Abstract
Endodontic treatment options for immature, nonvital teeth conventionally include surgical endodontics, apexification with calcium hydroxide, or single visit mineral trioxide aggregate plug. Regeneration is a new concept which is been introduced in the treatment of traumatized open apex tooth. Regeneration of pulp-dentin complex in an infected necrotic tooth with an open apex is possible if the canal is effectively disinfected. The purpose of this case report is to add a new vista in regenerative, endodontic therapy by using platelet-rich fibrin for revitalization of immature nonvital tooth.
Keywords: Open apex, regeneration, revitalization
Introduction
Immature teeth that have open and often divergent apices are not suitable for complete cleaning and obturation with traditional techniques and materials. In addition, because of their thin dentinal walls, these teeth are susceptible to subsequent fracture after treatment.[1] Teeth with necrotic pulps and immature apexes present special challenges to clinicians during obturation. Traditionally, the apexification procedure consists of multiple and long-term applications of, calcium hydroxide was used to create an apical barrier before obturation of root canals.[1] Because, this procedure might alter the mechanical properties of dentin and make these teeth more susceptible to fracture.[2] A one step or two step apexification procedure with mineral trioxide aggregate (MTA) has shown high success rates.[1] However, this procedure might not result in complete root formation and might not completely reduce the chances of root fracture.[3]
Regeneration of tissues is always preferred over repair. The purpose of the present case report is to use platelet-rich fibrin (PRF) as the regenerative material of choice in carrying out the procedure.
Case Report
A 14-year-old boy reported to the department with the chief complaint of the broken upper front tooth along with discoloration [Figure 1]. The dental history revealed trauma to his upper front tooth. The medical history of the patient was noncontributory. Intraoral examination of his teeth revealed the presence of discolored tooth w.r.t 11 along with Ellis class IV fracture. Tooth 11 was sensitive to both percussion and periapical palpation tests. Both 11 and 12 did not respond to CO2 ice and electric pulp test. Periodontal probing depth of the tooth 11 was within normal limit. Intraoral periapical radiographic examination of tooth revealed an immature root and an open apex associated with periapical radiolucency [Figure 2].
Figure 1.

Preoperative clinical photograph w.r.t 11
Figure 2.

Preoperative X-ray
Further, radiographic examination of the tooth revealed a 3 mm open apex along with thin dentinal walls that appeared prone to fracture. Hence, a clinical decision of performing a regenerative endodontic treatment using Choukroun's PRF was decided. A written informed consent was obtained from the patient's mother. Local anesthesia was achieved using lignocaine (1:100000 adrenaline, DJ Lab, India). After the rubber dam application, access cavity preparation was done w.r.t 11 and 12. The canal was thoroughly irrigated with 20 ml of 5.25% sodium hypochlorite solution (Novo Dental Product, India) and nuetralized with saline. Following this, irrigation was done using 10 ml of hexidine solution (0.2% chlorhexidine, Vishal Dentocare, India) and dried with paper points (Dentsply Maillefer Ballaigues). A mixture of ciprofloxacin (cifran 500 mg, Ranbaxy Lab, India), metronidazole (metrogyl 400 mg, J. B. Chemicals and Pharmaceuticals, India), and minocycline paste (minoz 50 mg, Ranbaxy Lab, India) was prepared into a creamy consistency and introduced into the canal using a lentulo spiral w.r.t 11. A cotton pellet was placed, and the cavity was temporarily sealed with cavit (Dental Products of India, India).
The patient returned after 21 days to the clinic and was asymptomatic. Local anesthesia was given, followed by rubber dam isolation; then the access cavity was reopened and thoroughly irrigated with sterile saline solution and dried with paper points. A 10 ml sample of whole blood was drawn intravenously from the patient's right antecubital vein and centrifuged (REMI Model R-8c with 12 ml × 15 ml swing out head) under 3000 rpm for 10 min to obtain the PRF which was jelly-like in consistency. The PRF was condensed into the canal using a hand plugger (Dentsply Maillefer Ballaigues) until the level the cementoenamel junction [Figure 3]. Gray MTA (ProRoot MTA; Dentsply) was placed directly over the PRF to a thickness of 3 mm followed by a wet cotton pellet and cavit. The patient was recalled after 3 days, and the setting of MTA was confirmed. The access cavity was then double sealed with glass ionomer cement and composite restoration [Figure 4].
Figure 3.
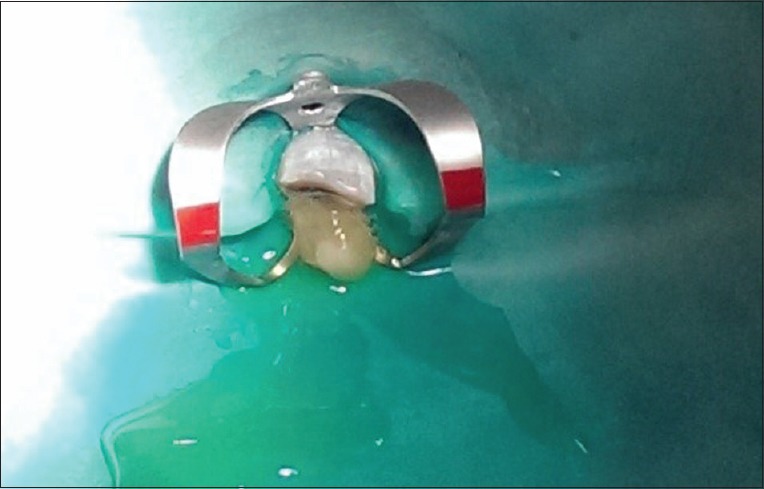
Platelet-rich fibrin placement into the canal
Figure 4.

