rich source of natural herbal products which have been used both topically and systemically for disease treatment. Unfortunately, the usage is very limited due to scant product testing.[7]
Tea is the second most commonly consumed liquid in the world after water.[8] Tea originates from the leaves of the plant Camellia sinensis.[9] It can be classified into three major types according to the level of fermentation: Green tea (not fermented), oolong tea (partially fermented), and black tea (fully fermented).[9,10,11]
Green tea is made solely with the leaves of C. sinensis that have undergone minimal oxidation during processing and hence it has more antioxidant and antibacterial properties.[10] The most abundant components in green tea are polyphenols, in particular, flavonoids such as the catechins.[7] Major catechins found in green tea are epicatechin gallate (ECG), epicatechin (EC), epigallocatechin (EGC), and EGC gallate (EGCG).[11] Green tea consumption was found to lower the incidence of cardiovascular disease, diabetes, and obesity.[12] Studies have shown that green tea polyphenols inhibit the growth of oral and periodontopathic bacteria thereby preventing dental caries, halitosis,[11] gingivitis, and periodontitis.[12] The beneficial effects of the natural products along with the lower prevalence of side effects could enhance patient compliance and long-term usage.
The aim of the present study was to compare the efficacy of green tea and chlorhexidine mouth rinses in the control of plaque and gingival inflammation.
Materials and Methods
Sample preparation
Leaves of green tea were fragmented and broken into small pieces and each 100 g of leaves were soaked in 500 ml of ethanol for 48 h. The leaves were filtered, kept on a plate, placed in hot air oven at 50°C for 3–4 days, and the extract was obtained. Finally, green tea mouthwash of 5%[12] was prepared by adding 0.5 g of the extract to 100 ml of distilled water and poured into bottles of 75 ml each.
The study was initially approved by the Institutional Review Committee. The single-blinded, randomized controlled trial was conducted on the patients seeking periodontal treatment at Chettinad Dental College and Research Institute and was screened for suitability. The age range of the patients was between 18 and 24 years. The examiner was completely blinded throughout the procedure. To be eligible for the study, the following inclusion and exclusion criteria were applied. Patients with a gingival index score of ≥1 at more than 60% of sites, plaque index of one or more, probing depths not more than 3 mm, and no clinical attachment loss were included in the study. In general, patients were in good medical health and were free from major oral hard or soft tissue lesions.
Systemic and/or topical steroidal and nonsteroidal anti-inflammatory drugs and the patients under antibiotics during the last 6 weeks prior to the study, fixed or removable orthodontic device, oral soft tissue pathology, physical or mental handicap that could interfere with adequate oral hygiene performance, and patients who underwent oral prophylaxis in the last 6 months were excluded from the study.
A total of 34 patients who satisfied the eligibility criteria were enrolled the study. Verbal and written information sheets were provided to the study patients with the details about the nature of the study and proposed claims for the product and the alternatives. However, only 30 patients expressed their willingness to participate in the study.
The patients were provided with mouth rinses according to a random number table (15 each) with 50 percent of the patients prescribed either with green tea-containing mouth rinse or a chlorhexidine mouth rinse. The random allocation sequence was concealed from the main investigator. The patients were instructed to use the prescribed rinses 30 min after tooth brushing. Written and verbal oral hygiene instructions were administered to all the patients. The modified bass technique[13] was demonstrated on the study models.
Clinical measurements were taken at baseline (prior to the study), at 15 days, and at the end of the study (4 weeks). Patients’ perception of odor, taste, and any discomfort were recorded. A single examiner, blinded to the mouth rinse used, performed all the measurements. The decoding of mouthrinses was made only after completion of all data acquisition and termination of the study.
At each visit, scoring of supragingival plaque was done using Turesky modification of the Quigley-Hein plaque index.[14] Scoring of gingival inflammation (gingivitis) was done using gingival index of Löe[15] and scoring of gingival bleeding was done by bleeding index of Ainamo and Bay.[16] Assessment of gingivitis was done prior to the scoring of plaque to avoid masking the gingival inflammation with plaque-disclosing agents.
Presence of stain on teeth was assessed by means of a gingival modification of the stain index (Gründemann et al. 2000).[17] Each examined tooth was divided into four zones and the intensity of each zone was subjectively scored, where 0 = stain, 1 = light stain (yellow), 2 = medium stain (brown), and 3 = heavy stain (black). Presence of tongue stain (TS) was assessed according to the method reported by Claydon et al. (2001).[18] Stain on the dorsal anterior two-thirds of the tongue were scored as follows: (a) Stain area: As a percentage where 0 = no stain; 1 = 1–25% coverage; 2 = 26–50% coverage; 3 = 51–75% coverage; 4 = 76–100% coverage and (b) stain intensity: Subjectively scored as 0 = no stain; 1 = light stain (yellow); 2 = medium stain (brown); and 3 = dark stain (black). For intensity scores where mixed colors were observed, the higher score was applied. Teeth and TS were assessed at baseline, 15 days, and at the end of 4 weeks.
Statistical analysis
The results were analyzed using SPSS software version 17.0 (IBM Corporation, Chicago, IL, USA). Unpaired t-test was used to assess the difference between the groups and paired test was used to compare the difference within the groups at different time periods.
Results
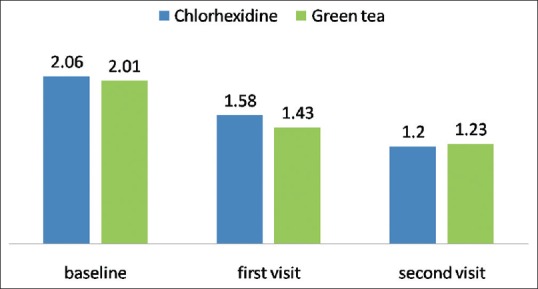
There was a significant decrease in the gingival index, plaque index, and bleeding index for both the mouthwashes at first and second visits as shown in Tables 1 and 2 and Figures 1–3, respectively. The plaque index showed a significant decrease in the first and second visits (P < 0.05). The gingival index decreased significantly from baseline to the subsequent visits. There was no statistically significant difference between the groups for gingival and plaque index at both the visits. However, patients under green tea mouthwash showed more reduction of bleeding scores and were statistically significant at the end of both the visits (P < 0.05). There was no significant difference between the groups for both tongue and tooth stain.
Table 1.
Comparison of clinical parameters at baseline and at first visit (15 days)
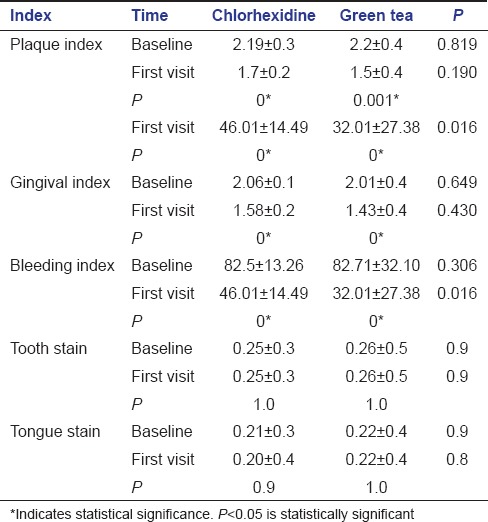
Table 2.
Comparison of clinical parameters at first and at second visit (30 days)
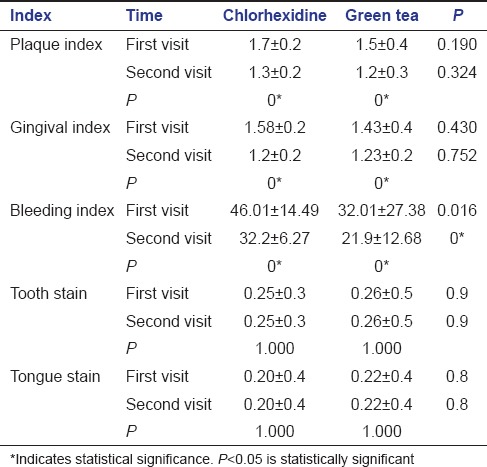
Figure 1.