After double coronal
The patient returned to the clinic after 3 months, 6 months, 9 months, 12 months, and 14 months for review and was asymptomatic; the tooth 11 showed negative response to percussion and palpation tests. The radiograph revealed regression of periapical lesion and initiation of root end closure [Figure 5]. Cone beam computed tomography (CBCT) evaluation is also carried out in order to confirm the results [Figures 6 and 7]. The patient is still under review.
Figure 5.

14 month follow up preoperative radiograph
Figure 6.

Sagittal section of CBCT with 14 months follow up
Figure 7.
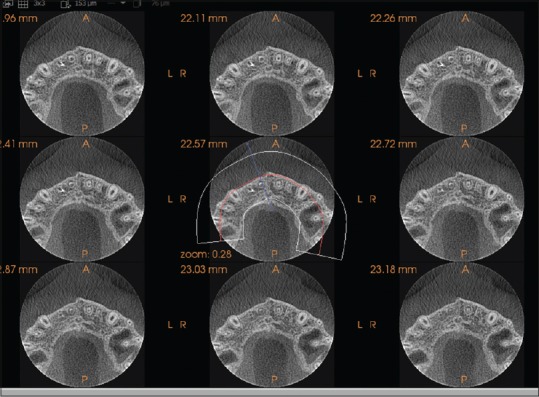
Axial section of CBCT with 14 months follow up
Discussion
Regenerative procedure in immature teeth was introduced in the field of endodontics by Ostby in 1961.[4] It leads to apexogenesis and maturogenesis in the necrotic immature permanent teeth. The thickened and convergent dentinal walls add to the long-term prognosis of the tooth by increasing its fracture resistance; hence in the present case, this novel technique was used.
Minimal instrumentation and copious irrigation were done with 2.5% NaOCl to achieve disinfection. Triple antibiotic paste,[5] a mixture of ciprofloxacin, metronidazole, and minocycline, was packed in the canal to achieve further reduction of microbial load.
PRF has been shown to have several advantages over traditionally prepared platelet-rich plasma–ease of preparation and lack of biochemical handling of blood, which makes this preparation strictly autologous; the PRF has a very significant slow sustained release of many key growth factors such as platelet-derived growth factor and transforming growth factor β for at least 1 week and up to 28 days, which means that PRF could release growth factors with its own biological scaffold for wound healing process.[6]
Directly over the PRF clot, the MTA was packed and condensed to obtain a tight coronal seal, and also MTA by itself provides signaling molecules for the growth of the stem cells.[7] The double coronal seal is done in order to provide a bacterial tight seal.
The case is followed at 3, 6, 9, 12, and 14 months radiographically. Even, the CBCT was carried out in order to confirm the results.
Conclusion
On the basis of short-term results of the present case report, it is reported that PRF is potentially an ideal scaffold for regeneration of vital tissue in the necrotic immature teeth. Long-term clinical trials and studies are needed in order to confirm its results and compare its efficacy with PRP and blood clot.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Hargreaves KM, Giesler T, Henry M, Wang Y. Regeneration potential of the young permanent tooth: What does the future hold? J Endod. 2008;34(7 Suppl):S51–6. doi: 10.1016/j.joen.2008.02.032. [DOI] [PubMed] [Google Scholar]
- 2.Andreasen JO, Farik B, Munksgaard EC. Long-term calcium hydroxide as a root canal dressing may increase risk of root fracture. Dent Traumatol. 2002;18:134–7. doi: 10.1034/j.1600-9657.2002.00097.x. [DOI] [PubMed] [Google Scholar]
- 3.Bose R, Nummikoski P, Hargreaves K. A retrospective evaluation of radiographic outcomes in immature teeth with necrotic root canal systems treated with regenerative endodontic procedures. J Endod. 2009;35:1343–9. doi: 10.1016/j.joen.2009.06.021. [DOI] [PubMed] [Google Scholar]
- 4.Ostby BN. The role of the blood clot in endodontic therapy. An experimental histologic study. Acta Odontol Scand. 1961;19:324–53. [PubMed] [Google Scholar]
- 5.Hoshino E, Kurihara-Ando N, Sato I, Uematsu H, Sato M, Kota K, et al. In-vitro antibacterial susceptibility of bacteria taken from infected root dentine to a mixture of ciprofloxacin, metronidazole and minocycline. Int Endod J. 1996;29:125–30. doi: 10.1111/j.1365-2591.1996.tb01173.x. [DOI] [PubMed] [Google Scholar]
- 6.Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, et al. Platelet-rich fibrin (PRF): A second-generation platelet concentrate. Part I: Technological concepts and evolution. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;101:e37–44. doi: 10.1016/j.tripleo.2005.07.008. [DOI] [PubMed] [Google Scholar]
- 7.Torabinejad M, Parirokh M. Mineral trioxide aggregate: A comprehensive literature review – Part II: Leakage and biocompatibility investigations. J Endod. 2010;36:190–202. doi: 10.1016/j.joen.2009.09.010. [DOI] [PubMed] [Google Scholar]