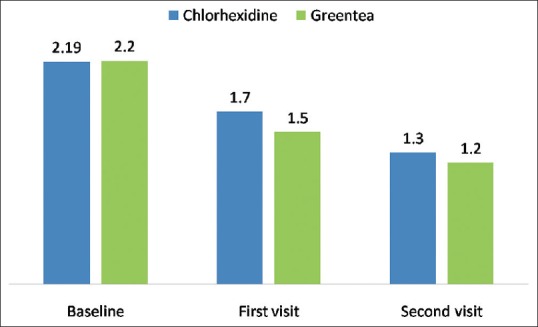
Change in the plaque index between the groups at different visits
Figure 3.
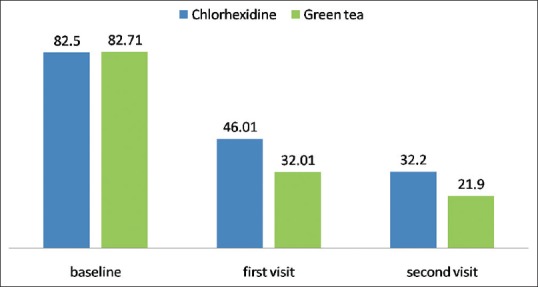
Changes in the bleeding index between the groups at different visits
Figure 2.
Changes in the gingival index between the groups at different visits
Discussion
Chemical plaque control agents act as effective adjuncts to mechanical plaque control in preventing plaque formation and gingival inflammation. Chemical plaque control agents are prescribed in the form of mouthwashes, irrigation solutions, and local drug delivery agents. Chlorhexidine[19] remains the gold standard antiplaque agent due to its superior substantivity and antiplaque effect. The major side effects of chlorhexidine include brownish discoloration of teeth and tongue, formation of supragingival calculus, taste alteration, and oral desquamation in children. In addition, allergic reaction has been reported, especially in some Asian patients.
The practice of alternate medicine with the use of plant and plant products have evolved widely in the form of mouth rinses and toothpastes. They have been shown to possess beneficial effects in the control of plaque and gingival inflammation.[20] Moreover, the drug resistance associated with the misuse of chemotherapeutic agents can be considerably reduced with the use of plant extracts.[21] Plant products of aloe, amla, babool, blue berry, Ginkgo biloba, Eucalyptus, marigold, myrrh, miswak, green tea, propolis, turmeric, rose, tulsi, and neem were found to have antioxidant, anti-inflammatory, antiseptic, antibacterial, and astringent properties. India has a rich source of these plant products.[21]
Among the 4000 bioactive compounds present in green tea, one-third is isopolyphenols. The most important of these polyphenols are tannins and flavonoids. The main flavonoids present in green tea include catechins (flavan-3-ols) such as EGC-3-gallate that represent approximately 59% of total catechins, EGC (19% approximately), EC-3-gallate (13.6% approximately), and EC (6.4% approximately).[22] Catechin was found to have antiplaque and antibacterial properties and contributed in caries prevention and in gingival enlargement.[23] Green tea is also a powerful antioxidant and has anti-inflammatory properties. Antioxidants play an important role in the control of gingival inflammation by inhibiting the oxidative stress.[24]
Green tea has been reported to be useful for the prevention of periodontal disease and maintenance of oral health. In the present study, there was a significant decrease in the plaque index in both the groups at the subsequent visits. Green tea has found to decrease the plaque formation in previous studies.[10,23,24] An epidemiologic study showed that there is an inverse association between the daily intake of green tea and periodontal disease, and suggested that drinking green tea at meals and breaks is a relatively easy habit to maintain a healthy periodontium (Kushiyama et al. 2009).[24] Green tea catechins and polyphenols in sugar-free chewing candies were found to have a positive influence on the inflammatory reaction of periodontal structures.[25] Green and black tea were reported to prevent gathering of bacteria and thereby preventing plaque formation on teeth.[10] Similarly, in a single-blinded cross-over study by Arab et al. on 30 participants concluded that the green tea catechin mouthwash (0.25%) and chlorhexidine mouthwash (0.12%) showed comparable results in plaque reduction.[12]
Green tea catechins, such as EGC, were found to inhibit the growth of periodontopathic bacteria such as Porphyromonas gingivalis, Prevotella intermedia, and Prevotella nigrescens, and the adherence of P. gingivalis onto human buccal epithelial cells in vitro (Makimura et al. 1993).[26] EGCG has been reported to inhibit production of toxic metabolites of P. gingivalis.[27] It has also been shown that purified tea polyphenols inhibited in vitro growth and hydrogen sulfide production of P. gingivalis and Fusobacterium nucleatum associated with human halitosis. The green tea induced decrease in the periodontopathic bacteria and reduced inflammation could have attributed to the significant decrease of bleeding index in the present study. However, in the study done by Ardakani et al., the in vitro anti-microbial activity of green tea was found to be inferior to 0.2% chlorhexidine though it had a considerable bactericidal effect.[28]
Green tea has shown inhibitory effect on collagenolytic enzymes thereby preventing periodontal inflammation. Green tea catechin significantly reduces the expression of matrix metalloproteinase-9 in osteoblasts and also inhibits the formation of osteoclast. Thus, EGCG may prevent alveolar bone resorption that occurs in periodontal disease.[29] Tea catechins containing the galloyl radicals possess the ability to inhibit both eukaryotic and prokaryotic cell-derived collagenase, an enzyme that plays an important role in the disruption of the collagen component in the gingival tissues of patients with periodontal disease. Green tea catechins have also been shown to inhibit protein tyrosine phosphatase in P. intermedia.[13]
In the present study, there is a significant decrease in the gingival index in both the groups at different visits. The decrease in the gingival index in green tea group is probably due to decreased collagenolytic activity and inhibitory effect on periodontal pathogens. However, in a clinical study performed on tea polyphenols in the form of chew candies on gingival inflammation over a 4 weeks period showed that the tea polyphenols might exert a positive influence on gingival inflammation. However, the reduction of the approximal plaque index and sulcus bleeding index was not statistically significant.[25]
A randomized blinded controlled trial was carried out with three groups of 30 human volunteers who were prescribed with 0.2% chlorhexidine gluconate, 2% neem, and 0.5% tea of 10 subjects per group. The effectiveness of 0.5% tea on the clinical parameters of plaque index and gingival index was more compared to 2% neem and 0.2% chlorhexidine mouth rinse.[9] In contrast, a single-blinded placebo-controlled clinical trial was conducted among high school female students with plaque-induced gingivitis and were distributed to receive either 5 ml of green tea 5% 2 times/days or normal saline with the same dosage. Gingival index (Sillness and Loe), plaque index (Sillness and Loe), and bleeding index (Barnett) were recorded at baseline and 5 consecutive weeks. Although total amount of improvement was higher in green tea mouthwash group, the differences did not reach a statistically significant level.[30]
The present study was carried out in a smaller sample size in a 4 weeks duration to assess the antiplaque and antigingivitis effect of two mouthwashes as per the Americans with Disabilities Act guidelines.[31] Further long-term studies should be carried out with more sample size. Green tea mouthwash can be recommended as a safe, anti-inflammatory, and anti-microbial mouthwash to control gingival inflammation and to maintain good oral and gingival health.
Conclusion
Both the mouthwashes were equally effective in reducing plaque and gingival inflammation, considering the fact that the chemical formulations of commercially available mouth rinses are chemically based, expensive, and have considerable side effects, which restricts their use. India has a rich source of herbal plant products with medicinal value. Green tea can be used as adjuvant to oral hygiene maintenance with a goal on the prevention as well as the prevalence of periodontal diseases due to its antibacterial and antioxidant properties.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Page RC, Kornman KS. The pathogenesis of human periodontitis: An introduction. Periodontol 2000. 1997;14:9–11. doi: 10.1111/j.1600-0757.1997.tb00189.x. [DOI] [PubMed] [Google Scholar]
- 2.Teles RP, Teles FR. Antimicrobial agents used in the control of periodontal biofilms: Effective adjuncts to mechanical plaque control? Braz Oral Res. 2009;23(Suppl 1):39–48. doi: 10.1590/s1806-83242009000500007. [DOI] [PubMed] [Google Scholar]
- 3.Socransky SS, Haffajee AD. Periodontal microbial ecology. Periodontol 2000. 2005;38:135–87. doi: 10.1111/j.1600-0757.2005.00107.x. [DOI] [PubMed] [Google Scholar]
- 4.Moran JM. Chemical plaque control – Prevention for the masses. Periodontol 2000. 1997;15:09–17. doi: 10.1111/j.1600-0757.1997.tb00110.x. [DOI] [PubMed] [Google Scholar]
- 5.Jones CG. Chlorhexidine: Is it still the gold standard? Periodontol 2000. 1997;15:55–62. doi: 10.1111/j.1600-0757.1997.tb00105.x. [DOI] [PubMed] [Google Scholar]
- 6.Mathur S, Mathur T, Shrivastava R, Khatri R. Chlorhexidine: The gold standard in chemical plaque control. Natl J Physiol Pharm Pharmacol. 2011;1:45–50. [Google Scholar]
- 7.Balappanavar AY, Sardana V, Singh M. Comparison of the effectiveness of 0.5% tea, 2% neem and 0.2% chlorhexidine mouthwashes on oral health. A randomized control trial. Indian J Dent Res. 2013;24:26–34. doi: 10.4103/0970-9290.114933. [DOI] [PubMed] [Google Scholar]
- 8.Moghbel A, Farjzadeh A, Aghel N, Agheli H, Raisi N. The effect of green tea on prevention of mouth bacterial infection, halitosis, and plaque formation on teeth. Iran J Toxicol. 2011;14:502–15. [Google Scholar]
- 9.Cheng TO. All teas are not created equal: The Chinese green tea and cardiovascular health. Int J Cardiol. 2006;108:301–8. doi: 10.1016/j.ijcard.2005.05.038. [DOI] [PubMed] [Google Scholar]
- 10.Kaur H, Jain S, Kaur A. Comparative evaluation of the antiplaque effectiveness of green tea catechin mouthwash with chlorhexidine gluconate. J Indian Soc Periodontol. 2014;18:178–82. doi: 10.4103/0972-124X.131320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Okamoto M, Sugimoto A, Leung KP, Nakayama K, Kamaguchi A, Maeda N. Inhibitory effect of green tea catechins on cysteine proteinases in Porphyromonas gingivalis. Oral Microbiol Immunol. 2004;19:118–20. doi: 10.1046/j.0902-0055.2003.00112.x. [DOI] [PubMed] [Google Scholar]
- 12.Arab H, Maroofian A, Golestani S, Shafaee H, Sohrabi K, Forouzanfar A. Review of the therapeutic effects of Camellia sinensis (green tea) on oral and periodontal health. J Med Plants Res. 2011;5:5465–9. [Google Scholar]
- 13.Poyato-Ferrera M, Segura-Egea JJ, Bullón-Fernández P. Comparison of modified bass technique with normal toothbrushing practices for efficacy in supragingival plaque removal. Int J Dent Hyg. 2003;1:110–4. doi: 10.1034/j.1601-5037.2003.00018.x. [DOI] [PubMed] [Google Scholar]
- 14.Turesky S, Gilmore ND, Glickman I. Reduced plaque formation by the chloromethyl analogue of victamine C. J Periodontol. 1970;41:41–3. doi: 10.1902/jop.1970.41.41.41. [DOI] [PubMed] [Google Scholar]
- 15.Löe H. The gingival index, the plaque index and the retention index systems. J Periodontol. 1967;38(Suppl):610–6. doi: 10.1902/jop.1967.38.6.610. [DOI] [PubMed] [Google Scholar]
- 16.Ainamo J, Bay I. Problems and proposals for recording gingivitis and plaque. Int Dent J. 1975;25:229–35. [PubMed] [Google Scholar]
- 17.Gründemann LJ, Timmerman MF, Ijzerman Y, van der Weijden GA, van der Weijden GA. Stain, plaque and gingivitis reduction by combining chlorhexidine and peroxyborate. J Clin Periodontol. 2000;27:9–15. doi: 10.1034/j.1600-051x.2000.027001009.x. [DOI] [PubMed] [Google Scholar]
- 18.Claydon N, Addy M, Jackson R, Smith S, Newcombe RG. Studies on the effect of polyvinyl pyrrolidone on the activity of chlorhexidine mouthrinses: Plaque and stain. J Clin Periodontol. 2001;28:558–64. doi: 10.1034/j.1600-051x.2001.028006558.x. [DOI] [PubMed] [Google Scholar]
- 19.Balagopal S, Arjunkumar R. Chlorhexidine: The gold standard antiplaque agent. J Pharm Sci Res. 2013;5:270–4. [Google Scholar]
- 20.Rao NJ, Subash KR, Kumar KS. Role of phytotherapy in gingivitis: A review. Int J Pharmacol. 2012;8:1–5. [Google Scholar]
- 21.Salgado AD, Maia JL, Pereira SL, de Lemos TL, Mota OM. Antiplaque and antigingivitis effects of a gel containing Punica granatum linn extract: A double-blind clinical study in humans. J Appl Oral Sci. 2006;14:162–6. doi: 10.1590/S1678-77572006000300003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Venkateswara B, Sirisha K, Chava VK. Green tea extract for periodontal health. J Indian Soc Periodontol. 2011;15:18–22. doi: 10.4103/0972-124X.82258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cabrera C, Artacho R, Giménez R. Beneficial effects of green tea – A review. J Am Coll Nutr. 2006;25:79–99. doi: 10.1080/07315724.2006.10719518. [DOI] [PubMed] [Google Scholar]
- 24.Kushiyama M, Shimazaki Y, Murakami M, Yamashita Y. Relationship between intake of green tea and periodontal disease. J Periodontol. 2009;80:372–7. doi: 10.1902/jop.2009.080510. [DOI] [PubMed] [Google Scholar]
- 25.Krahwinkel T, Willershausen B. The effect of sugar-free green tea chew candies on the degree of inflammation of the gingiva. Eur J Med Res. 2000;5:463–7. [PubMed] [Google Scholar]
- 26.Makimura M, Hirasawa M, Kobayashi K, Indo J, Sakanaka S, Taguchi T, et al. Inhibitory effect of tea catechins on collagenase activity. J Periodontol. 1993;64:630–6. doi: 10.1902/jop.1993.64.7.630. [DOI] [PubMed] [Google Scholar]
- 27.Sakanaka S, Okada Y. Inhibitory effects of green tea polyphenols on the production of a virulence factor of the periodontal-disease-causing anaerobic bacterium Porphyromonas gingivalis. J Agric Food Chem. 2004;52:1688–92. doi: 10.1021/jf0302815. [DOI] [PubMed] [Google Scholar]
- 28.Ardakani MR, Golmohammadi S, Ayremlou S, Taheri S, Daneshvar S, Meimandi M. Antibacterial effect of Iranian green-tea-containing mouthrinse vs chlorhexidine 0.2%: An in vitro study. Oral Health Prev Dent. 2014;12:157–62. doi: 10.3290/j.ohpd.a31663. [DOI] [PubMed] [Google Scholar]
- 29.Yun JH, Pang EK, Kim CS, Yoo YJ, Cho KS, Chai JK, et al. Inhibitory effects of green tea polyphenol (-)-epigallocatechin gallate on the expression of matrix metalloproteinase-9 and on the formation of osteoclasts. J Periodontal Res. 2004;39:300–7. doi: 10.1111/j.1600-0765.2004.00743.x. [DOI] [PubMed] [Google Scholar]
- 30.Jenabian N, Moghadamnia AA, Karami E, Mir A PB. The effect of Camellia sinensis (green tea) mouthwash on plaque-induced gingivitis: A single-blinded randomized controlled clinical trial. Daru. 2012;20:39. doi: 10.1186/2008-2231-20-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Acceptance Program Guidelines Chemotherapeutic Products for Control of Gingivitis, (ADA) American Dental Association®. Council on Scientific Affairs; November. 2011. [Last assessed 15 March 2014]. Available from: http://www.ada.org/~/media/ADA/Science%20and%20Research/Files/Seal%20guidelines/SCI_SealGuidelineChemotherepeuticProdforControlofGingivitis_2011Nov01.ashx .


